Abstract
Objective
The purpose of this study is to describe the chiropractic management of a student athlete with postconcussion syndrome.
Clinical Features
A 14-year-old male hockey player presented to a chiropractic clinic with postconcussion symptoms 13 days after his initial injury. He experienced an occipital headache with a pain rating of 8/10, upset stomach, blurry vision, nausea, dizziness, balance problems, a “foggy feeling,” difficulty with concentration, difficulty with memory, fatigue, confusion, drowsiness, and irritability. Prior to seeing the doctor of chiropractic, the patient was monitored by a medical doctor, and the care he had been receiving was in accordance with current concussion guidelines. At the time of presentation to the chiropractic clinic, he had failed to progress toward return to play, and his computerized neurocognitive testing scores had not improved.
Intervention and Outcome
Chiropractic manipulative therapy, myofascial release, instrument-assisted soft tissue technique, and therapeutic exercises were provided over 5 treatments spanning a 20-day period. The patient followed up each treatment with ImPACT testing. At the conclusion of the treatments, the patient’s computerized neurocognitive testing scores had improved, and the patient was returned to play.
Conclusion
This case demonstrates the improvement of postconcussion syndrome in a 14-year-old male hockey player under chiropractic management.
Key Indexing Terms: Postconcussion syndrome, Chiropractic, Brain concussion
Introduction
Concussion is a subset of a traumatic brain injury (TBI) and is often classified as a mild traumatic brain injury (mTBI). Concussion is a brain injury resulting from a low-velocity force in which the brain is shaken, resulting in clinical symptoms which are not necessarily related to a pathological injury. It is a complex pathophysiological process leading to a wide array of symptoms.1 It is the common result of a direct blow to the head in contact sports; however, it can be a consequence of collisions and falls. It can also be the result of a whiplash-type injury without a direct blow to the head.2 With the growing concern of TBIs in athletics, the balance between athletes maintaining a competitive edge in a sport and participant safety has become gray. The balancing between this has been left up to coaches, doctors, players, team trainers, and even parents. The role of the health care provider is the rapid assessment of the injured athlete and the guidance toward a safe return to play.
At present, there are very few case reports describing the chiropractic management of a patient with concussion and return to play. Therefore, the purpose of this case report is to describe the chiropractic management of a student athlete with postconcussion syndrome (PCS).
Case Report
A 14-year-old adolescent boy presented 13 days after sustaining a concussion while competing in a hockey game. He was skating along the boards with the puck, passed the puck to his teammate, and then lifted his head. At that moment, he saw his opponent skating toward him who then checked him into the boards. The opponent hit the left side of the athlete’s body, with the athlete’s right side of his body hitting the boards. He was knocked to the ground but able to get up. He continued to play for 2 more shifts, which usually last about 30-90 seconds, before becoming nauseous. At that time, he sat down for the rest of the game. He reports that he was told by numerous teammates that he was acting out of character. He was brought into the local emergency department, and at that time, he did not know what position he played and the date of his birthday, and he was struggling with name recognition. A computed tomography scan of his neck and head was ordered but found to be negative for pathology. Over the course of the next 2 weeks, the patient was monitored by a medical doctor and was seen by a physical therapist. The care he had been receiving was in accordance to current concussion guidelines. During this time, he failed to progress along the return-to-play protocol because of ongoing symptoms of PCS. His computerized neurocognitive (ImPACT Applications, Pittsburgh, PA) testing scores had remained poor.
The patient presented to a chiropractic clinic. Subjective findings on the date of initial examination included a constant occipital headache with a numeric pain rating of 8 of 10, upset stomach, blurry vision with concentration, difficulty remembering names, nausea, dizziness, balance problems, feeling in a “fog,” difficulty with concentration, difficulty with memory, fatigue, confusion, drowsiness, and irritability. The patient did not report neck pain. He denied any upper or lower extremity radicular symptoms.
Cognitively, the patient was alert and oriented to the month, day of the week, year, and time; however, he did not know the date of the month. He scored a 9 of 15 on immediate memory testing and a 2 of 5 on his concentration testing. His delayed memory assessment was a 3 of 5. Romberg’s test result was positive with his eyes open and eyes closed. The patient was unable to hop on 1 foot because it would cause dizziness and nausea. In a 20-second time period for balance testing in a double leg stance, he had 1 error; in single leg stance, he had 4 errors; and he had 4 errors in a tandem stance. Finger to nose test was abnormal with the patient tending to touch his finger to his upper lip. Results of diadochokinesia testing and heel-to-shin testing were normal. Musculoskeletal palpation revealed taut and tender muscle fibers in the left suboccipitals, left levator scapulae, left serratus posterior, right lumbosacral paraspinals, right quadratus lumborum, and right piriformis. He had mild reductions in cervical flexion, extension, and bilateral rotation and mild to moderate reduction in right lateral flexion. Left lateral flexion was normal. There was tenderness to palpation at C2, T2, and L2. He had a high left shoulder, high right ilium, bilateral rounded shoulders, and anterior head carriage. Neurologically, he had 4 of 5 strength testing for bilateral levels at C5, C6, C7, C8, T1, L4, L5, and S1. His reflexes were normal, and dermatomal sensory testing was not performed because he denied any radicular symptoms. Orthopedically, the patient had positive results in foraminal compression test and shoulder depression tests, reproducing midcervical spine pain without radicular pain. Soto Hall’s test caused pain in the cervical-thoracic junction. Valsalva’s test result was negative.
The patient was diagnosed with PCS in which his concussion was sustained 13 days prior to the initial examination. At this time, the patient and mother gave consent for him to go through a trial of chiropractic care.
Multimodal manual therapy interventions were used, which included spinal manipulative therapy, myofascial release, and instrument-assisted soft tissue mobilization in the form of Graston Technique. The patient followed up with care 3 days later. At this visit, he reported improvements in his headaches. He reported intermittent headaches, and the pain level was 6 of 10. The patient still did not have any neck pain. He also noted improvements in balance. Evaluation still revealed the same muscular hypertonicity as found at the initial examination. The same multimodal manual therapy approach was used, and therapeutic exercise was added. This consisted of 2 sets of 10 cervical retractions, 3 sets of 10 heel-to-shin walks, and 3 sets of 10 heel-to-toes backwards walk. He was instructed to perform these exercises 3 × a day at home.
During his third visit 2 days later, he reported having 1 mild headache since his previous visit, and he did not have a headache at the time of presentation. Earlier in the day, the patient had his first computerized neurocognitive test since care had been initiated in the chiropractic office. He reported that his score had improved substantially. He also relayed an improvement in balance and denied any vision problems.
During evaluation, improvements were noted in Romberg’s and heel-to-shin testing. Multimodal manual therapy intervention was again provided. In addition, it was deemed appropriate to begin treating along the posterior oblique fascial sling with instrument-assisted soft tissue mobilization. The patient was given more challenging exercises, including cervical retraction with superior ocular movement, heel-to-shin walk with the eyes open and closed, heel-to-toe backwards walk with the eyes open and closed, and karaoke (sideways, crisscross steps with the eyes open).
At the fourth visit 5 days later, the patient reported no headaches since the previous visit. He had been compliant with all of his exercises and indicated that they had become easy. He was also cleared by his medical doctor to perform light skating. Subjective findings included cervical stiffness and mild low back pain. During evaluation, Romberg’s test result with eyes open and closed was normal. Heel-to-toe backwards walk was normal with the eyes open and mildly difficult with the eyes closed. The patient was still having difficulty performing karaoke with his eyes open. Treatment at this session included multimodal manual therapy intervention identical to the previous treatment. Therapeutic exercises included cervical retraction with superior ocular movement, heel-to-shin walk with eyes open and closed, karaoke with eyes open, and high knee marching with arm swing to further engage both posterior oblique fascial slings.
Nine days after his fourth treatment, the patient returned for follow-up. At this point, the patient had been cleared to play by his primary medical doctor after completing the graded return-to-play protocol. He indicated that practice and games had been going well. He did take 1 hard hit at his last game, which did cause a mild headache. He sat out the remainder of the game. The headache later disappeared and did not return. The patient also reported that he had lifted weights twice since his last treatment. He noted mild left-sided neck stiffness and mild right-sided low back stiffness. During evaluation, the patient was able to perform Romberg’s test, heel-to-shin walk, heel-to-toe backwards walk, and high-knee march all well with eyes open and closed. His karaoke with eyes open was normal. The patient was treated with multimodal manual therapy intervention to the same spinal and myofascial regions. The patient was told to continue with them at home and was discharged at this time with instruction to contact his primary care provider if symptoms return.
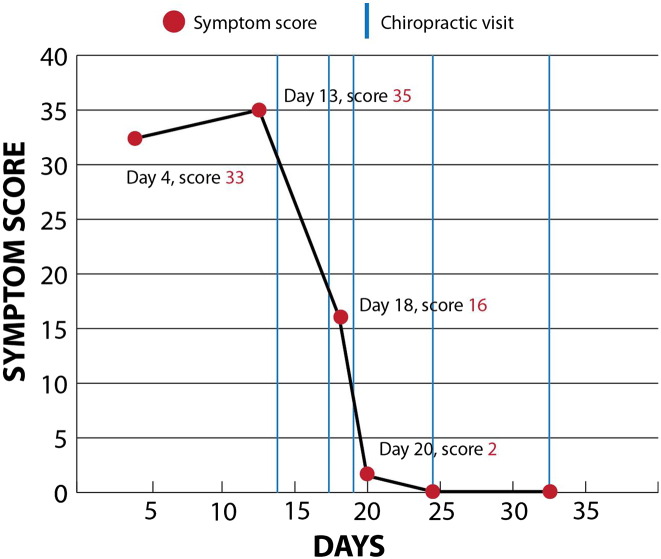
Throughout the course of care, this athlete’s progress was being monitored with computerized neurocognitive testing. Unfortunately, the patient did not have a baseline computerized neurocognitive test. However, after sustaining his concussion, he had his first computerized neurocognitive test administered 3 days later. His composite scores are displayed in Fig 1. He had a total of 4 computerized neurocognitive tests following his concussion.
Fig 1.
Composite scores.
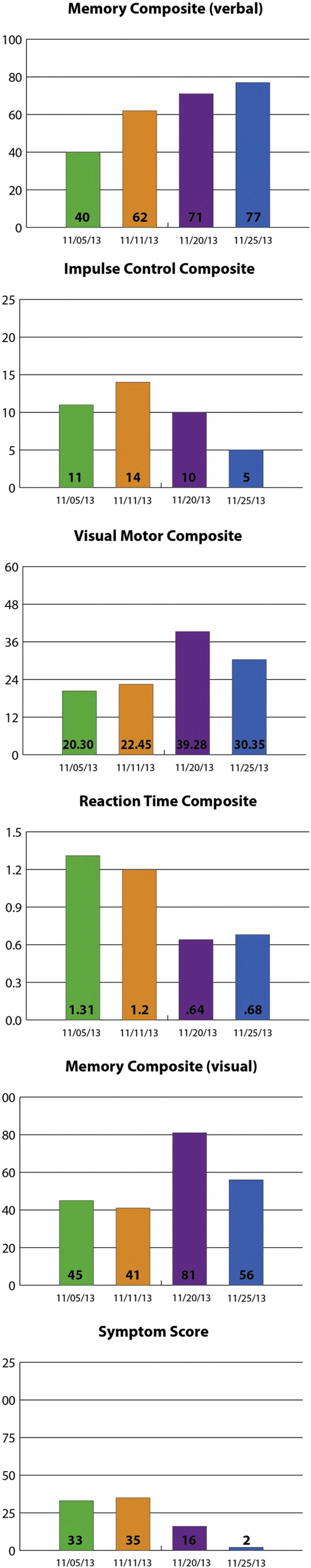
The athlete’s first 2 computerized neurocognitive examinations had been rendered before he started care in the chiropractic office. These examinations were ordered by the treating physician and rendered by the physical therapist. The first 2 computerized neurocognitive examinations were performed 11 days apart, in which the athlete’s treatment had only consisted of therapeutic exercises as prescribed by the physical therapist. During this time, the athlete did not receive any hands-on manual therapy to address vertebral or soft tissue dysfunction. The third computerized neurocognitive test results fell after the athlete had undergone 2 chiropractic treatments. His final computerized neurocognitive test was performed the same day as his fourth chiropractic treatment, again ordered by the medical doctor. Fig 2 displays his overall improvement in symptom scores along and the days that chiropractic intervention was used.
Fig 2.
Overall improvement in symptom scores during days of chiropractic management.
Throughout the entire course of chiropractic intervention, the patient was monitored by his medical doctor. It was not until his computerized neurocognitive testing score had substantially improved and his symptoms resolved that his medical doctor cleared him to play. The mother gave consent for her son’s health information to be included in this case report.
Discussion
Concussions are one of many injuries that present into a chiropractic office. Therefore, it is important that the practicing chiropractic physician be up-to-date with the current guidelines and literature that relate to mTBIs. The management of athletes with head injuries requires specific clinical decision making, adherence to already established protocols, and integrated care with other health care professionals.3 There are several concussion guidelines available in professional bodies, with a very helpful article being the “Consensus Statement on Concussion in Sport—the 4th International Conference on Concussion in Sport held in Zurich, November 2012.” These Zurich guidelines allow for a uniform perspective during the examination process of a concussion.4
The current protocols in place for returning an athlete back to play center around the resolution of physical symptoms of a concussion. Internationally accepted standards suggest that once the physical symptoms resolve, the athlete is taken through 5 graded stages, each stage lasting a minimum of 24 hours. During each stage, the athlete’s physical activity gradually increases to eventually allow full contact practice prior to game play. To progress through these stages, the athlete must remain symptom free.1, 4, 5 However, recent research has identified that balance dysfunction and cognitive deficits persist well beyond the physical symptoms of the recovery process.5 The length of recovery following a concussion varies, lasting anywhere from 1 week to several months.6, 7 Risk factors that can lead to increased recovery time include a history of 1 or multiple concussions and a greater number, severity, and duration of symptoms after the injury.7 More recent literature suggests that children and adolescents between the ages of 10 and 17 years display a gradual reduction of postconcussive symptoms over a 30-day time span following the injury. Five days after injury, 87% of the concussed individuals continued to display symptoms. The neurocognitive computerized testing scores returned to baseline levels by day 30.6 With this being said, simply following the current return-to-play guidelines with only resolution of an athlete’s physical symptoms may not be enough to warrant a safe return to play. A previously concussed athlete may be symptom free and returned to a neuropsychological baseline; however, the athlete may continue to have prolonged neurological abnormalities that could have resulted in disqualifying them from being ready to return to such a sport as evident by neurocognitive computerized testing. It appears that some neurological deficits persist beyond the current return-to-play standards and that there is discrepancy between common practices in returning athletes to competition.8 Using computerized neurocognitive test scores with subjective symptom complaints increases the sensitivity in identifying individuals that may require longer recovery.9 By combining physical symptom scores with the computerized neurocognitive scores, clinicians should be able to make safer return-to-play decisions.
The primary forms of treatment for PCS traditionally have included education, physical and cognitive rest, neurocognitive rehabilitation, and antidepressants. These forms of treatment have shown little effectiveness in the treatment of PCS.10 Recently, numerous studies have begun looking at multimodal treatment options to include but not be limited to cervical spine dysfunction, vestibular rehabilitation, visual training, and cardiovascular training. It has been reported in the literature that postconcussion symptoms may be associated with cervical spine and/or vestibular dysfunction.11, 12 Indeed, one study showed that there is no discrimination in symptoms following head injury between concussion and cervical/vestibular injury.13 Cervical spine dysfunction due to whiplash-type injury is a one of many proposed theories for PCS.14 This presents an excellent opportunity for chiropractors to play a role in the integrative approach to helping the athlete recover from a concussion.
Regarding the pathophysiology of concussions, it is hypothesized that, during the acute phase of mTBI, there are ion imbalance, metabolic disruption, blood flow abnormalities, and autonomic nervous system disruption as the primary culprit.14 However, the proposed mechanisms for PCS are inconsistent. As mentioned, the cervical spine whiplash injury is a proposed mechanism, but it has not been examined in great detail. It is reasonable to expect that any significant blunt impact and/or an acceleration/deceleration of the head will result in some amount of inertial loading of the neck resulting in a cervical spine strain/sprain injury.14 Injury and dysfunction of the cervical spine have been shown to cause headaches, dizziness, loss of balance, nausea, visual and auditory disturbances, reduced cognitive function, and many other signs and symptoms considered synonymous with mTBI.15, 16, 17, 18, 19, 20, 21, 22 Thus, in concussion injuries, it is proposed that headaches and dizziness, again so prevalent in mTBIs, may be the result of cervicogenic mechanisms due to a concomitant whiplash injury suffered at the same time the athlete sustained a concussion.23, 24, 25, 26 Whiplash injuries result in both pain and proprioceptive deficits, leading to headaches that are related to pain and cervicogenic dizziness and oculomotor control deficits associated with proprioceptive dysfunction.14
Limitations
This is a case report; therefore, causation cannot be implied. This is an example of 1 case only. To further gauge the effectiveness of care, further studies need to be completed. Most athletes with sports-related concussions will recover within 21-28 days. Symptoms demonstrated the greatest improvement in the first 2 weeks, although neurocognitive impairment lingered across various domains up to 28 days after a sport-related concussion.27 This athlete fell within this time frame in regard to improvement.
This athlete did not have a baseline ImPACT test performed. Therefore, a comparison was not made between his baseline score and his postinjury scores. This could have resulted in allowing the athlete to return to play before his cognitive scores had improved to those which would have been his baseline scores. As this case report demonstrates improvement in PCS, it is just 1 case with 1 particular treatment approach that was used. Furthermore, it is not evident that the athlete benefited from chiropractic vs natural progression of PCS. His recovery still fell within what the literature suggests is the normal time frame for PCS. However, the data display that his results improved quickly and substantially after chiropractic intervention. There was nearly a 50% improvement in his total symptom score only 3 days after chiropractic intervention started. Literature mentioned above describes more of a gradual resolution in symptoms. However, more research is required to determine if the management was the best approach to care. It is also limited in the fact that there was not a baseline to the computerized neurocognitive score to compare and determine how much of an overall change was attained prior to having a preinjury status. This type of treatment is certainly an area of need for the doctor of chiropractic to evaluate and understand other mechanisms that may be contributing to the patient’s symptomatology including cervicogenic and vestibular mechanisms.
Conclusion
A 14-year-old male hockey player with symptoms of PCS was managed in a chiropractic clinic with concurrent medical observation. Throughout the course of his care, his symptoms resolved and his neurocognitive computer-based testing scores improved. He was eventually cleared to play following the correct return-to-play guidelines.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
References
- 1.McCrory P, Meeuwiss WH, Aubry M. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2013;47:250–258. doi: 10.1136/bjsports-2013-092313. [DOI] [PubMed] [Google Scholar]
- 2.Kelly J, Rosenberg J. Diagnosis and management of concussion in sport. Neurology. 1997;48:575–580. doi: 10.1212/wnl.48.3.575. [DOI] [PubMed] [Google Scholar]
- 3.Johnson CD, Green BN, Nelson RC, Moreau B, Nabhan D. Chiropractic and concussion in sport: a narrative review of the literature. J Chiropr Med. 2013;12(4):216–229. doi: 10.1016/j.jcm.2013.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clay MB, Glover KL, Lowe DT. Epidemiology of concussion in sport: a literature review. J Chiropr Med. 2013;12(4):230–251. doi: 10.1016/j.jcm.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baker CS, Cinelli ME. Visuomotor deficits during locomotion in previously concussed athletes 30 or more days following return to play. Physiol Rep. 2014;2(12) doi: 10.14814/phy2.12252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crowe L, Collie A, Hearps S. Cognitive and physical symptoms of concussive injury in children: a detailed longitudinal recovery study. Br J Sports Med. 2016;50:311–316. doi: 10.1136/bjsports-2015-094663. [DOI] [PubMed] [Google Scholar]
- 7.Shim J, Smith DH, Van Lunen BL. On-field signs and symptoms associated with recovery duration after concussion in high school and college athletes: a critically appraised topic. J Sport Rehabil. 2015;24(1):72–76. doi: 10.1123/jsr.2013-0058. [DOI] [PubMed] [Google Scholar]
- 8.Porcher NJ, Solecki TJ. A narrative review of sports-related concussion and return-to-play testing with asymptomatic athletes. J Chiropr Med. 2013;12(4):260–268. doi: 10.1016/j.jcm.2013.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lau B, Collins M, Lovell M. Sensitivity and specificity of subacute computerized neurocognitive testing and symptom evaluation in predicting outcomes after sports-related concussion. Am J Sports Med. 2011;39(6):1209–1216. doi: 10.1177/0363546510392016. [DOI] [PubMed] [Google Scholar]
- 10.Willer B, Leddy JJ. Management of concussion and post-concussion syndrome. Curr Treat Options Neurol. 2006;8:415–426. doi: 10.1007/s11940-006-0031-9. [DOI] [PubMed] [Google Scholar]
- 11.Alsalaheen B, Mucha A, Morris L. Vestibular rehabilitation for dizziness and balance disorders after concussion. J Neurol Phys Ther. 2010;34:87–93. doi: 10.1097/NPT.0b013e3181dde568. [DOI] [PubMed] [Google Scholar]
- 12.Schneider K, Meeuwisse W, Nettel-Aguire A. Cervicovestibular rehabilitation in sport-related concussion: a randomized controlled trial. Br J Sports Med. 2014;48(17):1294–1298. doi: 10.1136/bjsports-2013-093267. [DOI] [PubMed] [Google Scholar]
- 13.Leddy J, Baker J, Merchant A. Brain or strain? Symptoms alone do not distinguish physiologic concussion from cervical/vestibular injury. Clin J Sport Med. 2015;25(3):237–242. doi: 10.1097/JSM.0000000000000128. [DOI] [PubMed] [Google Scholar]
- 14.Marshall CM, Vernon H, Leddy JJ, Baldwin BA. The role of the cervical spine in post-concussion syndrome. Physician Sportsmed. 2015;43(3):274–284. doi: 10.1080/00913847.2015.1064301. [DOI] [PubMed] [Google Scholar]
- 15.Sizer J, Phelps V, Brismee JM. Diagnosis and management of cervicogenic headache and local cervical syndrome with multiple pain generators. J Man Manip Ther. 2002;10:136–152. [Google Scholar]
- 16.Vincent MB. Headache and neck. Curr Pain Headache Rep. 2011;15:324–331. doi: 10.1007/s11916-011-0195-1. [DOI] [PubMed] [Google Scholar]
- 17.Ruhe A, Fejer R, Walker B. Altered postural sway in patients suffering from non-specific neck pain and whiplash associated disorder—a systematic review of the literature. Chiropr Man Therap. 2011;19:13. doi: 10.1186/2045-709X-19-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silva AG, Cruz AL. Standing balance in patients with whiplash associated neck pain and idiopathic neck pain when compared with asymptomatic participants: a systematic review. Physiother Theory Pract. 2012;29:1–18. doi: 10.3109/09593985.2012.677111. [DOI] [PubMed] [Google Scholar]
- 19.Kristjansson E, Treleaven J. Sensorimotor function and dizziness in neck pain: implications for assessment and management. J Orthop Sports Phys Ther. 2009;39:364–377. doi: 10.2519/jospt.2009.2834. [DOI] [PubMed] [Google Scholar]
- 20.Treleaven J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control. Man Ther. 2008;13:2–11. doi: 10.1016/j.math.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Spitzer WO, Skovron ML, Salmi LR. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining whiplash and its management. Spine. 1995;20:1S–73S. [PubMed] [Google Scholar]
- 22.Gimse R, Björgen IA, Tjell C, Tyssedal JSL, Bø K. Reduced cognitive functions in a group of whiplash patients with demonstrated disturbances in the posture control system. J Clin Exp Neuropsychol. 1997;19:838–849. doi: 10.1080/01688639708403764. [DOI] [PubMed] [Google Scholar]
- 23.Haldorsen T, Waterloo K, Dahl A, Mellgren SI, Davidsen PE, Molin PK. Symptoms and cognitive dysfunction in patients with the late whiplash syndrome. Appl Neuropsychol. 2003;10:170–175. doi: 10.1207/S15324826AN1003_06. [DOI] [PubMed] [Google Scholar]
- 24.Hynes LM, Dickey JP. Is there a relationship between whiplashassociated disorders and concussion in hockey? A preliminary study. Brain Inj. 2006;20:179–188. doi: 10.1080/02699050500443707. [DOI] [PubMed] [Google Scholar]
- 25.Treleaven J, Jull G, Atkinson L. Cervical musculoskeletal dysfunction in post-concussional headache. Cephalalgia. 1994;14:273–357. doi: 10.1046/j.1468-2982.1994.1404273.x. [DOI] [PubMed] [Google Scholar]
- 26.Schneider KJ, Meeuwisse WH, Kang J, Schneider GM, Emery CA. Preseason reports of neck pain, dizziness, and headache as risk factors for concussion in male youth ice hockey players. Clin J Sport Med. 2013;23:267–272. doi: 10.1097/JSM.0b013e318281f09f. [DOI] [PubMed] [Google Scholar]
- 27.Henry LC, Elbin RJ, Collins MW, Marchetti G, Kontos AP. Examining recovery trajectories after sport-related concussion with a multimodal clinical assessment approach. Neurosurgery. 2016;78:232–241. doi: 10.1227/NEU.0000000000001041. [DOI] [PMC free article] [PubMed] [Google Scholar]