Abstract
Previous studies have suggested an increase in the incidence of colorectal cancer (CRC) in young adults (younger than 50 years). Among older people, African Americans have disproportionally higher CRC incidence and mortality. It is unclear if this CRC disparity also applies to CRC diagnosed among young people
Methods
Using the Surveillance, Epidemiology, and End Results (SEER) cancer registries, a population-based cancer registry covering 25.6% of the United States’ African American population, we identified patients diagnosed with CRC between the years of 2000-2012. The age-adjusted rates for non-Hispanic whites (NHW), African Americans and Asian Pacific Islanders (API) were calculated for the age categories 20-24, 25-29, 30-34, 35-39, and 40-44.
Results
CRC age-adjusted incidence is increasing among all three racial groups and was higher for African Americans compared to NHW and API across all years 2000-2012 (P<0.001). Stage IV CRC was higher in African Americans compared with NHW while there was higher stage III CRC in API compared with NHWs.
Conclusion
CRC incidence is increasing among the young in all racial groups under study. This increase in frequency of CRC is true among young African American adults who display highly advanced tumors in comparison to other races. While the present attention to screening seems to have decreased CRC prevalence in individuals older than 50, special attention needs to be addressed to young African American adults as well, to counter the observed trend, as they have the highest incidence of CRC among young population groups by race/ethnicity.
Keywords: Colorectal Cancer, Race, Young Adults, SEER, Screening
Introduction
Colorectal cancer (CRC) is the third leading cause of cancer-related deaths for men and women in the United States [1]. For the year 2014, the American Cancer Society (ACS) published a report estimating 136,830 diagnoses and 50,310 deaths from colorectal cancer in men and women combined [1]. This is 4% less CRC diagnoses and 1% less deaths than the prior year [2]. In fact, despite its high position among the leading causes of cancers, it has been reported that for the past decade, the incidence of colorectal cancer has been decreasing, due to increased screening and diagnostic colonoscopy procedures [1,2]. This decrease in incidence is true for those aged 50 and older [3,4]. For individuals younger than the recommended screening guidelines, however, numerous studies have shown that the incidence is actually increasing [2,3,5-7]. Moreover, a study conducted by Amri et al. showed that cancers diagnosed in patients younger than 50 years of age have greater rates of metastasis, positive lymph nodes and extramural vascular invasion [8]. Therefore, colorectal cancer found in young adults is more likely to be diagnosed at an advanced stage and less likely to be curable, than if diagnosed at later age [2,8,9]. Researchers have correctly called for a greater focus on early detection efforts for young patient populations [9]. These findings are important not only because of the quality of life impact of cancer on the young but also because of the lack of screening efforts for this age group.
Historically, colorectal cancer incidence rates have been consistently higher in African Americans [1,10]. Recently, Siegel et al. showed rates that are highest in Africans Americans and lowest in Asian-Pacific Islanders (API) [11]. Given this information, it is therefore important to understand the effects of the apparent increased incidence on different racial and ethnic groups in the <50 age group. In the young population, some studies have reported stable or smaller increases in incidence in the African American population [3,12]. These findings are notable because African Americans have been confirmed to have a higher prevalence of CRC at all ages, poorer prognosis due to advanced stage tumors, be symptomatic at diagnosis, and be diagnosed at a younger age compared to their racial/ethnic counterparts[13]. The noted increase in CRC burden among blacks led to the recommendation that African Americans should undergo CRC screening from 45 years of age by the American College of Gastroenterology. In this study, we sought to examine incidence rates of CRC among 20-44 year old by race to determine whether young African Americans similar to their older counterparts, share a disproportionate burden of young-onset disease.
Methods & Materials
Incidence data from 2000 to 2012 were obtained from the National Cancer Institute's (NCI) Surveillance, Epidemiology, and End Results (SEER) program[14]. Incidence rates were based on data from all 18 SEER cancer registries (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New-Mexico, San Francisco-Oakland, Seattle-Puget Sound, Utah, Los Angeles, San-Jose-Monterey, Rural Georgia, Alaska, Greater California, Kentucky, Louisiana, New Jersey & Greater Georgia), covering approximately 27.8% of the total United States population and 25.6% of the African American population. Age-specific incidence rates for Whites, African Americans, and Asian-Pacific Islanders (API) were examined. An important consideration was that SEER-18 was adjusted to account for population changes as a result of hurricanes Katrina and Rita.
Using SEER Stat statistical software (version 8.2.1; National Cancer Institute), we examined colorectal cancer incidence based on the World Health Organization's (WHO) International Classification of Diseases for oncology, third edition (ICD-O-3) which defines colorectal cancer as cancer which encompasses the cecum, appendix, ascending colon, hepatic flexure, transverse colon, splenic flexure, descending colon, sigmoid colon, large intestine, Not otherwise Specified (NOS), rectosigmoid junction, and rectum[14].
Age-adjusted rates stratified by race and year of diagnosis as well as stage of disease according to the American Joint Committee on Cancer (AJCC) 6th edition guidelines, were also examined[15]. We applied American Joint Committee on Cancer 6th edition guidelines for all years, as 7th edition guidelines took effect in 2010. When calculating stage, we combined individuals with not applicable and blank variables into one Blank grouping. This grouping represented individuals with cancer histologies not defined by the AJCC [16]. Moreover, those individuals with stage unknown, cases for which sufficient evidence was not available to assign a stage, remained in a separate grouping[16]. We conducted a Poisson Regression with robust variance estimator to find the incidence ratio of API and NHW compared to African Americans as well as incidence ratio for each year. Since it has been shown that African Americans develop CRC at an earlier age than other racial/ethnic minorities reflecting a need to begin screening in this population group earlier[17], and the ACG has already recommended screening in AA beginning at 45[18], we left out the 45-49 age group when conducting our analysis, because we wanted to explore if CRC incidence was substantially different in the under 45 group as well. Therefore, racial groups were subdivided into five-year age categories: 20-24, 25-29, 30-34, 35-39, and 40-44.
Results
Age-Adjusted CRC Rate by Race
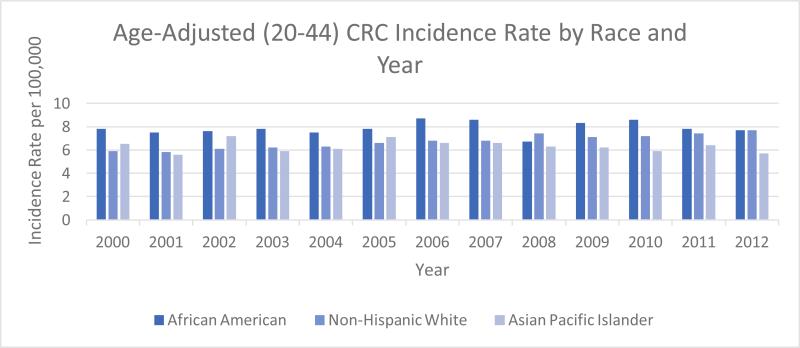
From 2000-2012, approximately 18,543 cases of CRC were diagnosed among young NHW, 3,581 among young African Americans, and 2,396 among young API aged 20-44. Based on the SEER-18 registry data[14], CRC incidence for all ages (20-44) was mostly higher for African Americans compared to Non-Hispanic Whites and APIs across all years 2000-2012[Figure 1]. From 2000-2012, African Americans had CRC incidence rates which averaged 7.9 per 100,000 compared to Non-Hispanic Whites at 6.7 per 100,000 and Asian Pacific Islanders at 6.3 per 100,000
Figure 1.
Age-Adjusted CRC Rate by Race and year in different populations. Differences in age-adjusted CRC incidence rate (2000 US Standard Population) among young African Americans, Non-Hispanic Whites, and Asian Pacific Islanders for the years 2000-2012.
CRC Rate by Year in young African Americans
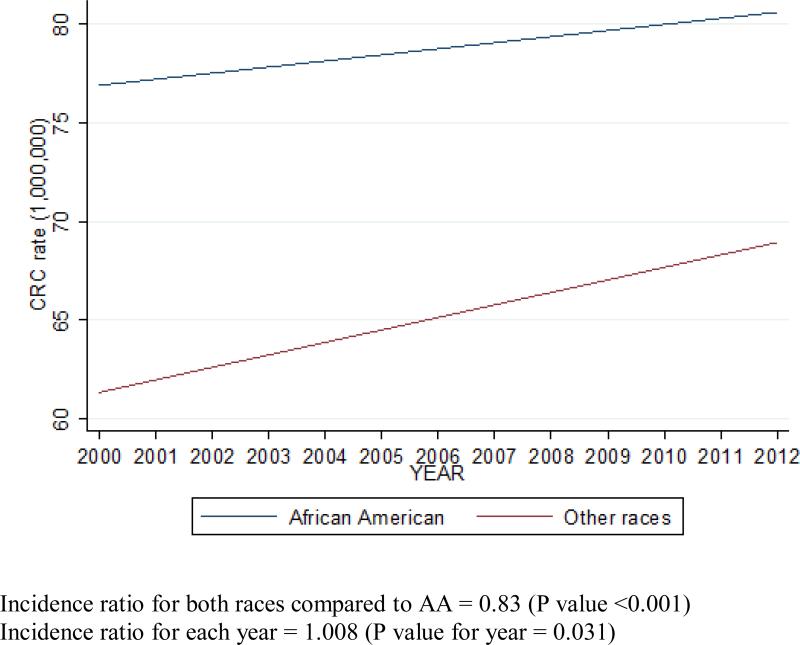
Using Poisson regression, the age-adjusted CRC rate was higher in African Americans (P<0.001) compared to other races under study throughout the period of analysis (P=0.031) [Figure 2]. The year of study is a continuous variable in the Poisson regression. An incidence ratio for this variable means the change of incidence per unit (one year). Each decimal after the 1 means a percentage increase in incidence by year, e.g. 0.008 means an average 0.8 increase in incidence in one year. Numerically it means that 12 years (2000-2012) there is a 9 (=0.8*12)/1,000,000 increase in incidence.
Figure 2.
Colorectal Cancer Rates in young adults (20-44 years) for Years 2000-2012
Stage of CRC by Race in Young African Americans
When stratified by age, we found that stage IV CRC is higher in African Americans compared to non-Hispanic Whites and API, while APIs have a higher stage III disease compared to non-Hispanic whites and African Americans [Table 1]. Stage 0, representing carcinoma in-situ had the lowest percentage of individuals across all racial groups. All staging were based on the AJCC 6th edition guidelines.
Table 1.
Colorectal Cancer Stage by Race for Years 2000-2012 n (%)
| Stage (ajcc 6th Edition) | African American (AA) | Asian-Pacific Islander (AP) | Non-Hispanic White (NHW) | Total |
|---|---|---|---|---|
| 0 | 51 (1.42) | 40 (1.67) | 337 (1.82) | 428 (1.75) |
| I | 337 (9.41) | 201 (8.39) | 1949 (10.51) | 2487 (10.14) |
| II | 433 (12.09) | 329 (13.73) | 2483 (13.39) | 3245 (13.23) |
| III | 624 (17.43) | 527 (22.00) | 3785 (20.41) | 4936 (20.13) |
| IV | 654 (18.26) | 423 (17.65) | 3058 (16.49) | 4135 (16.87) |
| Unknown | 111 (3.10) | 66 (2.75) | 522 (2.82) | 699 (2.85) |
| Blank | 1371(38.29) | 810 (33.81) | 6409 (34.56) | 8590(35.03) |
| Total | 3581 (100.0) | 2396 (100.0) | 18543 (100.0) | 24520 (100.0) |
Pearson Chi2(8)=35.4137 Pr≤0.001
Post hoc analysis indicates that the main differences are between NHW and AA in frequency of advanced stage (P = 0.001).
Discussion
According to recent studies conducted within the past decade, it has been found that there is an apparent increase in colorectal cancer among young individuals under the age of 50[2,3,5-7]. Since it is known that African Americans over the age of 50 have the highest overall incidence, highest incidence of advanced stage at disease presentation and highest attributable mortality, we explored whether this finding was applicable to young African Americans as well [12]. We aimed to evaluate whether there is an increased incidence of colorectal cancer among young African American population who are 20-44 years old.
Among the published data comparing racial/ethnic groups under 50 and incidence of colorectal cancer, we found that information was far from uniform. Some studies reported stable or no difference in age-specific incidence rates for African Americans compared to other groups [3,4,12]. Two of these studies, while examining SEER cancer registry data, similar to our present study, found age-specific incidence of CRC for young African Americans to be stable over the period of analysis, however, these rates were not significant [3,12]. Whereas, other studies analyzing the National Cancer Database (NCDB) reported increased incidence in non-white racial/ethnic groups compared to whites. These studies, however did not identify the specific racial/ethnic groups under study nor provide specific incidence rates, preventing adequate comparison [6,19]. In contrast, a few studies have specifically noted a higher incidence in CRC for African Americans under 50, however, these studies did not make any recommendations for addressing the implications of an increased incidence in this group [7,20-22].
Based on our analysis of the SEER-18 Registry for 2000-2012, we found that African Americans have in fact the highest incidence of CRC in the 20-44 year age groups. While Paquette et al. (2015) examined SEER database information from 2000-2011 and found that differences in incidence between Whites and African Americans are significant starting at age 45; the authors also noted that the age-specific incidence of colorectal cancer was 0.3 in whites and 0.4 in African Americans at 20 years of age[22]. This is consistent with our finding, that although the apparent differences in incidence are small in the young-onset group, African Americans begin to show higher increases in incidence at an earlier age. Moreover, although these incidence rates are relatively low compared to those in adults over the age of 50, this age – related disparity in the under 50 group is expected to increase further in the future with projections of newly diagnosed colon and rectal cancers expected to nearly double by 2030 [2,8]. Our investigation suggests an increased incidence of colorectal cancer in young 20-44 African Americans and lowest rates in young 20-44 APIs. Currently there are no screening options available for patients younger than 50 and most diagnoses depend on symptomatic presentation[8]. It is important to understand the root cause of CRC disparity among young people because of inherent differences in environmental and behavioral factors among different racial groups.
According to our evaluation of SEER data, African Americans, aged 20-44, had an average incidence rate of 7.9/100,000. In comparison, a 2013 study in Mortality and Morbidity Weekly (MMWR) which examined CRC incidence data in 2008, reported an incidence rate of 6.7/100,000 for all individuals younger than 50 [23]. African American incidence rates are important to understand in the young population because as a group, African Americans have a lower 5-year survival from cancer overall compared to whites in the United States. Moreover, with regards to colorectal cancer both African American men and women have higher rates of the disease compared to whites [10,24]. Since African Americans have the highest death rates and shortest survival of racial and/or ethnic groups, screening within this group is especially significant [25]. Recommendations to reduce the age to 45 for African Americans to begin screening compared with other racial/ethnic groups have already been advocated [18,24]. Despite the call for reduction in age for initiation of screening, only 56% of African Americans 50 and older were up to date on guideline-recommended screening compared to 62% of Whites[10]. Moreover, even when there is a finding of abnormality on different screening modalities such as flexible sigmoidoscopy, African Americans have a lower rate of follow-up diagnostic evaluation, suggesting that screening recommendation alone will not be enough to eliminate racial disparities in CRC burden[24].
A recent study, conducted by Wallace et al. (2016), comparing the prevalence of large bowel polyps among a poor and uninsured population found that a racial difference persists with African Americans having a higher prevalence of large bowel polyps and emphasizes the special attention needed for young African American adults to counter the observed trend[21]. While the present attention to adults >50 screening policy seems to have decreased CRC prevalence in this age group, it is unlikely that universal screening for young African Americans is possible, as age-cutoffs are used to make screening financially and logistically viable and given the fact that incidence in the young is still relatively low compared to >50 age group, [8]. However, increased investigation into factors both environmental and behavioral which are responsible for this increase can and should be implemented to impede any additional increases in the future.
One limitation to our present study, is that when colorectal cancer stage was compared by race for our study period 2000-2012, African Americans had the greatest percentage of blank data entries. Blank entries are comprised of cases which were not applicable or not defined by the current AJCC guidelines or for which pathologic staging criteria were not met. This limited the certainty for comparison of the aggressiveness of CRC diagnosed among the study population. In conclusion, although the relative increase in colorectal cancer in the young is small compared to the >50 age group, it is still an issue which requires special attention, especially with regards to racial/ethnic minorities. Since universal screening is not feasible, it would be important for physicians encountering symptomatic average-risk young patients to have increased awareness of the possibility of CRC. Additionally, further studies comparing risk factors and genetics between African Americans with the highest rate of CRC and API population group with the lowest rate of CRC could have the potential to address some of the causes for disparate incidences.
Footnotes
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.American Cancer Society Colorectal Cancer Facts & Figures 2014-2016. 2014 Available at: http://www.cancer.org/acs/groups/content/documents/document/acspc-042280.pdf.
- 2.Bailey CE, Hu CY, You YN, et al. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975-2010. JAMA Surg. 2015;150:17–22. doi: 10.1001/jamasurg.2014.1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siegel RL, Jemal A, Ward EM. Increase in incidence of colorectal cancer among young men and women in the United States. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2009;18:1695–1698. doi: 10.1158/1055-9965.EPI-09-0186. [DOI] [PubMed] [Google Scholar]
- 4.Austin H, Henley SJ, King J, Richardson LC, Eheman C. Changes in colorectal cancer incidence rates in young and older adults in the United States: what does it tell us about screening. Cancer Causes Control. 2014;25:191–201. doi: 10.1007/s10552-013-0321-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O'Connell JB, Maggard MA, Liu JH, Etzioni DA, Livingston EH, Ko CY. Rates of colon and rectal cancers are increasing in young adults. The American surgeon. 2003;69:866–872. [PubMed] [Google Scholar]
- 6.You YN, Xing Y, Feig BW, Chang GJ, Cormier JN. Young-onset colorectal cancer: is it time to pay attention? Archives of internal medicine. 2012;172:287–289. doi: 10.1001/archinternmed.2011.602. [DOI] [PubMed] [Google Scholar]
- 7.Fairley TL, Cardinez CJ, Martin J, et al. Colorectal cancer in U.S. adults younger than 50 years of age, 1998-2001. Cancer. 2006;107:1153–1161. doi: 10.1002/cncr.22012. [DOI] [PubMed] [Google Scholar]
- 8.Amri R, Bordeianou LG, Berger DL. The conundrum of the young colon cancer patient. Surgery. 2015;158:1696–1703. doi: 10.1016/j.surg.2015.07.018. [DOI] [PubMed] [Google Scholar]
- 9.Singh KE, Taylor TH, Pan CJG, Stamos MJ, Zell JA. Colorectal Cancer Incidence Among Young Adults in California. Journal of Adolescent and Young Adult Oncology. 2014;3:176–184. doi: 10.1089/jayao.2014.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Cancer Society [12/10/15];Cancer Facts & Figures for African Americans 2013-2014. 2013 Available at: http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036921.pdf. 2015.
- 11.Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin. 2014;64:104–117. doi: 10.3322/caac.21220. [DOI] [PubMed] [Google Scholar]
- 12.Rahman R, Schmaltz C, Jackson CS, Simoes EJ, Jackson-Thompson J, Ibdah JA. Increased risk for colorectal cancer under age 50 in racial and ethnic minorities living in the United States. Cancer Med. 2015 doi: 10.1002/cam4.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carethers JM. Screening for colorectal cancer in African Americans: determinants and rationale for an earlier age to commence screening. Dig Dis Sci. 2015;60:711–721. doi: 10.1007/s10620-014-3443-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.SEER*Stat Database: Incidence-SEER 18 Regs Research Data + Hurricane Katrina Impacted Louisana Cases. 2014 Nov; Available at: www.seer.cancer.gov.
- 15.Greene FL, Page DL, Fleming ID, et al., editors. AJCC Cancer Staging Manual. Springer; City: 2002. [Google Scholar]
- 16.Gress DM. Explaining Blanks and X, Ambiguous Terminology and Support for AJCC Staging. American Joint Committee on Cancer; City: 2014. [Google Scholar]
- 17.Ashktorab H, Paydar M, Namin HH, et al. Prevalence of colorectal neoplasia among young African Americans and Hispanic Americans. Dig Dis Sci. 2014;59:446–450. doi: 10.1007/s10620-013-2898-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, Inadomi JM. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected] Am J Gastroenterol. 2009;104:739–750. doi: 10.1038/ajg.2009.104. [DOI] [PubMed] [Google Scholar]
- 19.Ahnen DJ, Wade SW, Jones WF, et al. The increasing incidence of young-onset colorectal cancer: a call to action. Mayo Clin Proc. 2014;89:216–224. doi: 10.1016/j.mayocp.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 20.Gupta S, Shah J, Balasubramanian BA. Strategies for reducing colorectal cancer among blacks. Archives of internal medicine. 2012;172:182–184. doi: 10.1001/archinternmed.2011.594. [DOI] [PubMed] [Google Scholar]
- 21.Wallace K, Brandt HM, Bearden JD, et al. Race and Prevalence of Large Bowel Polyps Among the Low-Income and Uninsured in South Carolina. Dig Dis Sci. 2016;61:265–272. doi: 10.1007/s10620-015-3862-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paquette IM, Ying J, Shah SA, Abbott DE, Ho SM. African Americans should be screened at an earlier age for colorectal cancer. Gastrointest Endosc. 2015;82:878–883. doi: 10.1016/j.gie.2015.03.1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steele CB, Rim SH, Joseph DA, King JB, Seeff LC. Colorectal cancer incidence and screening - United States, 2008 and 2010. MMWR Surveill Summ. 2013;62(Suppl 3):53–60. [PubMed] [Google Scholar]
- 24.Laiyemo AO, Doubeni C, Pinsky PF, et al. Race and colorectal cancer disparities: health-care utilization vs different cancer susceptibilities. Journal of the National Cancer Institute. 2010;102:538–546. doi: 10.1093/jnci/djq068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DeSantis C, Naishadham D, Jemal A. Cancer statistics for African Americans, 2013. CA Cancer J Clin. 2013;63:151–166. doi: 10.3322/caac.21173. [DOI] [PubMed] [Google Scholar]