Highlights
-
•
A Conservative treatment of hepatic portal venous gas is described.
-
•
The literature showed only one clinical trial establishing a scoring system.
-
•
A pneumoportogram (hepatic portal venous gas) is a very rare and from poor prognosis.
Keywords: Pneumoportogram, Hepatic portal venous gas (HPVG), Sigmoid diverticulitis, Case report
Abstract
Introduction and presentation of case
Eight days after being diagnosed with multiple small strokes a 71 year old male patient is readmitted with suspicion of a petit mal seizure also complained of diarrhoea and abdominal pain. The patient was stable, not febrile and neurologically intact with a slight tenderness in the left lower quadrant. An ultrasound revealed presence of air in the hepatic portal venous system and a suspicion for sigmoid diverticulitis. A CT-scan confirmed both diagnoses. We proceeded with a conservative regimen under close observation. The clinical course and laboratory results were unremarkable.
Discussion
The review of the literature (PubMed database) triggered 685 items with only one clinical trial establishing a scoring system to detect adult individuals, which need operation.
Conclusion
A pneumoportogram (hepatic portal venous gas, HPVG) is a very rare and usually associated with bowel ischemia and from poor prognosis. The last decades saw the emergence of numerous other aetiologies (also benign) with a shift of paradigm from systematic emergency laparotomies to individual patient selection.
1. Introduction and case presentation
Eight days after being diagnosed with multiple small strokes a 71 year old male patient is readmitted with suspicion of a petit mal seizure. He also complained of diarrhoea and abdominal pain. The patient was hemodynamically stable (HR 66/min, BP 114/71 mmHg), not febrile (36.2 °C), the neurological examination revealed no further symptoms compared with the examination eight days ago. The abdominal examination showed slight tenderness with no guarding in the left lower quadrant.
A follow-up cranial CT-scan showed no further ischemia or bleeding.
The laboratory data presented a normal WBC count of 5.3G/l, a CRP level of 93.5 mg/l with elevated GGT 80 U/l and a normal blood urea nitrogen (BUN).
ECG outcome was a first grade block (PQ 208 ms) and the chest X-ray was unremarkable.
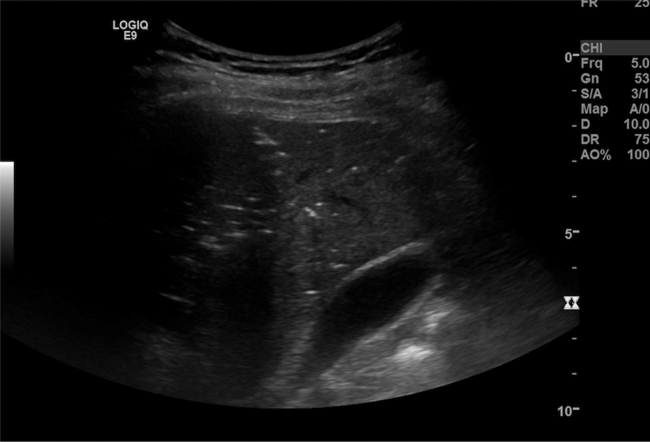
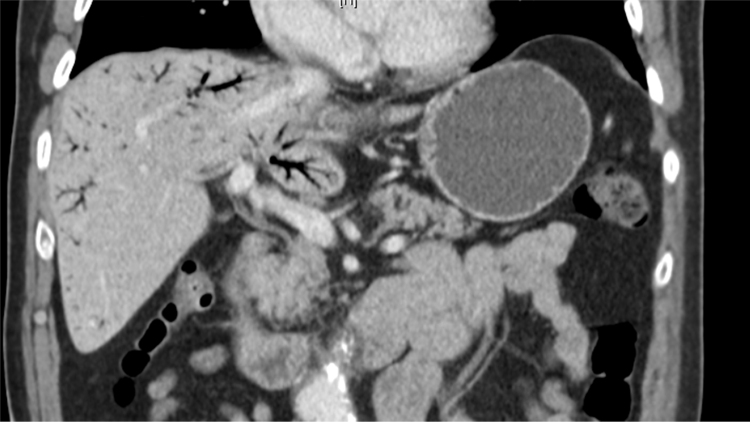
An ultrasound of the abdomen revealed the presence of massive air in the hepatic portal venous system (Image 1 ) and a suspicion for sigmoid diverticulitis. These findings were confirmed by a subsequent CT scan (Image 2 and 3 ). The sigmoid diverticulitis was staged as a covered perforation without abscess formation (IIb according to Hansen and Stock).
Image 1.
sonography with suspicion of HPVG.
Image 2 and 3.
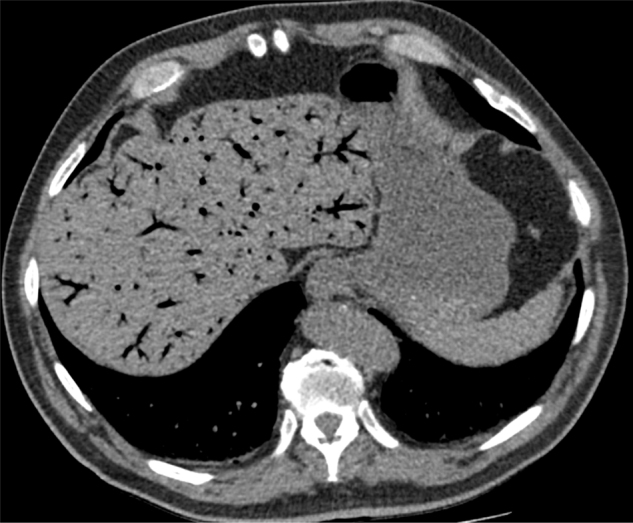
Pneumoportogram in the CT-scan.
We treated the patient with iv Piperacillin/Tazobactam (3 × 4.5 g/d) and fluid intake. To rule out a seizure an EEG was performed and showed no epileptical activity but without certain exclusion of a petit mal event.
Due to findings consistent with complicated but mild diverticulitis (no septic findings, no signs of a gangrenous process within the sigmoid colon) and the patients comorbidities we proceeded with the conservative regimen under close observation. After 48 h the patient was allowed on solid food with consecutive return to a light diet. The clinical course and laboratory results were unremarkable with a decline of the CRP and 8 days after admission the patient was discharged. The antibiotic therapy was changed to Amoxicillin and Clavulanic acid po for a total of 21 days since the onset of antibiotics. To rule out a secondary liver abscess or a portal venous thrombosis a CT scan was planned after 2 months or immediately in worsening conditions.
To rule out malignancy a colonoscopy was performed 6 weeks after discharge. The subsequent CT-scan revealed no signs of hepatic abscess formation and a resolved diverticulitis.
2. Review of the literature
The utilized search string was ‘portal venous gas’ and was exerted on PubMed database. In total it triggered 685 items. The results were limited to adult patients and clinical settings.
Besides retrospective review of HPVG or pneumatosis intestinalis or both to establish clinical algorithms based on clinical, labarotory and radiographic findings [1] there was only one multicenter clinical trial to detect risk factors for colic ischemia or necrosis if CT findings of pneumatosis intestinalis and portal venous gas were given [2]. Further 35 case reports and reviews were available.
3. Discussion
A pneumoportogram is described as the presence of air in the hepatic portal venous system (hepatic portal venous gas, HPVG), typically at the periphery of the liver in contrast to an aerobilie [3] and was first described in 1955 by Wolfe and Evans [4]. HPVG is a rare condition and can be associated with an overall mortality rate up to 40% [5] coming down from 75% as observed in a literature survey in 1978 [6]. Aetiologies are in most cases an ischemic bowel necrosis (43%), peritonitis or abscess (11%) as may be present in the case of a diverticulitis [7], [8], [9], [10]. The mortality risk is highest, if HPVG is present in combination with necrotic bowel (>50%) [6].
Though the presence of HPVG was formerly considered a mandatory indication for urgent exploratory laparotomy since the late 70s and early 80s cases of HPVG without ischemic necrosis were reported and the question arose, if it is still an indication for surgery or if there may be benign courses [2]. The increase of nonfatal and nonsurgical reported conditions associated with HPVG is on the one hand due to the increasing number of CT-scans as diagnostic tool and not any more on left lateral decubitus plain films [4], [11], [12], [13]. On the other hand sensitivity of gas detection in CT is much higher as with conventional X-ray [14], [15]. Thus maybe contributing as a bias to the decreasing mortality rate in contrast to a more restricted indication for surgery as outlined underneath.
Obviously the question of surgery indication would be complicated and probably impossible to be answered by randomized controlled trials. In absence of a larger cohort study parsing out implications of HPVG in series of laparotomies for abdominal catastrophe, remain only case reports and case series to make a therapeutic decision.
According to the fact that the presence of HPVG on CT could be associated with a range of non-surgical pathologies (Table 1), it’s sole presence does not mandate surgical exploration and has no prooven predictive power. Surgical intervention in all HPVG cases would result in approximately 30% non-therapeutic laparotomies [2], [6], [10].
Table 1.
summarizes various reasons for HPVG.
| Reason | Author |
|---|---|
| Diverticulitis | Haak et al. [7] |
| Sellner et al. (2007) [19] | |
| Ileus | Quirke (1995) [20] |
| Chemotherapy/Enterocolitis | Tan et al. (2015) [21] |
| Kanagushi et al. (2014) [22] | |
| Tubo-ovarian abscess | Onyeabor et al. (2015) [23] |
| Colonoscopy | Shinagawa et al. (2015) [24] |
| Viral gastroenteritis | Mirmanesh et al. (2013) [25] |
| Crohn’ s disease | Kirsch et al. (1990) [26] |
| Incarcerated diaphragmatic hernia | Mittal et al. (2015) [27] |
| Gastroduodenal ulcer | Choi et al. (2014) [28] |
| Blunt abdominal trauma | Vauthey et al. (1992) [29] |
| Bickerstaff’ s encephalitis | Slawinski et al. (2015) [30] |
| Cocaine-induced intestinal ischemia | Patel et al. (2015) [31] |
| Hydrogen peroxide ingestion | Papafragkou et al.(2012) [32] |
| Acute pancreatitis | Park et al. (2007) [33] |
| Endoscopic retrograde cholangiopancreatography | Hong et al. (1997) [34] |
| Seizure | Chen et al. (1997) [35] |
| Cystic fibrosis | Mallens et al. (1995) [36] |
A current evidence based indication for surgery is bowel ischemia/necrosis with or without mechanical obstruction. The significant risk factors delineated in a consecutive gathering of 88 cases by Wayne et al. to distinguish the patient towards surgery and develop an algorithm are pain, elevated lactate, presence of small bowel PI and calculated vascular disease score. This algorithm is based only on 70 cases of pneumatosis intestinalis and/or HPVG still with a sensitivity of 89%. Once distinguished into a subgroup the specificity and positive predictive value is 100% [2]. The Algorithm was tested only on a limited number of 14 cases and has to be proven on a larger population.
Keeping in mind that CT-scans alone are not always satisfactory in revealing bowel ischemia [1], [16], [17], [18]. Additional factors like older age, peritoneal signs and high BUN were found to be significantly associated with ischemia or necrosis [1].
If ischemia or necrosis is diagnosed the presence of HPVG has a predictive value since an increasing mortality could be observed [6].
According to the algorithm developed by Wayne et al. [2] our patient had a benign HPVG (score < 4), supporting our conservative treatment approach with a benign course.
4. Conclusion
HPVG is a very rare condition from poor prognosis when associated with bowel ischemia. The last decades saw the emergence of numerous other aetiologies including benign courses and a shift of paradigm from systematic emergency laparotomies to individual patient selection. Revealing bowel necrosis/ischemia is the most important step towards patient selection for surgery. Developed algorithms can aid the decision making as in our case but unfortunately are based on small populations and present a wide variety of variables. Establishing clinical guidelines by using a register would be desireable.
Conflict of interest
We have no conflict of interest and no source of funding to declare.
Funding
No sources of funding to declare.
Ethical approval
According to the Canton Bern (Switzerland) regulation, this manuscript doesn’t require ethical approval.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request (please ask: alexandre.moser@ssvnn.net)
Author contribution
All authors have made significant contribution to the submitted manuscript. Alexandre Moser and Alexander Radke wrote the manuscript and did the literature review. André Wyss wade significantly corrections to the script and was responsible for the radiologist point of view. Claudio Schneider and Anita Stauffer realized the US of he patient and participated at the literature review. Manfred ESSIG shared his expert opinion about this case.
Guarantor
Alexandre MOSER and Alexander RADKE.
References
- 1.Bani Hani M., Kamangar F., Goldberg S., Greenspon J., Shah P., Volpe C. Pneumatosis and portal venous gas: do CT findings reassure? J. Surg. Res. 2013;185(December (2)):581–586. doi: 10.1016/j.jss.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 2.Wayne E., Ough M., Wu A., Liao J., Andresen K.J., Kuehn D. Management algorithm for pneumatosis intestinalis and portal venous gas: treatment and outcome of 88 consecutive cases. J. Gastrointest. Surg. 2010;14(March (3)):437–448. doi: 10.1007/s11605-009-1143-9. [DOI] [PubMed] [Google Scholar]
- 3.Keller M., Epp C., Meyenberger C., Lauber A., Sulz M.C. Wenn gas in die leber kommt. Schweiz. Med. Forum. 2014;14(12):262. [Google Scholar]
- 4.Wolfe J.N., Evans W.A. Gas in the portal veins of the liver in infants; a roentgenographic demonstration with postmortem anatomical correlation. Am. J. Roentgenol. Radium Ther. Nucl. Med. 1955;74(September (3)):486–488. [PubMed] [Google Scholar]
- 5.Kinoshita H., Shinozaki M., Tanimura H., Umemoto Y., Sakaguchi S., Takifuji K. Clinical features and management of hepatic portal venous gas: four case reports and cumulative review of the literature. Arch. Surg. 1960;136(December (12)):1410–1414. doi: 10.1001/archsurg.136.12.1410. [DOI] [PubMed] [Google Scholar]
- 6.Nelson A.L., Millington T.M., Sahani D., Chung R.T., Bauer C., Hertl M. Hepatic portal venous gas: the ABCs of management. Arch. Surg. 1960;144(June (6)):575–581. doi: 10.1001/archsurg.2009.88. (discussion 581) [DOI] [PubMed] [Google Scholar]
- 7.Haak H.R., Kooymans-Coutinho M.F., von Teeffelen M.E., Adhin S., Falke T.H. Portal venous gas in a patient with diverticulitis. Hepatogastroenterology. 1990;37(5):528–529. [PubMed] [Google Scholar]
- 8.Traverso L.W. Is hepatic portal venous gas an indication for exploratory laparotomy? Arch Surg Chic Ill. Arch Surg Chic Ill. 1981;116(July (7)):936–938. doi: 10.1001/archsurg.1981.01380190066015. [DOI] [PubMed] [Google Scholar]
- 9.McElvanna K., Campbell A., Diamond T. Hepatic portal venous gas—three non-fatal cases and review of the literature. Ulster Med. J. 2012;81(May (2)):74–78. [PMC free article] [PubMed] [Google Scholar]
- 10.Iannitti D.A., Gregg S.C., Mayo-Smith W.W., Tomolonis R.J., Cioffi W.G., Pricolo V.E. Portal venous gas detected by computed tomography: is surgery imperative? Dig. Surg. 2003;20(4):306–315. doi: 10.1159/000071756. [DOI] [PubMed] [Google Scholar]
- 11.Liebman P.R., Patten M.T., Manny J., Benfield J.R., Hechtman H.B. Hepatic–portal venous gas in adults: etiology, pathophysiology and clinical significance. Ann. Surg. 1978;187(March (3)):281–287. doi: 10.1097/00000658-197803000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berne T.V., Meyers H.I., Donovan A.J. Gas in the portal vein of adults with necrotizing enteropathy. Am. J. Surg. 1970;120(August (2)):203–209. doi: 10.1016/s0002-9610(70)80112-x. [DOI] [PubMed] [Google Scholar]
- 13.Susman N., Senturia H.R. Gas embolization of the portal venous system. Am. J. Roentgenol. Radium Ther. Nucl. Med. 1960;83(May):847–850. [PubMed] [Google Scholar]
- 14.Earls J.P., Dachman A.H., Colon E., Garrett M.G., Molloy M. Prevalence and duration of postoperative pneumoperitoneum: sensitivity of CT vs left lateral decubitus radiography. AJR Am. J. Roentgenol. 1993;161(4):781–785. doi: 10.2214/ajr.161.4.8372757. [DOI] [PubMed] [Google Scholar]
- 15.Schulze C.G., Blum U., Haag K. Hepatic portal venous gas. Imaging modalities and clinical significance. Acta Radiol Stockh Swed. 1987;36(July (4)):377–380. [PubMed] [Google Scholar]
- 16.Shah P.A., Cunningham S.C., Morgan T.A., Daly B.D. Hepatic gas: widening spectrum of causes detected at CT and US in the interventional era. Radiogr. Rev. Publ. Radiol. Soc. N. Am. Inc. 2011;31(5):1403–1413. doi: 10.1148/rg.315095108. [DOI] [PubMed] [Google Scholar]
- 17.Hou S.-K., Chern C.-H., How C.-K., Chen J.-D., Wang L.-M., Lee C.-H. Hepatic portal venous gas: clinical significance of computed tomography findings. Am. J. Emerg. Med. 2004;22(May (3)):214–218. doi: 10.1016/j.ajem.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 18.Sebastià C., Quiroga S., Espin E., Boyé R., Alvarez-Castells A., Armengol M. Portomesenteric vein gas: pathologic mechanisms, CT findings, and prognosis. Radiogr. Rev. Publ. Radiol. Soc. N. Am. Inc. 2000;20(October (5)) doi: 10.1148/radiographics.20.5.g00se011213. (1213–1224–1226) [DOI] [PubMed] [Google Scholar]
- 19.Sellner F., Sobhian B., Baur M., Sellner S., Horvath B., Mostegel M. Intermittent hepatic portal vein gas complicating diverticulitis—a case report and literature review. Int. J. Colorectal. Dis. 2007;22(November (11)):1395–1399. doi: 10.1007/s00384-007-0346-3. [DOI] [PubMed] [Google Scholar]
- 20.Quirke T.E. Hepatic-portal venous gas associated with ileus. Am. Surg. 1995;61(December (12)):1084–1086. [PubMed] [Google Scholar]
- 21.Tan E.W., Smith M.D. A rare occurrence of hepatic portal venous gas in a patient with chemotherapy-induced enterocolitis: the rise of benign aetiologies. J. Surg. Case Rep. 2015;2015:9. doi: 10.1093/jscr/rjv114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kanagushi Y., Fujita T., Hanaoka J., Hayashi H. A case of hepatic portal venous gas in a patient treated with pemetrexed and carboplatin for lung cancer. Chemotherapy. 2014;60(2):88–90. doi: 10.1159/000371440. [DOI] [PubMed] [Google Scholar]
- 23.Onyeabor S., Cason F. Chronic tubo-ovarian abscess complicated by hepatic portal venous gas. J. Surg. Case Rep. 2015;2015:9. doi: 10.1093/jscr/rjv099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shinagawa T., Hata K., Watanabe T. Hepatic portal venous gas after colonoscopy for ulcerative colitis: a case report. J. Crohns. Colitis. 2015 doi: 10.1093/ecco-jcc/jjv125. [DOI] [PubMed] [Google Scholar]
- 25.Mirmanesh M., Nguyen Q.-S., Markelov A. A case of hepatic portal venous gas due to viral gastroenteritis. Hepatic Med. 2013;5:63–65. doi: 10.2147/HMER.S53241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kirsch M., Bozdech J., Gardner D.A. Hepatic portal venous gas: an unusual presentation of Crohn’s disease. Am. J. Gastroenterol. 1990;85(November (11)):1521–1523. [PubMed] [Google Scholar]
- 27.Mittal K., Anandpara K., Dey A.K., Kedar P., Hira P., Kale S. Left aberrant gastric vein causing isolated left hepatic portal venous gas secondary to an incarcerated diaphragmatic hernia. Pol. J. Radiol. Pol. Med. Soc. Radiol. 2015;80:364–367. doi: 10.12659/PJR.894103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Choi Y.J., Moon W., Park S.J., Park M.I., Kim S.E. Hepatic portal venous gas associated with hemorrhagic gastroduodenal ulcers. Turk. J. Gastroenterol. 2014;25(Suppl. 1):237–238. doi: 10.5152/tjg.2014.6289. [DOI] [PubMed] [Google Scholar]
- 29.Vauthey J., Matthews C. Hepatic portal venous gas identified by computed tomography in a patient with blunt abdominal trauma: a case report. J. Trauma. 1992;32(1):120. [PubMed] [Google Scholar]
- 30.Slawinski C., Parkin E., Casey P., Pettit S. Hepatic portal venous gas complicating Bickerstaff’s encephalitis with Guillain Barré overlap. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2015-211514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel H., Shaaban H., Shah N., Baddoura W. A rare case report of spontaneous resolution of hepatic portal venous gas associated with cocaine-induced intestinal ischemia. Ann. Med. Health Sci. Res. 2015;5(2):136–138. doi: 10.4103/2141-9248.153627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Papafragkou S., Gasparyan A., Batista R., Scott P. Treatment of portal venous gas embolism with hyperbaric oxygen after accidental ingestion of hydrogen peroxide: a case report and review of the literature. J. Emerg. Med. 2012;43(1):e21–e23. doi: 10.1016/j.jemermed.2009.07.043. [DOI] [PubMed] [Google Scholar]
- 33.Park H.C., Lee W.S., Joo S.Y., Park S.Y., Joo Y.E., Kim H.S. Hepatic portal venous gas associated with acute pancreatitis: reports of two cases and review of literature. Korean J. Gastroenterol. 2007;50(2):131–135. [PubMed] [Google Scholar]
- 34.Hong J.J., Gadaleta D., Rossi P., Esquivel J., Davis J.M. Portal vein gas, a changing clinical entity. Report of 7 patients and review of the literature. Arch. Surg. 1997;132(10):1071–1075. doi: 10.1001/archsurg.1997.01430340025003. [DOI] [PubMed] [Google Scholar]
- 35.Chen K.W., Shin J.S., Chi C.H., Cheng L. Seizure: a rare and transient cause of portal venous gas. Am. J. Gastroenterol. 1997;92(2):351–352. [PubMed] [Google Scholar]
- 36.Mallens W.M., Schepers-Bok R., Nicolai J.J., Jacobs F.A., Heyerman H.G. Portal and systemic venous gas in a patient with cystic fibrosis: CT findings. AJR Am. J. Roentgenol. 1995;165(2):338–339. doi: 10.2214/ajr.165.2.7618551. [DOI] [PubMed] [Google Scholar]