Abstract
Background
Identifying early markers of risk for anxiety disorders in children may aid in understanding underlying mechanisms and informing prevention efforts. Affective modulation of the startle response indexes sensitivity to pleasant and unpleasant environmental contexts and has been shown to relate to anxiety, yet the extent to which abnormalities in affect-modulated startle reflect vulnerability for anxiety disorders in children has yet to be examined. The current study assessed the effects of parental psychopathology on affective modulation of startle in offspring.
Methods
Nine-year-old children (N=144) with no history of anxiety or depressive disorders completed a passive picture viewing task in which eye blink startle responses were measured during the presentation of pleasant, neutral, and unpleasant images.
Results
Maternal anxiety was associated with distinct patterns of affective modulation of startle in offspring, such that children with maternal histories of anxiety showed potentiation of the startle response while viewing unpleasant images, but not attenuation during pleasant images, whereas children with no maternal history of anxiety exhibited attenuation of the startle response during pleasant images, but did not exhibit unpleasant potentiation—even when controlling for child symptoms of anxiety and depression. No effects of maternal depression or paternal psychopathology were observed.
Conclusions
These findings suggest that both enhanced startle responses in unpleasant conditions and failure to inhibit startle responses in pleasant conditions may reflect early-emerging vulnerabilities that contribute to the later development of anxiety disorders.
Anxiety disorders are the most common class of psychological disorders (Kessler et al. 2005), causing significant burden and suffering and highlighting the need for more effective prevention efforts (e.g., Donovan & Spence 2000, Zvolensky et al. 2006). Identifying trait-like, predisposing factors, or vulnerabilities (Ingram & Luxton 2005), for anxiety disorders may aid in elucidating mechanisms contributing to the development of these disorders and lead to more effective prevention efforts. Research examining youth at high risk for anxiety, such as children with parental histories of anxiety disorders, is a particularly useful approach for identifying potential vulnerability factors (Merikangas et al. 1998, Merikangas et al. 1999).
The startle response is a physiological measure of defensive responding that may be relevant for understanding the development of anxiety disorders. The startle response is a reflexive, cross-species fight-or-flight response to sudden, intense stimuli that is characterized by a cascade of behavioral responses, including rapid muscle contraction, and is most reliably assessed in through eye blinks in humans (e.g., Lang et al. 1990, Grillon 2002, Grillon and Baas 2003). As a measure of defensive responding, startle magnitude is potentiated in the context of a matching motivational or emotional state (e.g., fear) and inhibited in the context of an antithetical state (e.g., happiness); thus, startle is modulated by both pleasant and unpleasant affective states (Vrana et al., 1988, Bradley et al. 1990, Lang et al. 1990, Grillon and Baas 2003). Two common paradigms for assessing modulation of the startle response include affective modulation paradigms in which startle probes are presented while participants view both pleasant and unpleasant stimuli, and fear learning paradigms in which startle probes are presented along with cues that predict threat (e.g., threat of shock) and safety (e.g., no threat of shock).
Many previous studies have found evidence of abnormal modulation of startle responses in adults with anxiety disorders, though results vary across disorders (Grillon & Baas 2003, Vaidyanathan et al. 2009). In general, anxiety is associated with enhanced startle responses in threatening conditions, particularly when the threat is relevant to the disorder, with exaggerated startle responses most apparent in fear disorders (Lang and McTeague 2009, McTeague & Lang 2012). Individuals with specific phobias exhibit increased startle responses in the context of stimuli that are related to their fear (de Jong et al. 1991, Vrana et al. 1992, de Jong et al. 1996), social anxiety has been linked to heightened startle responses in the context of a socially threatening situation (Cornwell et al. 2006, McTeague & Lang 2012), and panic disorder has been associated with enhanced startle reactivity in threat conditions (Melzig et al. 2007, Shankman et al. 2013). Anxiety may also be characterized by abnormal startle responses in pleasant conditions. For example, symptoms of anxious arousal have been linked to enhanced startle responses during viewing of both pleasant and unpleasant images (Larson et al. 2007).
On the other hand, anxiety characterized by more chronic and pervasive avoidance and distress has been linked to attenuated startle responses (Lang & McTeague 2009, McTeague & Lang 2012). In addition, despite high comorbidity with anxiety (e.g., Fava et al. 2000), depression in adults has been associated with distinct abnormalities in modulation of startle, including reduced modulation of startle responses in both unpleasant and pleasant conditions (Allen et al. 1999, Dichter et al. 2004, Kaviani et al. 2004, Forbes et al. 2005, Dichter & Tomarken 2008). There is also evidence that comorbid depression may blunt affect-modulated startle effects among adults with anxiety disorders (Melzig et al. 2007, Vaidyanathan et al. 2009, Taylor-Clift et al. 2011).
Relatively few studies have evaluated startle in youth with anxiety disorders, though there is evidence of increased whole-body startle responses overall among anxious youth (Bakker et al. 2009). In addition, in two studies with small samples of anxious children, anxiety was related to increased startle responses overall at early stages of processing and after switching from the habituation to affective modulation phase of the startle task (Waters et al. 2005, Waters et al. 2008). More recently, in a fear-potentiated startle paradigm, adolescents with fear disorders (i.e., social or specific phobia) exhibited enhanced startle responses during safety cues and early phases of threat cues (Waters et al. 2014). However, another recent study failed to find differences in fear-potentiated startle in children and adolescents with generalized anxiety disorder (GAD) or social phobia compared to controls (Britton et al. 2013).
Importantly, there is some evidence suggesting that distinct patterns of modulation of the startle reflex may reflect a vulnerability to anxiety. Offspring of parents with anxiety disorders have been shown to exhibit heightened startle responses (Grillon & Dierker 1997, Grillon et al. 1998, Merikangas et al. 1999), with high-risk males exhibiting greater fear-potentiated startle (i.e., larger startle responses during fearful than neutral stimuli) and high-risk females exhibiting larger startle responses overall compared to low-risk youth (Grillon et al. 1998). Relatedly, exaggerated startle responses to unpredictable threat have been observed in individuals with a family history of panic disorder (Nelson et al. 2013). In addition to heightened startle responses to threat conditions, larger startle responses in safe conditions have been observed among children higher in trait anxiety (Jovanovic et al. 2014) and in children high in behavioral inhibition – a risk factor for anxiety (Barker, Reeb-Sutherland, & Fox 2014). Moreover, enhanced startle responses in safe conditions have been found to prospectively predict first onset of anxiety disorders from adolescence into young adulthood (Craske et al. 2012). These findings raise the possibility that failure to inhibit startle responses in safe, or pleasant emotional, contexts may play a role in the development of clinical anxiety.
Although there is growing evidence that abnormal startle responses may reflect a vulnerability for anxiety, a number of gaps in knowledge remain. First, previous studies have indicated that generalized defensive responses to safety cues may contribute to the development of anxiety (Reeb-Sutherland et al. 2009, Craske et al. 2012), which raises the question of how those at risk for anxiety may respond during pleasant emotional contexts. Second, previous research has focused on older children or adolescents and/or included youth with lifetime histories of anxiety or depressive disorders. In order to evaluate startle responses as a vulnerability for anxiety, it is necessary to examine these patterns earlier in childhood and prior to the onset of symptoms (e.g., Kraemer et al. 1997). Lastly, it is unclear whether abnormal affective modulation of startle may indicate risk for the broad class of anxiety disorders or a relatively specific vulnerability for certain disorders (e.g., fear disorders), as well as the extent to which startle modulation relates to risk for depression.
The current study evaluated associations between affective modulation of the startle response and anxiety risk in middle childhood. Eye blink startle responses during pleasant, neutral, and unpleasant images were measured in 144 nine-year-old children with no histories of mood or anxiety disorders. The primary goal was to evaluate startle responses as a vulnerability for anxiety, hypothesizing that children at high risk for anxiety (i.e., offspring of mothers or fathers with histories of anxiety disorder) would exhibit greater potentiation of the startle response in the context of unpleasant emotional images, as well as less attenuation of startle responses in the context of pleasant images compared to children at low risk (i.e., no parental history of anxiety). Additional exploratory aims were to evaluate main and interactive effects of maternal and paternal history of depression on startle responses in offspring and whether specific anxiety disorders in parents had stronger effects than others on the startle response in offspring.
Method
Participants
Participants were part of a larger longitudinal sample recruited through a commercial mailing list (Olino et al. 2010). At the initial assessment, children were eligible if they were three years old, had no significant medical conditions or developmental disabilities, and were living with at least one English-speaking biological parent (some participants were recruited at a follow up assessment in order to increase the racial/ethnic diversity of the sample). Participants were invited back to the laboratory as close as possible to their 9th birthdays, at which time a subset of the sample completed the startle paradigm. A total of 274 children completed the startle task. Of these children, 10 ended the task early due to technical difficulties or refusal to continue participation (resulting in too few trials for analysis), 67 were excluded due to excessive artifacts in the baseline period (50 ms before the startle probe) resulting in less than 50% artifact-free trials in one or more picture conditions, and 27 were excluded for failing to exhibit a measurable startle response on 50% or more trials per condition (nonresponses). Acceptable startle data were available for 170 children (62.0%), which is comparable to exclusion rates in previous startle studies with children (e.g., Glenn et al. 2012). Children included in analyses had 3–6 useable trials with observable startle responses in each picture condition. Children with acceptable startle data did not significantly differ from excluded participants with regard to depression or anxiety symptoms or frequency of parental depression or anxiety (ps>.11).
In order to evaluate risk for future anxiety, children who had already experienced a lifetime anxiety disorder (n=23) or lifetime mood disorder (n=3) were excluded from analyses.1 The final sample consisted of 144 children (56.9% male). Mean age at the startle assessment was 9.17 years (SD=.43). With regard to ethnicity, 13.2% of the final sample was Hispanic, and with regard to race, 92.4% was Caucasian, 4.9% African American, 2.1% Asian, and 0.7% Native American.
Parental Psychopathology
Detailed methods for assessing parental psychopathology are described in Kujawa, Proudfit, & Klein (2014). Both biological mothers and fathers were interviewed using the Structured Clinical Interview for DSM-IV non-patient version (SCID; First et al. 1996) when families initially entered the study and again when children returned to the lab at age 9 to complete the startle task. Interviews were conducted by advanced doctoral students and masters-level clinicians in person or by telephone, which generally yields comparable results to face-to-face interviews (Sobin et al. 1993, Rohde et al. 2005). Interrater reliability was acceptable at both the initial (kappa=0.91 for lifetime anxiety disorder and 0.93 for lifetime depressive disorder; n=30) and follow up assessments (kappa=0.73 for anxiety disorders and 0.91 for depressive disorders, n=45). Diagnoses from both assessments were combined to yield lifetime diagnoses. In cases where completion of the SCID with one parent was not possible, family history information was obtained from the other parent using a semi-structured interview (Andreasen et al., 1977). Diagnoses for eight fathers were derived using the family history method.
Child Psychopathology
At the age 9 assessment, one parent and the child were interviewed by advanced doctoral students or a masters-level clinician using the DSM-IV version of the Schedule of Affective Disorders and Schizophrenia for School-Age Children (K-SADS; Axelson et al. 2009). To assess interrater reliability, a second rater independently derived ratings from videotapes for 74 participants. Kappas for anxiety and depressive disorders were .68 and .79, respectively (see Kujawa et al. 2014 for details). Parents also completed the Screen for Child Anxiety Related Emotional Disorders (SCARED; Birmaher et al. 1997) to assess current child symptoms of anxiety, as well as the Children’s Depression Inventory (CDI; Kovacs 1992) to assess current child symptoms of depression. Child symptoms of anxiety and depression were included as covariates in main analyses.
Affect-Modulated Startle Paradigm
Stimuli and Presentation
Participants passively viewed 36 developmentally-appropriate images (12 pleasant, 12 neutral, and 12 unpleasant) from the International Affective Picture System (IAPS; Lang et al. 2008)2 divided into 2 blocks of 18 images. Neutral images included pictures of objects and scenes (e.g., lamp, desert), unpleasant images consisted of threatening stimuli (e.g., vicious animals, people with weapons) and pleasant images included a range of child-friendly scenes (e.g., cute animals, children having fun). IAPS images were presented randomly for 5 seconds each, with no more than 2 images of the same category presented consecutively. Intertrial intervals (ITI) ranged from 6 to 8 seconds for trials in which no startle probe was presented during ITI, and 11 to 15 seconds on trials in which startle probes were presented during the ITI.
Auditory startle probes, consisting of 50 ms approximately 95 dB bursts of white noise with near instantaneous rise time, were presented binaurally through headphones. Startle probes were produced with a noise/tone generator (Contact Precision Instruments; Cambridge, MA) and were presented randomly between 3, 4, or 5 seconds after picture or ITI onset in order to increase unpredictability of the startle probes and produce maximal affective modulation of the startle reflex (Bradley et al. 1993). During the experiment, startle probes were randomly presented during 6 neutral, 6 pleasant, 6 unpleasant, and 6 ITI periods.
Startle Procedure
All participants were tested in a dimly-lit, sound-attenuated enclosure, with the door propped slightly in order to make the children more comfortable. An initial 4-trial habituation phase was used to reduce extreme startle responses from the first few trials. During the task, children were instructed to sit still and passively view the images presented on the screen. Participants were monitored by a video camera in order to ensure compliance with instructions.
Startle Reflex Data Collection and Processing
Startle-elicited EMG activity was collected in accordance with current guidelines (Blumenthal et al. 2005). Two electrodes, 4 mm diameter Ag-AgCl filled with electrode gel (TD-40; Mansfield R and D), were positioned beneath the left eye with the first electrode placed in line with the pupil and the second electrode placed lateral to the first over the orbicularis oculi muscle with distance between electrodes adjusted as needed for each child’s facial anatomy, and a third electrode was placed on the forehead to serve as an isolated ground. EMG activity was recorded using a PSYLAB Stand Alone Monitor (SAM) unit and an attached BioAmplifier system (Contact Precision Instruments; Cambridge, MA), and was sampled at 1000 Hz and filtered between 30 and 500 Hz. EMG responses were rectified in a window 200 milliseconds long, beginning 50 milliseconds before the onset of the startle probe. A 6-point running average was applied to the rectified data to smooth out sharp peaks. Raw startle magnitude was expressed as the difference between the average of the EMG in the 50 ms window prior to the startle probe and the maximum in the 150 ms post-probe window. Each participant’s data were examined on a trial-by-trial basis. Trials with no perceptible eye blink response were scored as zero and included in the overall averages; trials with excessive baseline artifacts or magnitudes that were outliers for each subject were excluded from analysis.
Data Analysis
In order to control for interindividual variability in startle magnitudes, analyses focused on ITI-corrected (i.e., average of startle magnitudes during an emotion condition minus startle magnitude during ITI) startle magnitudes. A mixed-design ANCOVA was used to statistically evaluate startle responding during the three affective conditions with maternal and paternal history of anxiety and depressive disorders as between-subjects variables. Child sex, symptoms of depression and symptoms of anxiety were included as covariates to evaluate risk for psychopathology controlling for child symptoms. Significant results were followed by paired-samples t-tests; the Benjamini–Hochberg procedure was used to control the false discovery rate for multiple comparisons (Benjamini & Hochberg 1995).
Results
Participant Characteristics
With regard to parental psychopathology, 34.0% (n=49) of mothers and 20.8% (n=30) of fathers had histories of anxiety disorders (9.0% [n=13] of children had two parents with histories of anxiety disorders). The most common anxiety disorders were specific phobias (16.7% [n=24] mothers, 6.3% [n=9] of fathers) and social phobia (12.5% [n=18] of mothers, 7.6% [n=11] of fathers). Rates of panic disorder (6.3% [n=9] of mothers, 4.2% [n=6] of fathers), GAD (4.9% [n=7] of mothers, 4.2% [n=6] of fathers), obsessive-compulsive disorder (OCD; 4.2% [n=6] of mothers, 2.8% [n=4] of fathers), and post-traumatic stress disorder (PTSD; 2.1% [n=3] of mothers, 0.0% of fathers) were relatively low. In addition, 9.7% of mothers (n=14) and 3.5% of fathers (n=5) were diagnosed with two or three lifetime anxiety disorders.
With regard to depression, 32.6% (n=46) of mothers and 12.5% (n=18) of fathers met criteria for a lifetime depressive disorder (MDD or dysthymia), and 13.8% of mothers (n=20) and 4.2% of fathers (n=6) had comorbid depression and anxiety.
Child SCARED (M=5.76, SD=4.91) and CDI (M=5.79, SD=4.07) scores were relatively low. Higher CDI scores were observed among children with maternal histories of anxiety, t(142)=−2.18, p=.03, d=.38, and maternal histories of depression, t(142)=−2.70, p=.01, d=.45, but associations between SCARED scores and maternal psychopathology did not reach significance (ps>.08). None of the associations between child symptoms and paternal depression or anxiety were significant (ps>.14).
Effect of Parental Anxiety and Depression on Affect-Modulated Startle
A 3 (condition: pleasant, neutral, unpleasant) × 2 (maternal anxiety) × 2 (maternal depression) × 2 (paternal anxiety) × 2 (paternal depression) mixed-design ANCOVA was computed to evaluate effects of parental psychopathology on affective modulation of startle, with child sex and symptoms of depression and anxiety included as covariates.3
The interaction between foreground picture type and maternal history of anxiety was significant, F(2, 272)=4.20, p=.02, ηp2=.03, but all other interactions between emotion condition and between-subjects variables were not significant (ps>.47). In addition, the main effect of emotion condition did not reach significance when accounting for the interaction, F(2, 272)=0.40, p=.67, ηp2=.00.4 With regard to between-subjects effects, none of the main effects of parental psychopathology or child variables reached significance (ps>.29)5.
In order to evaluate the interaction between affective modulation of startle and maternal history of anxiety, data were split by maternal anxiety, and a within-subjects ANOVA was computed to evaluate the effects of emotion condition for children with (i.e., high risk) and without (i.e., low risk) maternal histories of anxiety disorders (Figure 1). Because effects of paternal psychopathology, maternal depression, sex, and child symptoms of depression and anxiety were not significant in the overall model, these variables were not included in follow up analyses. Affective modulation of the startle response was apparent for both low-risk, F(2, 188)=5.36, p=.01, ηp2=.05, and high-risk children, F(2, 96)=4.20, p=.01, ηp2=.10. However, the direction of the affective modulation differed between the two groups: low-risk children exhibited significant attenuation of the startle response during pleasant compared to both neutral, t(94)=2.16, p=.03, d=.30, and unpleasant picture conditions, t(94)=3.45, p=.001, d=.48, but the startle response during unpleasant images was not significantly potentiated relative to neutral, t(94)=-.89, p=.38, d=.12. On the other hand, high-risk children exhibited significant potentiation of the startle response during unpleasant compared to neutral images, t(48)=−3.20, p=.002, d=.63, with a trend for potentiated startle response during unpleasant relative to pleasant pictures, t(48)=2.01, p=.05, d=.40 (corrected p value=.076, Benjamini & Hochberg 1995). Among high-risk children, attenuation of the startle response was not apparent for pleasant relative to neutral pictures, t(48)= −1.19, p=.24, d=.23.6 In order to directly compare low-risk and high-risk children, we evaluated group effects based on two difference scores: (1) unpleasant potentiation: unpleasant startle magnitude minus neutral startle magnitude (greater unpleasant potentiation scores indicate larger startle responses during unpleasant stimuli), and (2) pleasant attenuation: neutral startle magnitude minus pleasant startle magnitude (greater pleasant attenuation scores indicate larger attenuation of the startle response during pleasant stimuli). Compared to children at relatively low risk, children at high risk for anxiety exhibited greater unpleasant potentiation, t(142)=2.22, p=.03, d=.39, and less pleasant attenuation, t(142)= −2.25, p=.03, d=.39, of the startle response.
Figure 1.
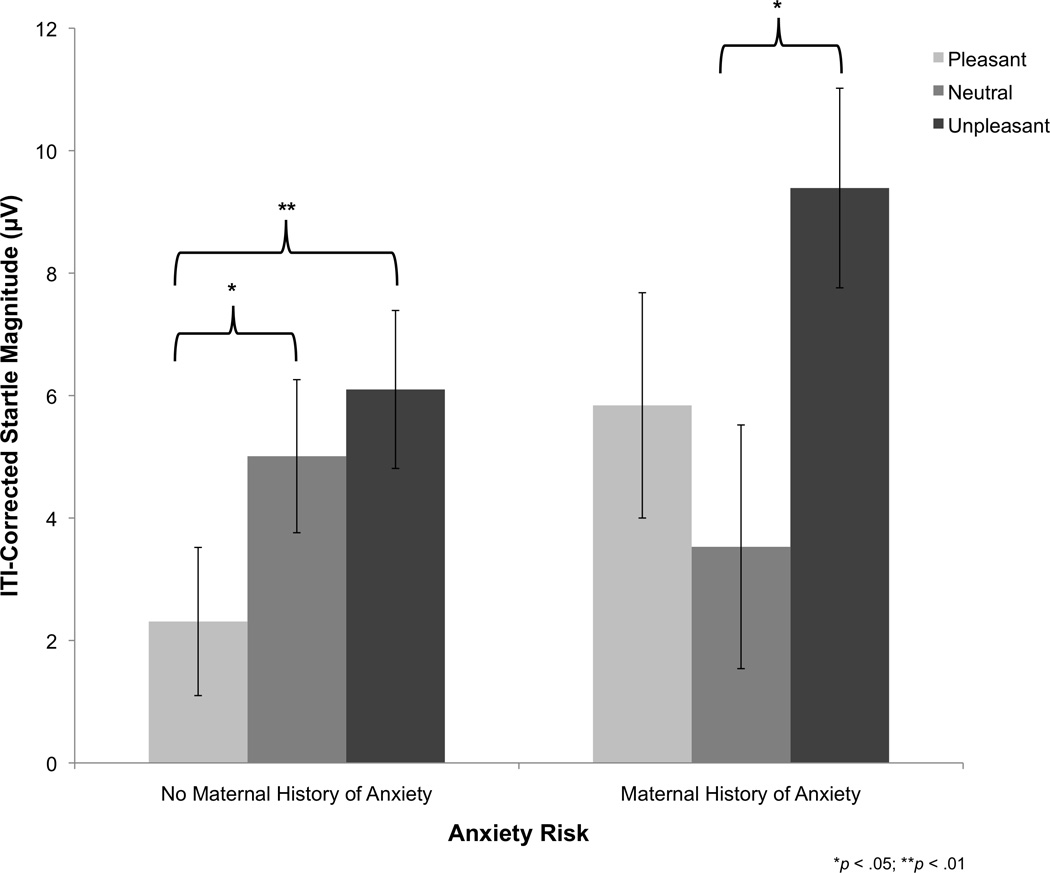
Affective modulation of the startle response in offspring as a function of maternal history of anxiety disorders (bars represent standard error).
Exploratory analyses were computed to evaluate whether specific maternal anxiety disorders uniquely predicted greater unpleasant potentiation and/or reduced pleasant attenuation of the startle response. Two ANOVAs were examined with the unpleasant potentiation and pleasant attenuation difference scores as the criterion variables. Maternal history of panic disorder, specific phobia, and social phobia were included as between-subjects factors in each model. Variables indicating GAD, PTSD, and OCD were not included because fewer than 5% of mothers met criteria for these disorders (ns=7, 3, and 6, respectively).7 Both panic disorder, F(1, 140)=4.90, p=.03, ηp2=.03, and social phobia, F(1, 140)=4.34, p=.04, ηp2=.03, were uniquely associated with greater unpleasant potentiation, but the effect of specific phobia on unpleasant potentiation was not significant, F(1, 140)=.002, p=.96, ηp2=.00. In addition, panic disorder, F(1, 140)=8.41, p=.004, ηp2=.06, and social phobia, F(1, 140)=4.15, p=.04, ηp2=.03, were associated with less pleasant attenuation, but the effect of specific phobia on pleasant attenuation was not significant, F(1, 140)=.03, p=.87, ηp2=.00.
Discussion
We evaluated affective modulation of the eye blink startle response among children at high and low risk for anxiety disorders based on parental history of anxiety. Compared to children with no maternal history of anxiety, offspring of mothers with anxiety disorders exhibited greater potentiation of the startle response while viewing unpleasant pictures, as well as less attenuation of startle during pleasant pictures. That is, children at high risk for anxiety may be characterized both by heightened defensive reactivity in unpleasant or threatening contexts and a failure to inhibit defensive mobilizations in pleasant contexts. To our knowledge, the current study is the first to evaluate affective modulation of startle responses by both pleasant and unpleasant stimuli in risk for anxiety; thus, our findings extend Craske et al.’s (2012) study by suggesting that in addition to heightened responses to safety cues, failure to inhibit defensive responding in pleasant conditions may contribute to vulnerability for anxiety.
Importantly, based on the design of the current study, we can conclude that the affect-modulated startle effects were not driven by children’s psychopathology, as no children met lifetime criteria for internalizing disorders, levels of current dimensional symptoms of internalizing disorders in the children were low, and we controlled for child symptoms of depression and anxiety in our analysis. Thus, abnormal affective modulation of startle does not appear to reflect a state marker or a consequence of a disorder, but instead may be a vulnerability that precedes the onset of anxiety and may play a causal role in the development of symptoms of anxiety (Kraemer et al. 1997, Ingram and Luxton 2005).
Effects of parental anxiety on startle responses in offspring were specific to maternal history of anxiety, with no effects observed for paternal anxiety. To our knowledge, this study is the first to evaluate the unique effects of maternal and paternal anxiety on startle in offspring. The lack of effects for paternal anxiety disorders is surprising given previous evidence of abnormal startle responses in a combined group of youth with maternal and/or paternal anxiety disorders (Grillon et al. 1997, Grillon et al. 1998). However, very little previous research has examined effects of maternal and paternal anxiety separately on outcomes in offspring, and it has been suggested that fathers may play different roles in the development of anxiety in offspring than mothers (Bögels & Phares 2008). In addition, the current results are consistent with previous evidence of stronger effects of maternal compared to paternal anxiety on anxiety disorders in offspring (McClure et al. 2001). That is, maternal anxiety may be associated with greater risk to offspring, possibly due to greater involvement by mothers in early parenting and more opportunities for mothers to model defensive reactions. It is important to also note that rates of anxiety disorders were lower among fathers than mothers, and diagnoses for a small proportion of fathers (5.5%) were obtained using family history interview methods; therefore, we cannot rule out the possibility that there was lower power to detect effects of paternal anxiety.
Though anxiety disorders characterized by focal fears have been linked to exaggerated startle responses in fearful or threatening conditions (Grillon & Baas 2003, Lang & McTeague 2009, Vaidyanathan et al. 2009, McTeague & Lang 2012), there is also evidence of attenuated modulation of startle responses to threat in more chronic anxiety and comorbid depression (Melzig et al. 2007, Vaidyanathan et al. 2009, Taylor-Clift et al. 2011, McTeague & Lang 2012). We did not find evidence of attenuated startle responses in unpleasant conditions among children at high risk for anxiety and failed to find effects of parental depression on startle responses. Instead, our findings indicate that risk for anxiety is characterized by exaggerated startle responses to threat. This finding raises the possibility that, for some individuals, enhanced defensive responding early in life may develop into reduced defensive reactivity in adulthood, with the onset of depressive symptoms and more pervasive and chronic distress (McTeague & Lang 2012). In addition, our results suggest that abnormalities in affect-modulated startle responses may be relatively specific to risk for anxiety rather than depression, which is consistent with previous evidence that startle responses during safety cues prospectively predict the development of anxiety but not depression (Craske et al. 2012).
Lastly, our results were relatively specific to parental history of social phobia and panic disorder, as opposed to specific phobia. Though modestly heritable, specific phobias have been shown to be less influenced by genes than other anxiety disorders and to often arise in response to specific traumatic events (Öst & Hugdahl, 1981, Kendler et al. 1992), which may account for the lack of effects of maternal specific phobias on startle responses in offspring.
A few limitations of the current study should be noted. First, given low rates of parental GAD, PTSD, and OCD in the sample, we were unable to adequately evaluate specific effects of these disorders on offspring startle responses, which may be an important area to consider in future work. In addition, we focused on children within a narrow range of development in middle childhood, which limits ability to generalize effects into adolescence or across development. It should also be noted that we did not ask participants to rate valence or arousal of the stimuli; thus, we are unable to evaluate group differences in subjective experience of the images. Lastly, data from a significant proportion (38.0%) of children were excluded due to children refusing to complete the task or inability to obtain enough artifact-free trials with visible startle responses, which raises the importance of developmental considerations and future work on optimal methods for obtaining startle data in childhood. Nonetheless, the current results suggest that distinct patterns of affect-modulated startle responses may be an early-emerging vulnerability for anxiety, which may be particularly useful for identifying children at greatest risk for anxiety and developing more targeted prevention efforts.
Acknowledgments
This work was supported by National Institute of Mental Health Grant RO1 MH069942 to Daniel N. Klein.
Footnotes
We did not find evidence that history of anxiety disorders in children predicted startle responses (ps>.64), which is likely due to limited power to detect effects given the relatively small number of children with an anxiety disorder as well as variability across disorders. For example, 39.1% of children with anxiety disorders had diagnoses of specific phobia, which may be associated with heightened startle responses only in the context of the feared stimulus (McTeague, Lang, Wangelin, Laplante, & Bradley, 2012).
IAPS images: Pleasant (1463, 1710, 1750, 1811, 2070, 2091, 2224, 2340, 2345, 7325, 7330, 8496), Neutral (5390, 5500, 5731, 5740, 5900, 7002, 7010, 7026, 7090, 7100, 7175), Unpleasant (1050, 1052, 1205, 1300, 1304, 2458, 2811, 3022, 6190, 6231, 6510, 6571). Based on normative ratings in adults (Lang et al. 2008), pleasant images mean (SD) valence=7.71(0.41), neutral images valence=5.28(0.31), unpleasant images valence=3.29(0.69); pleasant images mean (SD) arousal=4.84(0.61), neutral images arousal=2.76(0.71), and unpleasant images arousal=6.19(0.64)
The model was initially tested with two-way interactions between parental psychopathology variables included (e.g., maternal depression X maternal anxiety) to test for effects of comorbidity; however, none of the interactions reached significance. Thus, all interactions between parental psychopathology variables were removed from the final model.
There was evidence for affective modulation in the overall within-subjects ANOVA, F(2, 286)=7.13, p=.001, ηp2=.05. Unpleasant images significantly potentiated the startle response compared to both neutral, t(143)=2.63, p=.01, d=.30, and pleasant images, t(143)=3.95, p<.001, d=.45. The comparison between startle magnitude on neutral and pleasant trials did not reach significance, t(143)=0.93, p=.36, d=.11.
We also evaluated the model including the interaction between maternal anxiety and child sex. The effect of maternal history of anxiety was not significantly moderated by child sex (ps>.27).
No significant differences between maternal anxiety groups were observed for ITI startle magnitude, t(142)=−.18, p=.86, mean difference=−0.74, suggesting that differences in baseline startle response did not account for affective modulation effects.
Thus, the 7 children with a maternal history of GAD, PTSD or OCD but not panic disorder, social phobia of specific phobia were treated as not having maternal anxiety disorders. We also tested models that included variables for maternal GAD, PTSD and OCD; panic disorder and social phobia continued to be associated with greater unpleasant potentiation and less positive attenuation.
References
- Allen NB, Trinder J, Brennan C. Affective startle modulation in clinical depression: Preliminary findings. Biological Psychiatry. 1999;46:542–550. doi: 10.1016/s0006-3223(99)00025-6. [DOI] [PubMed] [Google Scholar]
- Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria: Reliability and validity. Archives of General Psychiatry. 1977;34:1229–1235. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- Axelson D, Birmaher B, Zelazny J, Kaufman J, Gill MK. The Schedule for Affective Disorders and Schizophrenia--Present and Lifetime Version (K-SADS-PL) 2009 working draft. Advanced Centre for Intervention and Services Research, Western Psychiatric Institute and Clinics. 2009 ( http://www.Psychiatry.Pitt.Edu/research/tools-research/ksads-pl-2009-working-draft) [Google Scholar]
- Bakker MJ, Tijssen MAJ, Van Der Meer JN, Koelman JHTM, Boer F. Increased whole-body auditory startle reflex and autonomic reactivity in children with anxiety disorders. Journal of Psychiatry & Neuroscience. 2009;34:314–322. [PMC free article] [PubMed] [Google Scholar]
- Barker TV, Reeb-Sutherland BC, Fox NA. Individual differences in fear potentiated startle in behaviorally inhibited children. Developmental Psychobiology. 2014;56:133–141. doi: 10.1002/dev.21096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. 1995:289–300. [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Blumenthal TD, Cuthbert BN, Filion DL, Hackley S, Lipp OV, Van Boxtel A. Committee report: Guidelines for human startle eyeblink electromyographic studies. Psychophysiology. 2005;42:1–15. doi: 10.1111/j.1469-8986.2005.00271.x. [DOI] [PubMed] [Google Scholar]
- Bögels S, Phares V. Fathers’ role in the etiology, prevention, and treatment of child anxiety: A review and new model. Clinical Psychology Review. 2008;28:539–558. doi: 10.1016/j.cpr.2007.07.011. [DOI] [PubMed] [Google Scholar]
- Bradley MM, Cuthbert BN, Lang PJ. Startle reflex modification: Emotion or attention? Psychophysiology. 1990;27:513–522. doi: 10.1111/j.1469-8986.1990.tb01966.x. [DOI] [PubMed] [Google Scholar]
- Bradley MM, Cuthbert BN, Lang PJ. Pictures as prepulse: Attention and emotion in startle modification. Psychophysiology. 1993;30:541–545. doi: 10.1111/j.1469-8986.1993.tb02079.x. [DOI] [PubMed] [Google Scholar]
- Britton JC, Grillon C, Lissek S, Norcross MA, Szuhany KL, Chen G, Pine DS. Response to learned threat: An fMRI study in adolescent and adult anxiety. American Journal of Psychiatry. 2013;170:1195–1204. doi: 10.1176/appi.ajp.2013.12050651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell BR, Johnson L, Berardi L, Grillon C. Anticipation of public speaking in virtual reality reveals a relationship between trait social anxiety and startle reactivity. Biological Psychiatry. 2006;59:664–666. doi: 10.1016/j.biopsych.2005.09.015. [DOI] [PubMed] [Google Scholar]
- Craske MG, Wolitzky–Taylor KB, Mineka S, Zinbarg R, Waters AM, Vrshek–Schallhorn S, Epstein A, Naliboff B, Ornitz E. Elevated responding to safe conditions as a specific risk factor for anxiety versus depressive disorders: Evidence from a longitudinal investigation. Journal of Abnormal Psychology. 2012;121:315. doi: 10.1037/a0025738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Jong P, Merckelbach H, Arntz A. Eyeblink startle responses in spider phobies before and after treatment: A pilot study. Journal of Psychopathology and Behavioral Assessment. 1991;13:213–223. [Google Scholar]
- De Jong P, Visser S, Merckelbach H. Startle and spider phobia: Unilateral probes and the prediction oi treatment ellects. Journal of Psychophysiology. 1996;10:150–160. [Google Scholar]
- Dichter GS, Tomarken AJ. The chronometry of affective startle modulation in unipolar depression. Journal of Abnormal Psychology. 2008;117:1–15. doi: 10.1037/0021-843X.117.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dichter GS, Tomarken AJ, Shelton RC, Sutton SK. Early-and late-onset startle modulation in unipolar depression. Psychophysiology. 2004;41:433–440. doi: 10.1111/j.1469-8986.00162.x. [DOI] [PubMed] [Google Scholar]
- Donovan CL, Spence SH. Prevention of childhood anxiety disorders. Clinical Psychology Review. 2000;20:509–531. doi: 10.1016/s0272-7358(99)00040-9. [DOI] [PubMed] [Google Scholar]
- Fava M, Rankin MA, Wright EC, Alpert JE, Nierenberg AA, Pava J, Rosenbaum JF. Anxiety disorders in major depression. Comprehensive Psychiatry. 2000;41:97–102. doi: 10.1016/s0010-440x(00)90140-8. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. The Structured Clinical Interview for DSM-IV Axis I Disorders - Non-Patient Editions. New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Forbes EE, Miller A, Cohn JF, Fox NA, Kovacs M. Affect-modulated startle in adults with childhood-onset depression: Relations to bipolar course and number of lifetime depressive episodes. Psychiatry Research. 2005;134:11–25. doi: 10.1016/j.psychres.2005.01.001. [DOI] [PubMed] [Google Scholar]
- Glenn CR, Klein DN, Lissek S, Britton JC, Pine DS, Hajcak G. The development of fear learning and generalization in 8–13 year-olds. Developmental Psychobiology. 2012;54:675–684. doi: 10.1002/dev.20616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grillon C. Startle reactivity and anxiety disorders : Aversive conditioning, context, and neurobiology. Biological Psychiatry. 2002;52:958–975. doi: 10.1016/s0006-3223(02)01665-7. [DOI] [PubMed] [Google Scholar]
- Grillon C, Baas J. A review of the modulation of the startle reflex by affective states and its application in psychiatry. Clinical Neurophysiology. 2003;114:1557–1579. doi: 10.1016/s1388-2457(03)00202-5. [DOI] [PubMed] [Google Scholar]
- Grillon C, Dierker L, Merikangas KR. Startle modulation in children at risk for anxiety disorders and/or alcoholism. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:925–932. doi: 10.1097/00004583-199707000-00014. [DOI] [PubMed] [Google Scholar]
- Grillon C, Dierker L, Merikangas KR. Fear-potentiated startle in adolescent offspring of parents with anxiety disorders. Biological Psychiatry. 1998;44:990–997. doi: 10.1016/s0006-3223(98)00188-7. [DOI] [PubMed] [Google Scholar]
- Ingram RE, Luxton DD. Vulnerability-stress models. In: Hankin BL, Abela JRZ, editors. Development of Psychopathology: A Vulnerability-Stress Perspective. Thousand Oaks: Sage Publications; 2005. pp. 32–46. [Google Scholar]
- Jovanovic T, Nylocks KM, Gamwell KL, Smith A, Davis TA, Norrholm SD, Bradley B. Development of fear acquisition and extinction in children: Effects of age and anxiety. Neurobiology of Learning and Memory. 2014;113:135–142. doi: 10.1016/j.nlm.2013.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaviani H, Gray J, Checkley S, Raven P, Wilson G, Kumari V. Affective modulation of the startle response in depression: Influence of the severity of depression, anhedonia, and anxiety. Journal of Affective Disorders. 2004;83:21–31. doi: 10.1016/j.jad.2004.04.007. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. The genetic epidemiology of phobias in women: The interrelationship of agoraphobia, social phobia, situational phobia, and simple phobia. Archives of General Psychiatry. 1992;49:273–281. doi: 10.1001/archpsyc.1992.01820040025003. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month dsm-iv disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. Children's Depression Inventory. Toronto: Multi-Health Systems; 1992. [Google Scholar]
- Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, Kupfer DJ. Coming to terms with the terms of risk. Archives of General Psychiatry. 1997;54:337–343. doi: 10.1001/archpsyc.1997.01830160065009. [DOI] [PubMed] [Google Scholar]
- Kujawa A, Proudfit GH, Klein DN. Neural reactivity to rewards and losses in offspring of mothers and fathers with histories of depressive and anxiety disorders. Journal of Abnormal Psychology. 2014;123:287–297. doi: 10.1037/a0036285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang PJ, Bradley MM, Cuthbert BN. Emotion, attention, and the startle reflex. Psychological Review. 1990;97:377–395. [PubMed] [Google Scholar]
- Lang PJ, Bradley MM, Cuthbert BN. International Affective Picture System (IAPS): Affective Ratings of Pictures and Instructional Manual. Technical report A-8. Gainesville: University of Florida; 2008. [Google Scholar]
- Lang PJ, McTeague LM. The anxiety disorder spectrum: Fear imagery, physiological reactivity, and differential diagnosis. Anxiety, Stress, & Coping. 2009;22:5–25. doi: 10.1080/10615800802478247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson CL, Nitschke JB, Davidson RJ. Common and distinct patterns of affective response in dimensions of anxiety and depression. Emotion. 2007;7:182–191. doi: 10.1037/1528-3542.7.1.182. [DOI] [PubMed] [Google Scholar]
- McClure EB, Brennan PA, Hammen C, Le Brocque RM. Parental anxiety disorders, child anxiety disorders, and the perceived parent–child relationship in an australian high-risk sample. Journal of Abnormal Child Psychology. 2001;29:1–10. doi: 10.1023/a:1005260311313. [DOI] [PubMed] [Google Scholar]
- McTeague LM, Lang PJ. The anxiety spectrum and the reflex physiology of defense: From circumscribed fear to broad distress. Depression and Anxiety. 2012;29:264–281. doi: 10.1002/da.21891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McTeague LM, Lang PJ, Wangelin BC, Laplante MC, Bradley MM. Defensive mobilization in specific phobia: Fear specificity, negative affectivity, and diagnostic prominence. Biological Psychiatry. 2012;72:8–18. doi: 10.1016/j.biopsych.2012.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melzig CA, Weike AI, Zimmermann J, Hamm AO. Startle reflex modulation and autonomic responding during anxious apprehension in panic disorder patients. Psychophysiology. 2007;44:846–854. doi: 10.1111/j.1469-8986.2007.00560.x. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Avenevoli S, Dierker L, Grillon C. Vulnerability factors among children at risk for anxiety disorders. Biological Psychiatry. 1999;46:1523–1535. doi: 10.1016/s0006-3223(99)00172-9. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Dierker LC, Szatmari P. Psychopathology among offspring of parents with substance abuse and/or anxiety disorders: A high–risk study. Journal of Child Psychology and Psychiatry. 1998;39:711–720. [PubMed] [Google Scholar]
- Nelson BD, Mcgowan SK, Sarapas C, Robison-Andrew EJ, Altman SE, Campbell ML, Gorka SM, Katz AC, Shankman SA. Biomarkers of threat and reward sensitivity demonstrate unique associations with risk for psychopathology. Journal of Abnormal Psychology. 2013;122:662–671. doi: 10.1037/a0033982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino TM, Klein DN, Dyson MW, Rose SA, Durbin CE. Temperamental emotionality in preschool-aged children and depressive disorders in parents: Associations in a large community sample. Journal of Abnormal Psychology. 2010;119:468–478. doi: 10.1037/a0020112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öst L-G, Hugdahl K. Acquisition of phobias and anxiety response patterns in clinical patients. Behaviour Research and Therapy. 1981;19:439–447. doi: 10.1016/0005-7967(81)90134-0. [DOI] [PubMed] [Google Scholar]
- Reeb-Sutherland BC, Helfinstein SM, Degnan KA, Pérez-Edgar K, Henderson HA, Lissek S, Chronis-Tuscano A, Grillon C, Pine DS, Fox NA. Startle response in behaviorally inhibited adolescents with a lifetime occurrence of anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48:610–617. doi: 10.1097/CHI.0b013e31819f70fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Klein DN, Seeley JR. Association of parental depression with psychiatric course from adolescence to young adulthood among formerly depressed individuals. Journal of Abnormal Psychology. 2005;114:409–420. doi: 10.1037/0021-843X.114.3.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankman SA, Nelson BD, Sarapas C, Robison-Andrew EJ, Campbell ML, Altman SE, Mcgowan SK, Katz AC, Gorka SM. A psychophysiological investigation of threat and reward sensitivity in individuals with panic disorder and/or major depressive disorder. Journal of Abnormal Psychology. 2013;122:322–328. doi: 10.1037/a0030747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobin C, Weissman MM, Goldstein RB, Adams P. Diagnostic interviewing for family studies: Comparing telephone and face-to-face methods for the diagnosis of lifetime psychiatric disorders. Psychiatric genetics. 1993;3:227–233. [Google Scholar]
- Taylor-Clift A, Morris B, Rottenberg J, Kovacs M. Emotion-modulated startle in anxiety disorders is blunted by co-morbid depressive episodes. Psychological Medicine. 2011;41:129–139. doi: 10.1017/S003329171000036X. [DOI] [PubMed] [Google Scholar]
- Vaidyanathan U, Patrick CJ, Cuthbert BN. Linking dimensional models of internalizing psychopathology to neurobiological systems: Affect-modulated startle as an indicator of fear and distress disorders and affiliated traits. Psychological Bulletin. 2009;135:909–942. doi: 10.1037/a0017222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrana SR, Constantine JA, Westman JS. Startle reflex modification as an outcome measure in the treatment of phobia: Two case studies. Behavioral Assessment. 1992;14:279–291. [Google Scholar]
- Vrana SR, Spence EL, Lang PJ. The startle probe response: A new measure of emotion? Journal of Abnormal Psychology. 1988;97:487–491. doi: 10.1037//0021-843x.97.4.487. [DOI] [PubMed] [Google Scholar]
- Waters AM, Lipp OV, Spence SH. The effects of affective picture stimuli on blink modulation in adults and children. Biological Psychology. 2005;68:257–281. doi: 10.1016/j.biopsycho.2004.05.002. [DOI] [PubMed] [Google Scholar]
- Waters AM, Nazarian M, Mineka S, Zinbarg RE, Griffith JW, Naliboff B, Ornitz EM, Craske MG. Context and explicit threat cue modulation of the startle reflex: Preliminary evidence of distinctions between adolescents with principal fear disorders versus distress disorders. Psychiatry Research. 2014;217:93–99. doi: 10.1016/j.psychres.2014.01.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters AM, Neumann DL, Henry J, Craske MG, Ornitz EM. Baseline and affective startle modulation by angry and neutral faces in 4–8-year-old anxious and non-anxious children. Biological Psychology. 2008;78:10–19. doi: 10.1016/j.biopsycho.2007.12.005. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Schmidt NB, Bernstein A, Keough ME. Risk-factor research and prevention programs for anxiety disorders: A translational research framework. Behaviour Research and Therapy. 2006;44:1219–1239. doi: 10.1016/j.brat.2006.06.001. [DOI] [PubMed] [Google Scholar]


