Melioidosis is an endemic communicable disease caused by Burkholderia pseudomallei and a prevalent amphixenosis in tropical and subtropical regions. The main routes of infection are thought to be through compromised surface tissues and through inhalation of contaminated soil and water. B. pseudomallei can affect all organs, but pulmonary infection is the most common symptom, which could easily lead to sepsis.[1] Here, we reported what we believe is a rare case of acute pericarditis caused by B. pseudomallei infection.
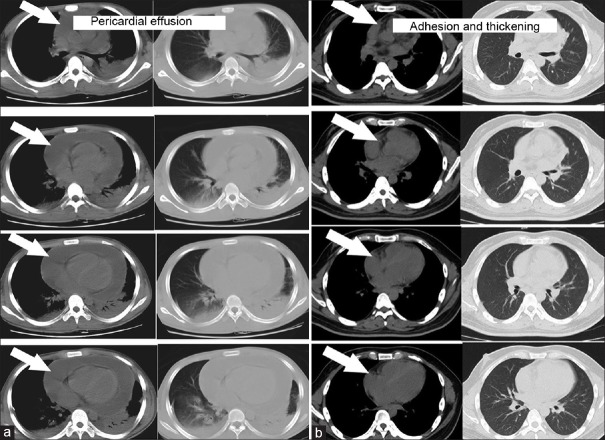
A 15-year-old male resident within a rural area in Dongfang County of Hainan Province in China was admitted on April 30, 2014, complaining of chills, fever lasting for more than 10 days, and difficulty in breathing due to chest congestion. The patient reported walking several times through a pond created by a typhoon 1 week prior in his residential area and had not particular medical history. Physical examination results at the time of admission showed a body temperature of 37.8°C, tachypnea, bilateral jugular venous engorgement, weak bilateral lower lung respiratory sounds without dry or moist rales, a laterally extended heart border, a heart rate of 122 beats/min with regular rhythm, and distant heart sounds, but without pathologic murmur in the auscultatory valve areas. A computed tomography (CT) scan revealed massive pericardial effusion and few bilateral pleural effusions [Figure 1a]. Routine blood test results showed a total leukocyte count of 9,900/mm3 with 81% neutrophils, C-reactive protein (CRP) of 168.78 mg/L, erythrocyte sedimentation rate of 46 mm/h, and procalcitonin (PCT) of 1.2 ng/ml. Since the patient presented with acute pericardial tamponade, an intrapericardial drainage tube was immediately inserted with the aid of ultrasound guidance, which resulted in an outflow of slightly yellowish and turbid pericardial fluid. Bilateral pleural effusion drainage was performed at the same time and an outflow of clear yellow fluid was seen. Pericardial effusion examination results showed a positive Rivalta test, protein concentration of 49 g/L, white blood cell (WBC) count of 6,400 × 106/L with 78% mononuclear leukocytes and 22% multinuclear leukocytes, and adenosine deaminase (ADA) level of 84 U/L. Pleural effusion examination results showed a negative Rivalta test, protein concentration of 25.8 g/L, 35% mononuclear leukocytes and 65% multinuclear leukocytes, and ADA level of 4 U/L. A preliminary diagnosis of tuberculous pericarditis and cardiac tamponade was made, and the patient was administered an antitubercular treatment consisting of isoniazid, rifampicin, pyrazinamide, and ethambutol, in addition to oral prednisone. However, the patient was still febrile and there was still a continuous outflow of slightly yellowish fluid from the pericardium. Reexamination of routine blood tests revealed that the patient's WBC count had increased to 18.3 × 109/L with 83% neutrophils. Blood and pericardial drainage fluid cultures were carried out over several days until a growth of B. pseudomallei was observed in the pericardial drainage fluid on day 13 while blood cultures were negative. Antitubercular treatment was stopped and an anti-infective combination therapy of ceftazidime and compound sulfamethoxazole was administered. The patient's body temperature gradually normalized after 3 days, and routine blood tests conducted 1 week later showed a WBC count of 8.4 × 109/L with 77% neutrophils, a CRP level of 38 mg/L, and a PCT level of 0.22 ng/ml. Ultrasonography imaging 1 month later indicated an adhesion of the left ventricular free wall with the visceral and parietal pericardium at the apex. The patient was discharged and oral administration of compound sulfamethoxazole was continued as maintenance treatment. Adhesion and thickening in the pericardium were found in 2 months after hospital discharge [Figure 1b], and the patient often complained about mild shortness of breath when activity.
Figure 1.
Computed tomography scan images:(a)before treatment, and (b) at follow-up.
The clinical manifestations associated with melioidosis are diverse and can present as acute, chronic, and latent disease. It is difficult to distinguish melioidosis from tuberculosis when considering the physical signs and symptoms, and chest radiological tests. Patients presenting with risk factors, such as diabetes mellitus, or who are taking steroid therapy, are predisposed to both bacterial diseases. Histological examination of tissue taken from patients with melioidosis might reveal granulomas with central necrosis, which is also found in cases of tuberculosis. B. pseudomallei and Mycobacterium tuberculosis are both intracellular pathogens. The main host response to intracellular pathogens is mediated by cellular immune responses through activated lymphocytes and interferon-mediated signaling pathways.[2] In the present case, the continuous increase in ADA levels in the pericardial fluid resulted in an initial misdiagnosis. It has been reported that the ADA value is > 25 U/L in tuberculous exudates with 89.66% sensitivity and 91.01% specificity.[3] The measurement of ADA is an important auxiliary method that might serve as a crucial diagnostic test of tuberculous exudates in the absence of direct evidence of infection because ADA is an enzyme biomarker indicating the activation status of the cellular immune response.[4] There is a great deal of confusion in the diagnosis of melioidosis and tuberculosis due to the similar presentation of the infections.
The patient in this case report was a resident of a rural area and, therefore, was more likely to be exposed to contaminated soil and water. Moreover, the patient was infected during the summer typhoon season, when the soil that might breed bacteria was washed by rainwater, leading to contamination of water sources. Melioidosis probably resulted from infection through compromised surface tissues by B. pseudomallei or through the inhalation of aerosol into the lungs. Pathogen invasion of the lungs might induce pneumonia and pulmonary cavity, causing the rapid development of sepsis. Although B. pseudomallei infection can cause abscesses at unusual sites such as brain, liver, and spleen, infective pericarditis is extremely rare. The pathogen might spread directly from the lungs or from the bloodstream and infect the pericardium, the route of infection in this case is a possible, but not definite. The current report indicates that the possibility of B. pseudomallei infection should not be excluded when considering a diagnosis of tuberculosis in patients living in melioidosis endemic areas. A delay in treatment would probably affect prognosis as discussed in this case where adhesion and thickening in the pericardium were found.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Peng Lyu
REFERENCES
- 1.Cheng AC, Currie BJ, Dance DA, Funnell SG, Limmathurotsakul D, Simpson AJ, et al. Clinical definitions of melioidosis. Am J Trop Med Hyg. 2013;88:411–3. doi: 10.4269/ajtmh.12-0555. doi: 10.4269/ajtmh.12-0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koh GC, Schreiber MF, Bautista R, Maude RR, Dunachie S, Limmathurotsakul D, et al. Host responses to melioidosis and tuberculosis are both dominated by interferon-mediated signaling. PLoS One. 2013;8:e54961. doi: 10.1371/journal.pone.0054961. doi: 10.1371/journal.pone.0054961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barrios Barreto D, Rodriquez EP, Gotera C, Meneses PL, Narvaez PA, Mirambeaux Villalona R, et al. Lymphocytic pleural effusion and change of the adenosine deaminase cut-off level in tuberculosis diagnosis. Chest. 2014;145:274A. doi: 10.1378/chest.1821853. [Google Scholar]
- 4.Arroyo M, Soberman JE. Adenosine deaminase in the diagnosis of tuberculous pericardial effusion. Am J Med Sci. 2008;335:227–9. doi: 10.1097/MAJ.0b013e3180cab71a. doi: 10.1097/MAJ.0b013e3180cab71a. [DOI] [PubMed] [Google Scholar]