Highlights
-
•
Only about 250 cases of bladder leiomyoma reported in English literature.
-
•
This is the first reported case to present in acute manner as a case of febrile UTI.
-
•
Imaging is mandatory to diagnose the underlying cause of febrile UTI.
-
•
Though benign, failure to diagnose the lesion may lead to recurrence of severe UTI.
Keywords: Case report, Urinary bladder, Leiomyoma, Urinary bladder neoplasms, Urinary tract infections
Abstract
Introduction
Leiomyomas of urinary bladder constitute only about 0.43% of all bladder tumors. Only about 250 cases were reported in English literature. This is the first reported case of bladder leiomyoma to present with febrile urinary tract infection.
Case presentation
We report a case of a 37- year old male who presented with febrile urinary tract infection. Imaging showed a bladder lesion. This lesion was managed by transurethral resection. Pathologic diagnosis was bladder leiomyoma.
Discussion
Although bladder leiomyomas are benign, they can cause serious sequelae, including serious urinary tract infections as the case we present here shows. This is why it is important to early diagnose and treat this condition.
Conclusion
This case highlights the importance of early introduction of imaging in patients presenting with severe urinary tract infections. Failure to diagnose this lesion as the underlying cause of infection may have easily led to recurrence of similar severe life-threatening infections.
1. Introduction
Most Urinary bladder tumors are malignant, the majority arise from urothelium. Mesenchymal tumors of the bladder are rare, forming about 1–5% of all bladder tumors, with leiomyoma constituting less than 0.43% of all [1]. Only about 250 cases were reported in English literature [2].
Most reported cases of bladder leiomyoma had presented with irritative symptoms, obstructive symptoms, or hematuria, in addition to asymptomatic incidental cases [3].
Here, we report a case of bladder leiomyoma, presented to emergency department as a case of febrile urinary tract infection. To our knowledge, this is the first reported case of bladder leiomyoma presenting in this manner. This case was reported in compliance with the CARE criteria [4].
2. Case presentation
A 37-year old male, previously medically fit, presented to emergency department with one day history of severe dysuria, urgency, significant frequency, fever and chills. There was no hematuria or loin pain. He had never experienced these symptoms before. He was a heavy smoker. On examination, the patient was ill-looking, febrile (39.3c), with normal blood pressure. Laboratory findings showed leukocytosis, with left shift. Urinalysis showed numerous white blood cells per high power field, 1–2 red blood cells per high power field and bacteria were seen.
Urinary tract ultrasound showed a relatively defined lobulated, heterogeneous, mostly isoechoic mass, with possible mural calcification and intralesional blood flow seen at the right anterolateral wall of urinary bladder. Normal kidneys with no hydronephrosis were seen.
A urinary tract computed tomography (CT) scan showed the same large oval-shaped right sided bladder mass, which measured 5.5 × 4.3 cm, with mildly dilated right lower ureter (Fig. 1).
Fig. 1.
Computed tomography showing a large oval bladder tumor seen mainly at the right side of bladder (arrow) measuring about 5.5 × 4.3 cm.
The patient was admitted to ward as a case of febrile urinary tract infection, for management and further evaluation of the bladder mass. The patient was started on intravenous imipenem-cilastatin, fluids and regular monitoring. Four days later, the patient improved. Urine culture at this time came with Escherichia coli that was resistant to most antibiotics except imipinem and ertapenem.
Urine cytology showed unremarkable squamous and urothelial cells, and was negative for malignancy.
Cystoscopy under general anesthesia was performed after stabilization; it showed a huge bulging mass from the right lateral wall with intact overlying mucosa and smooth contour. Examination under anesthesia revealed a palpable mobile centralized lower abdominal mass. Transurethral resection of bladder tumor (TURBT) was done, and tissue sent to pathology.
The patient’s postoperative period was unremarkable; he recovered fully and then was discharged home.
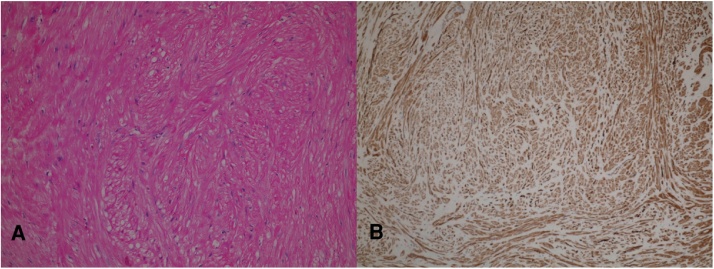
Pathology proved that the mass was a benign submucosal leiomyoma. The lesion consisted of interlacing fascicles of spindle-shaped cells. The cells displayed no pleomorphism, and contained bland looking central spindle nuclei and eosinophilic cytoplasm. No mitotic activity or coagulative necrosis was seen despite microscopic examination of the whole tissue fragments. The overlying urothelial mucosa was mildly inflamed; however, neither dysplasia nor malignancy was identified.
The submucosal lesion has the morphologic characteristics of a benign smooth muscle tumor (leiomyoma). This was confirmed by immunohistochemical stain with smooth muscle actin (SMA), which showed diffuse and strong positivity. The benign behavior of this tumor is favored histologically by the well-demarcated borders, absence of cytologic atypia, absence of increased mitotic activity, as well as lack of coagulative tumor necrosis (Fig. 2).
Fig. 2.
Microscopic picutre of the leiomyoma. Interlacing fasicles of spindle cell, hematoxylin and eosin stain (A). Immunohistochemical reactivity for smooth muscle actin (SMA) stain (B).
Original magnifications 100×.
2.1. Follow up
At follow-up, one year later, the patient has no urinary symptoms, doing well and urine culture is negative.
3. Discussion
Leiomyomas of urinary bladder, although rare, are the most common benign bladder neoplasms [5]. These smooth muscle benign tumors are more common in females, with a female: male ratio approaching 3:1 [3], [6]. Mean age of diagnosis is around 45 years [3], [6]. Leiomyomas can be endovesical, intramural or extravesical. Endovesical lesions are the most common, representing about 51–86% of cases, intramural lesions forming 3–30%, and extravesical lesions occur in 11–30% [3], [6], [7].
Some theories were proposed to explain the pathophysiology behind these lesions. Hormonal influences may play a role in the pathogenesis, and this theory may explain why a known risk factor is female gender [3], [5], [8]. Other theories include the presence of embryonic rests of tissue in bladder (dysontogenesis), metaplastic transformation of bladder vasculature, and bladder musculature infection causing inflammation and later development of these lesions [8].
Microscopically, bladder leiomyomas resemble leiomyomas of the uterus. They are characterized by fascicles of smooth muscle cells with centrally located oval or cigar-like nuclei without significant atypical changes [5].
The differential diagnoses of spindle cell lesions of the bladder include leiomyoma and leiomyosarcoma. Leiomyomas and leiomyosarcomas are distinguished morphologically by the circumscription, and lack of cytologic atypia, mitotic activity, and coagulative necrosis in the former. By contrast, leiomyosarcomas show an infiltrative growth pattern, frequent necrosis, high cellularity, cytologic atypia and increased mitotic activity [9]. Other differentials include postoperative spindle cell nodules, in which patients have a history of a recent surgical procedure. These reactive lesions also show marked cellularity and high mitotic activity, but lack the pleomorphism exhibited by leiomyosarcomas, and unlike leiomyosarcomas, are immunoreactive for low molecular weight cytokeratin. A lesion that enters the differential diagnostic list is inflammatory pseudotumour, a highly cellular and pleomorphic growth, that is distinguished from sarcomas by their highly myxoid and inflammatory background [9].
Bladder leiomyomas vary in mode of presentation, the most common presentation differs according to series studied, with irritative symptoms being the most common (50%) in a pooled analysis of 90 cases reported by Silva-Ramos [6], and obstructive symptoms were the most presenting complaint (49%) in the 37 cases studied by Goluboff [3]. The case we report here is the first case of bladder leiomyoma presenting in an acute manner, with fever due to urinary tract infection. The present case presented with resistant bacteria, which is unusual in non-hospital acquired urinary tract infections at our institution. The significance of this resistance and its relation to leiomyoma is not clear, and may need further research.
Imaging plays an important role in diagnosis of bladder leiomyomas. Excretory urography may show a bladder filling defect with no mucosal ulceration that may be confused with prostate in males [10]. Ultrasonography can show an intact mucosa, submucosal location, and can distinguish solid from cystic lesions. CT scans can identify the accurate location of these tumors, but they are not adequate to distinguish the solid nature of the lesion. Ultrasonography should be performed in indeterminate lesions seen on CT [10]. In the present case, ultrasonography showed a well-defined lobulated bladder lesion; findings that were also supported by CT.
Magnetic resonance imaging (MRI) can distinguish between mesenchymal and transitional cell tumors [11]. Leiomyomas have intermediate signal intensity on T1-weighted images, while T2-weighted images show low signal intensity [12].
Cystoscopy and biopsy are needed to accurately rule out malignancy, as it may be difficult to definitely differentiate between leiomyoma and leiomyosarcoma based on radiologic appearance alone [13]. Cystoscopy typically shows, as in our case, a bladder mass, with smooth intact mucosa [3].
Management of leiomyomas is mainly guided by size and location of the tumor [5]. Treatment options have ranged from enucleation, partial cystectomy and even rarely radical cystectomy. Transurethral resection has also been performed in amenable lesions with success [6]. The present case has been successfully managed with transurethral resection. Studies showed that leiomyomas can be readily and successfully treated with transurethral resection [3]. Laparoscopic approach has been described in a few cases [14].
Recurrence after surgical removal is rare and recurrent cases have been successfully managed with repeat enucleation or transurethral resection [5]. Putting in mind the rarity of recurrence of leiomyoma after treatment, and the ease of management when disease recurs, we suggest following the patient based on symptoms, without exposing him to invasive or radiologic investigations to detect small asymptomatic recurrences, given the fact that no clear guidelines exist regarding follow-up of these cases.
4. Conclusion
This case demonstrates that despite the benign nature of these lesions, they are not without serious sequelae. A serious febrile urinary tract infection has developed in this case as the first presentation of a bladder leiomyoma. Failure to diagnose this lesion as the underlying cause of infection may have easily led to recurrence of similar severe life-threatening infections. The lesson learned here is that imaging should be introduced in the evaluation of severe urinary tract infections.
Conflicts of interest
All authors declare that they have no conflicts of interest regarding this article.
Funding
All authors declare that they have no sources of funding for this article.
Ethical approval
This is a report of a case, no research was conducted on patients that needed ethical approval.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors contributions
Ra’ed Haddad: Literature Review, Case presentation, Corresponding and main author.
Mujalli Murshidi: Main Surgeon, Performed TURBT of the lesion and main attending for the patient.
Nisreen Abu Shahin: Pathology part from diagnosis to literature review.
Muayyad Murshidi: Imaging, literature review, Review of final manuscript.
Guarantor
Mujalli Murshidi and Ra’ed Haddad.
Contributor Information
Ra’ed Ghassan Haddad, Email: rgh_1986@yahoo.com.
Mujalli Mhailan Murshidi, Email: mujalli_mhailan@hotmail.com.
Nisreen Abu Shahin, Email: nisreenshahin@yahoo.com.
Muayyad Mujalli Murshidi, Email: moaiad_mhailan_1990@hotmail.com.
References
- 1.Cornella J.L., Larson T.R., Lee R.A., Magrina J.F., Kammerer-Doak D. Leiomyoma of the female urethra and bladder: report of twenty-three patients and review of the literature. Am. J. Obstet. Gynecol. 1997;176:1278–1285. doi: 10.1016/s0002-9378(97)70346-6. [DOI] [PubMed] [Google Scholar]
- 2.Jain S.K., Tanwar R., Mitra A. Bladder leiomyoma presenting with luts and coexisting bladder and uterine leiomyomata: a review of two cases. Rev. Urol. 2014;16:50–54. [PMC free article] [PubMed] [Google Scholar]
- 3.Goluboff E.T., O'Toole K., Sawczuk I.S. Leiomyoma of bladder: report of case and review of literature. Urology. 1994;43:238–241. doi: 10.1016/0090-4295(94)90053-1. [DOI] [PubMed] [Google Scholar]
- 4.Gagnier J.J., Kienle G., Altman D.G. The CARE guidelines: consensus-based clinical case report guideline development. J. Clin. Epidemiol. 2014;67:46–51. doi: 10.1016/j.jclinepi.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Park J.W., Jeong B.C., Seo S.I., Jeon S.S., Kwon G.Y., Lee H.M. Leiomyoma of the urinary bladder: a series of nine cases and review of the literature. Urology. 2010;76:1425–1429. doi: 10.1016/j.urology.2010.02.046. [DOI] [PubMed] [Google Scholar]
- 6.Silva-Ramos M., Masso P., Versos R., Soares J., Pimenta A. [Leiomyoma of the bladder. Analysis of a collection of 90 cases] Actas Urol. Esp. 2003;27:581–586. doi: 10.1016/s0210-4806(03)72979-9. [DOI] [PubMed] [Google Scholar]
- 7.Knoll L.D., Segura J.W., Scheithauer B.W. Leiomyoma of the bladder. J. Urol. 1986;136:906–908. doi: 10.1016/s0022-5347(17)45124-x. [DOI] [PubMed] [Google Scholar]
- 8.Teran A., Gambrell R., Jr. Leiomyoma of the bladder: case report and review of the literature. Int. J. Fertil. 1988;34:289–292. [PubMed] [Google Scholar]
- 9.Eble J.N., World Health Organization . Lyon : IARC Press; 2004. International Agency for Research on Cancer Pathology and Genetics of Tumours of The Urinary System and Male Genital Organs. [Google Scholar]
- 10.Illescas F.F., Baker M.E., Weinerth J.L. Bladder leiomyoma: advantages of sonography over computed tomography. Urol. Radiol. 1986;8:216–218. doi: 10.1007/BF02924110. [DOI] [PubMed] [Google Scholar]
- 11.Sundaram C.P., Rawal A., Saltzman B. Characteristics of bladder leiomyoma as noted on magnetic resonance imaging. Urology. 1998;52:1142–1143. doi: 10.1016/s0090-4295(98)00333-1. [DOI] [PubMed] [Google Scholar]
- 12.Maya M.M., Slywotzky C. Urinary bladder leiomyoma: magnetic resonance imaging findings. Urol. Radiol. 1992;14:197–199. doi: 10.1007/BF02926929. [DOI] [PubMed] [Google Scholar]
- 13.Wong-You-Cheong J.J., Woodward P.J., Manning M.A., Sesterhenn I.A. From the archives of the AFIP: neoplasms of the urinary bladder: radiologic-pathologic correlation. Radiographics. 2006;26:553–580. doi: 10.1148/rg.262055172. [DOI] [PubMed] [Google Scholar]
- 14.G. Vitagliano, R. Castilla, J. Fernandez Long, Giant asymptomatic endovesical bladder leiomyoma laparoscopically excised. CRSLS e2014.235.