Abstract
Aim:
Pathologic tooth migration (PTM) has been defined as tooth displacement that occurs when the balance among the factors that maintain physiologic tooth position is disturbed by periodontal disease. The aim of this cross-sectional epidemiological study was to determine the prevalence of pathologic tooth migration among patients with periodontitis.
Materials and Methods:
Recorded documents of 370 patients (72.4% females, 27.6% males) within the age range of 17 to 70 years (mean 37.77 ± 11.46) were studied. Statistical analysis was carried out using t-test and Chi-square test.
Results:
Pathologic migration prevalence was 11.4% (35/314 patients), however, there was no pathologic migration in patients with mild chronic periodontitis. The Chi-square test showed that there was no statistically significant difference between males and females.
Conclusions:
The results of this study confirm that pathologic tooth migration is relatively common among periodontal patients and its prevalence is increased by the severity of periodontal disease.
Key words: Epidemiology, pathologic tooth migration, periodontitis, prevalence
INTRODUCTION
Migrated tooth is defined as the movement of teeth into altered positions in relation to the basal bone of the alveolar process and the adjoining and opposing teeth due to loss of approximating or opposing teeth, occlusal interferences, habits, or inflammatory and dystrophic disease of the attaching and supporting structures of the teeth.[1] Pathologic tooth migration (PTM) is defined as tooth displacement that occurs when the balance among the factors that maintain the physiologic tooth position is disturbed by periodontal disease.[2] PTM is a periodontal disease that has aesthetic effects. Despite the prevalence of pathological migration among periodontal patients, there is limited data on the different aspects of this problem.[3,4] According to some studies, PTM is the one of the most common complaint that leads periodontal patients to dental clinics.[5,6] Case studies and clinical observations on this subject have shown that etiology of pathologic migration is multifactorial and lack of research in this field may be as a result of this complexity.[7,8] PTM may be an early sign of the disease or may be related to gingival inflammation and pocket formation during the progression of the disease. Even during the early stages of the disease, some degree of bone destruction may occur. Diagnosis in its early stages and prevention of severe complications by eliminating the causes has a major advantage. Pathologic migration is also one of the early signs of localized aggressive periodontitis. Pathologic migration occurs most often in the anterior region but may also involve the posterior areas.[2] Moreover, the prevalence of PTM in moderate to severe periodontitis has been studied. Severity of periodontitis can be characterized based on the amount of clinical attachment loss (CAL) as follows: Mild = 1 or 2 mm CAL, moderate = 3 or 4 mm CAL, and severe = ≥5 mm CAL.[9] In teeth with PTM, mean of CAL greater than 3.33 mm have been reported.[5,6,10,11] These measures are related to the moderate and advanced stages of periodontitis and are not related to the early stages. Nevertheless, the prevalence of PTM in mild periodontitis has not yet been studied. This study aims to determine the prevalence of PTM in terms of the patient's periodontal condition and the severity of disease based on measures of CAL.
MATERIALS AND METHODS
This cross-sectional epidemiological study was carried out in the Shiraz Dental School and included 370 recorded files of patients with periodontal disease. The study protocol was approved by the Research Committee of our institution. The number of studied cases belonged to periodontal patients who were referred to our clinic in a 5-year period. Sample size was calculated based on similar papers.[7,10,11] Patients with background characteristic or factors of smoking, diabetes, oral breathing, bruxism, and patients who were simply suffering from gingivitis (without periodontitis) were excluded (n = 56). Patients diagnosed with periodontitis were included in the study. Periodontitis was diagnosed in patients based on clinical examination according to the 1999 American academy of periodontology classification.[9] Severity of periodontitis (mild, moderate, severe) was classified based on the amount of CAL as mentioned previously.[12] CAL was measured as the distance between the cementoenamel junction (CEJ) and the base of the pocket. CAL at 6 points of each tooth was measured by the periodontal probe manually (mesiofacial, midfacial, distofacial, mesiolingual, midlingual, and distolingual). Verification of measurements was performed by expert periodontists. Data were analyzed using PASW Statistics 18 (SPSS Ltd, Hong Kong). Mean and standard deviations were calculated and subjected to t-test and Chi-square test. The level of statistical significance was set at P < 0.05.
RESULTS
Record files of 314 patients with periodontitis (228 females, 86 males; mean age = 37.7 years; age range: 17–70 years) were studied. The mean age of females and males were 36.53 ± 10.93 and 41.02 ± 12.05, respectively, and there were no significant differences. Table 1 summarizes the distribution of patients relative to the severity of the disease. PTM was observed in 35 cases (11.14%) among patients with periodontitis.
Table 1.
Characteristics of patients with periodontitis regarding tooth migration
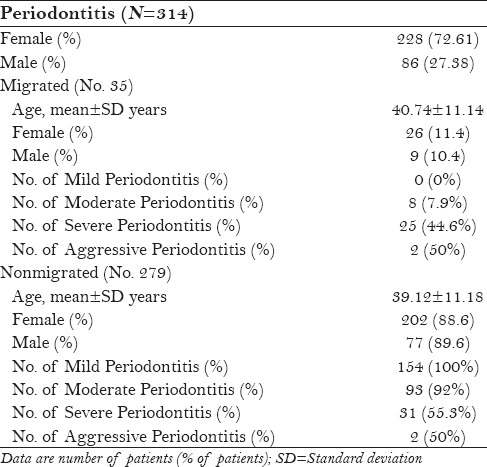
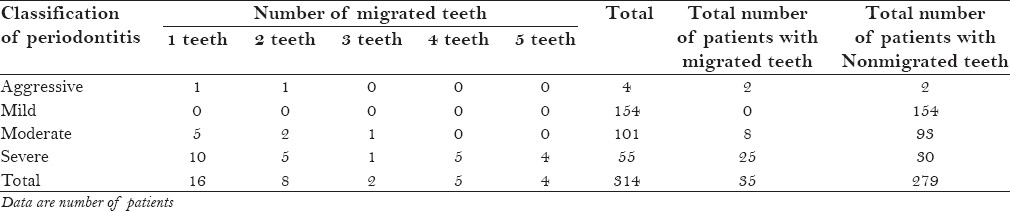
The prevalence of pathologic migration in terms of periodontal status was as follows: Pathologic migration was not observed in patients with mild chronic periodontitis; it was seen in 5.2% of patients with moderate chronic periodontitis; pathologic migration was seen 51% of patients with severe chronic periodontitis whereas it was seen in 50% of patients with aggressive periodontitis (localized and generalized) [Figure 1]. The maximum number of migrated teeth in patients was 5 teeth [Table 2].
Figure 1.
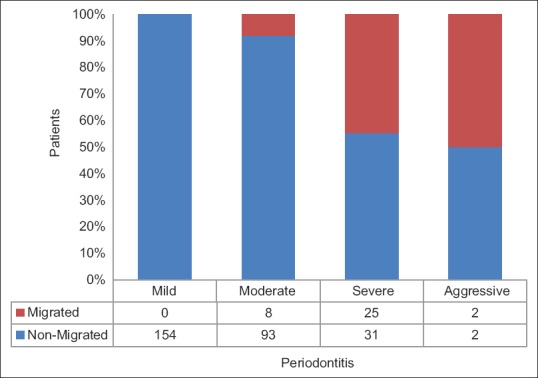
Frequency distribution of number of patients with pathologic tooth migration in different severity of periodontitis
Table 2.
Number of migrated teeth according to the severity of periodontitis in each patient. The diagnostic criteria for the diagnosis and classification of periodontitis are based on the “1999 American academy of periodontology classification”
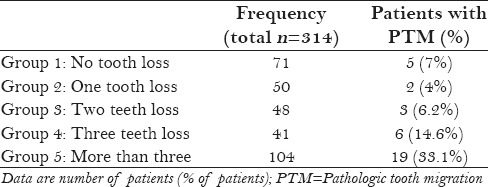
Among the 228 females with periodontitis, PTM was seen in 26 patients (11.40%), and among 86 males with periodontitis, 9 patients (10.46%) had PTM. Table 3 summarizes the distribution of patients based on the number of missing teeth. Patients were classified into five groups based on the number of missing teeth. Nineteen patients (33%) in the five groups (more than 3 teeth loss) had PTM.
Table 3.
Distribution of patients with periodontitis and prevalence of pathologic tooth migration according to the number of lost teeth
DISCUSSION
In this cross-sectional epidemiological study, the prevalence of PTM was studied with respect to the severity of periodontitis. The results of this study suggest that PTM is a common finding in periodontal patients (11.14%), and is also more prevalent in the more advanced stages of periodontal disease. The highest prevalence of PTM was seen in the severe form of chronic periodontitis and aggressive periodontitis.
To the best of our knowledge, this is the first study on the prevalence of PTM in different classes of periodontitis based on the 1999 American academy of periodontology classification.[9] The first study of prevalence of PTM was published in 1997 by Towfighi et al.;[5] the study only included patients with moderate to severe periodontitis. In our study, the prevalence of PTM was studied in different severity of periodontitis including mild periodontitis. Patients with mild periodontitis did not show tooth migration. In mild periodontitis, CAL is expected to be less than 3 mm. The mean of CAL in migrated teeth has been reported to be between 3.3 and 5.5 mm.[5,11,12] According to these studies, it can be assumed that, in the initial stages of periodontal disease, PTM does not occur.
According to some studies, PTM is one of the most common complaints that lead periodontal patients to dental clinics.[5,6] Pathological migration may be an early sign of the disease or may be related to gingival inflammation and pocket formation during the progression of the disease. Normally, there is a balance between the forces that hold the tooth in normal position and occlusal and muscular forces the tooth should normally bear. The weakened supporting tooth is unable to maintain its normal position and moves away from the opposing force.[2] All degrees of pathological migration have been observed and may involve one or more teeth. The early stages of PTM may have been corrected spontaneously after periodontal therapy.[7,8] Treatment of PTM in anterior teeth can be long and complex, and a multidisciplinary approach is often necessary.[13,14,15]
Martinez-Canut et al. carried out a cross-sectional study to determine the prevalence of PTM and assess its relation to bone loss, tooth loss, gingival inflammation, age, lingual interposition, parafunctions, and oral habits.[6] In their study, 852 patients were examined and the diagnosis of PTM was based on the presence of a developing diastema in the upper anterior sextant, which was not present in the past or already existing but was increased. The prevalence of pathologic migration in their study was 55.8%. They reported a significant relationship of PTM with bone loss, missing teeth, and gingival inflammation, whereas significant relationship between PTM and age and parafunction habits and tongue interactions have not been observed. One of the highlights of their study, despite the significant sample of radiographic and clinical records (e.g., assessment of gingival inflammation), was that the patients were examined by only one person. Due to the exclusion of patients with tooth loss in the anterior region, the prevalence of PTM was expected to be under-reported, however, due to subjective criteria utilized in their study, the amount estimated for PTM may be more than normal. Martinez-Canut et al. estimated the prevalence of pathological dental migration to be 55.8%. Prevalence obtained from their study (55.8%) is significantly higher than the results of our research (11.14%), and this may be as a result of the subjective nature of diagnosis of PTM in their study, which can overestimate the results.
The prevalence of PTM in the study by Towfighi et al.[5] was estimated as 30.03% ± 2.5 in a group of patients with moderate to severe periodontitis. In our study, prevalence of PTM in patients with periodontitis (including mild periodontitis) was 11.14%, however, when patients with mild periodontitis were excluded, the prevalence of PTM was 21.73%, which was less different from the results of our research.
The use of archival records in this study can be considered as an advantage because the examiners were been informed about the research.
In the present study, recorded files of patients referred to dental school were used; hence, they are not representative of all segments of the society. Hence, it is suggested that further studies should be carried out on large samples that are representative of all strata of the society.
CONCLUSION
The results of this study suggest that PTM is more prevalent in more advanced stages of periodontal disease. We would like to emphasize that we did not find any tooth migration among patients with mild periodontitis; nevertheless, the prevalence of PTM was seen in the severe form of chronic periodontitis and aggressive periodontitis, indicating that diagnosis and treatment of periodontitis in the early stage could reduce the incidence of pathologic tooth migration. Accordingly, there will be no need for time consuming, complex interdisciplinary treatments.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Boucher CO, Zwemer TJ. Boucher's clinical dental terminology: A glossary of accepted terms in all disciplines of dentistry. 4th ed. St. Louis: Mosby; 1993. [Google Scholar]
- 2.Carranza FA. Periodontal response to external forces. In: Newman MG, Takei HH, Klokkevold PR, Carranza FA, editors. Carranza's Clinical Periodontology. 12th ed. St. Louis: Saunders Elsevier; 2015. pp. 300–8. [Google Scholar]
- 3.Dumitrescu AL, Inagaki K. Occlusal Considerations in Pathogenesis of Periodontal Disease. In: Dumitrescu Al., editor. Etiology and Pathogenesis of Periodontal Disease. Heidelberg: Springer; 2010. pp. 300–6. [Google Scholar]
- 4.Brunsvold MA. Pathologic tooth migration. J Periodontol. 2005;76:859–66. doi: 10.1902/jop.2005.76.6.859. [DOI] [PubMed] [Google Scholar]
- 5.Towfighi PP, Brunsvold MA, Storey AT, Arnold RM, Willman DE, McMahan CA. Pathologic migration of anterior teeth in patients with moderate to severe periodontitis. J Periodontol. 1997;68:967–72. doi: 10.1902/jop.1997.68.10.967. [DOI] [PubMed] [Google Scholar]
- 6.Martinez-Canut P, Carrasquer A, Magán R, Lorca A. A study on factors associated with pathologic tooth migration. J Clin Periodontol. 1997;24:492–7. doi: 10.1111/j.1600-051x.1997.tb00217.x. [DOI] [PubMed] [Google Scholar]
- 7.Rohatgi S, Narula SC, Sharma RK, Tewari S, Bansal P. Clinical evaluation of correction of pathologic migration with periodontal therapy. Quintessence Int. 2011;42:e22–30. [PubMed] [Google Scholar]
- 8.Brunsvold MA, Zammit KW, Dongari AI. Spontaneous correction of pathologic migration following periodontal therapy. Int J Periodontics Restorative Dent. 1997;17:182–9. [PubMed] [Google Scholar]
- 9.Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4:1–6. doi: 10.1902/annals.1999.4.1.1. [DOI] [PubMed] [Google Scholar]
- 10.Costa MR, Silvério KG, Rossa CJ, Cirelli JA. Periodontal conditions of teeth presenting pathologic migration. Braz Oral Res. 2004;18:301–5. doi: 10.1590/s1806-83242004000400005. [DOI] [PubMed] [Google Scholar]
- 11.Rohatgi S, Narula SC, Sharma RK, Tewari S, Bansal P. A study on clinical attachment loss and gingival inflammation as etiologic factors in pathologic tooth migration. Niger J Clin Pract. 2011;14:449–53. doi: 10.4103/1119-3077.91754. [DOI] [PubMed] [Google Scholar]
- 12.Habibagahi Z, Khorshidi H, Hekmati S. Periodontal Health Status among Patients with Behçet's Disease. Scientifica. 2016;2016:7506041. doi: 10.1155/2016/7506041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta S, Deshmukh J, Khatri R, Kulkarni VK, Karthik B. From hopeless to good prognosis: Journey of a failing tooth. J Int Oral Health. 2015;7:53–7. [PMC free article] [PubMed] [Google Scholar]
- 14.Srinath S, Kumar YP, Ravishankar PL, Kalaivani V, Rajapandian K, Archana PM. Retracing capacity of pathologically migrated upper anterior teeth after surgical intervention. J Int Oral Health. 2015;7:75–9. [Google Scholar]
- 15.Jhingta PK, Negi KS, Sharma D, Bhardwaj VK, Vaid S, Nishant N. Interdisciplinary approach for the treatment of pathologic migration in teeth with advanced periodontal disease. SRM J Res Dent Sci. 2015;6:261–4. [Google Scholar]


