Abstract
This review assessed the most up-to-date literature on the accuracy of detecting vertical root fractures (VRFs] using the currently available diagnostic imaging methods. In addition, an overview of the biological and clinical aspects of VRFs will also be discussed. A systematic review of the literature was initiated in December of 2015 and then updated in May of 2016. The electronic databases searched included PubMed, Emabse, Ovid, and Google Scholar. An assessment of the methodological quality was performed using a modified version of the quality assessment of diagnostic accuracy studies tool. Twenty-two studies were included in this systematic review after applying specific inclusion and exclusion criteria. Of those, 12 favored using cone beam computed tomography (CBCT) for detecting VRF as compared to periapical radiographs, whereas 5 reported no differences between the two methods. The remaining 5 studies confirmed the advantages associated with using CBCT when diagnosing VRF and described the parameters and limitations associated with this method, but they were not comparative studies. In conclusion, overwhelming evidence suggests that the use of CBCT is a preferred method for detecting VRFs. Nevertheless, additional well controlled and high quality studies are needed to produce solid evidence and guidelines to support the routine use of CBCT in the diagnosis of VRFs as a standard of care.
Key words: Accuracy, cone beam computed tomography, periapical radiographs, vertical root facture
INTRODUCTION
Vertical root fractures (VRFs) present extremely challenging diagnostic tasks in dental practice. They are defined as fractures that extend longitudinally from the root apex to the crown.[1] The prevalence of VRFs after root canal treatment varies between 3.7% and 30.8%.[1,2] Moreover, VRFs can also be caused by physical and occlusal trauma, pathological resorption, and repetitive parafunctional habits in addition to iatrogenic complications during and after endodontic treatment.[1]
The detection of these fractures is usually challenging for clinicians, especially when the results from the typical clinical diagnostic tests are inconclusive. In most clinical settings, clinicians rely on findings from both clinical and radiographic tests to make the diagnosis. Unfortunately, some patients must still undergo exploratory surgery to determine if a VRF has actually occurred. Thus, there is a pressing need to find less invasive and more reliable methods to diagnose VRFs. Diagnostic imaging plays a pivotal role in the diagnosis of VRFs. Periapical radiographs (PRs) at different horizontal and vertical positions have been used for many years to aid in the diagnosis of VRFs because of their high spatial resolution, however, these two-dimensional (2D) images are inherently plagued with overlapping structures, which makes the diagnostic task especially challenging. Moreover, fractures are generally difficult to detect radiographically unless the X-ray beam is parallel to the line of fractures.[3] Therefore, clinicians often have to rely on indirect radiographic signs, such as perilateral radiolucencies and angular resorption of the crestal bone, for the indication of VRFs.[3] Cone beam computed tomography (CBCT) is currently being utilized with increasing frequency to detect VRFs because it provides submillimeter spatial resolution and three-dimensional (3D) visualization.
This review assessed all of the up-to-date literature regarding the accuracy of the currently available diagnostic imaging methods used to detect VRFs. In addition, an overview of the biological and clinical aspects of VRFs is also presented.
MATERIALS AND METHODS
The methodology used in this systematic review will be described in the following sections: (1) studies considered for this systematic review, (2) a literature search strategy, (3) the selection criteria, and (4) the target condition.
Types of studies
Case reports, case-series, clinical studies, in vitro and in vivo studies, and comparative studies were considered for this review.
Literature search strategy
For this review, the following electronic databases were searched: PubMed, Embase, Ovid, and Google Scholar. The following key words and subject heading terms were used in combination with the listed Boolean operators: “Cone Beam Computed Tomography,” OR “CBCT,” AND “Vertical root fracture,” OR “VRF,” AND “Diagnosis.” After the studies that matched these search terms were identified, duplications and unrelated studies were removed. The following inclusion and exclusion criteria were applied to narrow the focus on the appropriate research studies.
Selection criteria
Inclusion criteria
Studies that mention CBCT as a diagnostic tool for the detection of VRFs
In vitro or in vivo studies performed on human permanent teeth
Clinical studies that have verified VRFs by clinical and surgical exploration
Studies that have mentioned all exposure parameters for both radiographs and CBCT (e.g., kVp, mA, field of view, voxel size, and resolution) for image acquisition
Studies comparing CBCT and different digital and conventional radiographic techniques
Studies in which accuracy parameters, such as sensitivity, specificity, or receiver operating characteristic curves, were used (i.e., at least 1 of them).
Exclusion criteria
Unrelated studies (e.g., studies on jaw fractures, systemic disease, or regenerative endodontics)
Studies on horizontal root fractures
Studies focused on the management of tooth fractures
Studies that mention CBCT to evaluate manifestations other than VRFs
Studies associated with cracked teeth and craze lines.
Target condition
The target condition was VRFs in any permanent, endodontically, or non-endodontically treated tooth. After applying the above strategy, only 22 studies met our criteria and were thus included in this systematic review [Figure 1].
Figure 1.
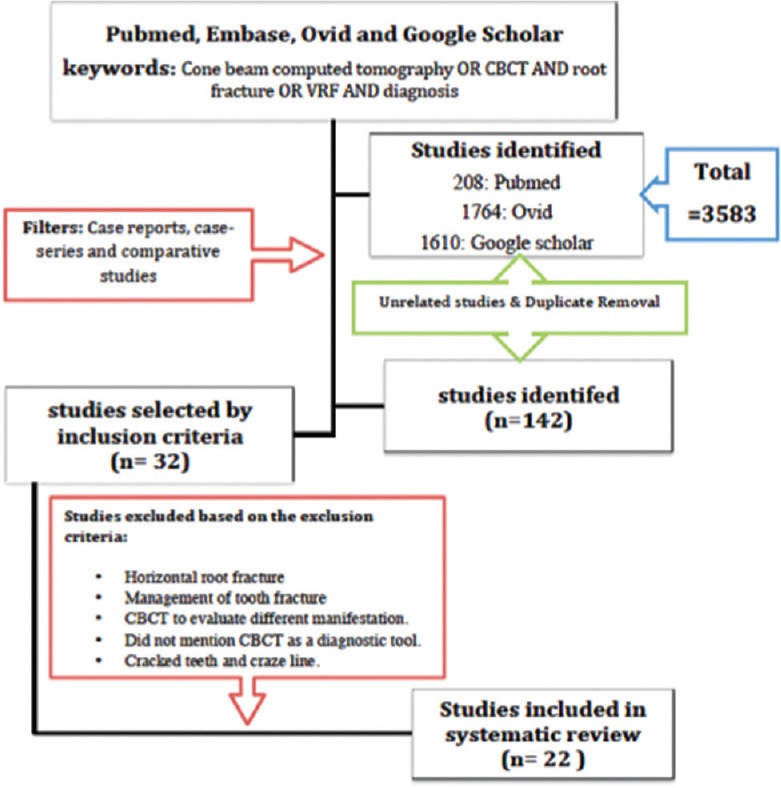
Flow chart of the search strategy used in this review
Biological effect
VRFs can be either complete or incomplete fractures of the tooth and usually occur in patients over 40 with endodontically treated teeth.[4] A complete VRF is a catastrophic event for a patient, and frequently can only be treated by extraction of the affected tooth. A VRF is more likely to occur in a tooth that has been previously extensively treated, such as a tooth with a compound restoration, a tooth that had too much dentine removed during a root canal treatment, or a compaction of a canal filling material during an endodontic treatment.[5] Preventive measures have been suggested by endodontists to reduce the possibility of developing a VRF during and after treatment. This includes using careful and conservative endodontic therapy approaches, such as performing conservative access cavities and avoiding extensive and over-tapered root canal preparations.[6,7] In addition, patients involved in sports or suffering from bruxism are recommended to use mouth guards when playing the sport of choice or sleeping, respectively. Furthermore, instructing the patient to avoid chewing, particularly hard items, such as ice or other hard foods, is important until these teeth receive the proper coverage after root canal treatment.[8]
Khasnis et al. investigated the difficulties in detecting VRFs in both endodontically treated and healthy teeth. Yet, clinical detection of VRFs is likely to be done by an endodontist rather than a general dentist since VRFs usually involve endodontically treated teeth.[4] Khasnis et al. discussed and recommended the use of CBCT due to its accuracy in detecting VRFs.
Llena-Puy et al. conducted a study investigating the theory that endodontically treated teeth were more susceptible to VRFs than healthy teeth.[9] They examined endodontically treated teeth with VRFs and found that the mean time for teeth to develop a VRF was 54 months despite the presence or absence of previous endodontic work.
Mullally and Ahmed studied the difficulties associated with diagnosing VRFs as well as the resulting challenges associated with tooth loss. They stated that VRFs should be considered whenever a periodontal crisis is found in an unusual site.[8] As such, early detection and extraction of the affected teeth will maintain proper alveolar bone levels for future implants.[4] On the other hand, other researchers are still trying to produce innovative ideas as alternative treatments for VRFs. For example, Haddrosek and Dammaschke reported the case of a 78-year-old woman who presented with a VRF. Her existing root canal filling was replaced by a calcium-based cement, and the tooth was stabilized with a composite and titanium splint after replantation. At a 24-month follow-up, the tooth was stable, and the gums had reattached to the tooth.[10] In addition, Nizam et al. reported that adhesive cementation of VRFs followed by intentional replantation can be a successfully alternative treatment plan for extraction in maxillary single-rooted teeth.[11]
Psychological effect of losing teeth
Unfortunately, the most common treatment option for VRFs seems to be extraction.[2,12] Thus, losing teeth can be a tragic life event; indeed, the long-term emotional effect may be underestimated. It not only affects the financial status of the patient it also involves pain and sometimes depression.
Davis et al. reported that most of the patients who had lost their teeth had suffered from emotional difficulties in terms of accepting their tooth loss. These patients were also more likely to have low confidence, feel inhibited in daily activities, and be less able or willing to accept the change in their facial shape due to the extraction.[13]
Similarly, Roohafza et al. reported an association between psychological factors such as depression, anxiety, and stress with tooth loss.[14] In addition, Okoje et al. also reported that only 40.9% of the patients were prepared for the emotional effect associated with the loss of their teeth. The emotional effects following tooth loss were reported as sadness, depression, feelings of aging, and the feeling that something was lost from their body; only a few respondents reported feeling unconcerned about their tooth loss.[15]
When considering the relevance of tooth loss from a psychological perspective combined with the biological effect of losing a tooth due to a VRF, we realize that the clinician and patient need to approach the problem holistically and not just from a purely clinical standpoint. For example, certain available treatment options may help the patient better transition to accept their tooth loss.
Symptoms and diagnosis
A VRF can cause a patient severe, deep, traumatic pain, which may be described as shooting or throbbing; moreover, this pain is usually surprising and frustrating. As previously indicated, there is a higher prevalence of VRFs amongst root canal treatment patients, though it is not the only procedure that can leave teeth vulnerable. Trauma, pathological resorption, and repetitive parafunctional habits are other predisposing factors.[16] In addition, the number of canals per root, and the type of the final irrigation and obturation materials can all be factors that influence the prevalence of VRFs in endodontically treated teeth.[17,18] Pain alone or a single event cannot explain the presence of VRFs as other potential causes can cause similar symptoms. Thus, ruling out these other potential issues may help in the diagnostic procedure to ensure that the patient receives the appropriate treatment more quickly.
Seo et al. analyzed the characteristics and the associated factors of fractured teeth to better understand and aid in correctly diagnosing these fractures. Their results revealed that fractured teeth displayed sensitivity to a standard bite test (82%). Most VRFs occurred in heavily restored teeth (72%) as compared to healthy ones (28%). The use of non-bonded restorations (i.e., gold or amalgam) increased the risk of VRF. The overall conclusion of their study was that the bite test was the best method for reproducing symptoms.[19]
Interestingly, there are demographic factors associated with VRFs. Teeth with VRFs have fractures that can extend through enamel, dentin, pulp, and down the long axis of the tooth. Cohen et al. investigated several factors and looked for statistical correlations for the presence of VRFs. Their findings indicated that VRFs are statistically more prevalent in mandibular molars and maxillary premolars. They can mostly be associated with pain to percussion, extensive restorative work, periradicular bone loss, and seem to occur more often in females and older patients.[5] Therefore, clinicians should remain aware of these factors when attempting to assess undiagnosed cases of VRFs.
In addition, to correctly diagnose VRFs, the clinician needs to understand the pathogenesis of the condition.[12] Clinical presentation and 2D radiographs were both deemed to be inadequate for confirmation of the diagnosis, especially when the correlation between the signs and symptoms and the severity of the symptoms are not sufficient for a definite diagnosis.[1,20] Hence, new approaches and methods are needed to better improve our diagnostic approach for VRFs. Moreover, treatment of root fractures depends on a number of factors, such as the position of the fracture line, mobility of the tooth, and pulpal status. Thus, treating such cases requires a multidisciplinary approach in order to achieve complete rehabilitation of the affected tooth.
Cone beam computed tomography as a novel approach to detect vertical root fractures
Diagnostic imaging is continually evolving and provides consistently accurate images and information. CBCT is one such example of a relatively new imaging technique that has overcome some of the inherent limitations of conventional radiographs, such as overlapping structures and limited spatial and contrast resolution.[16] Consequently, clinicians have gravitated toward this imaging method to assist them in challenging diagnostic tasks such as detecting VRFs.[1]
There is growing evidence that CBCT has superior accuracy in detecting VRFs as compared to conventional radiographs.[1,16] However, this accuracy is still limited for detecting small hairline fractures as compared to thick and displaced VRFs.[9] In addition, the specificity and sensitivity of the ability to detect VRFs varies depending upon several factors, including the make and model of the CBCT unit used.[21] Moreover, root canal filling materials usually create image artifacts that deteriorate the quality of the images, thereby reducing their accuracy. In 2015, Valizadeh et al. investigated this issue and tested teeth with posts that were scanned in five different positions. They concluded that the center-scanned position was found to be the only position that had reliable sensitivity for detecting VRFs.[22] Moreover, note that advances in radiology must also be accompanied by advanced user-level expertise with the specific diagnostic task.
The accuracy of cone beam computed tomography for detecting vertical root fractures
Before the introduction of volumetric CBCT imaging into the field of dentistry, 2D conventional PRs were routinely used for the task of detecting VRFs despite their limitations. Other 3D imaging techniques that were explored for this diagnostic task included conventional computed tomography (CT) and tuned-aperture CT (TACT). However, the cost and radiation risk associated with these 3D imaging modalities limited their use and application.[1] In 2010, Varshosaz et al. reported that 3D images from CBCT were significantly superior at detecting VRFs as compared to conventional PRs.[1] Then, in 2012, Khedmat et al. also concluded that CBCT is more accurate and sensitive than digital radiography (DR) in the detection of VRFs (P < 0.05).[23] More recently, Komatsu et al. investigated the 3D images from CBCT of 32 maxillary pre-molars, of which 16 had a fractured root and 16 did not. They found that the CBCT images offer a high degree of accuracy in detecting teeth with VRFs.[24] Takeshita et al. also reported higher sensitivity and specificity for CBCT images as compared to PRs based on the results of their study, which demonstrated a significant increase in the accuracy of CBCT with and without a metal post (MP) (0.953 vs 0.753) and (0.778 vs 0.956), respectively.[16]
The issue of an accurate diagnosis of VRF is highlighted repeatedly in the literature due to the critical and urgent nature of obtaining an early diagnosis to prevent treatment complications and improve clinical outcomes. Imaging plays a pivotal role in this diagnostic task, however, the risk of radiation exposure remains a concern to both clinicians and patients alike. With regards to the radiation risk associated with this technique, CBCT imaging used especially for endodontic purposes can be modified to deliver a reduced radiation dose that carries a significantly lower risk when compared to other volumetric imaging options.[16] However, there is always a tradeoff between radiation exposure and image quality. Thus, the goal of much of the current research is to reduce the radiation dose of the CBCT imaging while maintaining imaging quality. One technique was to decrease the level of resolution to some degree while still balancing the need for clarity.[1] However, there is still ongoing debate whether CBCT can be used as the standard of care for detecting VRFs.[25]
RESULTS
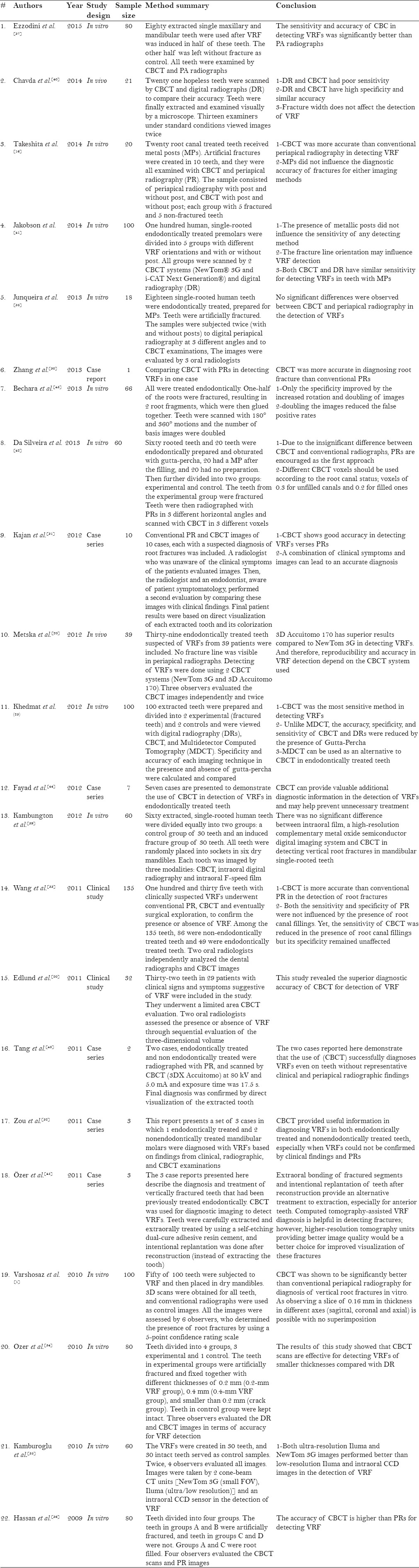
Twenty-two studies were included in the systematic review after applying the inclusion and exclusion criteria. Of those, 12 favored using CBCT for the detections of VRFs as compared to periapical radiographs, whereas 5 reported no differences between the two techniques. The remaining 5 studies confirmed the advantages of using CBCT in diagnosing VRFs and looked into parameters and limitations associated with this diagnostic procedure, but they were not comparative studies. A description and summary of all included studies are presented in Tables 1 and 2.
Table 1.
Summary of included studies type
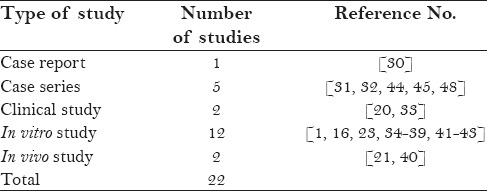
Table 2.
Description and summary of all included literature data
DISCUSSION
This systematic review described the best way to image and detect VRFs based on the best current literature. Twenty-two studies were considered in this review after applying the inclusion and exclusion criteria, however, these studies have a high level of heterogeneity. This heterogeneity may come from several factors, including the size of examined samples; the different CBCT types used; the different digital or conventional PRs used; the different testing parameters; whether the study was conducted in vitro, ex vivo, or in clinical settings; the population included in each study; and the expertise of the study evaluator.
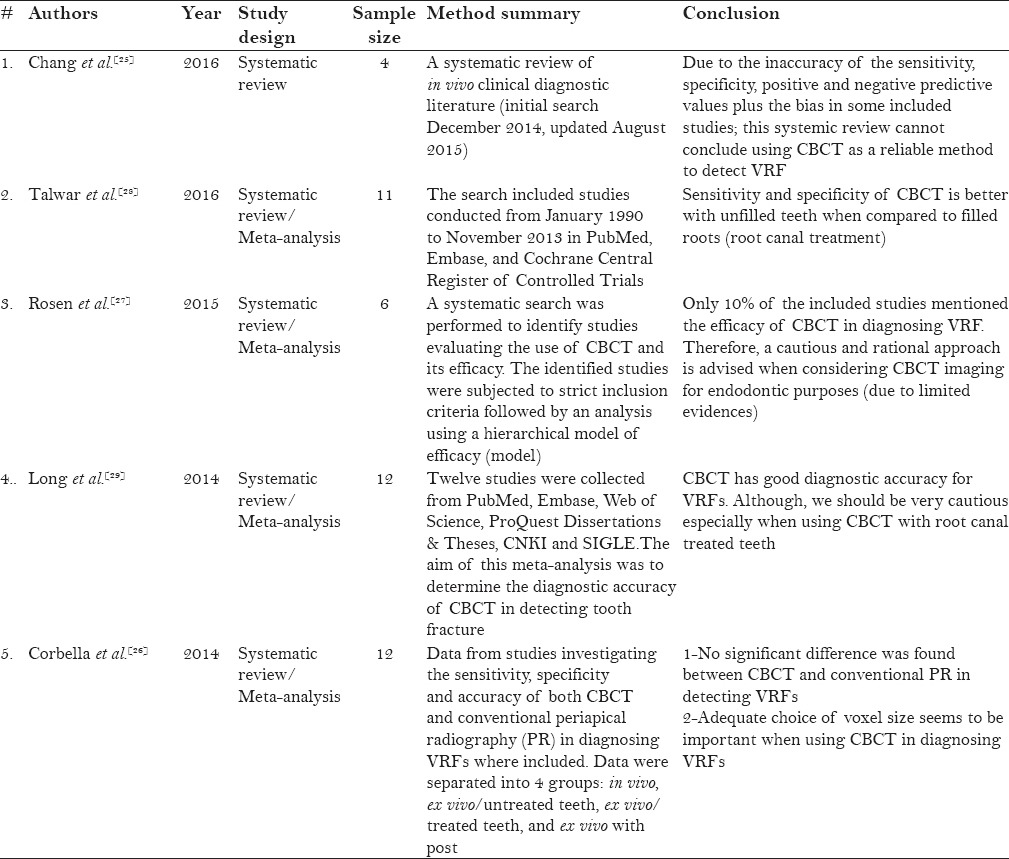
Several systematic reviews and meta-analyses had been conducted, and many have reached controversial conclusions regarding the use of CBCT for detecting VRFs [Table 3]. The recently published review by Chang et al. concluded that there is still deficiency in the current evidence to support the use of CBCT as a reliable method to diagnose VRFs.[25] In addition, the systematic reviews of Corbella et al. and Rose et al. also concluded that CBCT has no superiority compared to conventional radiographs for detecting VRFs, thereby indicating that there is still not sufficient evidence to advocate the use of CBCT as a reliable tool to diagnose VRFs.[26,27] In contrast, Talwar et al. reported that CBCT has better sensitivity and specificity compared to PRs in detecting VRFs.[28] Furthermore, Long et al. also reported that CBCT has a high diagnostic accuracy for VRFs.[29] This clearly shows discrepancies in the conclusions reached by systematic/meta-analysis reviews to date. This may be mainly due to the differences in applied inclusion and exclusion criteria in addition to the authors’ opinions on the statistical tests used. When examining our included studies individually, 12 studies favored the use of CBCT as compared to PRs in detecting VRFs,[1,16,21,23,30,31,32,33,34,35,36,37] whereas 5 studies concluded that there were no significant differences between CBCT and PRs in detecting VRFs and stated that both imaging modalities has their own set of limitations.[38,39,40,41,42] In addition, the remaining 5 studies were not comparative studies; however, they investigated the usefulness of CBCT for the detection of VRFs while using different parameters and conditions. They all agreed upon the advantages and accuracy of using CBCT for diagnosing VRFs. However, the type of CBCT used, the voxel size, the tooth condition, the fracture position, the number of rotations and image doubling, and the examiners (i.e. their clinical ability with the CBCT and the interpretation of the images) were all important factors that affected the accuracy of the VRF detection.[21,41,43,44,45] Our results clearly reveal the controversy in the literature; however, there is, indeed, a strong trend toward supporting the use of CBCT for the detection and diagnoses of VRFs. Hence, more studies are needed to formulate the proper guidelines and parameters of how and when CBCT can be used and considered as an accurate and reliable tool to diagnose VRFs. Horner et al. discussed some of these aspects that must be addressed by practicing dentists.[46]
Table 3.
Description and summary of all current systematic and meta-analysis reviews in the literature
Takeshita et al. stated that the accurate diagnosis of a VRF depends on a careful clinical examination, a complete evaluation of the case, and on an imaging examination that assessed the integrity of the bone and the dental structure.[16] In addition, the detection of a VRF is not only influenced by the type of imaging examination (i.e., conventional radiography or CBCT) but also by the presence of the material used in the root canal (e.g., metal posts, filling material, and the remaining restorative material), which can hinder the quality of the CBCT images.[16]
According to Chang et al., from a national health perspective, “the financial burden to the patient and/or the health-care system must also be considered.”[25] In Ontario, Canada, a small (i.e., <8-cm diameter) field-of-view CBCT scan can cost at least $125 CAD as compared to just $20 CAD for a conventional periapical radiograph. Thus, any unjustified use of CBCT may cause a financial strain. In addition, according to the updated 2015 joint statement of the American Association of Endodontists (AAE) and the American Academy of Oral and Maxillofacial Radiology (AAOMR), CBCT should not be used routinely for endodontic diagnosis and screening purposes; it should only be used when the patient's history and clinical examination suggest that the benefits to the patient outweigh the potential risk, especially in inconclusive, difficult cases where a VRF cannot be confirmed. Special measures should be taken such as the use of a limited field of view and seeking the opinion of an oral and maxillofacial radiologist for image interpretation.[47]
Furthermore, it is very difficult to discern such microscopic fractures even with high-powered systems. The limitations of the current systems are compounded by the limitations of the humans using them and vary with issues that stem from training to perception. Talwar et al. discussed the challenges that face clinicians when diagnosing VRFs. They noted that CBCT has been used with a high accuracy rate and sensitivity level, yet as seen with other studies, they also reported that the superiority of CBCT over PRs is debated in the literature. Interestingly, their research showed that CBCT was more accurate than PRs in detecting VRFs in unfilled teeth, yet low sensitivity and specificity was found for CBCT when detecting VRFs in teeth that had been filled.[28] This research is interesting in that it reveals a potentially new issue in detecting VRFs. That is, the detection of the VRF may not necessarily be better for one type of imaging over another; rather, the detection may depend upon the specific characteristics of the tooth. The clinician may need to choose the type of imaging depending upon whether or not the tooth has been previously treated.
The advice to cautiously use CBCT because of its expense and risk of radiation may seem like a sensible counter to the notion that CBCT should be preferred in all instances. However, this does not address the central problem that 2D analysis has proven to be inadequate. The problem is that 2D radiographs have resulted in radical under-diagnosis, even when a fracture is present. This implicates the need to develop or advance our current methods to fulfill our needs in dentistry while balancing risk, benefit, and the reasonable costs of service.
CONCLUSIONS
While there is overwhelming evidence that suggests that the use of CBCT is a preferred method to detect VRFs, more research is needed before we accept it as the standard of care. We believe that the joint position statement of the AAE and AAOMR is logical and sufficient to guide dentists in general and endodontists specifically for how and when CBCT should be considered.
Therefore, we agree that CBCT can be useful in detecting VRFs; however, it should be used with caution and must be used after a combination of clinical tests and radiographic approaches have failed to finally reach a definitive diagnosis. In addition, if surgical exploration is the only option to confirm a diagnosis, then the use of CBCT is recommended as a diagnostic tool before surgical intervention to prevent performing an unnecessary surgical procedure in the case that a VRF were to be confirmed. More well controlled and high quality studies are needed to formulate the proper guidelines and parameters for how and when CBCT can be considered as a standard of care for the routine diagnosis of VRFs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.[48]
REFERENCES
- 1.Varshosaz M, Tavakoli MA, Mostafavi M, Baghban AA. Comparison of conventional radiography with cone beam computed tomography for detection of vertical root fractures: An in vitro study. J Oral Sci. 2010;52:593–7. doi: 10.2334/josnusd.52.593. [DOI] [PubMed] [Google Scholar]
- 2.Yoshino K, Ito K, Kuroda M, Sugihara N. Prevalence of vertical root fracture as the reason for tooth extraction in dental clinics. Clin Oral Investig. 2015;19:1405–9. doi: 10.1007/s00784-014-1357-4. [DOI] [PubMed] [Google Scholar]
- 3.Tsesis I, Kamburoglu K, Katz A, Tamse A, Kaffe I, Kfir A. Comparison of digital with conventional radiography in detection of vertical root fractures in endodontically treated maxillary premolars: An ex vivo study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:124–8. doi: 10.1016/j.tripleo.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 4.Khasnis SA, Kidiyoor KH, Patil AB, Kenganal SB. Vertical root fractures and their management. J Conserv Dent. 2014;17:103–10. doi: 10.4103/0972-0707.128034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen S, Berman LH, Blanco L, Bakland L, Kim JS. A demographic analysis of vertical root fractures. J Endod. 2006;32:1160–3. doi: 10.1016/j.joen.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Adorno CG, Yoshioka T, Suda H. Crack initiation on the apical root surface caused by three different nickel-titanium rotary files at different working lengths. J Endod. 2011;37:522–5. doi: 10.1016/j.joen.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Tang W, Wu Y, Smales RJ. Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod. 2010;36:609–17. doi: 10.1016/j.joen.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Mullally BH, Ahmed M. Periodontal signs and symptoms associated with vertical root fracture. Dent Update. 2000;27:356–60. doi: 10.12968/denu.2000.27.7.356. [DOI] [PubMed] [Google Scholar]
- 9.Llena-Puy MC, Forner-Navarro L, Barbero-Navarro I. Vertical root fracture in endodontically treated teeth: A review of 25 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:553–5. doi: 10.1067/moe.2001.117262. [DOI] [PubMed] [Google Scholar]
- 10.Hadrossek PH, Dammaschke T. New treatment option for an incomplete vertical root fracture – A preliminary case report. Head Face Med. 2014;10:9. doi: 10.1186/1746-160X-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nizam N, Kaval ME, Gurlek O, Atila A, Caliskan MK. Intentional replantation of adhesively reattached vertically fractured maxillary single-rooted teeth. Int Endod J. 2016;49:227–36. doi: 10.1111/iej.12444. [DOI] [PubMed] [Google Scholar]
- 12.Haueisen H, Gartner K, Kaiser L, Trohorsch D, Heidemann D. Vertical root fracture: Prevalence, etiology, and diagnosis. Quintessence Int. 2013;44:467–74. doi: 10.3290/j.qi.a29715. [DOI] [PubMed] [Google Scholar]
- 13.Davis DM, Fiske J, Scott B, Radford DR. The emotional effects of tooth loss: A preliminary quantitative study. Br Dent J. 2000;188:503–6. doi: 10.1038/sj.bdj.4800522. [DOI] [PubMed] [Google Scholar]
- 14.Roohafza H, Afghari P, Keshteli AH, Vali A, Shirani M, Adibi P, et al. The relationship between tooth loss and psychological factors. Community Dent Health. 2015;32:16–9. [PubMed] [Google Scholar]
- 15.Okoje VN, Dosumu OO, Alonge TO, Onyeaso C. Tooth loss: Are the patients prepared? Niger J Clin Pract. 2012;15:172–5. doi: 10.4103/1119-3077.97305. [DOI] [PubMed] [Google Scholar]
- 16.Takeshita WM, Iwaki LC, da Silva MC, Sabio S, Albino PR. Comparison of periapical radiography with cone beam computed tomography in the diagnosis of vertical root fractures in teeth with metallic post. J Conserv Dent. 2014;17:225–9. doi: 10.4103/0972-0707.131781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sungur DD, Altundasar E, Uzunoglu E, Yilmaz Z. Influence of different final irrigation regimens and various endodontic filling materials on vertical root fracture resistance. Niger J Clin Pract. 2016;19:267–71. doi: 10.4103/1119-3077.164334. [DOI] [PubMed] [Google Scholar]
- 18.Chai H, Tamse A. The Effect of Isthmus on Vertical Root Fracture in Endodontically Treated Teeth. J Endod. 2015;41:1515–9. doi: 10.1016/j.joen.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 19.Seo DG, Yi YA, Shin SJ, Park JW. Analysis of factors associated with cracked teeth. J Endod. 2012;38:288–92. doi: 10.1016/j.joen.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 20.Edlund M, Nair MK, Nair UP. Detection of vertical root fractures by using cone-beam computed tomography: A clinical study. J Endod. 2011;37:768–72. doi: 10.1016/j.joen.2011.02.034. [DOI] [PubMed] [Google Scholar]
- 21.Metska ME, Aartman IH, Wesselink PR, Ozok AR. Detection of vertical root fractures in vivo in endodontically treated teeth by cone-beam computed tomography scans. J Endod. 2012;38:1344–7. doi: 10.1016/j.joen.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 22.Valizadeh S, Vasegh Z, Rezapanah S, Safi Y, Khaeazifard MJ. Effect of Object Position in Cone Beam Computed Tomography Field of View for Detection of Root Fractures in Teeth with Intra-Canal Posts. Iran J Radiol. 2015;12:e25272. doi: 10.5812/iranjradiol.25272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khedmat S, Rouhi N, Drage N, Shokouhinejad N, Nekoofar MH. Evaluation of three imaging techniques for the detection of vertical root fractures in the absence and presence of gutta-percha root fillings. Int Endod J. 2012;45:1004–9. doi: 10.1111/j.1365-2591.2012.02062.x. [DOI] [PubMed] [Google Scholar]
- 24.Komatsu K, Abe Y, Yoshioka T, Ishimura H, Ebihara A, Suda H. Differential diagnosis of vertical root fractures using reconstructed three-dimensional models of bone defects. Dentomaxillofac Radiol. 2014;43:20140256. doi: 10.1259/dmfr.20140256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chang E, Lam E, Shah P, Azarpazhooh A. Cone-beam Computed Tomography for Detecting Vertical Root Fractures in Endodontically Treated Teeth: A Systematic Review. J Endod. 2016;42:177–85. doi: 10.1016/j.joen.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 26.Corbella S, Del Fabbro M, Tamse A, Rosen E, Tsesis I, Taschieri S. Cone beam computed tomography for the diagnosis of vertical root fractures: A systematic review of the literature and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:593–602. doi: 10.1016/j.oooo.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 27.Rosen E, Taschieri S, Del Fabbro M, Beitlitum I, Tsesis I. The Diagnostic Efficacy of Cone-beam Computed Tomography in Endodontics: A Systematic Review and Analysis by a Hierarchical Model of Efficacy. J Endod. 2015;41:1008–14. doi: 10.1016/j.joen.2015.02.021. [DOI] [PubMed] [Google Scholar]
- 28.Talwar S, Utneja S, Nawal RR, Kaushik A, Srivastava D, Oberoy SS. Role of Cone-beam Computed Tomography in Diagnosis of Vertical Root Fractures: A Systematic Review and Meta-analysis. J Endod. 2016;42:12–24. doi: 10.1016/j.joen.2015.09.012. [DOI] [PubMed] [Google Scholar]
- 29.Long H, Zhou Y, Ye N, Liao L, Jian F, Wang Y, et al. Diagnostic accuracy of CBCT for tooth fractures: A meta-analysis. J Dent. 2014;42:240–8. doi: 10.1016/j.jdent.2013.11.024. [DOI] [PubMed] [Google Scholar]
- 30.Zhang GC. Use of cone-beam computed tomography to detect atypical vertical root fracture occurring at first left mandibular incisor: Report of one case. Shanghai Kou Qiang Yi Xue. 2013;22:718–20. [PubMed] [Google Scholar]
- 31.Kajan ZD, Taromsari M. Value of cone beam CT in detection of dental root fractures. Dentomaxillofac Radiol. 2012;41:3–10. doi: 10.1259/dmfr/25194588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zou X, Liu D, Yue L, Wu M. The ability of cone-beam computerized tomography to detect vertical root fractures in endodontically treated and nonendodontically treated teeth: A report of 3 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:797–801. doi: 10.1016/j.tripleo.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 33.Wang P, Yan XB, Lui DG, Zhang WL, Zhang Y, Ma XC. Detection of dental root fractures by using cone-beam computed tomography. Dentomaxillofac Radiol. 2011;40:290–8. doi: 10.1259/dmfr/84907460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ozer SY. Detection of vertical root fractures of different thicknesses in endodontically enlarged teeth by cone beam computed tomography versus digital radiography. J Endod. 2010;36:1245–9. doi: 10.1016/j.joen.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 35.Kamburoglu K, Murat S, Yuksel SP, Cebeci AR, Horasan S. Detection of vertical root fracture using cone-beam computerized tomography: An in vitro assessment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e74–81. doi: 10.1016/j.tripleo.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 36.Hassan B, Metska ME, Ozok AR, van der Stelt P, Wesselink PR. Detection of vertical root fractures in endodontically treated teeth by a cone beam computed tomography scan. J Endod. 2009;35:719–22. doi: 10.1016/j.joen.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 37.Ezzodini Ardakani F, Razavi SH, Tabrizizadeh M. Diagnostic value of cone-beam computed tomography and periapical radiography in detection of vertical root fracture. Iranian Endod J. 2015;10:122–6. [PMC free article] [PubMed] [Google Scholar]
- 38.Junqueira RB, Verner FS, Campos CN, Devito KL, do Carmo AM. Detection of vertical root fractures in the presence of intracanal metallic post: A comparison between periapical radiography and cone-beam computed tomography. J Endod. 2013;39:1620–4. doi: 10.1016/j.joen.2013.08.031. [DOI] [PubMed] [Google Scholar]
- 39.Kambungton J, Janhom A, Prapayasatok S, Pongsiriwet S. Assessment of vertical root fractures using three imaging modalities: Cone beam CT, intraoral digital radiography and film. Dentomaxillofac Radiol. 2012;41:91–5. doi: 10.1259/dmfr/49798768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chavda R, Mannocci F, Andiappan M, Patel S. Comparing the in vivo diagnostic accuracy of digital periapical radiography with cone-beam computed tomography for the detection of vertical root fracture. J Endod. 2014;40:1524–9. doi: 10.1016/j.joen.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 41.Jakobson SJ, Westphalen VP, Silva Neto UX, Fariniuk LF, Schroeder AG, Carneiro E. The influence of metallic posts in the detection of vertical root fractures using different imaging examinations. Dentomaxillofac Radiol. 2014;43:20130287. doi: 10.1259/dmfr.20130287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.da Silveira PF, Vizzotto MB, Liedke GS, da Silveira HL, Montagner F, da Silveira HE. Detection of vertical root fractures by conventional radiographic examination and cone beam computed tomography – An in vitro analysis. Dent Traumatol. 2013;29:41–6. doi: 10.1111/j.1600-9657.2012.01126.x. [DOI] [PubMed] [Google Scholar]
- 43.Bechara B, McMahan CA, Nasseh I, Geha H, Hayek E, Khawam G, et al. Number of basis images effect on detection of root fractures in endodontically treated teeth using a cone beam computed tomography machine: An in vitro study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:676–81. doi: 10.1016/j.oooo.2013.01.026. [DOI] [PubMed] [Google Scholar]
- 44.Fayad MI, Ashkenaz PJ, Johnson BR. Different representations of vertical root fractures detected by cone-beam volumetric tomography: A case series report. J Endod. 2012;38:1435–42. doi: 10.1016/j.joen.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 45.Ozer SY, Unlu G, Deger Y. Diagnosis and treatment of endodontically treated teeth with vertical root fracture: Three case reports with two-year follow-up. J Endod. 2011;37:97–102. doi: 10.1016/j.joen.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 46.Horner K, O’Malley L, Taylor K, Glenny AM. Guidelines for clinical use of CBCT: A review. Dentomaxillofac Radiol. 2015;44:20140225. doi: 10.1259/dmfr.20140225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. [Last accessed on 2016 May 28]. Available from: http://www.aae.org/publications-and-research/endodontics-colleagues-for-excellence-newsletter/cone-beamcomputed-tomography-in-endodontics.aspx .
- 48.Tang L, Zhou XD, Wang Y, Zhang L, Zheng QH, Huang DM. Detection of vertical root fracture using cone beam computed tomography: Report of two cases. Dent Traumatol. 2011;27:484–8. doi: 10.1111/j.1600-9657.2011.01030.x. [DOI] [PubMed] [Google Scholar]


