Abstract
With the advances in the field of imaging sciences, new methods have been developed in dental radiology. These include digital radiography, density analyzing methods, cone beam computed tomography (CBCT), magnetic resonance imaging, ultrasound, and nuclear imaging techniques, which provide high-resolution detailed images of oral structures. The current review aims to critically elaborate the use of CBCT in endodontics.
Key words: Cone beam computed tomography, endodontics, radiology
INTRODUCTION
Radiographs in endodontics help in a proper diagnosis, correct treatment planning, and are an important tool in intraoperative procedures and outcome assessments. Conventional intraoral periapical radiography is the most widely used radiographic technique, which gives valuable information regarding the presence, nature and location of periradicular diseases, root canal morphology, and adjacent important anatomical structures.[1,2]
CONVENTIONAL TWO-DIMENSIONAL IMAGING AND ITS LIMITATIONS
Conventional two-dimensional periapical lack three-dimensional data and there is overlapping of important anatomical areas of concern due to superimposition.[3]
Conventional X-rays use an analog film or digital receptor to produce a two-dimensional image of a three-dimensional object.[4,5] The three-dimensional relation of the root(s) to their surrounding anatomical structures, associated periapical lesions, and the canal anatomy within roots may not be precisely assessed with conventional radiographs.[6,7,8,9]
The difficulty in positioning the radiographic film parallel to the long axis of the tooth can cause forelengthening and foreshortening.[9] Certain anatomical features such as zygomatic buttress and maxillary sinus may superimpose on the areas of interest, thus masking the minute diagnostic details.[10]
These can be overcome using three-dimensional imaging techniques, such as conventional computed tomography, and more recently cone beam-computed tomography (CBCT).
CONVENTIONAL COMPUTED TOMOGRAPHY
CT produces three-dimensional image of an object by using a series of two-dimensional image data to mathematically reconstruct a particular cross-section of the object. It is unique in that it provides images of a combination of soft tissues, bone, and blood vessels.[11] The technique of dental CT also known as dentascan was developed by Schwartz et al.[12] The dental CT can be performed with a conventional CT, a spiral CT, or a multislice CT scanner.
Applications of conventional computed tomography
Computed tomography can be applied in various aspects of dentistry.
Limitations of conventional computed tomography
CT in endodontics was not widely accepted due to its high effective dose and relative low resolution.[17]
CONE BEAM COMPUTED TOMOGRAPHY OR CONE BEAM VOLUMETRIC TOMOGRAPHY
In dentistry, where the need for three-dimensional imaging is increasing, CBCT is a promising tool.[18,19] CBCT volume tomography (DVT) is an extraoral imaging system, which can produce three-dimensional scans of the maxillofacial hard tissues.[20,21,22]
CBCT images are attained with the help of a rotating gantry to which an X-ray source and detector are attached. A divergent beam of cone-shaped ionizing radiation is then passed through the area of interest to an X-ray detector on the other side of the patient. The X-ray source and detector revolve around a fixed fulcrum that is immovable within the region of interest (ROI). At the time of exposure sequence, hundreds of planar projection images are generated of the field of view (FOV) in an arc of at least 180°. In a single rotation, CBCT can generate accurate, instant three-dimensional radiographic images. Because CBCT exposure involves the entire FOV, one rotational sequence of the gantry is sufficient to acquire adequate data for the purpose of image reconstruction.[23,24,25]
Its major advantage over conventional CT is the marked reduction in radiation exposure. This is due to rapid scan times, pulsed X-ray beams and state of the art image receptor sensors. CBCT scanners are very simple to use and are approximately the same size of the panoramic radiographic machines, which make them a practical choice for dental practice.[18]
Limited volume CBCT scanners scan relatively smaller data volume that cover just two or three individual teeth, for instance, the 3D Accuitomo (J Morita Corporation, Osaka, Japan) can even capture a 40 mm height by 40 mm diameter volume of data, which is almost similar in dimensions to a conventional periapical radiograph.
The majority of CBCT systems scan the patient in a seated position. Scan times are typically between 10–40 s which is based on the scanner employed and the selected exposure parameters. The actual exposure time is a fraction of this, only approximately 2-5 s.
Each mini-exposure produces a pixel matrix comprising 262,144 (512 × 512) pixels. The attained dataset of these CBCT contains up to 580 individual matrices, which are then reconstructed with the use of advanced configuration computers into three-dimensional datasets, containing almost 100 million voxels (5123).[3]
Sophisticated high-end software processes the obtained data into a format, which resembles those produced by medical CT scanners. Reconstructed images are generated within minutes. The data acquired by CBCT are captured in terms of volumes, which are made up of voxels. With digital imaging, the picture is composed of pixels. In the case of CBCT, voxels are basically three-dimensional versions of pixels. CBCT voxels are isotropic, which means that they are equal in all three dimensions.
Images can be displayed in the three orthogonal planes, axial, sagittal, and coronal simultaneously. Selection of a particular area and moving the cursor over one image also changes the other reconstructed slices. This allows an area to be investigated three-dimensionally in “real time.” Surface rendering, which is a technique for visualizing a geometric representation of a surface from a three-dimensional volume dataset, makes it possible to produce three-dimensional images.
Numerous studies have reassured the geometric precision of CBCT in three dimensions.[26,27,28,29,30]
The quality of images from CBCT scans is better and far superior to helical CT in the assessment of important structures such as cancellous bone, periodontal ligament, lamina dura, enamel, dentine, and pulp.[25]
Cone beam CT scanners are simple to use, less complicated, and therefore less expensive than CT scanners.[31,32]
Limitations of cone-beam computed tomography
CBCT images only have a spatial resolution of 2 line pairs mm−1 compared to the 15–20 line pairs mm−1 of conventional packet film and digital sensors.[33,34] Still, the ability of this technique to reproduce geometrically accurate and reliable images in three dimensions and the elimination of anatomic noise facilitates the assessment of a large number of important features in endodontics.
One technical issue which may influence the quality of images and the diagnostic accuracy of CBCT images includes the beam hardening caused due to high density neighboring anatomical structures such as enamel, implants, metal posts, and metallic restorations.[35,36]
CBCT images are also highly prone to artifacts that affect image quality. X-ray beam that causes beam hardening (i.e. mean energy increases due to low-energy photons that are absorbed instead of high-energy photons) causes two types of artifact: (1) Distortion of metallic objects produced by differential absorption, which is termed as a cupping artifact, and (2) streaks and dark bands that usually appear between two thick objects. The presence of dental metallic restorations in the FOV can result in streaking artifacts. Owing to the fact that the CBCT X-ray beam is heterochromatic which contains lower mean kVp energy in comparison to conventional CT, this type of artifact is more prone to occur. In clinical scenario, CBCT scanners with a limited FOV may produce clearer images with better clarity because they can avoid structures out of the ROI, which are more prone to beam hardening.[37]
When this scattering and beam hardening is associated with the tooth being assessed, the resultant CBCT images may be of minimal diagnostic value.[38,39]
APPLICATIONS OF CONE-BEAM COMPUTED TOMOGRAPHY IN ENDODONTICS
Preoperative assessment
Root canal morphology: The outcome of endodontic treatment depends on the identification of all root canals so that it can be cleaned, shaped, and obturated effectively.[40]
Abella et al., used CBCT to demonstrate a case of a mandibular first molar with a severely curved additional distolingual root (radix entomolaris). They concluded that CBCT imaging can be used for identifying the root canal system and the surrounding structures[41]
Bauman et al. found that the reliability of detection of maxillary molar second mesiobuccal canal (MB2) canal in CBCT scans increased as the resolution improved[42]
In a case report by Loannidis et al., it was concluded that the availability of three-dimensional images increased the opportunity for the precise description of the anatomy of 7 maxillary and mandibular molars with single roots and single canals[43]
The results of an in vitro investigation by Blattner et al. showed that CBCT scanning is a reliable method to detect the MB2 canal when compared with the gold standard method of physical sectioning of the specimen[44]
Fan et al. reported that CBCT method for negotiation combined with careful exploration may provide a reliable method for identifying the anatomy of the canal system and enhancing debridement in these complex canal anatomies[45]
The CBCT scan is a reliable and noninvasive method, which can be used to assess the position of the mandibular canal. The variable position of this between patients suggests the need for CBCT to identify the proximity of the nerve bundle before initiating invasive treatment in this region. Potential differences in mandibular canal position when performing these procedures in this area should be considered[46]
The use of a dental operating microscope (DOM) and CBCT imaging in endodontically challenging cases can facilitate a better understanding of the complex root canal anatomy, which ultimately enables the clinician to explore the root canal system and clean, shape, and obturate it more efficiently.[47]
Dental periapical pathology:
CBCT was accurate in diagnosing the nature of periapical bone loss in chronic lesions, and the diagnostic information attained by CBCT was very useful for treatment planning.[48]
Stavropoulos and Wenzel compared CBCT to digital and film-based intraoral periapical radiography for the detection of periapical bone defects. They found that CBCT has a better diagnostic precision (61%) in comparison with digital (39%) and (44%) conventional radiographs.[49] In a similar study, Ozen et al. compared the detection of chemically-induced periapical lesions by three observers using digital and film-based conventional radiography to two CBCT systems. They concluded that, though detection rates for CBCT were higher, they did not recommend ignoring intraoral radiography for detecting periapical lesions in day-to-day clinical practice due to financial and radiation dose considerations.[50]
Estrela et al. compared the accuracy of CBCT, panoramic, and periapical radiographs from patients with endodontic lesions (1508 teeth) to detect apical periodontitis (AP). They showed that the prevalence of detection of AP was significantly better when CBCT is applied.[39] Estrela et al. formulated and proposed a periapical index using CBCT (CBCTPAI) for the detection of AP. They reported that CBCT imaging assessed 54.2% more AP lesions than using intraoral radiography alone.[51] Patel et al. reported a identification rate of 24.8% and 100% for intraoral radiography in comparison to CBCT imaging.[52]
Root fractures and perforations:
According to Costa et al.,[53] small-volume CBCT scanning showed better accuracy in the detection of horizontal root fracture without a metallic post
Edlundet al.[54] conducted a study which revealed the superior diagnostic accuracy of CBCT for detection of vertical root fracture (VRF)
Shemesh et al. concluded that the risk to misdiagnose strip perforations was high with both CBCT and periapical radiography, however, CBCT scans showed a significant higher sensitivity than periapical radiography[55]
Ozer et al. concluded that CBCT scans were more reliable in detecting simulated VRF, and a 0.2 mm voxel was the best protocol, considering the lower X-ray radiation exposure and good diagnostic accuracy[56]
According to Bueno et al., the accurate management of CBCT images might reveal an abnormality that is unable to be detected in conventional periapical radiography. A map-reading approach reduces problems related to the detection of root perforations near metallic artifacts.[57]
Root resorption:
CBCT provides useful information on the location, size, and nature of root resorptive defects in comparison with that achieved by conventional radiographs[58]
Even though digital intraoral radiography has resulted in an acceptable level of accuracy, the statistically superior accuracy and reliability of CBCT may result in a review of the radiographic techniques that may be used for the assessment of the type of resorptive lesion.[59]
Intraoperative assessment:
Based on the study by Janner et al., an already existing CBCT scan of teeth to be endodontically treated can be used to determine the working length in combination with clinical measurements such as the electronic apex locator (EAL). More studies should evaluate if intraoral radiography for measuring the length of root canals can be avoided when CBCT images are available.[60]
Postoperative assessment:
Liang et al. stated that treatment outcome, length, density, and quality of root fillings, and outcome predictors, as determined with the help of CBCT, may vary from the corresponding values determined with conventional periapical radiography.[61]
Other applications:
CBCT imaging revealed a lower-than-expected prevalence of mucositis adjacent to teeth with apical radiography[62]
A study by Cymerman et al. showed the value of CBCT scanning in evaluating and assessing patients reporting with concurrent sinus and dental complaints[63]
Changes in the maxillary sinuses seem to be associated with periapical pathology in more than 50% of the cases. Maxillary first or second molar teeth are most commonly involved and individual or multiple roots may be suspected in sinusitis. The use of CBCT can also identify changes in the maxillary sinus and possible causes of the sinusitis[64]
A study by Bornstein et al. described the advantages of limited CBCT in treatment planning in mandibular molars prior to apical surgery[65]
Thus, the application of new diagnostic tools, such as CBCT imaging, may provide detailed high-resolution images of oral structures, which may be pivotal in an initial diagnostic hypothesis as well as to plan surgery.[66,67]
EXAMPLES FOR CONE-BEAM COMPUTED TOMOGRAPHY USAGE IN CLINICAL ENDODONTICS
Kottoor et al.[68] reported the nonsurgical endodontic management of a left maxillary molar with three roots and eight root canals. This case of rare anatomic morphology was diagnosed with the help of DOM and confirmed with the use of CBCT images. CBCT axial images showed that both the mesiobuccal and distobuccal root contained a Sert and Bayirli type XV canal, whereas the palatal root showed a Vertucci type II canal configuration. This case report illustrates the importance of CBCT in managing cases with variation in root canal anatomy.
RADIATION DOSE FROM CONE-BEAM COMPUTED TOMOGRAPHY
To assess radiation risk, which is the chance of biological consequences after exposure to radiation in humans, the term effective dose is often employed. Effective dose is a quantitative measurement of the extent of harmful effects on humans when exposed to one kind of radiation. The international standard unit for the measurement effective dose is Sievert. In radiology milli or micro-sievert is generally mentioned.[69]
Effective doses from different CBCT units in comparison to other radiographic techniques in dentistry is shown in Table 1.[69]
Table 1.
Radiation dosage from different imaging modalities
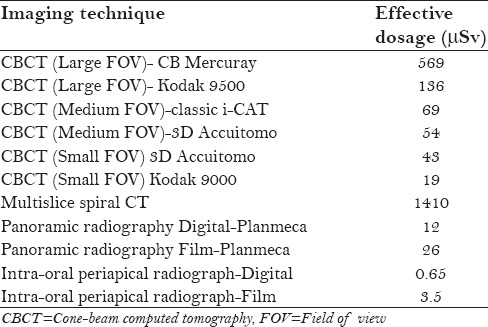
In endodontics, small FOV is sufficient. It is clear from Table 1 that the effective dosage from a small FOV is almost nothing greater than an orthopantomography.
CRITICAL ANALYSIS OF THE USE OF CONE-BEAM COMPUTED TOMOGRAPHY IN ENDODONTICS
The benefits of CBCT should outweigh the potential risks of using it in the field of endodontics. CBCT should be considered only for complex endodontic cases where conventional imaging techniques are not sufficient for diagnosis, treatment planning, and execution. Though the effective dose used in CBCT is less compared to spiral CT, it is still quite high compared to other imaging techniques, and hence may not be free of risk. Multiple angled conventional intraoral digital radiographs are quite sufficient in most situations for understanding the root canal anatomy and its variation.
If a patient is still subjected to CBCT, the question to be answered is, does CBCT imaging give the clinician an accurate imaging of all the intricate details of the root canal system. In real time in-vitro studies, it has been proved that clearing and staining of teeth is a foolproof method to study the microanatomy of the root canal system. As shown in Figure 1, CBCT images are far inferior in dictating the intercanal communications, apical delta, lateral canals, etc., in comparison to Figure 1b. Thus, the justification has to be made for subjecting a patient to radiation exposure if it cannot match the clearing and staining technique used in vitro. In addition, due to beam hardening, CBCT is of limited value in diagnosing vertical root fractures, especially in teeth that are obturated due to the beam hardening caused by the radiopaque obturating material.[70]
Figure 1.
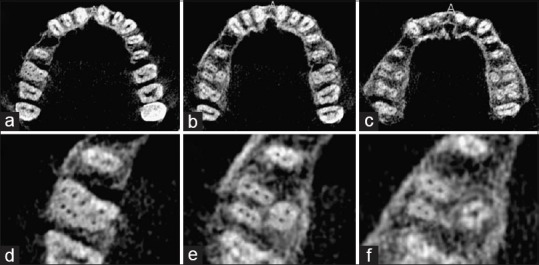
(a-c) Cone-beam computed tomography (CBCT) images of the maxillary arch showing axial sections at the (a) cervical, (b) middle, and (c) apical level. (d-f) Enlarged axial section CBCT images of tooth #14 at the (d) cervical, (e) middle, and (f) apical level showing three roots and eight root canals
CONTRAST ENHANCED CONE-BEAM COMPUTED TOMOGRAPHY
Ruddle et al.[71] injected a radio-opaque dye into the root canal system before subjecting it to a conventional radiography. The authors of this article suggest a similar technique with a novel approach for achieving better images with CBCT. We have experimented the injection of a radio-opaque dye into the canals after cleaning and shaping procedure. The CBCT imaging is performed after this. The images obtained in our pilot study are shown in Figure 2. We could appreciate better visualization of the root canal anatomy including root canal aberrations and variations. Further studies are required before this technique could be recommended for clinical usage [Figure 2].
Figure 2.
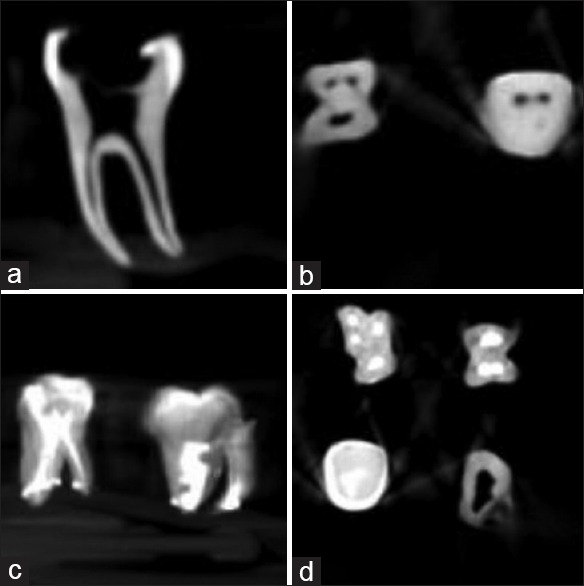
(a and b) Cone beam computed tomography. (c and d) Contrast media injected in the canal differentiates and highlights the complexity of the root canal system
CONCLUSION
Thus, it can be concluded that CBCT is an invaluable diagnostic tool in the field of endodontics. It is especially indicated in situations where a two-dimensional image from a conventional intraoral radiography does not help in understanding the root canal anatomy and its complexity. Though the radiation exposure is less in CBCT, it should be used only in situations where a conventional radiographic technique is not sufficient. Hence, whether CBCT sections reveal the truth completely is still a mystery, but is certainly more valuable than conventional two-dimensional imaging.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Abdinian M, Razavian H, Jenabi N. In vitro Comparison of Cone Beam Computed Tomography with Digital Periapical Radiography for Detection of Vertical Root Fracture in Posterior Teeth. J Dent. 2016;17:84–90. [PMC free article] [PubMed] [Google Scholar]
- 2.Mokhtari H, Niknami M, Mokhtari Zonouzi HR, Sohrabi A, Ghasemi N, Akbari Golzar. Accuracy of Cone-Beam Computed Tomography in determining the root Canal Morphology of Mandibular First Molars. Iran Endod J. 2016;11:101–5. doi: 10.7508/iej.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel S. New dimensions in endodontic imaging: Part 2. Cone beam computed tomography. Int Endod J. 2009;42:463–75. doi: 10.1111/j.1365-2591.2008.01531.x. [DOI] [PubMed] [Google Scholar]
- 4.Beach DA. CBCT Use in Endodontic Diagnosis. Dent Today. 2016;35:80. [PubMed] [Google Scholar]
- 5.Grondahl HG, Huumonen S. Radiographic manifestations of periapical inflammatory lesions. Endo Topics. 2004;8:55–67. [Google Scholar]
- 6.Rawtiya M, Somasundaram P, Wadhwani S, Munuga S, Agarwal M, Sethi P. Retrospective study of root canal configurations of maxillary third molars in Central India population using cone beam computed tomography Part-I. Eur J Dent. 2016;10:97–102. doi: 10.4103/1305-7456.175690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cotti E, Campisi G. Advanced radiographic techniques for the detection of lesions in bone. Endo Topics. 2004;7:52–72. [Google Scholar]
- 8.Cohenca N, Simon JH, Marhtur A, Malfaz JM. Clinical indications for digital imaging in dento-alveolar trauma. Part 2: root resorption. Dent Traumatol. 2007;23(2):105–13. doi: 10.1111/j.1600-9657.2006.00546.x. [DOI] [PubMed] [Google Scholar]
- 9.Whaites E. Essentials of Dental Radiology and Radiography. 4th ed. Philadelphia: Elsevier; 2007. [Google Scholar]
- 10.Patel S, Kanagasingam S, Mannocci F. Cone beam computed tomography (CBCT) in endodontics. Dent Update. 2010;37:373–9. doi: 10.12968/denu.2010.37.6.373. [DOI] [PubMed] [Google Scholar]
- 11.Worthington P, Rubenstein J, Hatcher DC. The role of cone beam computed tomography in the planning and placement of implants. J Am Dent Assoc. 2010;141:19S–24. doi: 10.14219/jada.archive.2010.0358. [DOI] [PubMed] [Google Scholar]
- 12.Schwartz MS, Rothman SL, Rhodes ML, Chafatz N. Computed tomography. Part I: Preoperative assessment of the mandible for endosseous implant surgery. Int J Oral Maxillofac Implants. 1987;2:134–41. [PubMed] [Google Scholar]
- 13.Taşdemir T, Aydemir H, Inan U, Unal O. Canal preparation with Hero 642 rotary Ni-Ti instruments compared with stainless steel hand K-file assessed using computed tomography. Int Endod J. 2005;38:402–8. doi: 10.1111/j.1365-2591.2005.00961.x. [DOI] [PubMed] [Google Scholar]
- 14.Gopikrishna V, Bhargavi N, Kandaswamy D. Endodontic management of a maxillary first molar with a single root and a single canal diagnosed with the aid of spiral CT: A case report. J Endod. 2006;32:687–91. doi: 10.1016/j.joen.2005.10.057. [DOI] [PubMed] [Google Scholar]
- 15.Deepak BS, Subash TS, Narmatha VJ, Anamika T, Snehil TK, Nandini DB. Imaging techniques in endodontics: An overview. J Clin Imaging Sci. 2012;2:13. doi: 10.4103/2156-7514.94227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Youssefzadeh S, Gahleitner A, Dorffner R, Bernhart T, Kainberger FM. Dental vertical root fractures: Value of CT in detection. Radiology. 1999;210:545–9. doi: 10.1148/radiology.210.2.r99ja20545. [DOI] [PubMed] [Google Scholar]
- 17.Ngan DCS, Kharbanda OP, Geenty JP, Darendeliler MA. Comparison of radiation levels from computed tomography and conventional dental radiographs. Aust Orthod J. 2003;19:67–75. [PubMed] [Google Scholar]
- 18.Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006;72:75–80. [PubMed] [Google Scholar]
- 19.Scarfe WC, Farman AG. Cone beam computed tomography: A paradigm shift for clinical dentistry. Aust Dent Pract. 2007:102–10. [Google Scholar]
- 20.Avsever H, Gunduz K, Orhan K, Uzun I, Ozmen B, Egrioglu E, et al. Comparison of intraoral radiography and cone-beam computed tomography for the detection of horizontal root fractures: An in vitro study. Clin Oral Investig. 2014;18:285–92. doi: 10.1007/s00784-013-0940-4. [DOI] [PubMed] [Google Scholar]
- 21.Takeshita WM, Chicarelli M, Iwaki LC. Comparison of diagnostic accuracy of root perforation, external resorption and fractures using cone-beam computed tomography, panoramic radiography and conventional & digital periapical radiography. Indian J Dent Res. 2015;26:619–26. doi: 10.4103/0970-9290.176927. [DOI] [PubMed] [Google Scholar]
- 22.Arnheiter C, Scarfe WC, Farman AG. Trends in maxillofacial cone-beam computed tomography usage. Oral Radiol. 2006;22:80–5. [Google Scholar]
- 23.Hayakawa Y, Sano T, Sukovic P, Scarfe WC, Farman AG. Cone beam computed tomography: A paradigm shift for clinical dentistry. Nippon Dent Rev. 2005;65:125–32. [Google Scholar]
- 24.Farman AG. Image guidance: The present future of dental care. Pract Proced Aesthet Dent. 2006;18:342–4. [PubMed] [Google Scholar]
- 25.Patel S, Dawood A, Whaites E, Pitt Ford T. New dimensions in endodontic imaging: Part 1. Conventional and alternative radiographic systems. Int Endod J. 2009;42:447–62. doi: 10.1111/j.1365-2591.2008.01530.x. [DOI] [PubMed] [Google Scholar]
- 26.Kobayashi K, Shimoda S, Nakagawa Y, Yamamoto A. Accuracy in measurement of distance using cone-beam computerized tomography. Int J Oral Maxillofac Implants. 2004;19:228–31. [PubMed] [Google Scholar]
- 27.Haghanifar S, Moudi E, Mesgarani A, Bijani A, Abbaszadeh N. A comparative study of cone-beam computed tomography and digital periapical radiography in detecting mandibular molars root perforations. Imaging Sci Dent. 2014;44:115–9. doi: 10.5624/isd.2014.44.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ludlow JB, Lester WS, See M, Bailey LJ, Hershey HG. Accuracy of measurements of mandibular anatomy in cone beam computed tomography images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:534–42. doi: 10.1016/j.tripleo.2006.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mischkowski RA, Pulsfort R, Ritter L, Neugebauer J, Brochhagen HG, Keeve E, et al. Geometric accuracy of a newly developed cone-beam device for maxillofacial imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:551–9. doi: 10.1016/j.tripleo.2007.02.021. [DOI] [PubMed] [Google Scholar]
- 30.Stratemann SA, Huang JC, Maki K, Miller AJ, Hatcher DC. Comparison of cone beam computed tomography imaging with physical measures. Dentomaxillofac Radiol. 2008;37:80–93. doi: 10.1259/dmfr/31349994. [DOI] [PubMed] [Google Scholar]
- 31.Baba R, Ueda K, Okabe M. Using a flat-panel detector in high resolution cone beam CT for dental imaging. Dento maxillofacial Radiology. 2004;33:285–90. doi: 10.1259/dmfr/87440549. [DOI] [PubMed] [Google Scholar]
- 32.Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG. Endodontic applications of cone-beam volumetric tomography. J Endod. 2007;9:1121–32. doi: 10.1016/j.joen.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 33.Farman AG, Farman TT. A comparison of 18 different X-ray detectors currently used in dentistry. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:485–9. doi: 10.1016/j.tripleo.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 34.Yamamoto K, Ueno K, Seo K, Shinohara D. Development of dento-maxillofacial cone beam X-ray computed tomography system. Orthod Craniofac Res. 2003;6(Suppl 1):160–2. doi: 10.1034/j.1600-0544.2003.249.x. [DOI] [PubMed] [Google Scholar]
- 35.Mora MA, Mol A, Tyndall DA, Rivera EM. In vitro assessment if local tomography for the detection of longitudinal tooth fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:825–9. doi: 10.1016/j.tripleo.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 36.Soður E, Baksi BG, Gröndahl HG. Imaging of root canal fillings: A comparison of subjective image quality between limited cone beam CT, storage phosphor and film radiography. Int Endod J. 2007;40:179–85. doi: 10.1111/j.1365-2591.2007.01204.x. [DOI] [PubMed] [Google Scholar]
- 37.Scarfe WC, Levin MD, Gane D, Farman AG. Use of cone beam CT in endodontics. Int J Dent. 2009;2009:634567. doi: 10.1155/2009/634567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lofthag-Hansen S, Huumonen S, Gröndahl K, Gröndahl HG. Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:114–9. doi: 10.1016/j.tripleo.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 39.Estrela C, Bueno MR, Leles CR, Azevedo B, Azevedo JR. Accuracy of cone beam computed tomography and panoramic radiography for the detection of apical periodontitis. J Endod. 2008;34:273–9. doi: 10.1016/j.joen.2007.11.023. [DOI] [PubMed] [Google Scholar]
- 40.Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984;58:589–99. doi: 10.1016/0030-4220(84)90085-9. [DOI] [PubMed] [Google Scholar]
- 41.Abella F, Mercadé M, Duran-Sindreu F, Roig M. Managing severe curvature of radix entomolaris: Three-dimensional analysis with cone beam computed tomography. Int Endod J. 2011;44:876–85. doi: 10.1111/j.1365-2591.2011.01898.x. [DOI] [PubMed] [Google Scholar]
- 42.Bauman R, Scarfe W, Clark S, Morelli J, Scheetz J, Farman A. Ex vivo detection of mesiobuccal canals in maxillary molars using CBCT at four different isotropic voxel dimensions. Int Endod J. 2011;44:752–8. doi: 10.1111/j.1365-2591.2011.01882.x. [DOI] [PubMed] [Google Scholar]
- 43.Loannidis K, Lambrianidis T, Beltes P, Besi E, Malliari M. Endodontic Management and Cone-beam Computed Tomography Evaluation of Seven Maxillary and Mandibular Molars with Single Roots and Single Canals in a Patient. J Endod. 2011;379:103–9. doi: 10.1016/j.joen.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 44.Blattner TC, George N, Lee CC, Kumar V, Yelton CD. Efficacy of Cone-Beam Computed Tomography as a Modality to Accurately Identify the Presence of Second Mesiobuccal Canals in Maxillary First and Second Molars: A Pilot Study. J Endod. 2010;36:867–70. doi: 10.1016/j.joen.2009.12.023. [DOI] [PubMed] [Google Scholar]
- 45.Fan B, Min Y, Lu G, Yang J, Cheung GS, Gutman JL. Negotiation of C-Shaped Canal Systems in Mandibular Second Molars. J Endod. 2009;35:1003–8. doi: 10.1016/j.joen.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 46.Kovisto T, Ahmad M, Bowles WR. Proximity of the Mandibular Canal to the Tooth Apex. J Endod. 2011;37:311–5. doi: 10.1016/j.joen.2010.11.030. [DOI] [PubMed] [Google Scholar]
- 47.Kottoor J, Velmurugan N, Surendran S. Endodontic Management of a Maxillary First Molar with Eight Root Canal Systems Evaluated Using Cone-beam Computed Tomography Scanning: A Case Report. J Endod. 2011;37:715–9. doi: 10.1016/j.joen.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 48.Yoshioka T, Kikuchi I, Adorno C.G, Suda H. Periapical bone defects of root filled teeth with persistent lesions evaluated by cone-beam computed tomography. Int Endod J. 2011;44:245–52. doi: 10.1111/j.1365-2591.2010.01814.x. [DOI] [PubMed] [Google Scholar]
- 49.Stavropoulos A, Wenzel A. Accuracy of cone beam dental CT, intraoral digital and conventional film radiography for the detection of periapical lesions. An ex vivo study in pig jaws. Clin Oral Investig. 2007;11:101–6. doi: 10.1007/s00784-006-0078-8. [DOI] [PubMed] [Google Scholar]
- 50.Ozen T, Kamburoðlu K, Cebeci AR, Yüksel SP, Paksoy CS. Interpretation of chemically created periapicallesions using 2 different dental cone-beam computerized tomography units, an intraoral digital sensor, and conventional film. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:426–32. doi: 10.1016/j.tripleo.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 51.Estrela C, Bueno MR, Azevedo BC, Azevedo JR, Pécora JD. A new periapical index based on cone beam computed tomography. J Endod. 2008;34:1325–31. doi: 10.1016/j.joen.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 52.Patel S, Dawood A, Mannocci F, Wilson R, Pitt Ford T. Detection of periapical bone defects in human jaws using cone beam computed tomography and intraoral radiography. Int Endod J. 2009;42:507–15. doi: 10.1111/j.1365-2591.2008.01538.x. [DOI] [PubMed] [Google Scholar]
- 53.Costa FF, Gaia BF, Umetsubo OS, Cavalcanti MG. Detection of Horizontal Root Fracture with Small-volume Cone-Beam Computed Tomography in the Presence and Absence of Intracanal Metallic Post. J Endod. 2011;37:1456–9. doi: 10.1016/j.joen.2011.05.040. [DOI] [PubMed] [Google Scholar]
- 54.Edlund M, Nair MK, Nair UP. Detection of Vertical Root Fractures by Using Cone-beam Computed Tomography: A Clinical Study. J Endod. 2011;37:768–72. doi: 10.1016/j.joen.2011.02.034. [DOI] [PubMed] [Google Scholar]
- 55.Shemesh H, Cristescu RC, Wesselink PR, Wu MK. The Use of Cone-beam Computed Tomography and Digital Periapical Radiographs to Diagnose Root Perforations. J Endod. 2011;37:513–6. doi: 10.1016/j.joen.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 56.Ozer SY. Detection of Vertical Root Fractures by Using Cone Beam Computed Tomography with Variable Voxel Sizes in an In vitro Model. J Endod. 2011;37:75–9. doi: 10.1016/j.joen.2010.04.021. [DOI] [PubMed] [Google Scholar]
- 57.Bueno MR, Estrela C, Fiqueiredo JA, Azevedo BC. Map-reading Strategy to Diagnose Root Perforations Near Metallic Intracanal Posts by Using Cone Beam Computed Tomography. J Endod. 2011;37:75–90. doi: 10.1016/j.joen.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 58.Bhuva B, Barnes JJ, Patel S. The use of limited cone beam computed tomography in the diagnosis and management of a case of perforating internal root resorption. Int Endod J. 2011;44:777–86. doi: 10.1111/j.1365-2591.2011.01870.x. [DOI] [PubMed] [Google Scholar]
- 59.Patel S, Dawood A, Wilson R, Horner K, Mannocci F. The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography – An in vivo investigation. Int Endod J. 2009;42:831–8. doi: 10.1111/j.1365-2591.2009.01592.x. [DOI] [PubMed] [Google Scholar]
- 60.Janner SFM, Jeger FB, Lussi A, Bornstein MM. Precision of Endodontic Working Length Measurements: A Pilot Investigation Comparing Cone-Beam Computed Tomography Scanning with Standard Measurement Techniques. J Endod. 2011;37:1046–51. doi: 10.1016/j.joen.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 61.Liang YH, Li G, Wesselink PR, Wu MK. Endodontic Outcome Predictors Identified with Periapical Radiographs and Cone-beam Computed Tomography Scans. J Endod. 2011;37:326–31. doi: 10.1016/j.joen.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 62.Nurbakhsh B, Friedman S, Kulkarni GV, Basrani B, Lam E. Resolution of Maxillary Sinus Mucositis after Endodontic Treatment of Maxillary Teeth with Apical Periodontitis: A Cone-Beam Computed Tomography Pilot Study. J Endod. 2011;37:1504–11. doi: 10.1016/j.joen.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 63.Cymerman JJ, Cymerman DH, O’Dwyer RS. Evaluation of Odontogenic Maxillary Sinusitis Using Cone-Beam Computed Tomography: Three Case Reports. J Endod. 2011;37:1465–9. doi: 10.1016/j.joen.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 64.Maillet M, Bowles WR, McClanahan SL, John MT, Ahmad M. Cone-beam Computed Tomography Evaluation of Maxillary Sinusitis. J Endod. 2011;37:753–7. doi: 10.1016/j.joen.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 65.Bornstein MM, Lauber R, Sendi P, Arx TV. Comparison of Periapical Radiography and Limited Cone-Beam Computed Tomography in Mandibular Molars for Analysis of Anatomical Landmarks before Apical Surgery. J Endod. 2011;37:151–7. doi: 10.1016/j.joen.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 66.Rawi BA, Hassan B, Vandenberge B, Jacobs R. Accuracy assessment of three-dimensional surface reconstructions of teeth from Cone Beam Computed Tomography scans. J Oral Rehabil. 2010;37:352–8. doi: 10.1111/j.1365-2842.2010.02065.x. [DOI] [PubMed] [Google Scholar]
- 67.Faitaroni LA, Bueno MR, Carvalhosa AA, Mendonca EF, Estrela C. Differential Diagnosis of Apical Periodontitis and Nasopalatine Duct Cyst. J Endod. 2011;37:403–10. doi: 10.1016/j.joen.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 68.Kottoor J, Velmurugan N, Surendran S. Endodontic management of a maxillary first molar with eight root canal systems evaluated using cone-beam computed tomography scanning: A case report. J Endod. 2011;37:715–9. doi: 10.1016/j.joen.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 69.Li G. Patient radiation dose and protection from cone-beam computed tomography. Imaging Sci Dent. 2013;43:63–9. doi: 10.5624/isd.2013.43.2.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chang E, Lam E, Shah P, Azarpazhooh A. Cone-beam Computed Tomography for Detecting Vertical Root Fractures in Endodontically Treated Teeth: A Systematic Review. J Endod. 2016;42:177–85. doi: 10.1016/j.joen.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 71.Ruddle CJ, Machtou P, West JD. Endodontic canal preparation: innovations in glide path management and shaping canals. Dent Today. 2014;33(7):118–23. [PubMed] [Google Scholar]


