Abstract
Osteosarcoma is a very uncommon tumor of the maxillofacial region. Due to the occurrence of the tumor at a young age and its aggressive nature, radical surgery forms the only modality of treatment. A combination of radiotherapy and postoperative chemotherapy has been used for the management of this tumor. A case report of osteosarcoma of the posterior maxilla in an adolescent with a 1-year disease-free follow-up is presented in this report.
Key words: Chemotherapy, osteosarcoma, positive margins, radiation therapy
INTRODUCTION
Osteosarcoma is a primary malignant bone tumor resulting into osteoid or bone and accounts for 23% of craniofacial malignancies.[1,2,3,4,5] Osteosarcomas commonly affect distal femur, proximal humerus parts, and proximal tibia.[1] Osteosarcomas of the jaw account for 2-10% of all sarcomas. It has been observed that osteosarcomas affect more commonly in mandible than in maxilla.[2] In maxilla, lesions are commonly seen at the alveolar ridge, sinus floor, and palate than at the superior aspects (zygoma, orbit).[6] There is no gender predilection, however, some authors consider more predilection in females. Nearly 60% of the osteosarcomas are seen in children and adolescents, and approximately 10% are noted during the third decade of life.[1,7] The etiology is unclear.[8]
The term osteosarcoma refers to the primary malignant neoplasm of heterogeneous nature affecting bone formation or mesenchymal tissues having a histopathological evidence of osteogenic differentiation.[1,8] Various types of osteosarcomas have been defined such as intramedullary low and high grade osteosarcoma, telangiectatic, small cell, and multifocal types. Other types include parosteal, periosteal, intracortical, high-grade surface, extraskeletal, and gnathic osteosarcomas.[9] Chondroblastic osteosarcoma is the most common variant of osteosarcoma of jaw bones, whereas osteoblastic osteosarcoma are common variant reported in the long bones.[4]
Osteosarcoma shows high metastatic rate and can be more aggressive. Jaw region osteosarcomas have a relatively low incidence of metastasis with good prognosis.[6] Because of the occurrence of the tumor at a young age, its aggressive nature, and chances of recurrence, there is need of sound clinical knowledge to diagnose and manage it.[1]
CASE REPORT
A 20 year-old male patient was referred to the maxillofacial surgery department with chief complaint of a rapidly growing swelling in the left upper back tooth region associated with pain. The patient had been noticing the swelling over a period of 2 weeks.
Clinical examination revealed an expansile swelling in the maxillary tuberosity region measuring 5 cm × 3 cm [Figure 1]. The swelling was tender on palpation and smooth in texture. Patient had parasthesia and pain in the involved areas. Facial asymmetry was evident. However, mouth opening was normal. Clinically, there was no regional lymph node involvement. No other relevant family and medical history could be elicited. Patient was advised an orthopantamogram and a cone beam computed tomography (CBCT) scan. A typical sun ray appearance was seen in the CBCT. The tumor was found to involve the entire maxillary sinus and superiorly extending onto the inferior orbital rim. Posterior extension was seen up to the pterygoid plates and medial extension to the lateral wall of the nose [Figure 2].
Figure 1.

Intraoral image showing swelling at the left posterior region of the jaw
Figure 2.

Computed tomography scan image of the maxilla shows maxillary sinus with surrounding soft tissue mass and sunray type of ossification
An incisional biopsy was confirmatory of osteosarcoma. A Weber Fergusson incision was planned for access to the tumor. Adequate access was obtained and resection of the tumor with at least 1 cm clearance was done at all the margins, and the specimen sent for histopathologic examination. Because of the extensive defect and considering the psychological status of the patient, reconstruction of the defect was planned. An anterolateral thigh flap was harvested and used for reconstruction, which also created a lining for the oral cavity [Figure 3]. Patient was on Ryle's tube feeding for 3 weeks. Postoperative healing was uneventful. Histopathologic report confirmed the diagnosis of osteosarcoma which was of the chondroblastic variety. The anterior, posterior, and lateral margins were found to be free of tumor. The superior, inferior, and medial margins shows tumor involvement, and hence, as per the medical oncologist's opinion, postoperative radiotherapy was started. Anterior and lateral portal radiation in combination with chemotherapy was done. Patient has been reviewed for the past 1 year and no evidence of recurrence has been noticed in clinical and radiographic evaluation [Figures 4 and 5].
Figure 3.

Postoperative image showing thigh flap at excised site in the oral cavity
Figure 4.
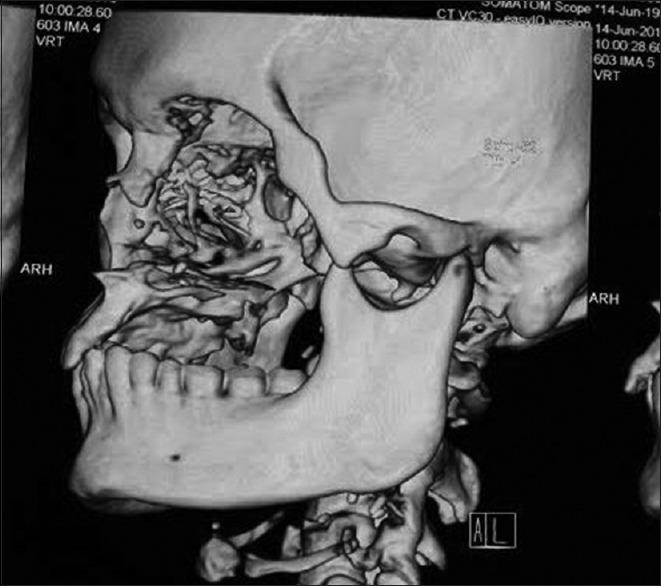
Computed tomography scan of the lateral view showing absence of lesion postoperatively
Figure 5.

Postoperative radiographic view of disease-free state
DISCUSSION
Osteosarcoma commonly affects long bones and rarely affects jaw bones.[1,10] Clinically, osteosarcoma presents with paresthesia, swelling, facial deformity, toothache, persistent pain, loose teeth, and sometimes presents with ulceration, epistaxis, eye problem, and nasal obstruction. Systemic symptoms such as fever, weight loss, and lymphadenopathy are rare. It usually does not metastasize to the lymph node.[1,2,3,10,11] The diagnosis of osteosarcoma is based on clinical, radiographic, and histopathologic features.[1]
Osteosarcomas radiographically show bone expansion. Its radiographic features depend on the interaction of three processes, that is, bone formation and mineralization, bone destruction, and periosteal bone formation.[2,10] It may present as a radiopacity, radiolucency, or of mixed nature with widening of the periodontal ligament space. Radiographically, it presents as classic “sunray or sunburst” appearance due to osteophytic bone production.[1,4] CT is used for definitive diagnosis to determine its extent and to check lung metastasis.[1,2,3]
Tissue biopsy of the lesions helps in definitive diagnosis. Osteosarcoma presents with variable histologic features. Sarcomatous stroma produces osteoid. The stromal cells may be osteoblastic, chondroblastic, and/or fibroblastic.[1] There is a focal area of atypical haphazardly arranged spindle-shaped cells with myxomatous areas. Deeper areas show chronic inflammatory cell infiltrate of lymphocytes, plasma cells, and eosinophils, along with areas of numerous vascular channels.[4]
Surgical excision of osteosarcoma is challenging to the dentist since adequate sectioning of tumor and its reconstruction is difficult, particularly in maxilla, due to its complex anatomy. Osteosarcomas of the jaws are usually managed by wide surgical resection, along with chemotherapy and irradiation.[2]
We have reported a rare case report of osteosarcoma of maxilla, which was confirmed on the basis of CT scan. There was involvement of superior and inferior border of maxilla and possibility of orbital involvement, and hence, surgical excision of the lesion followed by chemotherapy and radiotherapy to protect the orbital region was done.
Usually a temporal flap or radial forearm flap are suggested to correct the deformity after excision of the lesion. Some authors suggested use of soft tissue flap for correction of defect from various parts of the body such as abdominis, rectus femoris, latissimus dorsi, tensor fasciae latae myocutaneous, and arm.[12] In the present case, tumor was excised and the deformity was corrected using thigh flap for esthetic purpose as requested by the patient. This was followed by postoperative chemotherapy in combination of chemotherapy using the following drugs: ifosfamide –200 mg for 4 days, doxorubicin –60 mg on day 1, and cisplatin –40 mg on 1, 2, and 3 days. These drugs were administered once in 21 days. Two-dimensional radiotherapy using60 Cobalt with a total dose of 5500–200 cGy/day in divided doses was administered. The frequency of dosing was 5 days/week for 5.5 weeks. A total of 6-9 cycles were planned and completed. The patient has been reviewed for 1 year, and there was no evidence of recurrence during follow-up visits.
CONCLUSION
Clinical management of osteosarcoma of the maxilla is challenging to the dentist. Early diagnosis and complete resection of tumor along negative margins helps in better prognosis. An attempt has been made to use postoperative radiotherapy in this case due to the presence of positive margins with concomitant use of postoperative chemotherapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We thank Dr. M Varun and department of Oral and Maxillofacial Surgery, Best Dental Science College and Karpaga Vinayagar Institute of Medical Sciences for their support.
REFERENCES
- 1.Sheikh S, Pallagatti S, Aggarwal A, Gupta D, Puri N, Mittal A. Osteosarcoma of maxilla: A case report. J Clin Exp Dent. 2010;2:e117–20. [Google Scholar]
- 2.Nthumba PM. Osteosarcoma of the jaws: A review of literature and a case report on synchronous multicentric osteosarcomas. World J Surg Oncol. 2012;10:240. doi: 10.1186/1477-7819-10-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Praveena NM, Maragathavalli G. Osteosarcoma of maxilla. J Indian Acad Oral Med Radiol. 2012;24:236–8. [Google Scholar]
- 4.George A, Mani V, Sunil S, Sreenivasan BS, Gopakuma D. Osteosarcoma of maxilla: A case of missed initial diagnosis. Oral Maxillofac Pathol J. 2010;1:1–7. [Google Scholar]
- 5.ALQahtani D, AlSheddi M, Al-Sadhan R. Epithelioid Osteosarcoma of the Maxilla: A Case Report and Review of the Literature. Int J Surg Pathol. 2015;23:495–9. doi: 10.1177/1066896915591273. [DOI] [PubMed] [Google Scholar]
- 6.Sivakumar TT, Jeevadhas P, Raghavanpillai VB, Sivaraj S, Joseph AP, Denny SE. Recurrent osteosarcoma of maxilla presenting as fungating mass: A case report. Int J Case Rep Images. 2016;7:149–53. [Google Scholar]
- 7.Mohindra S, Bal AK, Yadav J. Osteosarcoma of the Maxilla Masquerading as Maxillary Mucocele on CT Scan: A Case Report. Clin Rhinol. 2009;2:51–4. [Google Scholar]
- 8.Al-Yahya A, BinAhmed A, Alshammari T. Maxillary Osteosarcoma: Two Case Reports and Literature Review. Oral Health Dent Manag. 2014;13:525–8. [PubMed] [Google Scholar]
- 9.Yildiz FR, Avci A, Dereci O, Erol B, Celasun B, Gunhan O. Gnathic osteosarcomas, experience of four institutions from Turkey. Int J Clin Exp Pathol. 2014;7:2800–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Prasad K, Dexith J, Lalitha RM, Ranganath K, Shuba R, Kumari MK, et al. Maxillary osteosarcoma masquerading as chondromyxoid fibroma: Report of a case. J Maxillofac Oral Surg. 2015;14(Suppl 1):87–92. doi: 10.1007/s12663-012-0338-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Puranik SR, Puranik RS, Ramdurg PK, Choudhary GR. Parosteal osteosarcoma: Report of a rare juxtacortical variant of osteosarcoma affecting the maxilla. J Oral Maxillofac Pathol. 2014;18:432–6. doi: 10.4103/0973-029X.151340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wei FC, Demirkan F, Chen HC, Chen IH, Liao CT, Hau SP. Management of Secondary Soft-Tissue Deficits following Microsurgical Head and Neck Reconstruction by Means of Another Free Flap. Plast Reconstr Surg. 1999;103:1158–66. doi: 10.1097/00006534-199904040-00009. [DOI] [PubMed] [Google Scholar]


