Abstract
The anterior inferior iliac spine (AIIS) has variable morphology that correlates with hip range of motion. Subspinal impingement is an extracapsular cause for femoroacetabular impingement (FAI) and is clinically significant because it results in decreased range of motion and groin pain with flexion-based activity. In symptomatic patients with AIIS extension to or below the acetabular rim, AIIS decompression is considered part of an FAI corrective procedure. A consistent exposed bony area on the anterior and inferomedial aspect of the AIIS serves as a “safe zone” of resection allowing for decompression with preservation of the origin of the rectus femoris tendon. This surgical note describes a technique for AIIS decompression. The goal for low AIIS osteoplasty is to resect the AIIS to 2 burr widths (using a 5.5-mm burr) above the acetabular rim, achieving an 11-mm clearance, creating a type I AIIS. The resultant flat anterior acetabular surface between the most anteroinferior prominent point of the AIIS and the acetabular rim allows for free movement of the hip joint without impingement. Careful execution of AIIS decompression can alleviate clinical symptoms of FAI and restore function to the hip joint.
The anterior inferior iliac spine (AIIS) is an extracapsular bony prominence superior to the anterolateral acetabular rim. It comprises 2 facets (superior and inferior) separated by a ridge and serves as the origin of the extra-articular direct head of the rectus femoris, superior to the insertion of the joint capsule (the iliofemoral ligament) and iliocapsularis muscle.1 Computed tomography (CT) studies in asymptomatic patients have shown that the mean distances from the AIIS to the acetabular rim are 13.5 mm and 11.4 mm in male and female patients, respectively.2 Cadaver studies showed a distance of 19.2 mm between the rectus femoris footprint and the acetabular rim and 12.5 mm between the iliocapsularis and the rim.1 Subspinal impingement is a newly recognized etiology of extra-articular femoroacetabular impingement (FAI). This impingement is clinically significant as it results in decreased range of motion and hip pain.3 Table 1 describes hints for clinical diagnosis of low AIIS.
Table 1.
Hints for Clinical Diagnosis of Subspinal Impingement
| • Anterior groin pain |
| • Limitation in flexion and internal rotation |
| • Pain in strait hip flexion |
| • Limitations in range of motion |
| • Pain on palpation of the anterior inferior iliac spine |
| • Pain with prolonged sitting |
Hetsroni et al.4 described 3 morphological variants of the AIIS in CT scans. Each morphologic variant correlates with a specific range of motion in the hip joint.4 Clinical series have shown the efficacy of arthroscopic and open AIIS resection.4, 5 Low AIIS may be an underaddressed pathology because nonresected low AIIS has been found in up to 46% of revision hip arthroscopy surgeries.6
The possible causes of low AIIS include traction apophysitis or avulsion fractures, usually attributed to kicking sports. A consistent exposed bony area on the anterior and inferomedial aspect of the AIIS serves as a “safe zone” for decompression, allowing for preservation of the origin of the rectus femoris tendon.5 The goal for low AIIS osteoplasty is to resect the AIIS to 2 burr widths (using a 5.5-mm burr) above the acetabular rim, achieving an 11-mm clearance to treat low AIIS impingement, creating a type I AIIS.4
Surgical Technique
The surgical technique for low AIIS decompression is shown in Video 1.
Preoperative Planning
Groin pain and limitation in flexion and internal rotation are the most common manifestations of subspinal impingement. Larson et al.7 described diagnostic pearls consistent with AIIS impingement. These pearls include anterior groin pain, pain in straight hip flexion, and limitations in range of motion. The typical presentation of patients with subspinal impingement is anterior hip or groin pain aggravated by hip flexion; in addition, pain can be elicited by palpation of the AIIS on physical examination. The physical examination should be repeated with the patient on the operating table to illicit subspinal impingement.
Plain radiography may underestimate the prevalence of low AIIS.8 The small distance between the AIIS and the acetabular rim in types II and III AIIS may cause the AIIS to be superimposed on the iliac bone in an anterior posterior pelvic radiography, thus effectively hiding the AIIS. However, false profile radiographs may allow for the appreciation of low AIIS and the close relation to the acetabulum. CT scans and 3-dimensional reconstruction images can offer comprehensive assessment of pelvic anatomy and help to clarify the often-missed diagnosis of low AIIS (Figs 1 and 2). When considering pelvic CT imaging, exposure to radiation must be weighed against the added benefit of the films for diagnosis and surgical planning.
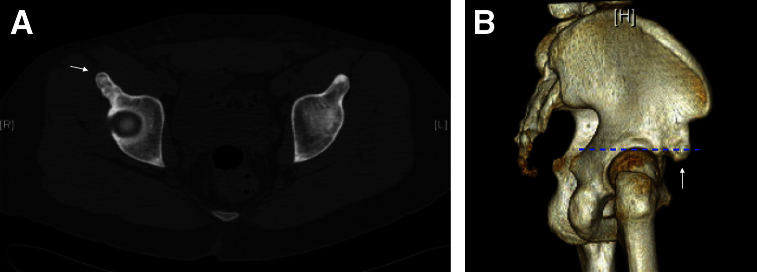
Fig 1.
(A) A transverse section computed tomography at the level of the anterior inferior iliac spine (AIIS). The computed tomography shows type III AIIS on the right side. The femoral head can be seen on the right side, showing that the AIIS is protruding at a level lower than the superior joint line. The AIIS is demarcated with an arrow. (B) A 3-dimensional reconstruction of the pelvis. The low AIIS can be seen crossing the joint line. The joint line is marked with a dashed line and the low AIIS is shown with an arrow.
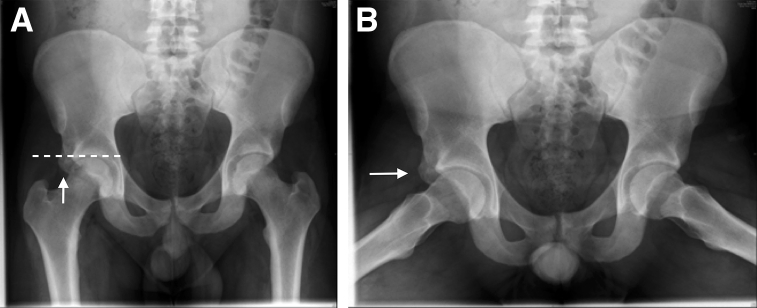
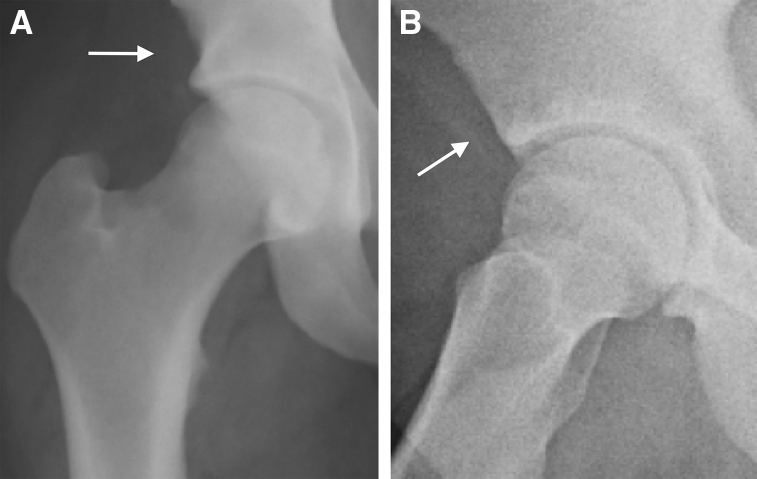
Fig 2.
(A) An anterior posterior pelvic radiograph of a 21-year-old patient with right-sided low anterior inferior iliac spine (AIIS). The low AIIS is shown with an arrow and can be seen protruding inferior to the joint line, which is shown with a dashed line. (B) The frog view image of the radiograph of the same patient. The low AIIS is shown with an arrow and can be seen articulating with the femoral neck. The right side of the radiograph should be compared with the nonpathologic left side.
Patient Positioning
The patient is positioned supine on a fracture table (Maquet, Wayne, NJ). The feet are well padded, and an extra-large perineal cushion is used to optimize distraction of the hip joint with the least amount of traction. The hip is then prepared and draped in a standard fashion. Adequate distraction is confirmed with fluoroscopic visualization of 10 to 15 mm of joint space widening in the anteroposterior plane. Key bony landmarks are identified, including the anterior superior iliac spine and the greater trochanter.
Portal Establishment
Portal establishment is performed in accordance with that previously described by Weiland and Philippon.9 To obtain adequate central compartment access the anterolateral portal is placed directly off of the anterior-superior portion of the greater trochanter under fluoroscopic guidance. This is followed by a placement of a modified anterolateral portal, under direct vision. This portal is established by identifying the intersection of the vertical line drawn from the anterior superior iliac spine distally and the horizontal line drawn from the superior surface of the femoral greater trochanter medially.
AIIS Exposure and Decompression
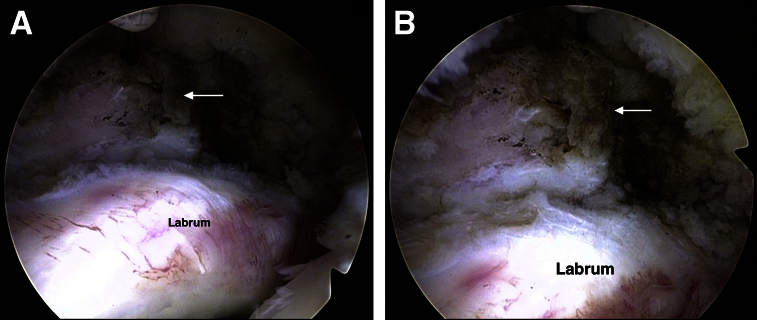
Capsulotomy between the 2 portals is conducted with an arthroscopic blade (DePuy Mitek, Raynham, MA) to facilitate instrument maneuverability. A thorough diagnostic evaluation of the hip is performed using a 70° arthroscope. Signs of pathology due to low AIIS can be seen in Figure 3. The arthroscopic diagnosis of prominent or low AIIS is performed both statically by probing the anterior capsule covering a bony protuberance on the anterior acetabular rim and dynamically by flexing the hip for proof of impingement (Fig 4). There are typical intraoperative findings associated with subspinal impingement. These findings include bruising of the labrum facing the protruding AIIS, or tearing of the labrum, and an adjacent wave sign on the corresponding chondrolabral junction (Fig 5). Capsular stripping off the AIIS as well as partial labral elevation off the acetabular rim is facilitated with a shoulder elevator and a 3.5-mm full radius resector shaver (Smith & Nephew, Andover, MA). AIIS decompression is performed with an arthroscopic burr (5.5-mm round burr, Smith & Nephew) to achieve a minimum of 11-mm (2 burr widths) clearance between the most anterior-inferior prominent point of the AIIS and the acetabular rim (Fig 6). During the osteoplasty, extra care is taken both at the borders of the acetabular rim and at attachment point of the rectus femoris tendon to protect the surrounding tissues. The osteoplasty creates a type I AIIS as described by Hetsroni et al.4 A false profile fluoroscopy confirms adequate AIIS decompression and dynamic hip flexion confirms clinical decompression. Labral repair and femoral osteoplasty is followed as needed. Tables 2 and 3 describe key steps and pearls and pitfalls of low AIIS decompression, respectively. Figure 7 shows the radiographic results of low AIIS decompression.
Fig 3.
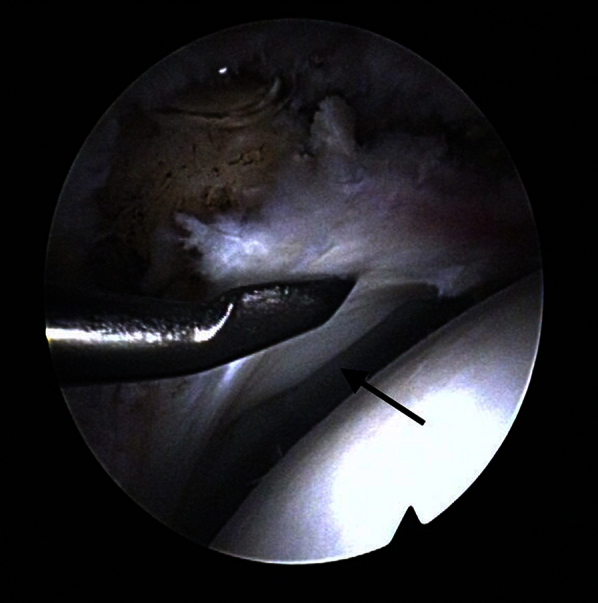
The labral wave sign. The physician produces the wave intraoperatively by applying pressure on the acetabular labrum and the “wave” is elicited in the articular cartilage of the acetabulum. The wave is shown with an arrow.
Fig 4.
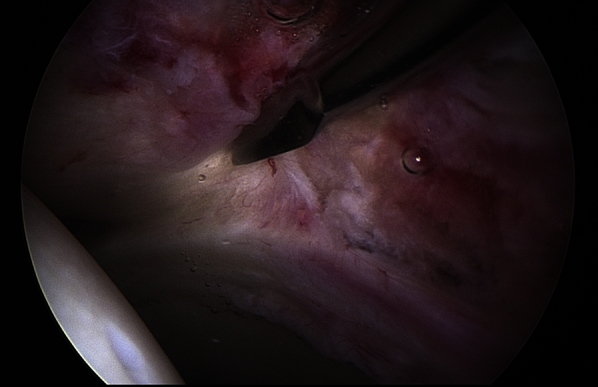
This image shows the surgeon palpating the low anterior inferior iliac spine (AIIS) through the capsule using a shoulder elevator tool. The AIIS should be probed through the capsule before capsular stripping and AIIS decompression.
Fig 5.
(A) Exposure of the low anterior inferior iliac spine (AIIS) with a radiofrequency ablation prob. Signs of labral pathology caused by the low AIIS, including hyperemia, can be seen on the labrum. (B) Further exposure of the low AIIS with the radiofrequency ablation prob. The exposed AIIS is labeled with an arrow in (A) and (B).
Fig 6.
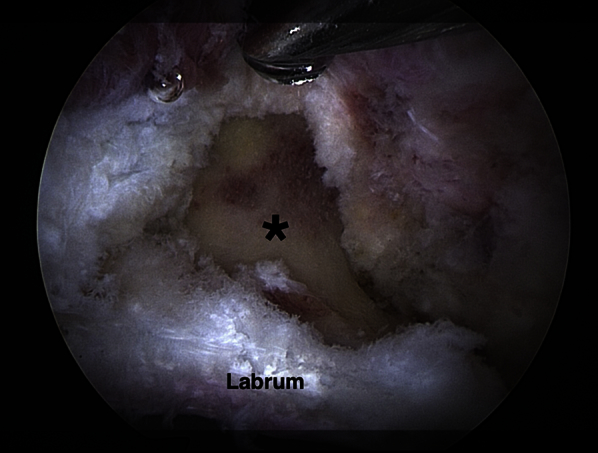
Intraoperative picture showing the result of low anterior inferior iliac spine decompression. The labrum can be seen inferiorly. Above the labrum the asterisk denotes the zone of decompression extending to the rim of the bony acetabulum inferiorly and to the attachment of the direct head of the rectus femoris tendon superiorly.
Table 2.
Key Steps in Low AIIS Decompression
| Step | Description |
|---|---|
| Find arthroscopic signs of impingement | Labral pathology, bruising, labral hyperemia acetabular cartilage wave sign |
| Assess protruding AIIS | Probe the bone deep to the capsule, facing the labral pathology |
| Expose the AIIS | Strip the capsule from the level of the labrum proximally to the level of the origin of the direct head of the rectus femoris |
| Preserve the labrum from injury during burring | Partially detach the labrum and expose the anterior rim of the acetabulum facing the AIIS |
| Burring | Osteoplasty of the AIIS from the level of the acetabular rim to the level of the direct head of the rectus femoris with care to protect the rectus origin |
AIIS, anterior inferior iliac spine.
Table 3.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| • Suspect subspinal impingement in any case of limited hip flexion and internal rotation • Obtain a false profile radiograph to visualize low AIIS • Use a blunt instrument to palpate bony protrusions extending beyond the capsule before capsular stripping • Avoid tendon damage by placing the external cannula of the burr against to rectus femoris tendon • Prescribe COX-2 inhibitors for 2 wk postoperatively to prevent heterotopic ossification |
• Failure to recognize the presence of low AIIS when the bony protuberance is projected anteriorly in anterior posterior radiographs • Overaggressive decompression can cause tendon damage • Wide capsulotomy on AIIS exposure |
AIIS, anterior inferior iliac spine.
Fig 7.
Postoperative radiograph of the patient in Figure 2. (A) The arrow shows the area in which the protruding low anterior inferior iliac spine (AIIS) was resected. This postoperative film can be compared with the preoperative film (Fig 2A). (B) The frog view postoperative radiograph of the patient in Fig 2. The arrow shows the area in which the low AIIS has been decompressed.
Postoperative Rehabilitation
Postoperative rehabilitation consists of weight bearing as tolerated with crutches for 2 weeks. Early range-of-motion exercises are encouraged to prevent soft tissue adhesions and promote early recovery. Passive motion is first restored, followed by active motion and then strength.
Discussion
AIIS is a relatively common form of extra-articular FAI. However, the first reports of low AIIS were only recently published. Low AIIS may be an underaddressed pathology because nonresected low AIIS has been found in up to 46% of revision hip arthroscopy surgeries.6 Amar et al.2 described normal AIIS morphology and concluded that the mean vertical distances from the AIIS to the acetabular rim are 13.5 mm and 11.4 mm in male and female patients, respectively. Low AIIS may not be easily visible on plain anterior posterior radiographs because the AIIS often does not extend laterally and is projected onto acetabulum making low AIIS challenging to diagnose with anterior posterior radiographs alone.2 AIIS extension to the level of the acetabular rim or distally is associated with a decrease in hip flexion and internal rotation (Fig 1).4 Accordingly, AIIS protruding to the level of the acetabular rim or distally can be considered a low AIIS (Fig 2). Low AIIS is underestimated radiographically because distally projecting AIIS morphology can cause the appearance of a crossover sign in up to 95% of hips independent of the presence or absence of true acetabular retroversion.10 Typical intraoperative findings are common in the case of subspinal impingement including labral bruising and acetabular cartilage wave sign facing the caudally prominent AIIS. Capsular stripping of the anterior acetabular rim is essential for AIIS exposure. Care must be taken not to resect bone overaggressively at the superior boarder of the osteoplasty because the rectus femoris could be detached from its origin, leading to a potential hip flexion deficit. Preserving the origin of the rectus femoris tendon is one advantage of arthroscopic AIIS decompression when compared with open techniques. Arthroscopic AIIS decompression allows for anatomical decompression and access to the articular surface of the acetabulum to simultaneously treat associated intra-articular pathologies. This technique is minimally invasive and allows for rapid recovery and return to activity. The risk and limitations of this procedure include decreased visualization and access compared with open techniques. Increased access to the AIIS may be required in the case of massive heterotopic ossification of the AIIS to achieve adequate decompression. In the case of type III AIIS where the bone protrudes beyond the level of the acetabulum, the surgeon is required to work in the extra-articular space, which requires additional knowledge and expertise. False profile fluoroscopy performed at the beginning and end of the procedure can accurately assess the AIIS morphology and show adequate AIIS osteoplaty (Fig 3).
Low AIIS decompression is a safe, effective, and reproducible procedure for addressing subspinal impingement. Creating a flat anterior acetabular surface between the most anteroinferior prominent point of the AIIS and the acetabular rim allows flexion and internal rotation of the hip joint without impingement. Careful execution of AIIS decompression can alleviate clinical symptoms of FAI and restore function to the hip joint. Further studies reporting and comparing outcomes of AIIS decompression surgical techniques are needed.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Low anterior inferior iliac spine (AIIS) decompression. A 21-year-old male patient presented to the hip clinic with a 4 months' history of groin pain exacerbated by squatting. There was no obvious history of an inciting event or previous injury. Physical examination was positive for anterior impingement tests and pain with flexion adduction internal rotation. Hip flexion and internal rotation were limited to 100° and 0°, respectively. Radiographs showed bilateral crossover sign and a low extending (grade III) AIIS on the right, in addition to CAM and Pincer lesions (Fig 2). The central edge angle was measured at 43° and the α angle at 70°. Magnetic resonance arthrography was negative for labral tear. Computed tomography showed significant hypertrophy of the AIIS bilaterally, although greater on the right side. The patient was placed on the operating table (supine position right side) and the portal establishment was conducted as previously described by Weiland and Philippon. Capsulotomy is performed using an arthroscopic blade and a diagnostic evaluation of the joint is performed. The AIIS is palpated and then the hip is dynamically motioned reproduce impingement. The capsule is stripped off of the AIIS and then the AIIS is decompressed using a 5.5-mm burr. Fluoroscopic images are taken intraoperatively to ensure that adequate decompression has been achieved.
References
- 1.Philippon M.J., Michalski M.P., Campbell K.J. An anatomical study of the acetabulum with clinical applications to hip arthroscopy. J Bone Joint Surg Am. 2014;96:1673–1682. doi: 10.2106/JBJS.M.01502. [DOI] [PubMed] [Google Scholar]
- 2.Amar E., Druckmann I., Flusser G., Safran M.R., Salai M., Rath E. The anterior inferior iliac spine: Size, position, and location. An anthropometric and sex survey. Arthroscopy. 2013;29:874–881. doi: 10.1016/j.arthro.2013.01.023. [DOI] [PubMed] [Google Scholar]
- 3.Hetsroni I., Larson C.M., Dela Torre K., Zbeda R.M., Magennis E., Kelly B.T. Anterior inferior iliac spine deformity as an extra-articular source for hip impingement: A series of 10 patients treated with arthroscopic decompression. Arthroscopy. 2012;28:1644–1653. doi: 10.1016/j.arthro.2012.05.882. [DOI] [PubMed] [Google Scholar]
- 4.Hetsroni I., Poultsides L., Bedi A., Larson C.M., Kelly B.T. Anterior inferior iliac spine morphology correlates with hip range of motion: A classification system and dynamic model. Clin Orthop Relat Res. 2013;471:2497–2503. doi: 10.1007/s11999-013-2847-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hapa O., Bedi A., Gursan O. Anatomic footprint of the direct head of the rectus femoris origin: Cadaveric study and clinical series of hips after arthroscopic anterior inferior iliac spine/subspine decompression. Arthroscopy. 2013;29:1932–1940. doi: 10.1016/j.arthro.2013.08.023. [DOI] [PubMed] [Google Scholar]
- 6.Larson C.M., Giveans M.R., Samuelson K.M., Stone R.M., Bedi A. Arthroscopic hip revision surgery for residual femoroacetabular impingement (FAI): Surgical outcomes compared with a matched cohort after primary arthroscopic FAI correction. Am J Sports Med. 2014;42:1785–1790. doi: 10.1177/0363546514534181. [DOI] [PubMed] [Google Scholar]
- 7.Larson C.M., Kelly B.T., Stone R.M. Making a case for anterior inferior iliac spine/subspine hip impingement: Three representative case reports and proposed concept. Arthroscopy. 2011;27:1732–1737. doi: 10.1016/j.arthro.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Amar E, Warschawski Y, Sharfman ZT, Martin HD, Safran MR, Rath E. Pathological findings in patients with low anterior inferior iliac spine impingement [published online November 30, 2015]. Surg Radiol Anat. doi:10.1007/s00276-015-1591-8. [DOI] [PubMed]
- 9.Kelly B.T., Weiland D.E., Schenker M.L., Philippon M.J. Arthroscopic labral repair in the hip: Surgical technique and review of the literature. Arthroscopy. 2005;21:1496–1504. doi: 10.1016/j.arthro.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 10.Zaltz I., Kelly B.T., Hetsroni I., Bedi A. The crossover sign overestimates acetabular retroversion. Clin Orthop Relat Res. 2013;471:2463–2470. doi: 10.1007/s11999-012-2689-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Low anterior inferior iliac spine (AIIS) decompression. A 21-year-old male patient presented to the hip clinic with a 4 months' history of groin pain exacerbated by squatting. There was no obvious history of an inciting event or previous injury. Physical examination was positive for anterior impingement tests and pain with flexion adduction internal rotation. Hip flexion and internal rotation were limited to 100° and 0°, respectively. Radiographs showed bilateral crossover sign and a low extending (grade III) AIIS on the right, in addition to CAM and Pincer lesions (Fig 2). The central edge angle was measured at 43° and the α angle at 70°. Magnetic resonance arthrography was negative for labral tear. Computed tomography showed significant hypertrophy of the AIIS bilaterally, although greater on the right side. The patient was placed on the operating table (supine position right side) and the portal establishment was conducted as previously described by Weiland and Philippon. Capsulotomy is performed using an arthroscopic blade and a diagnostic evaluation of the joint is performed. The AIIS is palpated and then the hip is dynamically motioned reproduce impingement. The capsule is stripped off of the AIIS and then the AIIS is decompressed using a 5.5-mm burr. Fluoroscopic images are taken intraoperatively to ensure that adequate decompression has been achieved.