Abstract
Objective
Youth in war-affected regions are at risk for poor psychological, social, and educational outcomes. Effective interventions are needed to improve mental health, social behavior, and school functioning. This randomized controlled trial tested the effectiveness of a 10-session cognitive-behavioral therapy (CBT)–based group mental health intervention for multisymptomatic war-affected youth (aged 15–24 years) in Sierra Leone.
Method
War-affected youth identified by elevated distress and impairment via community screening were randomized (stratified by sex and age) to the Youth Readiness Intervention (YRI) (n = 222) or to a control condition (n = 214). After treatment, youth were again randomized and offered an education subsidy immediately (n = 220) or waitlisted (n = 216). Emotion regulation, psychological distress, prosocial attitudes/behaviors, social support, functional impairment, and posttraumatic stress disorder (PTSD) symptoms were assessed at pre- and postintervention and at 6-month follow-up. For youth in school, enrollment, attendance, and classroom performance were assessed after 8 months. Linear mixed-effects regressions evaluated outcomes.
Results
The YRI showed significant postintervention effects on emotion regulation, prosocial attitudes/behaviors, social support, and reduced functional impairment, and significant follow-up effects on school enrollment, school attendance, and classroom behavior. In contrast, education subsidy was associated with better attendance but had no effect on mental health or functioning, school retention, or classroom behavior. Interactions between education subsidy and YRI were not significant.
Conclusion
YRI produced acute improvements in mental health and functioning as well as longer-term effects on school engagement and behavior, suggesting potential to prepare war-affected youth for educational and other opportunities. Clinical trial registration information-Trial of the Youth Readiness Intervention (YRI); http://clinicaltrials.gov; NCT01684488.
Keywords: youth, intervention, mental health, war-affected, randomized controlled trial
The mental health consequences of war are well documented.1 Both the direct effects of witnessing and participating in violent acts2 and the indirect effects of war on community and family structures can be devastating to young people.3 In children, adolescents, and youth, violence exposure and loss are associated with psychological distress in the form of depression and anxiety (internalizing problems), including posttraumatic stress reactions, which may also manifest as anger problems (externalizing), difficulties with anger/emotional regulation,4 interpersonal deficits, and impairments in daily functioning.5 Although interventions in war-affected groups may target singular conditions such as posttraumatic stress disorder (PTSD)6 or depression,7 few cost-effective transdiagnostic interventions exist to address multisymptomatic presentations that can cause major impairments in school and community functioning. In addition, given limited human resources for mental health, brief and effective skills and stabilization-focused interventions are needed to improve comorbid symptoms and functioning and help youth to connect with life opportunities such as education and employment programs. Failure to address the mental health consequences of war can perpetuate cycles of violence and lost human capital.8
Sierra Leone’s 11-year civil war (1991–2002), notorious for the involvement of child soldiers, devastated the nation’s infrastructure and economy. An estimated 50,000 persons were killed, and more than 20,000 children and adolescents were involved with armed groups.9 Youth—both combatants and civilians—were exposed to high levels of violence and loss.10 After the conflict, access to mental health services has remained limited.11
Longitudinal research on war-affected youth in the region demonstrates high levels of comorbid mental health problems,10 suggesting a need for trauma-informed, broad-based interventions. For survivors of repeated violence, loss, and trauma exposure in childhood, models of complex trauma have been useful for explaining the constellation of anger problems, interpersonal deficits, and functional impairments that may result. Often, treating complex trauma involves stabilization and coping skills development12 to reduce comorbid symptoms and to improve functioning and emotion regulation.13 Such interventions can be sufficient for reducing symptoms and improving functioning in many young people, even in low-cost, community-based models, and those requiring higher-level mental health care for conditions such as PTSD may then continue on individualized and targeted treatments for persistent symptoms via stepped care models if needed.
Innovative solutions are required to address the post-conflict mental health needs of war-affected children, adolescents, and youth. In Sierra Leone, programs to advance youth employment and educational opportunities (e.g., the World Bank’s $20 million Youth Employment Scheme) may be inaccessible to those whose anger problems or functional impairments complicate interactions with peers and supervisors. Human resource limitations also necessitate broadening the range of health workers who can provide mental health care using task-sharing models14 whereby interventions are delivered by health workers with a basic level of training within a robust training and supervision structure.15,16
After an extensive period of mixed methods research to examine key deficit areas and treatment targets of broad salience in the post-conflict setting,17 we developed a stabilization- and skills-focused group intervention, the Youth Readiness Intervention (YRI), which integrates evidence-based common practice elements from cognitive-behavioral therapy (CBT) and group interpersonal therapy (IPT) to address co-occurring mental health symptoms and functional problems that may impede life success and functioning in war-affected youth.18 The intervention does not use exposure-based trauma processing, given concerns about potential iatrogenic effects and the intensity of such processing in groups facilitated by lay health workers.19,20 Nonetheless, the YRI incorporates trauma psychoeducation and discussion of the impact of trauma on interpersonal relationships and self-concept as a core guiding framework. The trauma-informed focus on comorbid anger, emotion dysregulation, and overall distress (internalizing/externalizing problems and interpersonal and functional impairments, including school functioning) was identified via intervention development research on the mental health of war-affected youth in the region.10,21,22
In testing the effectiveness of the YRI in a randomized controlled trial, we hypothesized that war-affected youth assigned to the YRI (n = 222) would demonstrate greater improvements in emotion regulation, prosocial skills, psychological distress, social support, and daily functioning compared to youth assigned to a control condition (n = 214). In addition, we sought to learn whether a simple education subsidy alone (less complex and labor intensive than the YRI) might be beneficial, and whether such a subsidy might interact with the YRI in its impact. To investigate these questions, we randomly assigned all youth to receive an education subsidy immediately after the YRI intervention period (n = 220) or to be waitlisted (n = 216).
METHOD
Study Sample
Youth were recruited though outreach centers and referrals by workers at youth-serving agencies, religious leaders, and community elders. Inclusion criteria were as follows: age 15 to 24 years (consistent with the UN definition of “youth”); indication of interest to continue education per a series of survey screening questions; psychological distress as indicated by a total score 0.5 standard deviations above total psychological distress levels (combined internalizing and externalizing problem scores) previously documented in longitudinal research on war-affected youth using a measure validated for use in Sierra Leone10; and self-reported impairment in daily functioning. Individuals were excluded and referred for mental health services for active suicidality or psychosis (2 youth referred).
Internal review board approval was obtained from the Harvard School of Public Health and the Sierra Leonean Ministry of Health ethics committee. A local community advisory board, comprising adult caregivers, health care professionals, and youth representatives, advised the research. Given low literacy levels in Sierra Leone, all participants aged 18 years and older provided verbal consent; those younger than 18 years provided verbal assent, and a primary caregiver provided verbal consent.
A randomization sequence generated in STATA 12.0 SE23 was used to assign participants to condition, stratified by sex and age (younger: 15–17 years old; older: 18–24 years old). Randomization occurred after baseline assessment; assessors were blinded to participants’ condition (Figure 1 provides a Consolidated Standards of Reporting [CONSORT] diagram). After the YRI intervention period (during which half of all YRI and control participants were randomly assigned to receive the YRI), youth were randomly assigned to receive access to a free educational opportunity, EducAid, in either Fall 2012 or 2013, stratifying by condition (YRI or control). EducAid is a program run by a British charity that uses an alternative educational style in which students study in small groups and work at their own pace to achieve competency per each grade of the national curriculum. Students then sit for a grade completion examination per the national standard. Although subsidies were offered only at EducAid, we followed up all participants in any educational opportunities that they pursued. After an intention-to-treat approach, all youth participants, including those lost to follow-up during the first phase of the trial, were included in the second step of randomization.
FIGURE 1.
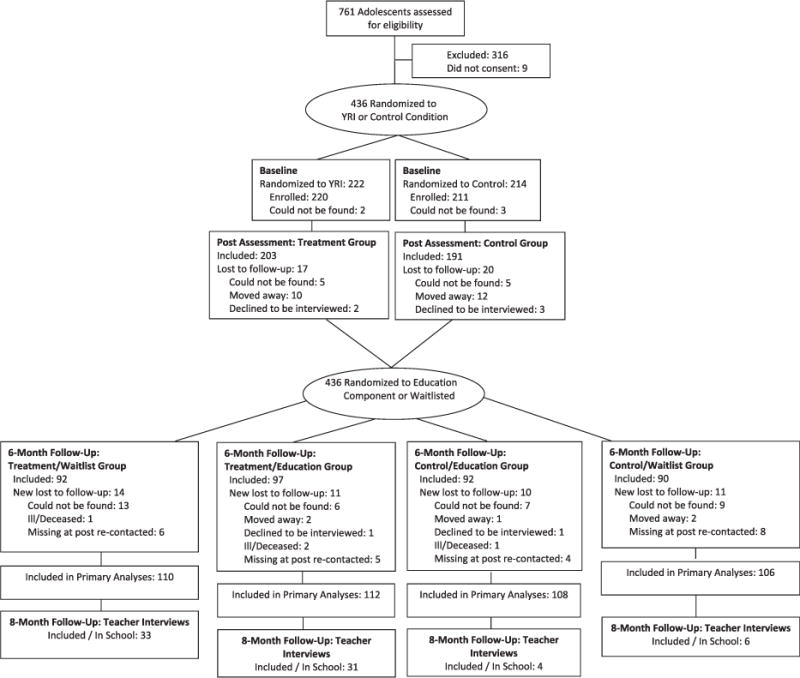
Consolidated Standards of Reporting (CONSORT) flow diagram. Note: Those excluded did not meet inclusion criteria (described in study eligibility criteria section of Methods). Primary analyses included all randomized participants, using 100 multiply imputed data sets to account for missingness. YRI = Youth Readiness Intervention.
Measures
Psychological distress (28 items, sample α = 0.86) was assessed by combining 16 internalizing (depression and anxiety) and 12 externalizing (hostility and aggression) items from the Oxford Measure of Psychosocial Adjustment (OMPA; scored 0–3), which was developed and validated for use in Sierra Leone24 and is correlated with standard measures of anxiety/depression such as the Hopkins Symptom Checklist (r = 0.51).10 In addition, a subscale measuring prosocial attitudes/behaviors (18 items, α = 0.82) was used as a key outcome measure. Capacity for emotion regulation was assessed using 23 items (scored 1–5) from the Difficulties in Emotion Regulation Scale (DERS; sample α = 0.65).25
The World Health Organization Disability Adjustment Scale (WHODAS, v. II)26 comprises 12-items (scored 0–4) that assess functional impairment across 5 domains: understanding and communicating, mobility, self-care, life activities, and participation in society. The instrument has been tested for validity and reliability in 14 countries, including in sub-Saharan Africa (sample α = 0.91). Social support was assessed with 25 items (scored 0–4) adapted from the Inventory of Socially Supportive Behaviors (sample α = 0.87).27 Posttraumatic stress symptoms were not a priority outcome of interest but were included as an exploratory outcome and were measured using the 12-item (scored 0–2) University of California, Los Angeles (UCLA) Post-Traumatic Stress Disorder Reaction Index (PTSD-RI, sample α = 0.86).28
At the end of the 2012 to 2013 academic year (8-month follow-up), the number and percentage of participants enrolled in school were evaluated, and a 20-item teacher survey, the Classroom Performance Scale (CPS; sample α = 0.95)29 was used to assess classroom behavior, including completion of coursework, classroom behavior, and classroom participation. Finally, teachers, blinded to condition, were asked to rate students’ attendance over the past month as poor, average, or good.
All measures new to this setting were reviewed by local collaborators for face validity, examined item-by-item for local comprehension, and forward- and backward-translated between English and Krio, the lingua franca, following a standard protocol.30
Intervention
The YRI combines elements drawn primarily from CBT and IPT, both evidence-based therapies with demonstrated effectiveness in treating depression, anxiety, and interpersonal deficits due to trauma.7,31 After a preliminary intervention development study that interviewed youth, caregivers, and key experts working with war-affected youth, the 6 core YRI components were deemed to be safe and feasible by lay health workers for delivery in community settings in groups of war-affected youth.13,18 In particular, the YRI was developed to address symptoms and impairments related to emotion dysregulation, risky behavior, and functional impairments, including interpersonal deficits, common among war-affected youth. Core components of the YRI include the following: psychoeducation about trauma and its impact on interpersonal relationships; self-regulation and relaxation skills (i.e., deep abdominal breathing); cognitive restructuring (i.e., addressing negative self-perceptions due to trauma); behavioral activation; communication and interpersonal skills; and sequential problem solving. The YRI is delivered over 10 to 12 sessions (Figure 2), depending on group needs, and also includes community and family meetings where appropriate, to enhance engagement and social support. All YRI components were culturally and contextually adapted and were reviewed and approved by the CAB.17 Intervention content was also adapted for older and younger age groups and gender in terms of the examples and vignettes used and in the content of group discussion and role play for skill building.
FIGURE 2.
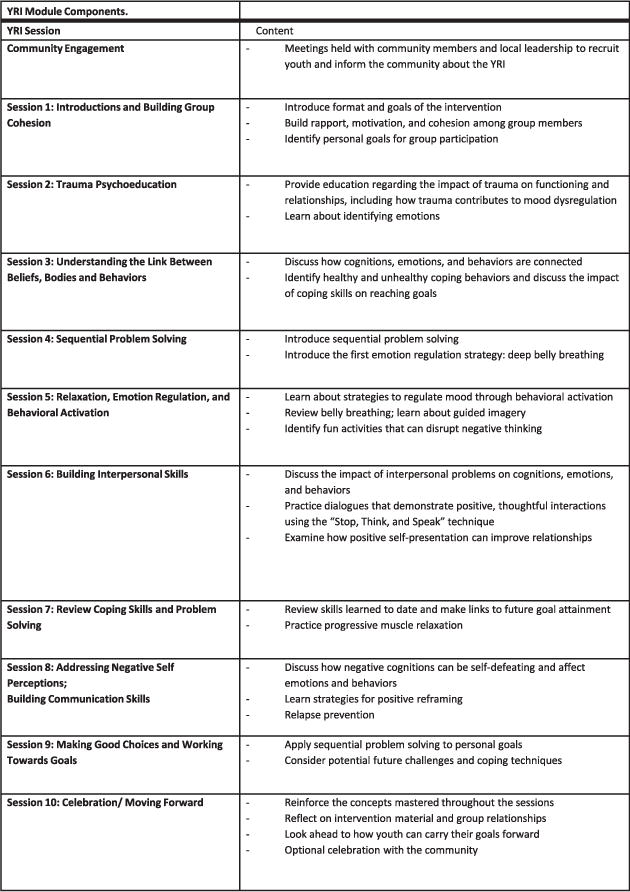
Overview of Youth Readiness Intervention (YRI).
We used a tiered approach for training and supervision. Four counselors who completed an intensive 2-week training conducted by members of the authorship team led training workshops for other potential counselors. Those who completed the training and achieved a high level of competency in the manualized treatment were employed by the study (n = 8). A senior local mental health worker provided weekly supervision to all counselors in-country, and study leaders, including 2 clinical psychologists, provided additional weekly group clinical supervision by telephone.
Procedures
Four male and 4 female local mental health workers were trained as counselors to facilitate the YRI in same-sex pairs. Delivery of the intervention was stratified by sex and age. All counselors had a bachelor’s degree or diploma in social work or a related field. A team of trained local research assistants conducted blinded interviews (approximately 90 minutes) in Krio at baseline, postintervention assessment, and 6-month follow-up.
To reduce transportation costs, group sessions were delivered at 6 community-based sites throughout Freetown. These locations were established with help from local community leaders and usually involved community meeting spaces or school buildings used during off hours. Sessions were held weekly for 10 weeks and lasted 90 minutes, followed by a meal. All group sessions were audio-recorded. Fidelity to the treatment manual was evaluated by the local supervisor via reviews of audio recording, using a fidelity checklist.
After the YRI, all study youth were randomized to receive a subsidized educational experience, starting in 2012 (n = 220) or 2013 (n = 216) at an alternative school for impoverished youth, which covered textbooks and tuition (youth/families were responsible for transportation). At the end of the first academic year (July 2013), the effect of assignment to an education subsidy on mental health and functioning was tested, and teachers blinded to condition were interviewed about youth school enrollment, attendance, and classroom performance. In this manner, the free education program was intended to serve as an active nonspecific intervention to examine whether social contact with peers and teachers alone would improve symptoms and impairments in war-affected youth.
Data Analysis
Based on a meta-analysis of evidence-based psychotherapies for youth,32 we adopted a standardized effect size (equivalent to Cohen’s d) of 0.30 as potentially achievable by the YRI and clinically significant for youth.32 Assuming a standard α level of 0.05 with a 0.5 correlation (r) across 2 time points, 436 participants were required to have 0.8 power to detect an effect size of 0.3, allowing for 20% attrition.
We used linear mixed-effects regression models33 to assess the effects of the YRI on mental health and functional outcomes over time, as well as the effect of the education subsidy. Models shown incorporated both postintervention and 6-month follow-up observations and accounted for clustering of youth within treatment groups and correlation of observations within persons over time. We included predictors to account for the stratified study design by incorporating age group and sex as main effects and interactions with treatment and time in all of our models, as well as an interaction between assignment to the education subsidy and treatment (YRI) assignment in all models for time points after the educational subsidy randomization had occurred.
For binary outcomes (e.g., school enrollment), logit mixed-effects regression models were used. Ordered logit regression models were used for ordinal outcomes (e.g., school attendance). For educational outcomes reported by teachers, a similar analytic approach used mixed-effects models to account for clustering of youth within treatment groups. The same stratification variables were incorporated in accordance with the study design but without terms for time. All statistical analyses were conducted in STATA 12.0 SE23 using 2-sided tests, with an α = 0.05 threshold for statistical significance.
The primary mode of analysis was intention-to-treat with 20 multiply-imputed data sets incorporated to account for missing values of all individuals, including those lost to follow-up (10% at postintervention, 15% at 6-month follow-up). Multiple imputation characterizes the joint probability distribution of all variables in the dataset to create plausible values for missing observations, in addition to adding an error term to each imputed value in each data set to create variability across imputations. Multiple imputation was also used to impute values for scales when item-level missingness was greater than 25% for a given scale.34 Otherwise, missing items within scales were imputed using Markov chain Monte Carlo (MCMC) methods with an added error term.
RESULTS
Baseline Characteristics
Participants comprised 237 males and 199 females. Mean age at baseline was 18.0 years (SD = 2.4 years). Twenty-six YRI groups were created with an average of 9 participants per group (range, 5–11 participants). Youth reported 8.5 years (SD = 2.0 years) of prior educational experience in the YRI group and 8.6 years (SD = 2.1 years) for controls. More than one-half of the participants reported losing a family member or friend as a direct result of the war, more than one-third had been separated from their caregiver during the war, and one-fifth had direct exposure to armed conflict (Table 1).
TABLE 1.
Study Sample Characteristics at Baseline
| Characteristic | Treatment Group (n = 222) | Control Group (n = 214) | ||
|---|---|---|---|---|
| Demographics | ||||
| Male sex, n (%) | 123 | (55.4) | 114 | (53.3) |
| Age, y | 17.8 | (2.3) | 18.1 | (2.6) |
| Years of education | 8.5 | (2.0) | 8.6 | (2.1) |
| Currently employed, n (%) | 87 | (39.2) | 84 | (39.3) |
| War Experience, n (%) | ||||
| Separated from caregiver due to war | 70 | (38.5) | 62 | (35.2) |
| Friend/family died due to war | 114 | (58.5) | 105 | (54.7) |
| Exposure to armed conflict | 35 | (18.9) | 38 | (20.5) |
| Member of armed forces | 11 | (6.0) | 12 | (6.7) |
| Outcome | ||||
| Emotion regulation | 3.42 | (0.29) | 3.40 | (0.29) |
| Prosocial behavior | 1.76 | (0.41) | 1.79 | (0.39) |
| Functional impairment | 0.60 | (0.60) | 0.57 | (0.51) |
| Psychological distress | 2.19 | (0.74) | 2.23 | (0.69) |
| Social support | 1.09 | (0.47) | 1.11 | (0.45) |
| Posttraumatic stress | 0.68 | (0.39) | 0.77 | (0.41) |
Note: Data shown as mean (SD) except percentages where noted.
Attendance in YRI
Of the 222 YRI participants, 82% attended at least 1 session, and more than 50% attended 75% or more of the sessions. The mean number of sessions attended was 6.3 (SD = 3.8).
Symptom Severity at Postintervention Assessment, and 6-Month Follow-Up
Coefficients at postintervention assessment and 6-month follow-up (time × intervention) are displayed in Table 2; all estimates represent the magnitude of the difference between treatment and control condition. At postintervention, YRI participants reported significantly greater improvements in emotion regulation (β = 0.108, 95% CI = 0.026–0.190, δ = 0.31) and prosocial attitudes/behaviors (β = 0.151, CI = 0.060–0.241, δ = 0.39) compared to controls. YRI participants also reported significantly greater reductions in functional impairment (β = −0.173, CI = −0.299 to −0.048, δ = −0.32) and greater improvements in social support (β = 0.134, CI = 0.025–0.242, δ = 0.29). The 2 conditions did not differ significantly on improvement in psychological distress (β = −0.021, CI = −0.196 to 0.154, δ = −0.03) or the exploratory outcome of posttraumatic stress symptoms (β = −0.007, CI = −0.097 to 0.083, δ = −0.02).
TABLE 2.
Intervention Effectiveness Estimates From Mixed-Effects Models
| Outcome | Treatment Effect: Postintervention
|
Treatment Effect: 6-Month Follow-Up
|
||||
|---|---|---|---|---|---|---|
| Coefficient (CI) | Effect Size | p Value | Coefficient (CI) | Effect Size | p Value | |
| Emotion regulation | 0.108 (0.026, 0.190) | 0.31 | .01 | 0.012 (−0.101, 0.125) | 0.03 | .84 |
| Prosocial behavior | 0.151 (0.060, 0.241) | 0.39 | .001 | .003 (−0.119, 0.124) | 0.01 | .92 |
| Functional impairment | −0.173 (−0.299, 0.048) | −0.32 | .007 | −0.052 (−0.220, 0.116) | −0.10 | .54 |
| Psychological distress | −0.021 (−0.196,0.154) | −0.03 | .92 | −0.027 (−0.267, 0.213) | −0.03 | .83 |
| Social support | 0.134 (0.025, 0.242) | 0.29 | .02 | 0.054 (−0.094, 0.202) | 0.12 | .47 |
| Posttraumatic stress | −0.007 (−0.097, 0.083) | −0.02 | .88 | 0.062 (−0.062, 0.187) | 0.14 | .33 |
Note: Treatment effect reported as per-item difference between treatment and control groups. Regression coefficients (β) are unstandardized. Ninety-five percent confidence interval reported in parentheses. Effect size for the treatment effect is reported as δ, equivalent to standardized mean difference.
At 6-month follow-up, the difference in symptom improvement between conditions was no longer greatly significant, as both treatment and control groups showed similar improvement relative to the elevated levels of symptoms on the initial screening.
School Functioning
Independent teacher assessments conducted 8 months after the sample was randomized to the education subsidy indicated further important differences by treatment. Teachers, blind to condition, rated YRI participants as having markedly better school attendance compared to controls (see Table 3). Although not all youth pursued the free educational opportunity, 28.8% (n = 64) of all YRI participants were in school, either the free program or other opportunities pursued by the youth themselves, at the time of the teacher interviews, whereas only 4.7% (n = 10) of the non-YRI control group had maintained enrollment in school (β[OR] = 8.88, CI = 3.29–23.97). Among youth in school, teachers reported that YRI participants, compared to controls, demonstrated significantly better classroom behavior (β = −0.95, CI = −1.81 to −0.10, δ = 1.17) based on the CPS, as well as better attendance over the past month (β[OR] = 34.93, CI = 2.69–454.00).
TABLE 3.
School Functioning Outcomes 8 Months After Youth Readiness Intervention (YRI) Completion
| Outcome | Range | Effect of YRI B, OR (CI) | Effect of Education Subsidy B, OR (CI) | ||||
|---|---|---|---|---|---|---|---|
| School retention | Yes/no | 8.88*** | 3.29 | 23.97 | 0.65 | 0.17 | 2.44 |
| Academic performance | 1–5 | −0.95* | −1.81 | −0.10 | −0.36 | −1.48 | 0.76 |
| School attendancea | 1–3 | 34.93** | 2.69 | 454.00 | 24.23* | 1.59 | 369.13 |
Note: all school functioning outcomes were reported by students’ teachers at follow-up. Classroom performance was measured by Classroom Performance Scale; lower scores denote better performance.
Teachers rated school attendance on a Likert scale (1 = poor, 2 = average, 3 = good).
p < .05;
p < .01;
p < .001.
Those randomized to receive the immediate educational opportunity demonstrated greater school attendance (β[OR] = 24.23, CI = 1.59–369.13) than those who were waitlisted, but there was no effect of the educational opportunity on mental health symptoms, functioning, school retention, or classroom behavior. Interactions between education assignment and YRI assignment were nonsignificant.
DISCUSSION
The YRI, tested in a low-resource, post-conflict setting and delivered by trained local counselors, had beneficial effects on emotion regulation, prosocial behavior, social support, and daily functioning at postintervention, and on school enrollment, attendance, and performance at follow-up. Indeed, YRI participants were 6 times as likely as non-YRI youth to persevere in school. By contrast, a straightforward educational subsidy, which might have been considered a less complex alternative to improving mood and behaviors in war-affected youth, showed an effect only on school enrollment and did not influence any of the other educational or psychological outcomes. In addition, the educational subsidy did not interact with YRI in relation to any study measure. Taken together, these findings suggest that YRI produced multiple acute and longer-term emotional and behavioral benefits, markedly outpacing the impact of financial support for education. Education is widely regarded as a key to success in life for youth whose lives have been disrupted by war. Thus, our finding that YRI boosted educational engagement, attendance, and behavior may be especially important.
A core aim of the YRI was to equip distressed, war-affected youth to excel in educational or employment opportunities. “Readiness” for educational programs was achieved among youth by addressing interpersonal functioning and behaviors that can block school success. Specifically, YRI modules focused on self-regulation/anger management, building interpersonal skills, and problem solving. Our findings are consistent with other studies that indicate successful adaptation of components of common evidence-based treatments, even when delivered in a task-sharing model in which community health workers are provided with training and expert supervision.5,7 The current study expands on previous work by linking mental health symptom improvement to other domains of functioning—specifically daily functioning, school persistence, and classroom behavior.
Although retention was strong, YRI attendance and school attendance were affected by our inability to provide transportation for participants, especially to the subsidized education opportunity, EducAid, and the percentage of youth who demonstrated school retention overall was low (17%). Thus, provision of the free education opportunity was not effective for most, perhaps because of distance and personal expense required for transport, and other complications confronting war-affected youth living in poverty. A limitation of our findings was that the effects on psychological measures found at postintervention were not evident at 6-month follow-up. Yet the impact of YRI was quite evident in the YRI main effects on school enrollment, attendance, and performance. In future research, it will be useful to investigate which aspects of the YRI are most responsible for its long-term beneficial effects on such school outcomes. It is noteworthy that neither YRI nor the school subsidy was associated with significant reductions in overall psychological distress or PTSD symptoms. PTSD symptoms were not the primary focus of either intervention, but distress might be expected to be reduced, particularly by YRI.
Given the role of daily stressors in influencing psychological distress,35,36 and as documented in prior research in the region,10 it is possible that reductions in distress may not be seen unless concurrent reductions in daily stressors and increases in economic security are evident. Such effects may be evident over a longer time horizon of follow-up. A final limitation is that our symptom outcomes were derived mainly from self-report measures. School-related measures, however, were all derived from ratings by teachers who were blinded to participants’ group membership, measures that strengthen and triangulate the findings on improved behavior and functioning among YRI participants.
Our results point to areas for future research. First, the findings warrant replication in other conflict-affected settings. Second, it will be useful to test strategies for boosting the impact of the intervention, for example, by offering check-in (i.e., booster) sessions, whereby youth discuss application of learned skills to daily routines and personal goals. Third, it will be useful to test whether YRI—given its focus on improving self-regulation, functioning, and interpersonal skills to maximize life opportunities—improves prospects for youth transition to employment, clearly a critical life objective for those in economically disadvantaged post-war regions.
Youth struggling with the mental health consequences of war merit special attention by policymakers, health workers, researchers, and mental health professionals globally. School drop-out, underemployment, violence, and poverty are inextricably linked to poor mental health and functioning in war-affected youth. The YRI is a promising intervention to improve youth mental health and functioning, including functioning in school. Future research on the YRI should focus on understanding mediators and moderators of the intervention’s impact as well as testing its effects with youth in other conflict-affected settings.
Clinical Guidance.
Youth struggling with the mental health consequences of war merit special attention by policymakers, health workers, researchers, and mental health professionals globally.
A core aim of the Youth Readiness Intervention (YRI) was to equip distressed, war-affected youth to excel in educational or employment opportunities.
YRI modules focused on self-regulation/anger management, building interpersonal skills, and problem solving.
YRI produced multiple acute emotional and behavioral benefits. School drop-out, underemployment, violence, and poverty are inextricably linked to poor mental health and functioning in war-affected youth.
“Readiness” for educational programs was achieved among youth by addressing interpersonal functioning and behaviors that can block school success.
The YRI is a promising intervention to improve youth mental health and functioning, including functioning in school.
Acknowledgments
This study was supported by the United States Institute of Peace (USIP-008-10F), the UBS Optimus Foundation (UBS-5253), the National Institute for Mental Health (5K01MH077246-05; 1F31MH097333-01A1), the National Institute of Aging (5P30AG024409-08), Harvard Catalyst, the Julie Henry Junior Faculty Development Fund, the Australian Psychological Society, and the Australian National Health and Medical Research Council.
Dr. McBain and Dr. Brennan served as the statistical experts for this research.
The authors thank Caritas Internationalis, EducAid Sierra Leone, the FXB Center for Health and Human Rights at Harvard University, and Sarah Kate Bearman, PhD, of Yeshiva University and Anne Willhoite, MA, of the Center for Victims of Torture for their assistance in developing the Youth Readiness Intervention (YRI), as well as Katrina Hann, MA, who managed the trial in country. Above all, the authors thank their local advisory board for their steadfast guidance, their local facilitators and supervisors, and the many youth and families who participated in the study.
Footnotes
Disclosure: Drs. Betancourt, Newnham, Akinsulure-Smith, Brennan, Weisz, Hansen, and McBain report no biomedical interests or potential conflicts of interest.
Contributor Information
Dr. Theresa S. Betancourt, Harvard T. H. Chan School of Public Health, Cambridge, MA.
Dr. Ryan McBain, François-Xavier Bagnoud (FXB) Center for Health and Human Rights at Harvard University and the Harvard T. H. Chan School of Public Health.
Dr. Elizabeth A. Newnham, The University of Western Australia, Crawley, Western Australia, and the FXB Center for Health and Human Rights at Harvard University.
Dr. Adeyinka M. Akinsulure-Smith, City College of the City University of New York.
Dr. Robert T. Brennan, FXB Center for Health and Human Rights at Harvard University.
Dr. John R. Weisz, Harvard University Faculty of Arts and Sciences and Harvard Medical School.
Dr. Nathan B. Hansen, College of Public Health at the University of Georgia, Athens, GA.
References
- 1.Tol WA, Barbui C, Galappatti A, et al. Mental health and psychosocial support in humanitarian settings: linking practice and research. Lancet. 2011;378:1581–1591. doi: 10.1016/S0140-6736(11)61094-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Machel G. Impact of Armed Conflict on Children. New York: United Nations; 1996. [Google Scholar]
- 3.Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet. 2007;369:1302–1313. doi: 10.1016/S0140-6736(07)60368-7. [DOI] [PubMed] [Google Scholar]
- 4.Derluyn I, Broekaert E, Schuyten G, De Temmerman E. Post-traumatic stress in former Ugandan child soldiers. Lancet. 2004;363:861–863. doi: 10.1016/S0140-6736(04)15734-6. [DOI] [PubMed] [Google Scholar]
- 5.Ruf M, Schauer M, Neuner F, Catani C, Schauer E, Elbert T. Narrative exposure therapy for 7- to 16-year-olds: a randomized controlled trial with traumatized refugee children. J Traum Stress. 2010;23:437–445. doi: 10.1002/jts.20548. [DOI] [PubMed] [Google Scholar]
- 6.Neuner F, Catani C, Ruf M, Schauer E, Schauer M, Elbert T. Narrative exposure therapy for the treatment of traumatized children and adolescents (KidNET): from neurocognitive theory to field intervention. Child Adolesc Psychiatr Clin N Am. 2008;17:641–664. doi: 10.1016/j.chc.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Bolton P, Bass J, Betancourt TS, et al. Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: a randomized controlled trial. JAMA. 2007;298:519–527. doi: 10.1001/jama.298.5.519. [DOI] [PubMed] [Google Scholar]
- 8.Collier P. The Bottom Billion. New York: Oxford University Press; 2008. [Google Scholar]
- 9.Human Rights Watch. Youth Poverty and Blood: the Lethal Legacy of West Africa’s Regional Warriors. New York: Human Rights Watch; 2005. [Google Scholar]
- 10.Betancourt TS, Brennan RT, Rubin-Smith J, Fitzmaurice GM, Gilman SE. Sierra Leone’s former child soldiers: a longitudinal study of risk, protective factors, and mental health. J Am Acad Child Adolesc Psychiatry. 2010;49:606–615. doi: 10.1016/j.jaac.2010.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Sierra Leone: Mental Health Atlas. Geneva, Switzerland: World Health Organization; 2011. 2011. [Google Scholar]
- 12.Herman J. Trauma and Recovery: The Aftermath of Violence—From Domestic Abuse to Political Terror. New York: BasicBooks; 1997. [Google Scholar]
- 13.Cloitre M, Koenen KC, Cohen LR, Han H. Skills training in affective and interpersonal regulation followed by exposure: a phase-based treatment for PTSD related to childhood abuse. J Consult Clin Psychol. 2002;70:1067–1074. doi: 10.1037//0022-006x.70.5.1067. [DOI] [PubMed] [Google Scholar]
- 14.Patel V, Belkin GS, Chockalingam A, Cooper J, Saxena S, Unützer J. Grand challenges: integrating mental health services into priority health care platforms. PLoS Med. 2013;10:e1001448. doi: 10.1371/journal.pmed.1001448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Betancourt T, Newnham E, Hann K, McBain R, Akinsulure-Smith A, Weisz J, Lilienthal G, Hansen N. Addressing the Consequences of Violence and Adversity: The Development of a Group Mental Health Intervention for War-Affected Youth in Sierra Leone. In: Raynaud J, Gau S, Hodes M, editors. From Research to Practice in Child and Adolescent Mental Health. Maryland: Rowman & Littlefield; 2014. pp. 157–178. [Google Scholar]
- 16.Balaji M, Chatterjee S, Koschorke M, et al. The development of a lay health worker delivered collaborative community based intervention for people with schizophrenia in India. BMC Health Serv Res. 2012;12:42. doi: 10.1186/1472-6963-12-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Betancourt T, Newnham E, Hann K, et al. Addressing the consequences of violence and adversity: the development of a group mental health intervention for war-affected youth in Sierra Leone. In: Raynaud J, Gau S, Hodes M, editors. From Research to Practice in Child and Adolescent Mental Health. Lanham, MD: Rowman and Littlefield; 2014. pp. 157–178. [Google Scholar]
- 18.Chorpita BF, Becker KD, Daleiden EL. Understanding the common elements of evidence-based practice: misconceptions and clinical examples. J Am Acad Child Adolesc Psychiatry. 2007;46:647–652. doi: 10.1097/chi.0b013e318033ff71. [DOI] [PubMed] [Google Scholar]
- 19.Ford JD. Disorders of extreme stress following war-zone military trauma: associated features of posttraumatic stress disorder or comorbid but distinct syndromes? J Consult Clin Psychol. 1999;67:3–12. doi: 10.1037//0022-006x.67.1.3. [DOI] [PubMed] [Google Scholar]
- 20.van Minnen A, Harned MS, Zoellner L, Mills K. Examining potential contraindications for prolonged exposure therapy for PTSD. Eur J Psychotraumatol. 2012;3 doi: 10.3402/ejpt.v3i0.18805. http://dx.doi.org/10.3402/ejpt.v3i0.18805. Epub 2012 Jul 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Betancourt TS, McBain R, Newnham EA, Brennan RT. Trajectories of internalizing problems in war-affected Sierra Leonean youth: examining conflict and postconflict factors. Child Dev. 2013;84:455–470. doi: 10.1111/j.1467-8624.2012.01861.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Betancourt TS, Newnham EA, McBain R, Brennan RT. Post-traumatic stress symptoms among former child soldiers in Sierra Leone: follow-up study. Br J Psychiatry. 2013;203:196–202. doi: 10.1192/bjp.bp.112.113514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stata Longitudinal-Data/Panel-Data Reference Manual. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- 24.MacMullin C, Loughry M. Investigating psychosocial adjustment of former child soldiers in Sierra Leone and Uganda. J Refugee Stud. 2004;17:460–472. [Google Scholar]
- 25.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. J Psychopathol Behav Assess. 2004;26:41–54. [Google Scholar]
- 26.World Health Organization. World Health Organization Disability Assessment Schedule II (WHODAS II) Geneva: World Health Organization; 2001. [Google Scholar]
- 27.Barrera M, Sandler IN, Ramsay TB. Preliminary development of a scale of social support: studies on college students. Am J Commun Psychol. 1981;9:435–447. [Google Scholar]
- 28.Steinberg A, Brymer M, Decker K, Pynoos R. The University of California at Los Angeles Post-Traumatic Stress Disorder Reaction Index. Curr Psychiatry Rep. 2004;6:96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- 29.Children and Adults with Attention Deficit Disorder (CHADD) ADD and Adolescence: Strategies for Success From CHADD. Plantation, FL: CHADD; 1996. [Google Scholar]
- 30.Betancourt T, Scorza P, Meyers-Ohki S, et al. Validating the Center for Epidemiological Studies Depression Scale for Children in Rwanda. J Am Acad Child Adolesc Psychiatry. 2012;51:1284–1292. doi: 10.1016/j.jaac.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jordans MJ, Tol WA, Susanty D, et al. Implementation of a mental health care package for children in areas of armed conflict: a case study from Burundi, Indonesia, Nepal, Sri Lanka, and Sudan. PLoS Med. 2013;10:e1001371. doi: 10.1371/journal.pmed.1001371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weisz JR, Jensen-Doss A, Hawley KM. Evidence-based youth psychotherapies versus usual clinical care: a meta-analysis of direct comparisons. Am Psychologist. 2006;61:671–689. doi: 10.1037/0003-066X.61.7.671. [DOI] [PubMed] [Google Scholar]
- 33.Picat MQ, Lewis J, Musiime V, et al. Predicting patterns of long-term CD4 reconstitution in HIV-infected children starting antiretroviral therapy in sub-Saharan Africa: a cohort-based modelling study. PLoS Med. 2013;10:e1001542. doi: 10.1371/journal.pmed.1001542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tang L, Song J, Belin TR, Unutzer J. A comparison of imputation methods in a longitudinal randomized clinical trial. Stat Med. 2005;24:2111–2128. doi: 10.1002/sim.2099. [DOI] [PubMed] [Google Scholar]
- 35.Miller KE, Rasmussen A. War exposure, daily stressors, and mental health in conflict and post-conflict settings: bridging the divide between trauma-focused and psychosocial frameworks. Soc Sci Med. 2010;70:7–16. doi: 10.1016/j.socscimed.2009.09.029. [DOI] [PubMed] [Google Scholar]
- 36.Lund C, Breen A, Flisher AJ, et al. Poverty and common mental disorders in low and middle income countries: a systematic review. Soc Sci Med. 2010;71:517–528. doi: 10.1016/j.socscimed.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]


