Abstract
Aims:
To identify the relation between need, demand, and effective demand for dental services in Andhra Pradesh, India.
Materials and Methods:
This is a cross-sectional study performed among populations residing in the rural and urban areas of Krishna district, Andhra Pradesh, India. Data were collected from 3102 individuals who were selected through multiphase random sampling. Data regarding self-perceived dental need, dental service utilization, and barriers for utilization were collected through s pretested questionnaire followed by type-III clinical examination to assess the normative need of the individuals. Chi-square test was used to compare independent and dependent variables, and further comparison was done with multivariate logistic regression analysis for significant variables.
Results:
Less than half (40%) of the participants perceived a need for dental care. Among the people who perceived need for care, only 21.4% utilized dental care and 78.6% of them had unmet dental needs. The two main reasons for not seeking dental care was lack of money, i.e., unaffordable dental treatment (48%) and having the perception that they do not have any dental problem (19.4%).
Conclusions:
There is an enormous difference between normative need, demand, and actual utilization rates in dental care, and hindrances for effective demand need to be addressed to improve dental care delivery system.
Key words: Demand for dental care, dental service utilization, normative need
INTRODUCTION
India is a nation with one of the fastest growing economies in the world with more than one billion population with varied geography, culture, language, habits, and even per capita income. This diversity also encompasses socioeconomic status, literacy, indicators of health, such as maternal and infant mortality rates, and nutritional practices.[1] As per the National Oral Health Survey and fluoride mapping report (2002-2003), prevalence of dental caries in 15-year old individuals was 63.1% and 80.2% in 35–44-year age group. Prevalence of periodontal disease was 67.7% in 15-year olds and 89.6% in 35–44 year olds. The mean decayed, missing, filled teeth (DMFT) score is 2.4 in 15-year olds and as high as 5.4 among 35–44 year olds. India stands first in oral cancer prevalence (19 cases per 100,000 population). Rural population and low income socioeconomic families exhibited higher prevalence of oral diseases.[2]
According to a National report on human resources for health, 117,825 dentists were registered at the end of 2011,[3] with 1 dentist per 10271 people. The dentist–population ratio in India is far less than many Asian countries such as Sri Lanka (1:13000) and China (1:12727); however, the per capita dental utilization of dental services has also been reported to be less.[4,5]
The fact that oral diseases are seldom responsible for direct mortality may be one of the reasons for lack of dental service utilization behavior.[6] Dental service utilization is defined as the proportion of the population who utilized dental care over a specified time period.[7] Actual dental care utilization typically describes the proportion of the population who have visited a dentist at specified periods of time. It is an important factor in oral health policy designing.[7] Both oral health and dental service utilization are interrelated, i.e., utilization also has a positive influence on oral health.[8] A study in Udaipur reported that the cost oftreatment, distance travelled to get dental care, and the needs of the society play a major role in reduction of dental services utilization.[9] According to a study conducted in Shimla, only 15.1% visited a dental care facility within the last 1 year; the reason for this was reported to be pain or dental emergency.[10]
Kadaluru et al. reported in their study that only 28% of the study participants visited dentist in the past 1 year, and poverty is the major reason for not visiting a dentist.[11] A study conducted by Bommireddy et al. found that half of the (50.8%) of the people who did not visit a dentist felt that oral health holds less priority for them in relation to general health; another study conducted by Devraj et al. reported that only 38% visited a dentist in the past 2 years.[12,13]
The consumption side of the dental services has three important components which are defined as need, perception that need exists (demand), and action by the individual to have that need met (effective demand). There is limited information available regarding the dental need, demand, and effective demand for dental services and factors influencing these variables, which can help in oral health policy making. Hence, the aim of this study is to assess the relation between need, demand, and effective demand for dental services in Krishna district, Andhra Pradesh, India.
MATERIALS AND METHODS
This was a cross-sectional study conducted at Krishna district, Andhra Pradesh, India between January–May 2015. The selected participants were interviewed, and then later clinically examined to determine their dental needs. Prior to the main study, a pilot study was performed among 50 individuals to assess the feasibility, in which 50% of the participants perceived need for care and only 23% the effective demand. The sample size was determined using 50% response in pilot study (P = 0.5%), 5% of error, and 95% of confidence level.
Sample size for infinite population, N = Z (α) × P (1 − P)/C2
Z (α) = Type 1 Error = Z (α) value, P = Proportion of perceived need, and C = confidence interval
Adjustment for known population (pop) of Krishna district was done using the formula:
N = 1 + SS − 1/pop; where, SS is sample size for infinite population, pop is 45,17,398.
Hence, the required sample size is 2499; assuming 25% of nonresponse, the sample size was adjusted to 3124. Participants were selected through cluster random sampling. In the first phase, 14 rural villages and 7 urban census enumeration blocks were selected by using simple random method. The author and his assistants initially selected households by systematic random sampling method (every 3rd house) from the list of houses, and members in that house were included in study. The response rate was 99%, with the nonresponse rate largely resulting from unavailability. A total of 3102 respondents (1852 rural and 1250 urban) participated in this study. Prior approval of study protocol was obtained from the Institutional Review board of Drs. Sudha and Nageswara Rao Siddhartha Institute of Dental Sciences (SIDS_EC/04/2015), and necessary permissions to conduct this study were obtained from the district administration authorities and village development officers. Written consent was obtained from all participants. A semi-structured questionnaire was designed in the local language. Internal consistency of the questionnaire was tested with Cronbach's α (0.78) and test-retest reliability was tested with Kappa statistic (0.86). Socioeconomic status was assessed using Prasad's classification.[11] After completion of the interview, every individual was examined using the World Health Organization (WHO) oral assessment criteria (1997) by type-III clinical examination under natural day light. Respondents were asked about their self-perceived need (felt need/demand) for dental care with a 1-year recall period. Perceived need for care (demand) and actual dental service utilization (effective demand) were the first and second dependent variables of this study. The responses were dichotomized as “yes” or “no” answers. The third variable of reason for not seeking dental care was an open-ended question, and in the fourth variable, normative need of an individual participant, i.e., the presence of need was considered, if a person required some form of dental care. Independent variables in this study included age (<15, 16-24, 25-34, 35-44, 45-54, 55-64, and >65 years), gender (female or male), socioeconomic class, residence (rural or urban), etc.
Data was analyzed with the Statistical Package for Social Sciences [Version 17.0. Chicago: SPSS Inc.]. Descriptive statistics were used to describe the percentage of perceived need for and utilization of dental care. Chi-square test was used to compare independent and dependent variables and further comparison was done with multivariate logistic regression analysis for significant variables. Significant variables (P < 0.05) in bivariate analysis were included in the logistic regression model.
RESULTS
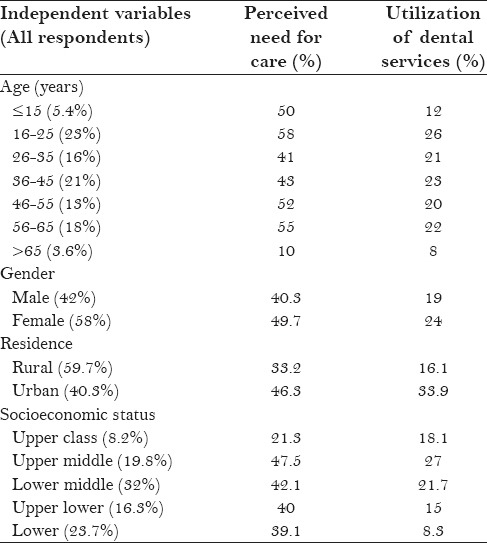
The demand for dental services was higher in participants aged 16-25 years, females, those in the upper middle class, and those residing in urban areas [Table 1]. Utilization of dental care was greater in individuals aged 26–35, females, those in the upper middle class, and those residing in urban areas. People from the highest socioeconomic strata reported to have the least perceived need for dental care, however at the same time, this group utilized more than what they perceived; the poorest class utilized the least amount of services [Table 1].
Table 1.
Comparison between independent variables, perceived need, and actual utilization of dental services
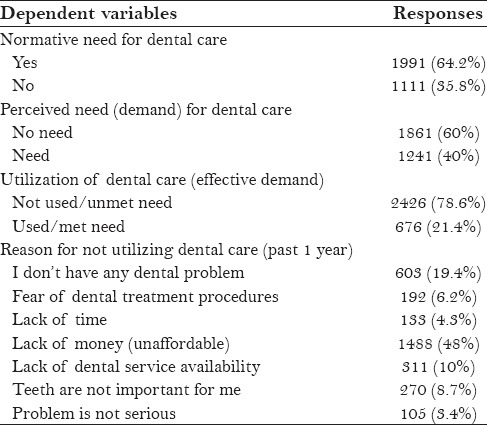
Less than half (40%) of the participants perceived a need for dental care [Table 2]. Among the people who perceived need for care, only 21.4% of them utilized dental care and 78.6% of them had unmet dental needs, as they had perceived need for dental care but did not receive any dental treatment. The two main reasons for not seeking dental care was lack of money, i.e., unaffordable dental treatment (48%) and having the perception that they do not have any dental problem (19.4%) [Table 2].
Table 2.
Participants overall responses to dependent variables
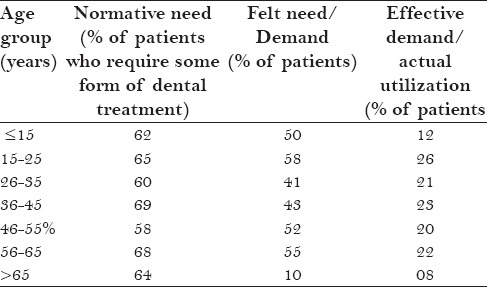
The overall normative need of the study participants was 64.2%, which was highest in 36–45 year age group, and demand for dental treatment was more in children and young adults [Table 1]. There is a huge gap in participants (%) who utilized dental services, i.e. less than 25% in any age cohort visited a dentist during a 1-year duration [Table 3].
Table 3.
Comparison between normative need, demand and effective demand for dental care with age groups
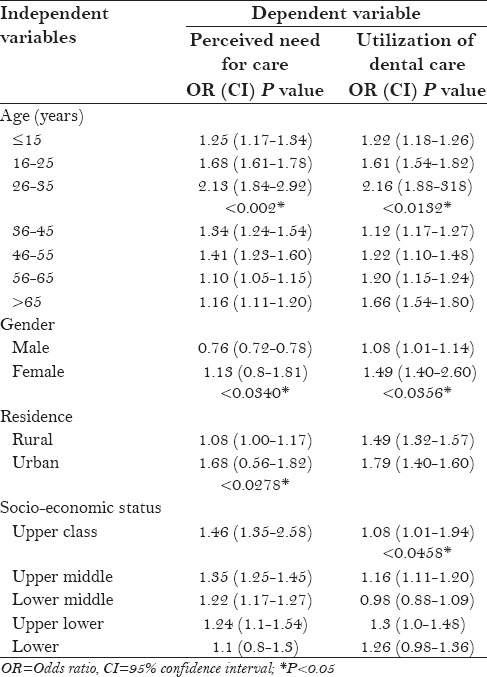
The results of the logistic regression analysis revealed that the 26–35 year age group demonstrated the highest odds ratio for perceiving a need for dental care [Table 4]. The utilization of dental care services was directly proportional to socioeconomic status. The upper middle class, which carried an odds ratio of 2.19, yielded the strongest association with utilization of dental care. Participants who were older than 65 years and those who lived in rural areas had generally lower odds ratio in perceiving need for and utilization of dental care.
Table 4.
Multivariate analysis between dependent and independent variables
DISCUSSION
Assessment of clinical oral health was not the center of attention of this study. The main aim of this study was to accomplish a better understanding of the percentage of demand for dental treatment to actual dental service utilization behavior in India. Even though the fact that the national prevalence of caries was 61.4% for 15 year age group and 79.2% in 35–44 year age group (National oral health survey 2002-03),[2] but the respondents to this survey who perceived a need for dental care were only 40% (approximately). Furthermore, the unmet needs for dental care was high, which is similar to the findings from the study conducted in Udaipur.[9] The two most common reasons for nonutilization of dental services are economic reasons, and a response that “I don't have any dental problem,” which is an agreement with a study reported from Shimla where 68.5% reported that they do not have any dental pain, and hence no dental problem.[10] The utilization rates (21.4%) and reasons for nonutilization in this study were similar to studies conducted by Kadaluru et al.[11] in which only 28% utilized dental services, as well as a study conducted in Thailand, where 63.9% of study participants never used any dental services.[14] The findings of the present are contradictory to the study reported by Kakatkar et al,[9] in which males utilized more services than females. Results of this study call for an urgent need to educate the people regarding the importance of oral health and its relation to general health. People need to be educated about nonpainful signs and symptoms of oral diseases to ensure self-examination and motivation to seek dental care. To this end, use of mass media and alliance with other medical specialties may also disseminate dental health literacy.[9] By doing so, people would be able to identify initial signs and symptoms of dental diseases at an initial stage and seek dental treatment.[15] Less dental service utilization rate reported could be because barriers, as mentioned in literature, such as different socioeconomic groups,[16] age, geographic location, etc., which make it difficult for information to reach certain communities.
The current study had certain limitations. The first limitation is the use of a dichotomous question regarding perceived dental care needs. A “no” answer may represent an absence of current dental problems. However, the same “no” response can be attributed to many reasons. Previous studies have highlighted the differences in pain perception, with males being less likely to report pain than females.[8] On the other hand, nonperception for dental care can be due to nonpainful signs and symptoms.[17]
Another limitation is the subjective nature of perceived dental care because they were influenced by an individual's viewpoint on the sense of his or her oral health and problem.[18,19] Therefore, it is not only the severity of signs and symptoms of dental illness which influence perceived need for care but it can also be influenced by dental health literacy.[20,21] Many people are often unaware of their dental care needs, which may be due to less severity of pain and unaffected daily activities.[22] The study participants often forget or would have ignored their illness that does not disrupt their daily activities, as reported in a Sri Lankan study.[23] A study reported from Iran highlighted the mental health status that plays an important role in dental service utilization.[24] Moreover, if the study goal is to assess the need that is both normative and subjective, then subjective indicators alone may not be as good as clinical examination/screening. Clearly, further research is needed to assess the factors influencing demand for dental care and actual utilization.
CONCLUSION
Dental service utilization among residents of Krishna district, Andhra Pradesh, India, was low, and was influenced by some demographic and socioeconomic factors. Because the gaps exist between normative need and demand (felt need), which clearly indicates a lack of dental health awareness among these populations, for which health education programs should be planned to improve awareness. Enhancement in dental care utilization (effective demand) in this population will broadly depend on the overall socioeconomic development, as well as on the improvements in the oral health care service delivery system, which should incorporate the needs of underprivileged populations. Future research should explore the cultural dimensions on utilization of dental services.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Shaju JP, Zade RM, Das M. Prevalence of periodontitis in the Indian population: A literature review. J Indian Soc Periodontol. 2011;15:29–34. doi: 10.4103/0972-124X.82261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bali RK, Mathur VB, Talwar PP, Chanana HB. National oral health survey and fluoride mapping; 2002-2003. New Delhi, India: Dental Council of India; 2004. pp. 16–7. [Google Scholar]
- 3.National Health Profile. [Last accessed on July 25, 2013]. Available at: http://www.cbhidghs.nic.in/writereaddata/mainlinkFile/10%20%20Human%20Resources%20%20in%20Health%20Sector%20%202011.pdf .
- 4.Dileep de Silva, Sally Brailsford, Jayasundara Bandara. Dental workforce planning, Sri Lankan experience. [Last accessed on July 14, 2013]. Available from: www.econ.kuleuven.be/eng/tew/academic/prodbel/ORAHS2009/10.pdf .
- 5. [Last accessed on July 15, 2013]. http://www.hc.bios.com/en/news_view.php?sn=17 .
- 6.Mohanty U, Parkash H. Perception of accredited social health activists regarding oral health in Northern India. Indian J Public Health. 2011;55:340–1. doi: 10.4103/0019-557X.92424. [DOI] [PubMed] [Google Scholar]
- 7.Brown J, Lazar V. Dental care utilization: How saturated is the patient market. J Am Dent Assoc. 1999;130:573–80. doi: 10.14219/jada.archive.1999.0255. [DOI] [PubMed] [Google Scholar]
- 8.Freeman R. Barriers to accessing dental care: Dental health professional factors. Br Dent J. 1999;187:197–200. doi: 10.1038/sj.bdj.4800238. [DOI] [PubMed] [Google Scholar]
- 9.Kakatkar G, Bhat N, Nagarajappa R, Prasad V, Sharda A, Asawa K, Agrawal A. Barriers to the Utilization of Dental Services in Udaipur, India. J Dent. 2011;8:81–9. [PMC free article] [PubMed] [Google Scholar]
- 10.Fotedar S, Sharma KR, Bhardwaj V, Sogi GM. Barriers to the Utilization of Dental Services in Shimla, India. Eur J Gen Dent. 2013;2:139–43. [Google Scholar]
- 11.Kadaluru UG, Kempraj VM, Muddaiah P. Utilization of oral health care services among adults attending community outreach programs. Indian J Dent Res. 2012;23:841–2. doi: 10.4103/0970-9290.111290. [DOI] [PubMed] [Google Scholar]
- 12.Bommireddy VS, Pachava S, Ravoori S, Sanikommu S, Talluri D, Vinnakota NR. Socio-economic Status, Needs, and Utilization of Dental Services among Rural Adults in a Primary Health Center Area in Southern India. J Int Oral Health. 2014;6:56–60. [PMC free article] [PubMed] [Google Scholar]
- 13.Devaraj C, Eswar P. Reasons for use and non-use of dental services among people visiting a dental college hospital in India: A descriptive cross-sectional study. Eur J Dent. 2012;6:422–7. [PMC free article] [PubMed] [Google Scholar]
- 14.Jaidee J, Ratanasiri A, Chatrchaiwiwatana S, Soonthon S. Prevalence and Factors Associated with the Utilization of Dental Care Services among Factory Workers in Nava Nakorn Industrial Estate, Pathumthani Province, Thailand. J Med Assoc Thai. 2015;98:S73–80. [PubMed] [Google Scholar]
- 15.Olusile AO, Adeniyi AA, Orebanjo O. Self-rated oral health status, oral health service utilization, and oral hygiene practices among adult Nigerians. BMC Oral Health. 2014;14:140. doi: 10.1186/1472-6831-14-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cornejo-Ovalle M, Paraje G, Vásquez-Lavín F, Pérez G, Palència L, Borrell C. Changes in socioeconomic inequalities in the use of dental care following major healthcare reform in Chile, 2004-2009. Int J Environ Res Public Health. 2015;12:2823–36. doi: 10.3390/ijerph120302823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lal S. Community and Community diagnosis. In: Sunder Lal, Adarsh, Pankaj, editors. Text book of Community Medicine. 3rd edition. India: CBS publishers; 2011. pp. 17–9. [Google Scholar]
- 18.Vargas CM, Dye BA, Hayes K. Oral health care utilization by US rural residents, National Health Interview Survey 1999. J Public Health Dent. 2003;63:150–7. doi: 10.1111/j.1752-7325.2003.tb03493.x. [DOI] [PubMed] [Google Scholar]
- 19.Simon AK, Rao A, Rajesh G, Shenoy R, Pai MB. Trends in self-medication for dental conditions among patients attending oral health outreach programs in coastal Karnataka, India. Indian J Pharmacol. 2015;47:524–9. doi: 10.4103/0253-7613.165195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slaughter A, Taylor L. Perceptions of dental care need among African-American elders: Implications for health promotion. Spec Care Dentist. 2005;25:158–63. doi: 10.1111/j.1754-4505.2005.tb01427.x. [DOI] [PubMed] [Google Scholar]
- 21.Kristiansen S, Santosh P. Surviving decentralization? Impacts of regional autonomy on health service provision in Indonesia. Health Policy. 2006;77:247–59. doi: 10.1016/j.healthpol.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 22.Maharani DA. Perceived need for and utilization of dental care in Indonesia in 2006 and 2007: A secondary analysis. J Oral Sci. 2009;51:545–50. doi: 10.2334/josnusd.51.545. [DOI] [PubMed] [Google Scholar]
- 23.Ekanayake L, Perera I. Perceived need for dental care among dentate older individuals in Sri Lanka. Spec Care Dentist. 2005;25:199–205. doi: 10.1111/j.1754-4505.2005.tb01650.x. [DOI] [PubMed] [Google Scholar]
- 24.Bahramian H, Mohebbi SZ, Khami MR, Asadi-Lari M, Shamshiri AR, Hessari H. Psychosocial determinants of dental service utilization among adults: Results from a population-based survey (Urban HEART-2) in Tehran, Iran. Eur J Dent. 2015;9:542–50. doi: 10.4103/1305-7456.172622. [DOI] [PMC free article] [PubMed] [Google Scholar]


