Pulmonary arteriovenous malformations (AVM) lung is defined by an abnormal communication between pulmonary artery(ies) and vein(s) responsible for a right-left shunt. Congenital forms are most common and usually associated with Rendu-Osler disease (ROD). Inversely, 15–45% of patients with ROD present lung AVM.[1] Nowadays, embolization is preferred to surgical resection in the majority of cases. Except for certain cases where surgery is indicated. This paper shows the role of surgery in AVMs.
A 29-year-old man, with a medical history of nose bleeding since the age of ten, showed up at our service for the management of pulmonary AVMs that was discovered after he had been operated for cerebral abscesses. Clinical examination found a labial and upper extremities cyanosis, digital clubbing, and dyspnea without murmurs on auscultation. Chest X-ray showed a homogenous parenchymal right mid thoracic rounded opacity. A three-dimensional chest computed tomography (CT) angiography with vascular reconstruction presented four AVM in the right lung with three located in the lower lobe and one in middle lobe: The largest AVM [Figure 1] was located in the apical segment of the lower lobe. It was supplied by an afferent artery measuring 8.4 mm in diameter and a large vein of 11 mm draining an aneurysm of 38 mm in diameter. Second, AVM still in the apical segment of the lower lobe was smaller measuring 9 mm. It was supplied by an afferent artery and an efferent vein of 3 mm in diameter [Figure 2]. The third AVM located on the posterobasal segment of the lower lobe and measuring 16 mm. It was supplied by an afferent artery and an efferent vein measuring 6 and 7 mm in diameters, respectively [Figure 2]. Fourth, AVM was located on the anterior border of the middle lobe was small.
Figure 1.
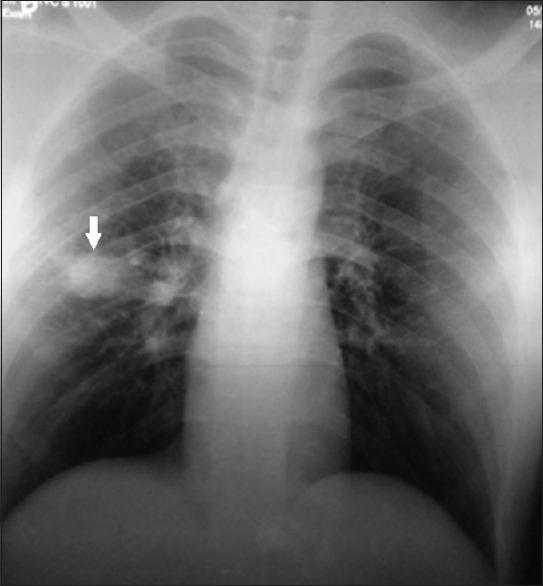
Chest X-ray showing a rounded homogenous parenchymal opacity in the right mid lung (arrow).
Figure 2.
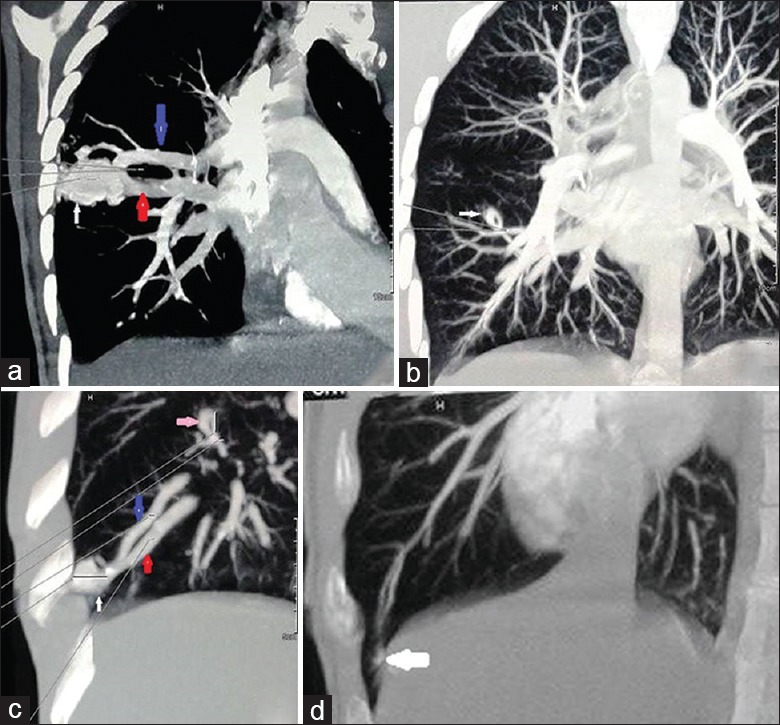
Pulmonary angioscan showing the right arteriovenous malformation, (a) coronal section showing a voluminous arteriovenous malformation in inferior lobe formed by an afferent artery (blue arrow), an efferent vein (red arrow), and an aneurysmal sac (white arrow); (b) maximum intensity projection reformation of second arteriovenous malformation in lower lobe (white arrow); (c) third arteriovenous malformation in inferior lobe on maximum intensity projection reformation with the aneurysmal sac (white arrow), the feeding artery (blue arrow), and draining vein (red arrow). Second arteriovenous malformation (pink arrow), (d) fourth arteriovenous malformation on the anterior border of the middle lobe on maximum intensity projection reformation (white arrow).
Brain and abdominopelvic CT scans did not show any other AVM. Other work-up examinations showed hypoxemia of 51 mmHg (1mmHg=0.133kPa) and 86% oxygen saturation without polycythemia. Heart ultrasound showed no pulmonary hypertension. The patient was discussed in the institute multidisciplinary thoracic team. Surgery was indicated because: (1) these pulmonary AVMs, complicated to cerebral abscesses, and was symptomatic (dyspnea, cyanosis, clubbing, and hypoxemia); (2) a unilateral site; (3) The three AVMs were located in one lobe and the fourth on the frontal border of the middle lobe; (4) The unavailability of a specialized center for embolization. The surgical approach was a right conservative posterolateral thoracotomy. After a proximal control of the right pulmonary trunk artery, a right lower lobectomy associated with a wedge resection of the middle lobe lung permitted the resection of all four AVMs. Antibiotic prophylaxis and anticoagulation were given before during and after surgery. Postoperative gasometry was satisfactory with the partial pressure of oxygen in arterial blood of 94 mmHg, an oxygen saturation of 97.7% with the disappearance of cyanosis and dyspnea.
Pulmonary AVMs are rare entities. Their incidence varies between 3 and 5 cases per 100,000 inhabitants with a female predominance (male:female ratio 1:2).[2] They can be revealed by its complications as ischemic stroke or brain abscess. The diagnosis of ROD was retained in our patient following the Curacao criteria. An enhanced helical chest CT is the gold standard for diagnosis. It enabled the diagnosis in our patient and determined the appropriate therapeutic approach. Its sensitivity is higher (98% vs. 60%) than conventional pulmonary angiography.[2] The treatment of choice for pulmonary AVM is by embolization coiling.[3] It is usually practiced by experienced operators in specialized centers. Several coiling is sometimes necessary, and when the pulmonary AVMs is multipedicular or diffuse, embolization becomes more difficult to handle technically, and the result becomes less durable.[2,3] Antibiotic prophylaxis for infective endocarditis is that recommended in pulmonary AVMs. It is indicated in cases of embolization, dental, or surgical procedures to reduce the risk of paradoxical emboli and brain abscess.[4] Surgical treatment consists of a conservative parenchymal resection. Vascular ligation, wedge resections, segmentectomies, lobectomies, or even pneumonectomies were described. It is indicated in cases of pulmonary AVM with a high risk of embolization failure or with centrally located or large AVMs. Lung transplantation has been indicated in diffuse AVMs associated with respiratory failure.[5] The classic approach is a conservative posterolateral thoracotomy [Figure 3]. Several arguments motivated the surgical treatment in our patient:
Figure 3.
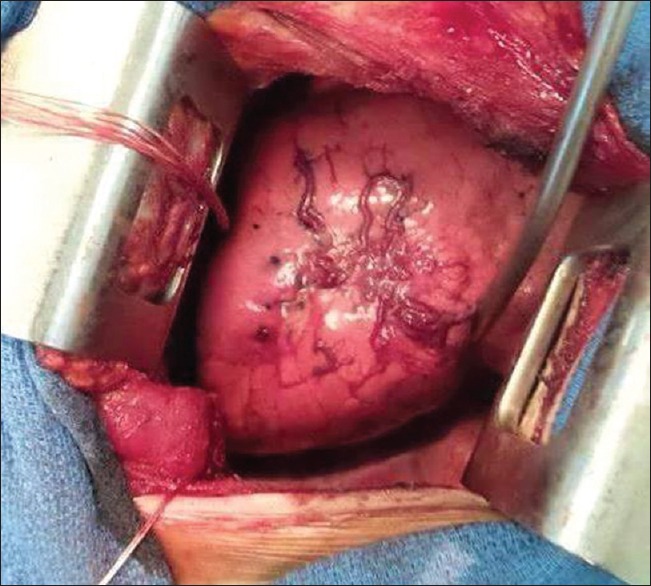
Operative view of the aneurysmal sac of large arteriovenous malformations in the inferior lobe of right lung (the left of the figure: To the patient's head).
The brain abscesses were due to a septic paradoxical emboli originating from the pulmonary AVM.
The localized unilateral nature of AVMs rendering limited surgical resections a better success.
A large pulmonary AVM (aneurysms measuring 16 and 38 mm, afferent artery of 8.4 mm in diameter). In fact, the risk of recanalization after embolization (8%) is high when the afferent artery is large (at least 8 mm diameter) and some authors recommend surgery for localized pulmonary AVM measuring at least 2 cm in diameter.[2,5]
And finally, the absence of a center specialized in interventional radiology in our country.
Thus, surgical treatment is an alternative management in symptomatic patients or in cases of complications when lung AVMs are localized, unilateral, without increased operative risk.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Yi Cui
REFERENCES
- 1.Faughnan ME, Granton JT, Young LH. The pulmonary vascular complications of hereditary haemorrhagic telangiectasia. Eur Respir J. 2009;33:1186–94. doi: 10.1183/09031936.00061308. doi: 10.1183/09031936.00061308. [DOI] [PubMed] [Google Scholar]
- 2.Blivet S, Lacombe P, Chinet T. Pulmonary arteriovenous malformations. Rev Mal Respir Actual. 2011;3:S61–6. doi: 10.1016/S1877-1203 (11) 70035-0. [Google Scholar]
- 3.Cottin V, Blanchet AS, Cordier JF. Pulmonary manifestations of hereditary hemorrhagic telangiectasia. Rev Mal Respir. 2006;23:4S53–66. doi: 10.1019/200530231. [PubMed] [Google Scholar]
- 4.Lacombe P, Lacout A, Marcy PY, Binsse S, Sellier J, Bensalah M, et al. Diagnosis and treatment of pulmonary arteriovenous malformations in hereditary hemorrhagic telangiectasia: An overview. Diagn Interv Imaging. 2013;94:835–48. doi: 10.1016/j.diii.2013.03.014. doi: 10.1016/j.diii.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 5.Georghiou GP, Berman M, Vidne BA, Saute M. Pulmonary arteriovenous malformation treated by lobectomy. Eur J Cardiothorac Surg. 2003;24:328–30. doi: 10.1016/s1010-7940(03)00249-5. doi: 10.1016/S1010-7940(03)00249-5. [DOI] [PubMed] [Google Scholar]


