Abstract
Marburg virus (Marburg marburgvirus; MARV) causes sporadic outbreaks of Marburg hemorrhagic fever (MHF) in Africa. The Egyptian fruit bat (Rousettus aegyptiacus) has been identified as a natural reservoir based most-recently on the repeated isolation of MARV directly from bats caught at two locations in southwestern Uganda where miners and tourists separately contracted MHF from 2007–08. Despite learning much about the ecology of MARV through extensive field investigations, there remained unanswered questions such as determining the primary routes of virus shedding and the severity of disease, if any, caused by MARV in infected bats. To answer these questions and others, we experimentally infected captive-bred R. aegyptiacus with MARV under high (biosafety level 4) containment. These experiments have shown infection profiles consistent with R. aegyptiacus being a bona fide natural reservoir host for MARV and demonstrated routes of viral shedding capable of infecting humans and other animals.
Keywords: Experimental infection, Marburg virus, Rousettus aegyptiacus, shedding, transmission
INTRODUCTION
Marburg hemorrhagic fever is a severe and often fatal disease in humans caused by infection with Marburg virus (family Filoviridae, Marburg marburgvirus; MARV). Human-to-human transmission of MARV occurs primarily through contact with infected body fluids, similar to that for several members of the genus Ebolavirus (family Filoviridae): Zaire ebolavirus (Ebola virus), Sudan ebolavirus (Sudan virus), and Bundibugyo ebolavirus (Bundibugyo virus). The first documented MARV infection in humans occurred in laboratory workers in Germany and Yugoslavia in 1967, when MARV-infected green monkeys (Cercopithecidae: formerly Cercopithecus aethiops; currently Chlorocebus tantalus; Wilson and Reeder 2005) were imported from Uganda (Siegert et al. 1968) and used for vaccine development. Since that time, 10 additional outbreaks have occurred, most in eastern sub-Saharan Africa. Two of these outbreaks, one in Durba, Democratic Republic of the Congo and another in Uige, Angola, had over 150 cases with >80% case fatality (Bausch et al. 2006; Towner et al. 2006). The Durba outbreak lasted for 2 yr, (1998–2000) and was epidemiologically linked to subterranean gold mining (Bausch et al. 2006). The mine contained large numbers of a common cave-dwelling fruit bat, Rousettus aegyptiacus (Egyptian fruit bat; EFB), that has been subsequently identified as a natural reservoir for MARV. This discovery was based on finding MARV-specific RNA and IgG antibodies (Swanepoel et al. 2007; Towner et al. 2007) and the presence of infectious virus (Towner et al. 2009; Amman et al. 2012) in wild EFB, including those inhabiting gold mines and tourist attractions in Uganda where more-recent MARV outbreaks have occurred. Moreover, longitudinal studies have shown that periods of spillover to humans may be associated with seasonal pulses of active MARV infections in juvenile EFB during annual reproductive cycles (Amman et al. 2012).
Many basic aspects of MARV ecology are not well known, including MARV replication kinetics and dissemination in bat tissues and the mechanism(s) by which the virus is transmitted from bats to other bats or to humans. Two experimental infection studies involving filoviruses in captive bats have been informative. The first study utilized a variety of plants and animals, including three species of bats (Mops condylurus [Angolan free-tailed bat], Chaerephon pumila [little free-tailed bat], and Epomophorus wahlbergi [Wahlberg’s epauletted fruit bat]) that were either exposed to or injected with Ebola virus (Swanepoel et al. 1996). Ebola virus replicated only in bats and could be detected for up to 3 wk in feces. In a second study, a high-passage (P38) Vero cell-adapted MARV strain (Hogan) was used to infect EFB (Paweska et al. 2012). Virus was injected subcutaneously and intraperitoneally into adult and newborn bats from mixed gender groups. Marburg virus replicated in EFB without obvious disease, consistent with expectations for MARV replication in its reservoir host. However, virus shedding could not be detected in oral secretions, feces, or urine.
Here, we report a serial euthanasia study in which low-passage (P2) MARV, isolated from a naturally infected EFB, was used to infect first generation, age-and gender-matched, captive-bred EFB. We determined the infection kinetics in 15 major tissues including blood from days 3–28 postinfection (PI), and we isolated virus multiple times from oral secretions of infected bats. Further, we show that MARV can be detected for up to 6 consecutive days in oral secretions between days 3–14 PI and up to 4 days after virus has been cleared from the blood.
MATERIALS AND METHODS
Animals and biosafety
All experimental procedures were conducted with approval from the Centers for Disease Control and Prevention (CDC, Atlanta, Georgia, USA) Institutional Animal Care and Use Committee, and in strict accordance with the Guide for the Care and Use of Laboratory Animals (Committee for the Update of the Guide for the Care and Use of Laboratory Animals 2011). The CDC is an Association for Assessment and Accreditation of Laboratory Animal Care International fully accredited research facility. No human patient-derived clinical materials were used in these studies.
Procedures conducted with infectious MARV or with infected bats were performed at the CDC under biosafety level 4 (BSL-4) laboratory conditions in accordance with Select Agent regulations (Animal and Plant Health Inspection Service and Centers for Disease Control and Prevention 2014). All investigators and animal handlers followed strict BSL-4 biosafety and infection control practices (CDC 2009b) to prevent cross-contamination between experimentally infected and control bats.
All bats used in this study were first-generation, captive-born bats from an MARV-free breeding colony founded from wild-caught EFB imported from Uganda. The experimental group consisted of 30 juvenile males, 4–5 mo old, with an average weight of 107 g. The bats were housed in groups of ≤9 in designated experimental and control caging (interior dimensions 61×71×76 cm long, wide, and high, respectively) in a climate-controlled BSL-4 laboratory animal room with a 12 h day:night cycle. Cross-contamination between experimental and control bats was prevented by housing within separate isolation units (Duo-Flow Mobile Units, Lab Products Inc., Seaford, Delaware, USA) with high efficiency particulate air-filtered inlet and exhaust air supply. Daily food consisted of chopped bananas, watermelon, cantaloupe, seedless grapes, apples, and pears dusted with a protein vitamin supplement (Lubee Bat Conservancy, Gainesville, Florida, USA).
Virus stock
An MARV isolate (371bat virus; second passage on Vero-E6 cells), obtained from a naturally infected EFB (371bat) collected during an MARV outbreak ecologic investigation in southwestern Uganda (Towner et al. 2009), was diluted in a solution of Dulbecco’s modified Eagle’s medium (DMEM) to a concentration of 1×104 tissue culture infective dose 50 (TCID50)/mL.
Experimental design
The bats were randomly divided into three groups (A–C), each consisting of nine virus-inoculated bats and one control bat. Baseline blood samples, body weights, and temperatures were taken prior to inoculation. For inoculations, all bats were anesthetized with isoflurane and subcutaneously injected in the mid-ventral abdomen with either 250 μL of MARV prepared in DMEM for a total dose of 104 TCID50 per bat (n=27), or 250 μL of sterile DMEM for control bats (n=3). Rectal temperatures and body weights were recorded daily. Oral and rectal samples were collected daily for subsequent virus titration. Blood samples were taken from each bat on alternate days. On days 3, 5, 6, 7, 8, 9, 10, 12, and 28 PI, one bat from each group (A–C, n=3 per time point) was euthanized under anesthesia via cardiac exsanguination and full postmortem necropsies were performed. The three negative control bats were euthanized and similarly processed on day 28 PI. Cardiac blood was taken upon euthanasia for later analysis. Complete tissue sets (see below) were taken and either stored in RNA extraction buffer for PCR analysis or frozen and stored under liquid nitrogen vapor.
Postinfection procedures
Beginning on day 1 PI, body weights and temperatures of all animals were recorded. A temperature probe covered with a plastic sheath (MABIS Healthcare, Waukegan, Illinois, USA) was used to measure the rectal temperature of each bat. The plastic sheath was then cut and placed into a deep-well plate with 500 μL of MagMax lysis buffer solution (Life Technologies, Grand Island, New York, USA) for PCR analysis. Two polyester-tipped applicators (Fisher Scientific, Grand Island, New York, USA) were used to swab the inside of each bat’s mouth. The swabs were immediately placed in either a deep-well plate with 500 μL of lysis binding solution for PCR analysis or in viral transport medium for isolation. Blood samples (≤60 μL) were taken via venipuncture from the cephalic vein on the propatagium every-other day on days 1–14 and then on days 21 and 28. Necropsies were performed on the aforementioned euthanasia days to collect skin, liver, spleen, large intestine (colon-rectum), small intestine, mesenteric lymph node, kidney, adrenal gland, heart, lung, salivary gland, testis, urinary bladder, and brain.
Sample testing and RNA extraction
All tissue, blood, and swab samples were analyzed with quantitative reverse transcriptase PCR (qRT-PCR) targeting VP40 and using reagents and procedures described by Amman et al. (2012). For tissue specimens, approximately 100 mg were placed in 2-mL grinding vials (OPS Diagnostics, Lebanon, New Jersey, USA) with 1 mL of MagMax lysis buffer concentrate and homogenized as described by Amman et al. (2012). Specimen sizes of some tissues (urinary bladder, adrenal gland, and testis) were under 100 mg due to availability but remained consistent within a tissue type. Total RNA extraction was achieved using the MagMax-96 Total RNA Isolation kit (Life Technologies) per manufacturer’s recommendations and the AM1830_DW protocol preloaded on the MagMax Express-96 Deep Well Magnetic Particle Processor. Each reaction used 125 μL of the tissue lysate with 75 μL of 100% isopropanol. To account for sample-to-sample variation, qRT-PCR results for tissues were normalized to results for 18s rRNA using a commercially available eukaryotic 18S rRNA primer-probe assay (Applied Biosystems, Grand Island, New York, USA) according to manufacturer’s instructions. Gamma-irradiated Rift Valley fever virus (RVFV; 0.25 μL per sample) was added to the lysis buffer solutions as an extraction control for blood and swab samples. The RVFV qRT-PCR was performed as described by Bird et al. (2007) but using 58 C for the annealing temperature, as for MARV.
Blood samples (20 μL; whole, nonheparinized) were added to 130 μL of lysis binding solution (1:1 ratio of lysis buffer concentrate and 100% isopropanol) and extracted using the MagMax-96 Viral RNA Isolation kit and the AM1836_DW_50v2 protocol preloaded on the MagMax Express-96 Deep Well Magnetic Particle Processor.
Polyester-tipped applicators used as oral swabs and the plastic probe cover sheaths used for rectal swabs were placed into wells of a deep-well plate containing 500 μL of lysis binding solution. Viral RNA was extracted using the 5× MagMax Pathogen RNA/DNA kit per manufacturer’s instructions, using 200 μL of sample and 500 μL of lysis binding solution, and the 4462359_DW_HV protocol preloaded on the MagMax Express-96 Deep Well Magnetic Particle Processor.
Standard curves for qRT-PCR results were generated by serial, 10-fold dilutions of 371bat MARV stock virus of known titer (TCID50/mL) in DMEM and added to blood, tissue (calf liver) homogenate, or DMEM in the same proportions and methods as that used for collecting blood, tissues, or swab samples from bats. The relative TCID50/mL (fluid samples) or TCID50/g (tissue samples) equivalents were interpolated from the relevant standard curve. The standard curve for swab samples was based on a calculation in which 20 μL of virus solution was absorbed by the swab applicator.
Virus isolation
Polyester-tipped applicators used for oral swabs were placed into 500 μL DMEM-fungizone-penstrep (100 units/mL penicillin; 100 μg/mL streptomycin; 2.50 μg/mL amphotericin B; Life Technologies) with 2% fetal calf serum and then flash frozen in liquid nitrogen until virus isolations were attempted. The entire eluate was used to inoculate Vero-E6 cells in 25-cm2 flasks for 1 h at 37 C and 5% CO2. DMEM-fungizone-penstrep containing 2% fetal calf serum was then added and cultures were monitored for 14 days with a media change on day 7. All cultures were tested by immunofluorescent assays for MARV.
Serology
Blood samples taken for serologic analysis were tested by enzyme-linked immunosorbent assay (ELISA) for IgG antibodies reactive to MARV, exactly as described in Ksiazek et al. (1999a, b) with the modification that 96-well plates were coated with 50 ng/well of recombinant MARV nucleocapsid protein (NP; Angola strain) expressed in Escherichia coli and the sum optical density (OD) values adjusted by subtracting reactivity at each 4-fold dilution (1:100 to 1:6,400) to Reston ebolavirus NP protein similarly expressed and purified from E. coli.
RESULTS
Evidence of infection was found in all 27 bats inoculated subcutaneously with MARV. No disease-related mortality or overt signs of morbidity were observed in any of the animals. The bats were monitored daily and maintained normal feeding routines. No significant differences in percentage weight change were found throughout the course of the infections between the experimentally infected bats and the control bats or among experimental groups (F3,26=0.58; P>0.10; data not shown). Average body temperatures for experimental groups were within normal ranges and were consistent with those observed in the control groups (data not shown).
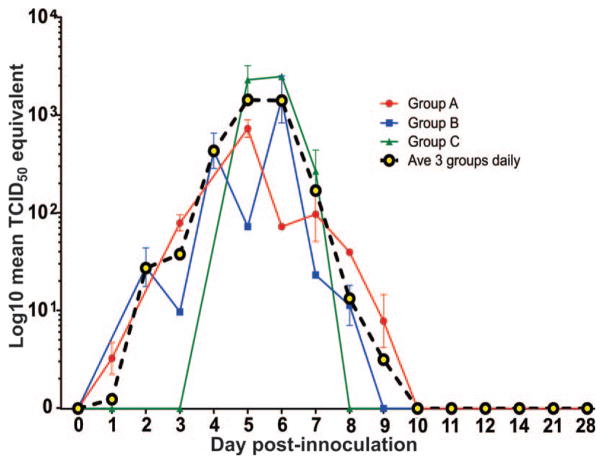
Viral loads (Table 1), measured by qRT-PCR analysis of viral RNA, are hereafter reported as mean TCID50 equivalents per gram of tissue or milliliter of fluid. Viremia (Fig. 1) was detected in all but three (bats 40002, 42509, and 42336) of the 27 bats infected with MARV as early as day 1 PI. Mean viral load values peaked on day 5 PI (mean value: 2.23×103 TCID50/mL; single bat: 7.79×103 TCID50/mL) and were cleared from the blood by day 10 PI. The largest number of bats viremic at one time was 20 on day 4 PI. The average time span of detectable viremia for all bats was short, 3 days, and ranged from 1–9 days.
Table 1.
Quantitative reverse-transcriptase–PCR-positivea tissues from Egyptian fruit bats (Rousettus aegyptiacus) inoculated in the laboratory with Marburg virus.
| Day | Bat | Tissuesb
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Li | Sp | Bld | Ht | Ki | AG | LD | LC | LIn | SIn | ML | Ts | Br | SI | Bla | SG | ||
| 3 | 40088 | ++ | +++ | ++ | + | + | − | + | − | + | − | + | + | + | +++++ | + | − |
| 42250 | ++ | ++ | + | − | − | − | − | − | − | − | + | − | − | +++++ | − | − | |
| 42336 | ++++ | +++ | − | − | − | − | − | − | − | − | − | − | − | +++++ | − | + | |
| 5 | 19854 | +++ | +++++ | +++ | + | + | − | + | + | + | − | + | − | − | ++++++ | + | + |
| 42919 | ++++ | ++++ | ++ | + | − | − | − | − | + | − | + | − | − | +++++ | + | − | |
| 56159 | +++++ | +++++ | +++ | − | − | − | − | − | − | − | ++ | − | − | +++++ | ++ | − | |
| 6 | 42672 | ++ | ++++ | ++ | − | + | − | − | + | + | − | − | − | − | +++++ | − | − |
| 38666 | ++++ | +++ | ++ | − | − | − | − | − | − | − | + | − | − | +++++ | + | − | |
| 36412 | +++++ | ++++ | +++ | − | − | − | − | − | ++ | − | − | − | − | +++++ | + | + | |
| 7 | 40896 | +++ | +++ | − | − | +++ | − | − | − | − | − | − | + | − | ++++ | − | ++ |
| 43165 | ++++ | +++ | + | ++ | + | − | − | − | + | +++ | − | − | − | ++++++ | + | − | |
| 38702 | ++++ | +++ | − | − | − | − | − | − | + | − | − | − | − | ++++ | − | − | |
| 8 | 42853 | +++++ | +++ | + | + | ++ | ++ | − | ++ | +++ | ++ | ++++ | ++++ | + | +++++ | + | +++ |
| 41032 | ++ | +++ | − | − | − | − | ++ | − | − | − | + | − | − | ++++ | − | + | |
| 90906 | ++++ | ++ | − | − | − | − | − | − | − | − | − | − | − | ++ | − | − | |
| 9 | 36089 | +++ | +++ | + | − | ++ | + | − | − | ++ | + | +++ | − | − | ++++ | − | − |
| 43133 | + | + | − | − | − | − | − | − | − | − | − | − | − | +++ | − | − | |
| 20712 | ++ | − | − | − | − | − | − | − | − | − | − | − | − | +++ | − | − | |
| 10 | 41880 | + | ++ | − | − | − | − | − | − | + | − | − | − | − | +++ | − | + |
| 42030 | ++ | ++ | − | − | ++ | − | − | − | + | + | − | ++ | + | ++ | − | ++ | |
| 40002 | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | |
| 12 | 43662 | + | ++ | − | + | − | − | − | − | − | − | − | − | − | − | − | − |
| 41671 | ++ | ++ | − | + | ++ | − | − | + | − | − | − | − | − | − | − | − | |
| 42509 | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | |
| 28 | 41468 | − | + | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| 41412 | − | + | − | − | − | − | − | − | − | − | − | − | − | − | − | − | |
| 85963 | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | |
The number of + symbols represents the viral load in tissue culture infective dose 50 (TCID50)/g equivalents derived from cycle threshold values generated by RT-PCR: + <102 TCID50/g eq; ++ <103 TCID50/g eq; +++ <104 TCID50/g eq; ++++ <105 TCID50/g eq; +++++ <106 TCID50/g eq; ++++++ ≥106 TCID50/g eq.
Li = liver; Sp = spleen; Bld = blood; Ht = heart; Ki = kidney; AG = adrenal gland; LD = distal lung; LC = cranial lung; LIn = large intestine; SIn = small intestine; ML = mesenteric lymph node; Ts = testes; Br = brain; SI = skin at inoculation site; Bla = bladder; SG = salivary gland; (−) = negative.
Figure 1.
Viral RNA in blood of Egyptian fruit bats (Rousettus aegyptiacus) inoculated in the laboratory with Marburg virus. Viral RNA levels in blood (log10 tissue culture infective dose 50 [TCID50]/mL equivalent) days postinfection for each bat (n=27) are shown for three groups of bats.
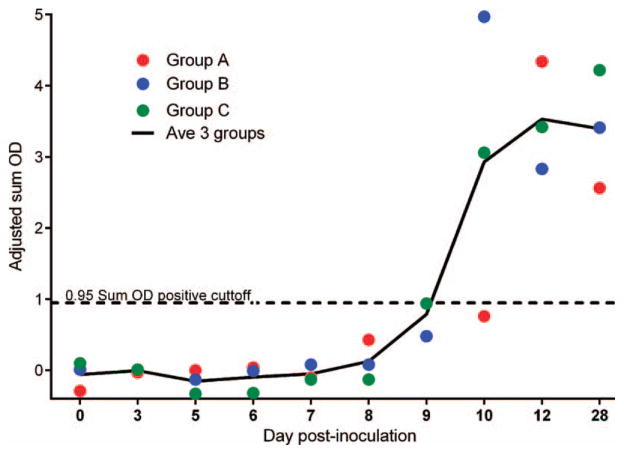
The ELISA results show anti-MARV IgG levels, represented by adjusted sum OD values (Fig. 2) approaching a sum OD positive cut-off value of 0.95 by day 9 PI. All bats euthanized after day 10 PI seroconverted with sum ODs ranging from 2.56–4.97 with titers ≥400.
Figure 2.
Serology results for Egyptian fruit bats (Rousettus aegyptiacus) inoculated with Marburg virus. Results for anti-Marburg virus IgG measured by enzyme-linked immunosorbent assay are shown as adjusted sum optical densities (OD) by day postinoculation for all infected bats (n=27) at the time of euthanasia for each group.
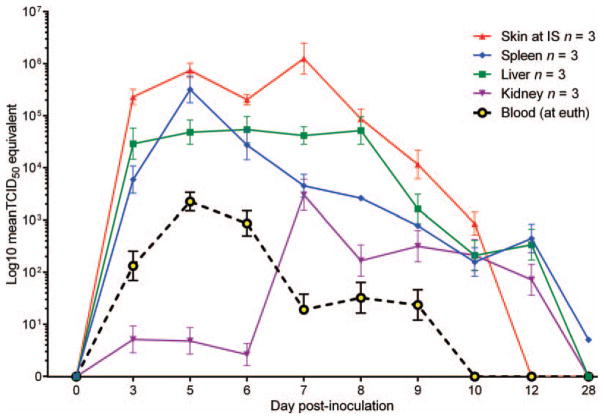
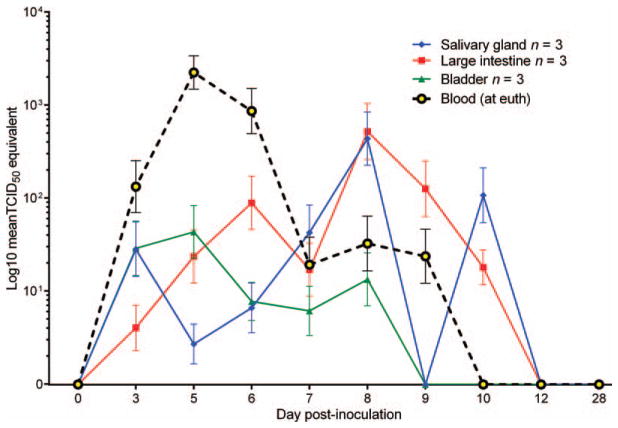
Signs of disseminated infection in tissues, detectable by increases in mean viral loads relative to blood, occurred in the spleen and liver (Fig. 3). Infection was first detected in liver on day 3 PI, the first scheduled day of euthanasia, and mean viral loads peaked on day 6 (5.41×104 TCID50/g). Infection in the spleen was also detected on day 3 and peaked on day 5 (3.18×105 TCID50/g). Mean viral loads decreased dramatically in both of these tissues by 10–12 days PI and were cleared (liver) or only weakly positive (spleen; 5.04×101 TCID50/g) by day 28. Mean viral loads in skin samples taken from the inoculation site showed the highest viral loads of all tissues (Fig. 3). Infection in the skin was detected on day 3, peaked on day 7 (1.26×106 TCID50/g), and was cleared by day 12. Spleen, liver, blood, and skin at the inoculation site were the most-frequently qRT-PCR–positive samples from infected bats, although virus was detected in 14 additional tissue types (Table 1). Of note, infection in bat 42853 was widespread on day 8 PI with detectable virus present in all but one tissue type. Most organs compatible with virus shedding, e.g., kidney, salivary gland, bladder, and large intestine (Figs. 3, 4), also showed signs of infection as early as day 3, but with lower viral loads, and peaked at later times than did liver, spleen, or skin. The quantity of MARV in the kidney did not peak until day 7 (3.02×103 TCID50/mg), but persisted through day 12 and was cleared by day 28, while those for salivary gland and large intestine peaked on day 8 (4.34×102 TCID50/g and 5.17×102 TCID50/g, respectively) and were cleared by day 12. In the bladder, mean viral loads peaked on day 5 (4.31×101 TCID50/g) and were cleared by day 9. Viral loads detected in the inoculation-site skin, liver, and spleen samples were all much higher than those detected in corresponding blood samples taken at the same time, as well as the 104 TCID50 inoculum dose, indicating true viral replication in these tissues.
Figure 3.
Marburg virus RNA in skin, liver, spleen, and kidneys of Marburg virus-infected Egyptian fruit bats (Rousettus aegyptiacus). Mean viral RNA levels measured by quantitative reverse-transcriptase–PCR in skin at inoculation site (IS), liver, spleen, and kidneys (n=3; log10 TCID50/g equivalent) at the time of euthanasia (days). Each symbol (point) represents the mean viral load detected in that tissue in the three bats euthanized on that day. For reference, the mean viral loads detected in blood from those same bats on that day are shown (dashed black-yellow line). TCID=tissue culture infective dose.
Figure 4.
Marburg virus RNA in salivary gland, bladder, and large intestine of Egyptian fruit bats (Rousettus aegyptiacus) inoculated with Marburg virus. Mean viral RNA levels were measured by quantitative reverse transcriptase PCR (log10 TCID50/g equivalent) at the time of euthanasia (days). Each symbol (point) represents the mean viral load detected in that tissue in the three bats euthanized on that day. For reference, the mean viral loads detected in blood from those same bats on that day are shown (dashed black-yellow line). TCID=tissue culture infective dose.
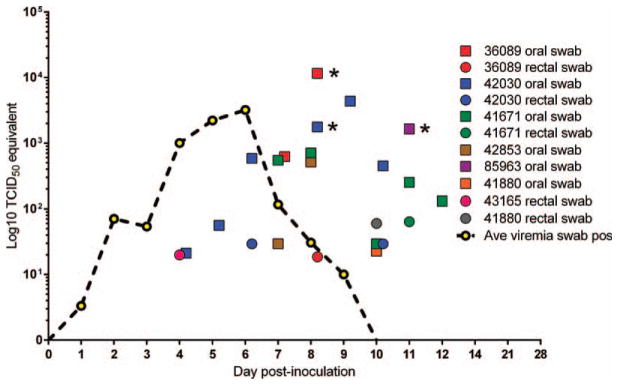
Marburg virus-positive oral swabs were obtained on day 4–14 PI (n=17). The highest viral loads were detected on day 8 (1.16×104 TCID50/mL) and cleared from oral secretions by day 14 (Fig. 5). Three virus isolates were obtained from oral swabs from three infected bats, two bats (36089, 42030) on day 8, and one bat (85963) on day 11. Marburg virus RNA was also detected in rectal swabs (n=6, Fig. 5) from days 4–11 PI, albeit with much less frequency than in oral swabs and at much lower levels than that found in blood taken from the same animals on the same day, indicating that blood contamination of the rectal swabs cannot be ruled out.
Figure 5.
Marburg virus RNA in oral and rectal swabs from Egyptian fruit bats (Rousettus aegyptiacus) inoculated with Marburg virus. Viral levels from oral (square) and rectal (circle) swabs by day postinfection. Swab viral level values (log10 TCID50/mL equivalent) are equivalents of a stock tested (see Materials and Methods), not the actual amount of virus in saliva or feces, because the volume of absorbed oral secretion could not be calculated. Oral swabs from which Marburg virus could be isolated are depicted by an asterisks on days 8 (n=2) and 11 (n=1). The average viremia (Ave viremia swab pos) over time for bats with positive swabs (oral or rectal) is shown. TCID=tissue culture infective dose.
DISCUSSION
Our results show that R. aegyptiacus can become infected with MARV through experimental subcutaneous inoculation and without mortality or any indication of explicit morbidity. Our experimental approach differs significantly from an MARV study described by Paweska et al. (2012). The bats we used were one generation removed from the wild-caught colony founder bats and had not experienced multiple generations of colony inbreeding. Additionally, our bats were 5-mo-old juveniles which are the approximate age-cohort most frequently infected by MARV in the wild (Amman et al. 2012). Further, we used a low-passage, bat-borne virus (371bat MARV; Towner et al. 2009), thus minimizing the potential for confounding effects of adaptive mutations accumulated through passage in cell culture or humans. Finally, all bats in this study were uniformly inoculated by a single subcutaneous injection route, with representative daily tissue samples taken through the acute phase of the infection, days 5–10 PI, and additionally sampled on days 3, 12, and 28. Oral and rectal swabbing was performed on a rigorous schedule, daily from days 1–12 PI and on days 14, 21, and 28.
All 27 bats inoculated with MARV became infected, and all but three underwent a viremic stage. Many bats were viremic for 1 day only (n=6), and it is likely that the days on which some bats (40002 and 42509) were viremic were missed due to the alternate-day bleeding schedule. These two bats seroconverted on days 10 and 12, respectively, while the third nonviremic bat (42336) was euthanized on day 3 and had MARV-positive (by qRT-PCR) liver, spleen, salivary gland, and skin at the inoculation site (Table 1). Detectable viremia in naturally infected bats was found in only four of 71 (6%) that were positive for virus RNA in pooled liver-spleen samples (Towner et al. 2009; Amman et al. 2012).
Viral RNA levels (by qRT-PCR) in visceral tissues indicate that liver and spleen have the highest viral loads and are the first and most-frequent sites of disseminated viral replication. These data are consistent with those from naturally infected bats caught at MARV outbreak locations in Uganda (Towner et al. 2009; Amman et al. 2012). Mean viral loads in tissues from experimentally infected bats were considerably higher (liver, day 5: 5.41×104 TCID50/mg; spleen, day 5: 3.18×105 TCID50/mg) than those found in the blood (day 5: 2.23×103 TCID50/mL), ruling out residual virus in blood as a major contributor to the qRT-PCR signal. Peak viral loads in kidneys were also higher than that in blood (day 7: 3.02×103 TCID50/mg) and also peaked later than in liver and spleen. Finding MARV in salivary gland, kidney, bladder, and large intestine are significant because these organs represent potential avenues of virus shedding. Also, viral loads in these four tissues peaked as the loads in blood were declining. Visceral tissues positive for MARV by qRT-PCR were not found in bats 40002, 42509, and 85963 but, as mentioned previously, bats 40002 and 42509 seroconverted on days 10 and 12, respectively, and bat 85963 was viremic on day 5 and seroconverted by day 28. These three bats (40002, 42509, 85963) were euthanized in the later days of the experiment (day 10, 12, and 28, respectively) when viral loads were waning or were completely cleared from visceral tissues of other bats. The number of qRT-PCR–positive tissues found in one bat (428530) indicates the potential for widespread infection during the acute phase of virus replication, a finding also observed in wild-caught MARV-infected bats (Amman et al. 2012). Despite widespread virus dissemination, we observed no significant changes in daily food consumption, body weight, or daily body temperature, and no signs of overt morbidity or behavioral changes such as waning appetite, overly aggressive behavior, separation from cage mates, lethargy, or reduced or abandoned grooming.
A key outcome in this study was the detection of MARV-positive oral and rectal swabs. Importantly, infectious MARV was isolated from the oral cavities (oral swabs) of bats with 103 TCID50/mL equivalent or greater viral loads (Fig. 5). Unfortunately, urine samples were difficult to collect because bats tended to urinate during the capture process. These findings demonstrate MARV shedding in a filovirus natural reservoir species and have implications for virus transmission to human and nonhuman primates and perhaps other bats. Fruit bats are known for test-biting fruit and generating large amounts of masticated fruit spats under the trees in which they feed (Jacobsen and Du Plessis 1976). Spats and half-eaten fruit with residual MARV could be readily consumed by susceptible animals. We speculate that a major route of horizontal bat-to-bat MARV transmission is through biting, based on the success of the subcutaneous inoculation route and the reported inability of EFB to be infected by an oronasal route (Paweska et al. 2012). However, a mucosal route of infection in bats cannot be completely discounted because the bats receiving oronasal inoculation in that study were only monitored for 21 days, and oronasal inoculation with a nonculture-adapted, bat-borne MARV has not been attempted. Egyptian fruit bats occupy extremely close quarters with their roost mates (Fig. 6) and altercations are common (Kingdon 1974; Jacobsen and Du Plessis 1976; Kwiecinski and Griffiths 1999; Amman et al. 2012). Moreover, sexual interactions are typically preceded by males biting unwilling females, followed by continual muzzle licking during copulation (Kingdon 1974). Transmission of other zoonotic viruses through biting has been reported (Rupprecht et al. 2002; Calisher et al. 2007).
Figure 6.
A large, densely populated colony of Egyptian fruit bats (Rousettus aegyptiacus) at Python Cave in Queen Elizabeth National Park, Uganda is shown. The large number of bats and their affinity for close contact is thought to perpetuate the circulation of Marburg virus infection within the colony. Marburg virus has been found in this population during every sampling effort (Amman et al. 2012).
The viral loads found in rectal swabs were low but may still represent a potential avenue for viral shedding and bat-to-human (or nonhuman primate) or bat-to-bat transmission. In Python Cave, Uganda, the most actively infected group of bats (older juveniles; Amman et al. 2012) tend to occupy a variety of spaces at lower levels along the cave walls and floor, where deposits of fresh guano and urine are distributed continually. The excretory route may be a mechanism of MARV transmission between bats and primates and would not require any physical contact (bites, butchering for consumption, etc.). When the bats are disturbed by human entry into their roost, they typically excrete bodily wastes on takeoff or soon after taking flight (B.R.A., J.S.T., pers. obs.), dropping potentially infectious bodily waste that, without appropriate personal protective equipment, could come into contact with exposed skin and mucous membranes. Tourists infected with MARV at Python Cave reported not having any direct contact with the bats (CDC 2009a; Timen et al. 2009).
Our experimental infections shed new light on the virus-host interactions between EFB and MARV. First and foremost, these experimental infections provide strong evidence of viral shedding through oral secretions, indicating a viable route for horizontal transmission. Our data also point to a potential secondary route of infection among bats through a rectal excretory route, which may also be a route of infection from bats to humans. Regardless of the exact mechanisms, this study confirms that exposure to MARV-contaminated bat fluids (saliva and feces) should be avoided. Public health authorities should continue to discourage people from entering EFB roosting sites (caves and mines) for any reason or from harvesting these bats for food.
Acknowledgments
We thank the Centers for Disease Control and Prevention’s Animal Resource Branch for care and support of the bats during this study. We also thank B. R. Erickson for the photograph used in this publication and T. Klimova for editorial assistance. Funding for this study was provided by the US Department of Health and Human Services. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention or Health and Human Services.
LITERATURE CITED
- Amman BR, Carroll SA, Reed ZD, Sealy TK, Balinandi S, Swanepoel R, Kemp A, Erickson BR, Comer JA, Campbell S, et al. Seasonal pulses of Marburg virus circulation in juvenile Rousettus aegyptiacus bats coincide with periods of increased risk of human infection. PLoS Pathog. 2012;8:e1002877. doi: 10.1371/journal.ppat.1002877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Animal and Plant Health Inspection Service and Centers for Disease Control and Prevention. [Accessed September 2014];National select agent registry. 2014 www.selectagents.gov/Regulations.html.
- Bausch DG, Nichol ST, Muyembe-Tamfum JJ, Borchert M, Rollin PE, Sleurs H, Campbell P, Tshioko FK, Roth C, Colebunders R, et al. Marburg hemorrhagic fever associated with multiple genetic lineages of virus. N Engl J Med. 2006;355:909–919. doi: 10.1056/NEJMoa051465. [DOI] [PubMed] [Google Scholar]
- Bird BH, Bawiec DA, Ksiazek TG, Shoemaker TR, Nichol ST. Highly sensitive and broadly reactive quantitative reverse transcription-PCR assay for high-throughput detection of Rift Valley fever virus. J Clin Microbiol. 2007;45:3506–3513. doi: 10.1128/JCM.00936-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calisher CH, Wagoner KD, Amman BR, Root JJ, Douglass RJ, Kuenzi AJ, Abbott KD, Parmenter C, Yates TL, Ksiazek TG, et al. Demographic factors associated with prevalence of antibody to Sin Nombre virus in deer mice in the western United States. J Wildl Dis. 2007;43:1–11. doi: 10.7589/0090-3558-43.1.1. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Imported case of Marburg hemorrhagic fever—Colorado, 2008. Morb Mortal Wkly Rep. 2009a;58:1377–1381. [PubMed] [Google Scholar]
- CDC. Biosafety in microbiological and biomedical laboratories. Public Health Service Centers for Disease Control and Prevention, National Institutes of Health; Atlanta, Georgia: 2009b. HHS Publication No. (CDC) 21-1112. [Google Scholar]
- Committee for the Update of the Guide for the Care and Use of Laboratory Animals, National Research Council of the National Academies. Guide for the care and use of laboratory animals. 8. National Academy Press; Washington, DC: 2011. p. 220. [Google Scholar]
- Jacobsen NHG, Du Plessis E. Observations on the ecology and biology of the Cape fruit bat Rousettus aegyptiacus leachi in the Eastern Transvaal. S Afr J Sci. 1976;72:270–273. [Google Scholar]
- Kingdon J. East African mammals, an atlas of evolution in Africa, Volume IIA (insectivores and bats) University of Chicago Press; Chicago, Illinois: 1974. p. 341. [Google Scholar]
- Ksiazek TG, Rollin PE, Williams AJ, Bressler DS, Martin ML, Swanepoel R, Burt FJ, Leman PA, Khan AS, Rowe AK, et al. Clinical virology of Ebola hemorrhagic fever (EHF): Virus, virus antigen, and IgG and IgM antibody findings among EHF patients in Kikwit, Democratic Republic of the Congo, 1995. J Infect Dis. 1999a;179:S177–S187. doi: 10.1086/514321. [DOI] [PubMed] [Google Scholar]
- Ksiazek TG, West CP, Rollin PE, Jahrling PB, Peters CJ. ELISA for the detection of antibodies to Ebola viruses. J Infect Dis. 1999b;179:S192–S198. doi: 10.1086/514313. [DOI] [PubMed] [Google Scholar]
- Kwiecinski GG, Griffiths TA. Rousettus egyptiacus (aegyptiacus) Mamm Species. 1999;611:1–9. [Google Scholar]
- Paweska JT, van Vuran JP, Masumu J, Leman PA, Grobbelaar AA, Birkhead M, Clift S, Swanepoel R, Kemp A. Virological and serological findings in Rousettus aegyptiacus experimentally inoculated with Vero cells-adapted Hogan strain of Marburg virus. PLoS One. 2012;7:e45479. doi: 10.1371/journal.pone.0045479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rupprecht CE, Hanlon CA, Hemachudha T. Rabies re-examined. Lancet Infect Dis. 2002;2:327–343. doi: 10.1016/s1473-3099(02)00287-6. [DOI] [PubMed] [Google Scholar]
- Siegert R, Shu HL, Slenczka HL, Peters D, Muller G. The aetiology of an unknown human infection transmitted by monkeys (preliminary communication) Ger Med Mon. 1968;13:1–2. [PubMed] [Google Scholar]
- Swanepoel R, Leman PA, Burt FJ, Zachariades NA, Braack LE, Ksiazek TG, Rollin PE, Zaki SR, Peters CJ. Experimental inoculation of plants and animals with Ebola virus. Emerg Infect Dis. 1996;2:321–325. doi: 10.3201/eid0204.960407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanepoel R, Smit SB, Rollin PE, Formenty P, Leman PA, Kemp A, Burt FJ, Grobbelaar AA, Croft J, Bausch DG, et al. Studies of reservoir hosts for Marburg virus. Emerg Infect Dis. 2007;13:1847–1851. doi: 10.3201/eid1312.071115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timen A, Koopmans MP, Vossen AC, van Doornum GJ, Gunther S, van den Berkmortel F, Verduin KM, Dittrich S, Emmerich P, Osterhaus AD, et al. Response to imported case of Marburg hemorrhagic fever, the Netherlands. Emerg Infect Dis. 2009;15:1171–1175. doi: 10.3201/eid1508.090051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towner JS, Khristova ML, Sealy TK, Vincent MJ, Erickson BR, Bawiec DA, Hartman AL, Comer JA, Zaki SR, Stroher U, et al. Marburg-virus genomics and association with a large hemorrhagic fever outbreak in Angola. J Virol. 2006;80:6497–6516. doi: 10.1128/JVI.00069-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towner JS, Pourrut X, Albarino CG, Nkogue CN, Bird BH, Grard G, Ksiazek TG, Gonzalez JP, Nichol ST, Leroy EM. Marburg virus infection detected in a common African bat. PLoS One. 2007;2:e764. doi: 10.1371/journal.pone.0000764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towner JS, Amman BR, Sealy TK, Carroll SA, Comer JA, Kemp A, Swanepoel R, Paddock CD, Balinandi S, Khristova ML, et al. Isolation of genetically diverse Marburg viruses from Egyptian fruit bats. PLoS Pathog. 2009;5:e1000536. doi: 10.1371/journal.ppat.1000536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DE, Reeder DM. Mammal species of the world. 3. Smithsonian Institution Press; Washington, DC: 2005. p. 2142. [Google Scholar]