Abstract
Purpose
Determine the relationship between balance impairments and the ability to increase walking speed (WS) on demand in individuals with chronic stroke.
Methods
WS and Berg Balance Scale (BBS) data were collected on 124 individuals with chronic stroke (>6 months). The ability to increase WS on demand (walking speed reserve, WSR) was quantified as the difference between participants’ self-selected (SSWS) and maximal (MWS) walking speeds. Correlation, regression and receiver operating characteristic (ROC) analyses were performed to investigate the relationship between balance and the ability to increase WS.
Results
Of sample, 58.9% were unable to increase WS on demand (WSR < 0.2 m/s). BBS scores were associated with WSR values (rs=0.74, 0.65–0.81) and were predictive of ‘able/unable’ to increase WS [odds ratio (OR)=0.75, 0.67–0.84]. The AUC for the ROC curve constructed to assess the accuracy of BBS to discriminate between able/unable to increase WS was 0.85 (0.78–0.92). A BBS cutscore of 47 points was identified [sensitivity: 72.6%, specificity: 90.2%,+ likelihood ratio (LR): 7.41, − LR: 0.30].
Conclusions
The inability to increase WS on demand is common in individuals with chronic stroke, and balance appears to be a significant contributor to this difficulty. A BBS cutscore of 47 points can identify individuals who may benefit from balance interventions to improve the ability to increase their WS.
Keywords: Ambulation, balance, cerebrovascular accident, difficulty walking, gait, outcome measures, postural
Introduction
Difficulty walking often persists into the chronic phase of stroke,[1] with gait-related impairments [2–5] resulting in reduced (WS).[2,6] Although self-selected walking speeds (SSWS) in this population are typically slow, of particular concern is that many individuals exhibit an inability to “increase” speed while walking.[6–8] This inability implies that the individual typically walks at, or close to, their maximal speed and lacks the capacity to increase their WS in response to environmental demands. Walking can be a vulnerable activity for individuals with stroke, as a majority of falls occur while walking.[9–11] Perhaps, it is the individuals who are already walking “at capacity” that are at greatest risk for falls. By assessing an individual’s ability to increase their WS, we can identify those individuals who are walking at their capacity, without a reserve to draw on if necessary.
The ability to increase WS on demand can be quantified clinically by determining the difference between an individual’s SSWS and their maximal walking speed (MWS). Termed “walking speed reserve” (WSR), this value represents the speed increase an individual has available to utilize when needed. Determining why some individuals can increase their WS while others cannot, will help inform interventions targeting this ability.
Although lower extremity strength has been associated with both SSWS and MWS,[12,13] this relationship does not appear to extend to an individual’s WSR.[14] However, slower walkers are less able to increase their speed on demand [6] and also demonstrate reduced balance compared to faster walkers.[1] This suggests that individuals post-stroke may be unable to access their “reserve” due to diminished balance. Specifically, the Berg Balance Scale (BBS) has been related to the ability to increase WS in higher functioning individuals post-stroke who walked without an assistive device.[14] Exclusion of individuals who use an assistive device represents a notable limitation given that up to 43% of this population relies on an assistive device for mobility.[15,16]
The primary objective of this study was to determine the relationship between balance impairments and the ability to increase WS (WSR) in individuals with chronic stroke across a wide range of functional abilities. We hypothesized that individuals with more impaired balance would exhibit greater deficits in WSR. A secondary objective was to identify a BBS cutscore that could be used to distinguish individuals with chronic stroke with low WSR due to balance impairments from those with low WSR due to other factors. This finding will help guide clinical practice by indicating potential targets for intervention.
Methods
A cross-sectional design was used to address the stated aims of the study. All participants reviewed and signed an informed consent form approved by the University of South Carolina or University of North Carolina at Chapel Hill’s Institutional Review Board prior to participation.
Participants
Community-dwelling individuals with chronic stroke undergoing baseline testing for ongoing clinical trials at two University sites were included in the present study. To be eligible for this study, participants had to be ≥18 years of age, >6 months post-stroke, able to understand testing instructions and correctly carry them out, and able to walk 10 m with or without an assistive device. Participants were excluded if they had severe weight-bearing pain, severe visual impairment, other neurological conditions such as Parkinson’s disease, and/or severe cardiovascular or musculoskeletal problems that limited ability to ambulate. A formal power analysis was not performed, rather all participants meeting study criteria were included. Assessments were performed by individuals trained on standardized protocols for the following selected measures.
Selected measures
Walking speed
Walking speed was assessed in all participants via either a 3 Meter Walk Test (3MWT) or using a 4.27m GAITRite mat (CIR Systems, Havertown, PA). The assessment method utilized was based on testing site. For assessment of SSWS, participants were instructed to walk at their “usual, comfortable speed”. For MWS, the instructions were to walk as “quickly, but safely as possible”. The three trials under each condition were then averaged to determine SSWS and MWS (m/s), respectively. Assistive devices and/or orthoses typically used during community ambulation were permitted during testing, but participants did not receive physical assistance during gait.
3 Meter Walk Test
The 3MWT is a reliable method for assessing WS in individuals with chronic stroke.[17] A handheld stopwatch was used to time participants over a three meter path. Timing started when the participant’s lead leg broke the plane of the marker at the beginning of the path and stopped when their lead leg broke the plane of the marker at the end of the three meter path. Two meters were provided prior to and following the timed portion to allow acceleration and deceleration to occur outside of the timed segment and ensure that steady-state SSWS and MWS were captured for analysis.[18,19]
GAITRite
The GAITRite mat is a portable gait analysis system that can be used to reliably assess the WS of individuals with chronic stroke.[17] The active portion of the mat (width: 61 cm, length: 4.27 m) is embedded with 16 128 pressure sensors. For WS data collection, the sensors were set to sample data at 60 Hz. Participants were provided ~1.5 m prior to and following the GAITRite mat to allow for acceleration and deceleration and ensure that steady-state WSs were captured for analysis. SSWS and MWS were automatically computed for each trial by the associated GAITRite software.[20]
WSR was calculated as the difference between the individual’s MWS and SSWS (WSR=MWS – SSWS). As with WS, WSR is reported in meters per second.
Balance
Berg Balance Scale
The BBS is a valid, reliable measure for assessing balance in individuals with stroke.[21] The measure consists of 14 items scored on a 0–4 scale, making 56 the maximal score. Higher scores are indicative of better balance. The measure assesses both static (e.g. standing eyes open/eyes closed) and dynamic (e.g. foot taps on a step) balance and includes functional activities (e.g. transfers).[22] The use of assistive devices was not permitted during performance of the BBS.
Data analysis
Descriptive statistics (mean or median, standard deviation, range, percentages) were calculated on all collected variables to characterize the sample. Distributions were assessed for normality using Shapiro–Wilk tests. Both WSR and BBS exhibited non-normal distributions and underwent a square root and reflected square root transformation, respectively. To determine the strength of the association between balance impairments and the ability to increase WS, a Spearman’s correlation coefficient was calculated for the relationship between BBS scores and WSR values. Given the well-known association between age and gait speed, we assessed the association between age and WSR using a Pearson’s correlation. If age was found to be significantly correlated with WSR, age would be entered as a covariate in regression analyses.
To further examine the relationship between balance and the ability to increase WS, logistic regression was performed with BBS scores as the independent variable and “able/unable to increase WS” as the dichotomous dependent variable. Those with WSRs ≥0.2 m/s were classified as “able to increase WS”, and those with WSRs <0.2 m/s were classified as “unable to increase WS”. The 0.2 m/s threshold was selected to correspond with the minimal detectable change (MDC) value for SSWS in individuals with chronic stroke.[20] Descriptive statistics were calculated for each subgroup (able/unable to increase WS) and between-group comparisons were performed using independent sample t-tests, Mann–Whitney U-tests or chi-squared (χ2) tests, as appropriate. Alpha was set at 0.05 for all significance testing.
To assess the accuracy of using BBS scores to discriminate between those who were able and unable to increase WS, a receiver operating characteristic (ROC) curve was constructed. The area under the curve (AUC) was calculated to represent the accuracy of the test at discriminating between “positive” (WSR≥0.2 m/s) and “negative” (WSR < 0.2 m/s) test results. An AUC of 1.0 corresponds to perfect discrimination, while an AUC of 0.5 indicates the test is not better than chance at discriminating between those who are able/unable to increase WS. The ROC curve constructed was also used to identify a BBS cutscore that best discriminated (maximized combined sensitivity and specificity) between those who were able/unable to increase WS. Using the sensitivity and specificity for the identified cutscore, positive and negative likelihood ratios [+ LR=sensitivity/(1− specificity), − LR=(1−sensitivty)/specificity] were calculated. The LRs provide information on the clinical utility of using the identified BBS cut-score to identify those who are unable to increase WS. LRs can be interpreted as follows:+ LRs > 10 and –LRs < 0.1 result in shifts in probability that are “large and conclusive”,+ LRs between 5 and 10 and –LRs between 0.1 and 0.2 result in “moderate” shifts, + LRs from 2 to 5 and− LRs from 0.5 to 0.2 result in “small” shifts, and + LRs from 1 to 2 and − LRs from 0.5 to 1 result in shifts that are “rarely important”.[23] All data analyses were performed using IBM® SPSS 22, Armonk, NY.
Results
Participants
Sample characteristics (n=124) are presented in Table 1. WSs were assessed in 68 participants via the 3MWT and 56 participants using the GAITRite mat.
Table 1.
Sample characteristics (n = 124).
| Sample characteristics | |
|---|---|
| Age in years | 62.97 (SD: 12.04) |
| Years post-stroke | 4.62 (0.50, 22.68) |
| Femalea | 49 (39.52) |
| Assistive devicea | |
| Cane | 49 (39.52) |
| Hemi-walker | 1 (0.81) |
| Walker | 6 (4.84) |
| BBS (points) | 47 (13, 56) |
| SSWS | 0.49 (0.04, 1.16) |
| MWS | 0.70 (0.05, 1.59) |
| WSR (m/s) | 0.16 (0.00, 0.64) |
Years post-stroke, BBS, SSWS, MWS and WSR not normally distributed. Median and range presented.
Female and assistive device data presented as (n, %).
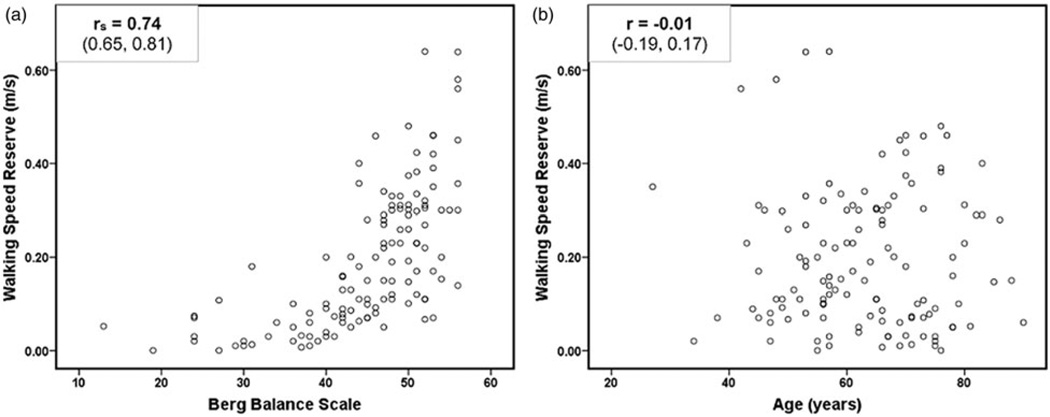
Correlation
BBS scores were significantly and positively associated with WSR values [r=0.74, 95% confidence interval (CI): 0.65, 0.81]. Age was not associated with WSR values (r=−0.01, 95% CI: −0.19, 0.17). Relationships between BBS and WSR and between age and WSR are depicted in Figure 1.
Figure 1.
Scatter plots depicting relationship between (a) BBS scores and WSR (rs=Spearman’s correlation coefficient and associated 95% CI) (b) age and WSR (r=Pearson’s correlation coefficient and associated 95% CI).
Logistic regression
Fifty-one participants were able to increase their WS and 73 were unable (WSR above/below 0.2 m/s, respectively). The two groups demonstrated similar demographic characteristics (age, sex, time post-stroke), but differed on all functional measures (BBS, SSWS, MWS, WSR). Refer to Table 2 for able/unable group characteristics. BBS scores were a significant predictor of being able/unable to increase WS. As BBS scores increased, a participant’s risk of being unable to increase their WS decreased [odds ratio (OR)=0.75; 95% CI: 0.67, 0.84; p < 0.001]. Age was not significantly associated with WSR and was not entered as a covariate in logistic regression.
Table 2.
Group characteristics for able and unable to increase WS.
| Group characteristics | Able to increase WS | Unable to increase WS | p Valuesb |
|---|---|---|---|
| n (%) | 51 (41.1) | 73 (58.9) | |
| Age in years | 63.53 (SD: 12.17) | 62.59 (SD: 12.00) | 0.53 |
| Years post-stroke | 5.17 (0.50, 15.00) | 4.00 (0.50, 22.67) | 0.08 |
| Femalea | 17 (33.3) | 32 (43.8) | 0.24 |
| Assistive devicea | |||
| None | 46 (90.2) | 22 (30.1) | <0.001 |
| Cane | 3 (5.9) | 46 (63.0) | <0.001 |
| Hemi-walker | 0 (0.0) | 1 (1.4) | 0.40 |
| Walker | 2 (3.9) | 4 (5.5) | 0.69 |
| BBS (points) | 50 (43, 56) | 42 (13, 56) | <0.001 |
| SSWS | 0.68 (0.26, 1.11) | 0.36 (0.04, 1.16) | <0.001 |
| MWS | 1.02 (0.46, 1.59) | 0.46 (0.05, 1.30) | <0.001 |
| WSR (m/s) | 0.31 (0.20, 0.64) | 0.08 (0.00, 0.19) | <0.001 |
Years post-stroke, BBS scores, SSWS, MWS and WSR not normally distributed in one or both groups, so median and range presented.
Female and assistive device data presented as (n, %).
p values presented are for the Mann–Whitney U-test or chi-squared (χ2) between-group comparisons.
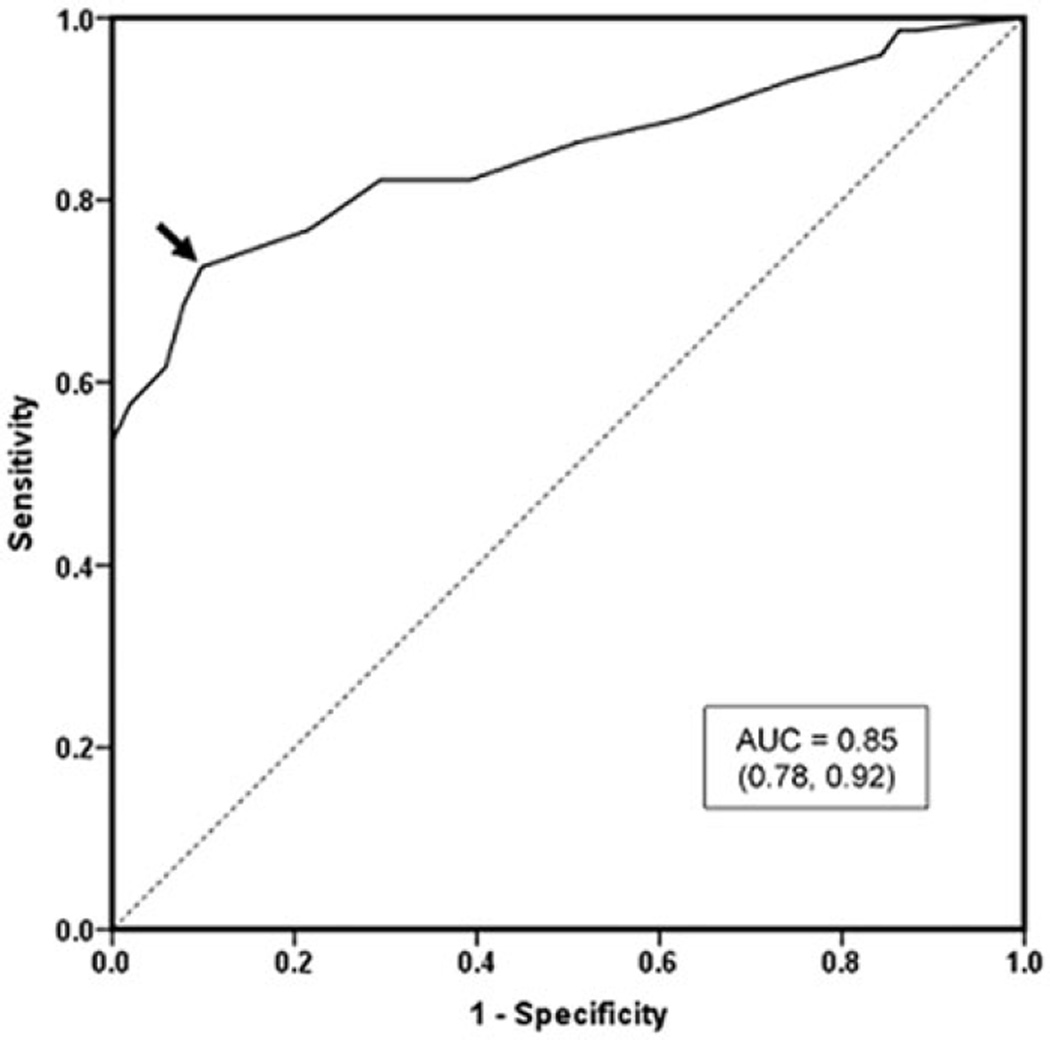
ROC curve analysis
The AUC for the ROC curve (Figure 2) constructed to assess the accuracy of BBS scores to discriminate between those who were able/unable to increase WS was 0.85 (95% CI: 0.78, 0.92). The BBS cutscore identified on the curve that maximized combined sensitivity (72.6%) and specificity (90.2%) was 47 points. The + LR associated with this cutscore is 7.41 and the− LR is 0.30.
Figure 2.
ROC curve for predicting inability to increase WS (WSR < 0.2 m/s) based on BBS scores. Values presented in parentheses is 95% CI for AUC. Arrow corresponds to BBS Score (47 points) which maximized sensitivity (72.6%) and specificity (90.2%).
Discussion
The ability to increase WS on demand is important for successful, safe and adaptable community ambulation. Individuals walking “at capacity” lack the speed reserves needed to respond to environmental demands. We observed that a majority of our participants (59%) were unable to increase their WS and were walking at capacity; highlighting the prevalence of the problem among individuals with chronic stroke. Before interventions can be implemented to address this functional limitation, the impairments contributing to the inability to increase WS must be determined. Our results suggest that impaired balance, as measured with the BBS, contributes to the inability to increase WS on-demand.
As a commonly used, psychometrically sound outcome measure for assessing balance in individuals with stroke, the BBS has been well-studied.[21] A variety of cutscores are available in the literature, allowing clinicians to identify “at-risk” clients. Fall risk cutscores range from 31 [24] to 50 [25] for discriminating between fallers and non-fallers, and 42 [26] to 52 [11] for identification of “multiple fallers” or “injurious falls” among individuals with stroke. Given the balance requirements for maintaining stability, the relationship between BBS scores and fall risk is not surprising; however, BBS scores also appear to provide insight into walking ability in individuals with stroke.
BBS scores are related to SSWS,[1] MWS,[27] and community ambulatory activity [28] and are predictive of walking outcomes in this population. For example, an individual receiving inpatient rehabilitation for stroke’s admission BBS score combined with their FIM walk item score can be used to predict whether they will be a community ambulator at discharge.[29] Admission BBS scores are also predictive of independence with walking at 3 months in this population.[30] Patterson et al. [1], found BBS score to be a significant predictor of both WS and endurance in individuals with chronic stroke who had moderate to severe impairments (SSWS ≤ 0.48 m/s). Our findings indicate that in addition to the previously published cutscores, a score of <47 points on the BBS may identify clients with chronic stroke who have difficulty increasing WS secondary to impaired balance. If balance impairments are identified as a contributor (i.e. client scores <47 on BBS), appropriate treatment activities targeting balance can be implemented. Importantly, it appears that addressing balance deficits may improve the ability to increase WS on demand.
Addressing balance impairments in order to improve gait is not a novel concept; balance plays an important role in gait. Due to the nature of bipedal locomotion, a majority of the gait cycle is spent in single limb support. During these phases, the center of mass travels outside of the base of support, making it inherently unstable.[31] Accordingly, evidence supports the role of balance in gait rehabilitation for individuals with stroke.[32] Improvements in balance coincide with improvements in gait-related outcomes, [33,34] and baseline balance may provide insight into who will improve SSWS following intervention in this population, as well.[35] Our findings emphasize the importance of balance in gait rehabilitation, especially when the gait-related target of intervention is the ability to increase WS. In order for individuals to maximize their ability to functionally ambulate in the community, they need to have the capacity to speed up in response to environmental demands. Woollacott et al. [31] list four criteria for “successful” ambulation, one of which is “adaptability to meet any changes in the environment or other concurrent tasks”. For individuals with chronic stroke, balance impairments may limit this ability.
Assistive device use appeared to have a role in our participant’s ability to increase WS. Specifically, we noted that individuals with an inability to increase WS tended to use assistive devices, whereas those able to increase WS did not tend to use an assistive device. Although the use of an assistive device will increase an individual’s base of support, these participants were still unable to increase gait speed. This suggests that either the assistive device didn’t provide them with sufficient balance control to increase WS, or there were additional underlying impairments that prohibited them from increasing WS. Although BBS scores were associated with WSR values among those who used an assistive device and those who did not, the association appears stronger for those who used a device (Spearman’s r=0.39 for no assistive device and 0.65 for assistive device, p < 0.001). Lee et al. [14] previously reported an association between balance impairments and the ability to increase WS in individuals with chronic stroke who did not require an assistive device. Our findings expand on that work by demonstrating that this relationship exists, and may actually be stronger, in those who require an assistive device for ambulation.
The BBS threshold for identifying individuals with chronic stroke who were unable to increase their WS on demand was higher than the 42 point fall risk cutscore that emerged from the Locomotor Experience Applied Post-Stroke (LEAPS) trial.[26] The LEAPS cutscore was selected for comparison because it was prospectively derived from a large sample. The threshold for identifying individuals who do not have the capacity to increase WS is higher than the threshold for fall risk, indicating that among individuals with stroke, balance impairments do not have to reach the severity of “fall risk” before functional ambulation is affected. Interventions to improve balance may need to be initiated at this higher threshold, if the individual demonstrates an inability to increase WS. Perhaps by intervening “earlier” (before balance impairments reach a severity of < 42 points on the BBS), safety during functional ambulation can be increased and risk of falls while walking can be decreased. A majority of falls in individuals with stroke occur while walking,[9–11] so safety during this task is a priority. Determining if an inability to increase WS on demand is associated with risk for falls while walking is an area for future research.
Limitations
Two methods of collecting WS data were utilized, the 3MWT and the GAITRite portable gait analysis system. Both are highly reliable methods of assessing WS in individuals with chronic stroke [17] and timed distance varies by only 1.27 m. While consistency in protocol would have been preferable, the outcome of interest was WSR. This value was calculated using SSWS and MWS collected by reliable methods; therefore, the difference score should be minimally affected. Additionally, all WS data was collected in clinical laboratory settings by staff trained on standardized procedures, further improving the reliability of the protocols used.
The purpose of the study was to determine the role balance plays in the ability to increase WS in individuals with chronic stroke. By limiting our analyses to balance, our findings do not provide insight into other potential contributors. Increasing speed while walking is a complex task, and it is likely that other factors, such as strength, endurance and tone, also play a role. This is supported by the fact that BBS scores as high as 56 points were observed among participants classified as “unable to increase WS”. Balance impairments are not likely limiting the ability to increase WS in this subgroup of participants with high BBS scores and low WSR values. Determining the relative importance of other factors contributing to the inability to increase WS will allow for more comprehensive intervention strategies and should be a focus of future research. Another limitation was the use of 0.2 m/s to dichotomize the sample into those able and unable to increase WS. The value was selected as it represents the minimal increase in WS required to ensure that “true change” has occurred in this population.[20] Although this is an evidence-based cutscore, it does not perfectly discriminate between those who are able and unable to increase WS within our sample. Finally, the potential role of comorbidities, such as arthritis, which may impact both BBS scores and the ability to increase WS was not considered in the current analyses.
Conclusions
Some individuals with chronic stroke are already walking “at capacity” in the community and, as a result, are unable to increase their WS in response to environmental demands. The inability to increase WS on demand may limit these individuals’ ability to be functional ambulators in the community. Balance is a significant contributor to the ability to increase WS in individuals with chronic stroke. A BBS cutscore of 47 points can be used to identify clients walking “at capacity” due to balance impairments. Future research will be need to determine if addressing these balance impairments via appropriately targeted interventions can lead to a greater WSR.
IMPLICATIONS FOR REHABILITATION.
A majority of individuals with chronic stroke may be unable to increase their walking speed beyond their self-selected speed on demand.
This may limit functional ambulation, as these individuals are walking “at capacity”.
Balance impairments contribute to the inability to increase walking speed.
A Berg Balance Scale score <47 points can be used to identify individuals with chronic stroke walking “at capacity” due to balance impairments.
Acknowledgments
Funding information
This work was partially funded by NIH [Grant Nos T32GM081740 (Middleton) and R21-HD068805 (Lewek)], AHA [Grant Nos 09BGIA2210015 (Lewek) and 0835160N (Scientist Development Grant, Fritz)] and a grant from Health Games Research, a national program of the Robert Wood Johnson Foundation [Grant No. 64450 (Fritz)].
Footnotes
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- 1.Patterson SL, Forrester LW, Rodgers MM, et al. Determinants of walking function after stroke: differences by deficit severity. Arch Phys Med Rehabil. 2007;88:115–119. doi: 10.1016/j.apmr.2006.10.025. [DOI] [PubMed] [Google Scholar]
- 2.Patterson KK, Gage WH, Brooks D, et al. Changes in gait symmetry and velocity after stroke: a cross-sectional study from weeks to years after stroke. Neurorehabil Neural Repair. 2010;24:783–790. doi: 10.1177/1545968310372091. [DOI] [PubMed] [Google Scholar]
- 3.Kautz SA, Duncan PW, Perera S, et al. Coordination of hemiparetic locomotion after stroke rehabilitation. Neurorehabil Neural Repair. 2005;19:250–258. doi: 10.1177/1545968305279279. [DOI] [PubMed] [Google Scholar]
- 4.Severinsen K, Jakobsen JK, Overgaard K, et al. Normalized muscle strength, aerobic capacity, and walking performance in chronic stroke: a population-based study on the potential for endurance and resistance training. Arch Phys Med Rehabil. 2011;92:1663–1668. doi: 10.1016/j.apmr.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 5.Chen G, Patten C, Kothari DH, et al. Gait differences between individuals with post-stroke hemiparesis and nondisabled controls at matched speeds. Gait Posture. 2005;22:51–56. doi: 10.1016/j.gaitpost.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 6.Bohannon RW. Walking after stroke: comfortable versus maximum safe speed. Int J Rehabil Res. 1992;15:246–248. [PubMed] [Google Scholar]
- 7.Jonkers I, Delp S, Patten C. Capacity to increase walking speed is limited by impaired hip and ankle power generation in lower functioning persons post-stroke. Gait Posture. 2009;29:129–137. doi: 10.1016/j.gaitpost.2008.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turnbull GI, Charteris J, Wall JC. A comparison of the range of walking speeds between normal and hemiplegic subjects. Scand J Rehabil Med. 1995;27:175–182. [PubMed] [Google Scholar]
- 9.Jorgensen L, Engstad T, Jacobsen BK. Higher incidence of falls in long-term stroke survivors than in population controls: depressive symptoms predict falls after stroke. Stroke. 2002;33:542–547. doi: 10.1161/hs0202.102375. [DOI] [PubMed] [Google Scholar]
- 10.Pinto EB, Nascimento C, Marinho C, et al. Risk factors associated with falls in adult patients after stroke living in the community: baseline data from a stroke cohort in Brazil. Top Stroke Rehabil. 2014;21:220–227. doi: 10.1310/tsr2103-220. [DOI] [PubMed] [Google Scholar]
- 11.Belgen B, Beninato M, Sullivan PE, et al. The association of balance capacity and falls self-efficacy with history of falling in community-dwelling people with chronic stroke. Arch Phys Med Rehabil. 2006;87:554–561. doi: 10.1016/j.apmr.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 12.Hsu AL, Tang PF, Jan MH. Analysis of impairments influencing gait velocity and asymmetry of hemiplegic patients after mild to moderate stroke. Arch Phys Med Rehabil. 2003;84:1185–1193. doi: 10.1016/s0003-9993(03)00030-3. [DOI] [PubMed] [Google Scholar]
- 13.Kim CM, Eng JJ. The relationship of lower-extremity muscle torque to locomotor performance in people with stroke. Phys Ther. 2003;83:49–57. [PubMed] [Google Scholar]
- 14.Lee KB, Lim SH, Ko EH, et al. Factors related to community ambulation in patients with chronic stroke. Top Stroke Rehabil. 2015;22:63–71. doi: 10.1179/1074935714Z.0000000001. [DOI] [PubMed] [Google Scholar]
- 15.Jutai J, Coulson S, Teasell R, et al. Mobility assistive device utilization in a prospective study of patients with first-ever stroke. Arch Phys Med Rehabil. 2007;88:1268–1275. doi: 10.1016/j.apmr.2007.06.773. [DOI] [PubMed] [Google Scholar]
- 16.Skolarus LE, Burke JF, Freedman VA. The role of accommodations in poststroke disability management. J Gerontol B Psychol Sci Soc Sci. 2014;69:S26–S34. doi: 10.1093/geronb/gbu117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peters DM, Middleton A, Donley JW, et al. Concurrent validity of walking speed values calculated via the GAITRite electronic walkway and 3 Meter Walk Test in the chronic stroke population. Physiother Theory Pract. 2014;30:183–188. doi: 10.3109/09593985.2013.845805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Graham JE, Ostir GV, Fisher SR, et al. Assessing walking speed in clinical research: a systematic review. J Eval Clin Pract. 2008;14:552–562. doi: 10.1111/j.1365-2753.2007.00917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lindemann U, Najafi B, Zijlstra W, et al. Distance to achieve steady state walking speed in frail elderly persons. Gait Posture. 2008;27:91–96. doi: 10.1016/j.gaitpost.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 20.Lewek MD, Randall EP. Reliability of spatiotemporal asymmetry during overground walking for individuals following chronic stroke. J Neurol Phys Ther. 2011;35:116–121. doi: 10.1097/NPT.0b013e318227fe70. [DOI] [PubMed] [Google Scholar]
- 21.Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther. 2008;88:559–566. doi: 10.2522/ptj.20070205. [DOI] [PubMed] [Google Scholar]
- 22.Berg KO, Wood-Dauphinee SL, Williams JI, et al. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83:S7–S11. [PubMed] [Google Scholar]
- 23.Jaeschke R, Guyatt GH, Sackett DL. Users’ guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The Evidence-Based Medicine Working Group. JAMA. 1994;271:703–707. doi: 10.1001/jama.271.9.703. [DOI] [PubMed] [Google Scholar]
- 24.Maeda N, Urabe Y, Murakami M, et al. Discriminant Analysis for predictor of falls in stroke patients by using the Berg Balance Scale. Singapore Med J. 2015;56:280–283. doi: 10.11622/smedj.2015033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tsang CS, Liao LR, Chung RC, et al. Psychometric properties of the Mini-Balance Evaluation Systems Test (Mini-BESTest) in community-dwelling individuals with chronic stroke. Phys Ther. 2013;93:1102–1115. doi: 10.2522/ptj.20120454. [DOI] [PubMed] [Google Scholar]
- 26.Tilson JK, Wu SS, Cen SY, et al. Characterizing and identifying risk for falls in the LEAPS study: a randomized clinical trial of interventions to improve walking poststroke. Stroke. 2012;43:446–452. doi: 10.1161/STROKEAHA.111.636258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lewek MD, Bradley CE, Wutzke CJ, et al. The relationship between spatiotemporal gait asymmetry and balance in individuals with chronic stroke. J Appl Biomech. 2014;30:31–36. doi: 10.1123/jab.2012-0208. [DOI] [PubMed] [Google Scholar]
- 28.Michael KM, Allen JK, Macko RF. Reduced ambulatory activity after stroke: the role of balance, gait, and cardiovascular fitness. Arch Phys Med Rehabil. 2005;86:1552–1556. doi: 10.1016/j.apmr.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 29.Bland MD, Sturmoski A, Whitson M, et al. Prediction of discharge walking ability from initial assessment in a stroke inpatient rehabilitation facility population. Arch Phys Med Rehabil. 2012;93:1441–1447. doi: 10.1016/j.apmr.2012.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Makizako H, Kabe N, Takano A, et al. Use of the Berg Balance Scale to predict independent gait after stroke: a study of an inpatient population in Japan. PMR. 2015;7:392–399. doi: 10.1016/j.pmrj.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 31.Woollacott MH, Tang PF. Balance control during walking in the older adult: research and its implications. Phys Ther. 1997;77:646–660. doi: 10.1093/ptj/77.6.646. [DOI] [PubMed] [Google Scholar]
- 32.Bowden MG, Embry AE, Gregory CM. Physical therapy adjuvants to promote optimization of walking recovery after stroke. Stroke Res Treat. 2011;2011:601416. doi: 10.4061/2011/601416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bowden MG, Behrman AL, Neptune RR, et al. Locomotor rehabilitation of individuals with chronic stroke: difference between responders and nonresponders. Arch Phys Med Rehabil. 2013;94:856–862. doi: 10.1016/j.apmr.2012.11.032. [DOI] [PubMed] [Google Scholar]
- 34.Duncan PW, Sullivan KJ, Behrman AL, et al. Body-weight-supported treadmill rehabilitation after stroke. N Engl J Med. 2011;364:2026–2036. doi: 10.1056/NEJMoa1010790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dobkin BH, Nadeau SE, Behrman AL, et al. Prediction of responders for outcome measures of locomotor Experience Applied Post Stroke trial. J Rehabil Res Dev. 2014;51:39–50. doi: 10.1682/JRRD.2013.04.0080. [DOI] [PMC free article] [PubMed] [Google Scholar]