TO THE EDITOR
Proton pump inhibitors (PPIs) are highly effective in treating gastric acid-related disorders but are often overused.1 Intravenous (IV) PPIs are expensive compared to oral PPIs and have few absolute indications; over half of hospitalized patients prescribed IV PPIs could instead receive oral PPIs.2 Health information technologies have the potential to improve physician ordering of medications, but have not been applied to IV PPIs.3
METHODS
On October 21, 2011, our institution introduced an alert that was triggered by all IV PPI orders, excluding continuous infusion PPIs. Esomeprazole is our institution’s only formulary PPI. The alert explains that oral PPIs cost one-tenth as much as IV PPIs, yet are 90% bioavailable (Supplementary Figure). Provider response to the alert was automatically captured. Our primary outcome was a change in the proportion of all PPIs given intravenously during one year before the alert compared to one year after the alert, assessed retrospectively using an interrupted time series analysis.4 There were no other interventions related to PPI ordering during the study period. Multivariable logistical regression modeling was performed to assess predictors of an IV compared to oral PPI order, stratified by alert period. To characterize orders in terms of indications, we randomly selected 50 charts from before and 50 charts from after alert implementation, and classified IV PPI orders as indicated or not indicated based on criteria derived from current guidelines.
RESULTS
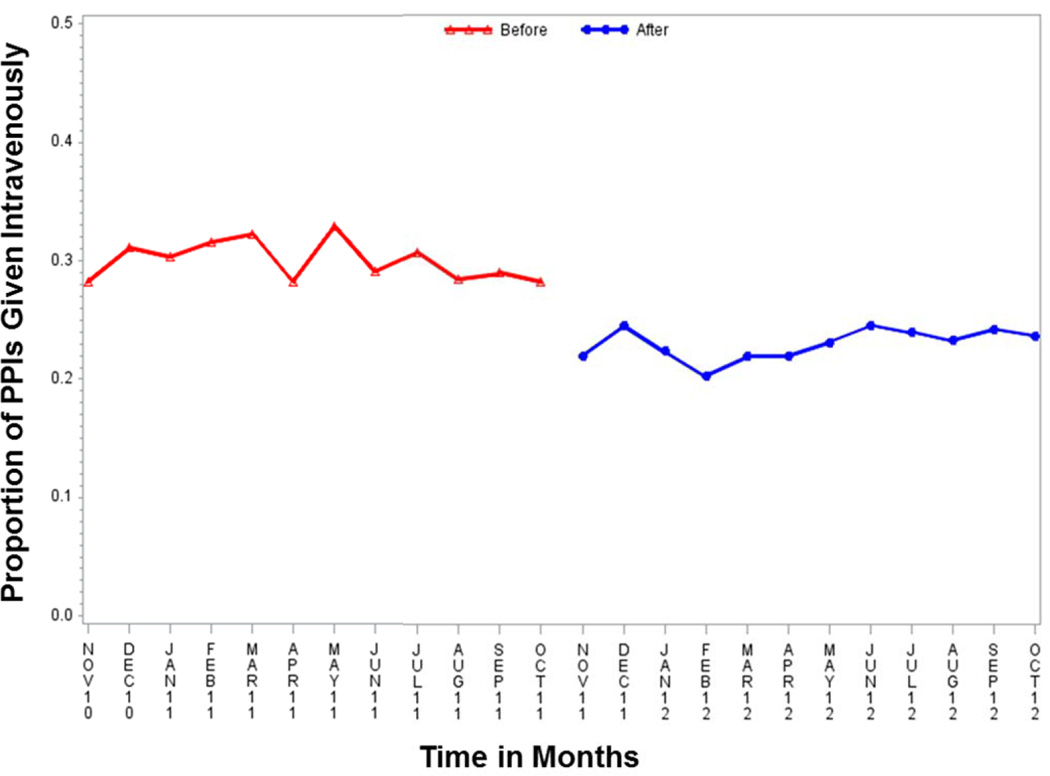
During the two year study period there were 65,078 completed orders for PPIs, including 10,050 (30.0%) orders for IV PPIs before alert implementation and 7,247 (23.0%) orders for IV PPIs after implementation (chi-squared p < 0.001), representing a 7.0% absolute and 23.4% relative reduction in the proportion of PPIs given intravenously (Figure). During the year before the alert, the proportion of PPIs ordered intravenously decreased an average of 0.7% monthly (p = 0.049). After adjusting for the trend in IV PPI use before the alert, the proportion of PPIs given intravenously remained significantly decreased after implementation of the alert (p < 0.001). Provider-level factors were significant predictors of IV compared to oral route of PPI administration, including the presence of the PPI within an order set (Table). There was a non-significant trend towards improved indication after implementation of the alert (88.0% indicated after vs. 74.0% before; p = 0.074). Based on the institutional cost differences between IV and oral PPIs and the observed reduction in IV PPI orders during the year after the alert, we estimate a $450,692 annual decrease in institutional costs related to IV PPI use.
Figure. Proportion of proton pump inhibitors (PPIs) given intravenously before and after implementation of an electronic alert, November 2010 – October 2012.
Red line with triangles indicates the proportion of PPIs given intravenously before the alert was implemented on October 21, 2011; blue line with squares indicates the proportion of PPIs given intravenously after the alert.
Table.
Multivariable logistic regression analysis for odds of completing an intravenous compared to oral proton pump inhibitor order, stratified by alert period
| Before Alert Implementation | After Alert Implementation | |||||
|---|---|---|---|---|---|---|
| Risk factor | Total PPI orders |
IV orders (% total) |
Adjusted OR (95% CI) |
Total PPI orders |
IV orders (% total) |
Adjusted OR (95% CI) |
| Total | 33520 | 10050 (30.0%) | N/A | 31558 | 7247 (23.0%) | N/A |
| Order frequency | ||||||
| Once daily or less | 30142 | 8474 (28.1%) | Reference | 28464 | 6131 (21.5%) | Reference |
| More than daily | 3378 | 1576 (46.7%) | 2.95 (2.72–3.21) | 3094 | 1116 (36.1%) | 2.61 (2.39–2.85) |
| Service | ||||||
| Medicine | 19796 | 5637 (28.5%) | Reference | 18265 | 3627 (19.9%) | Reference |
| Surgery | 9783 | 3599 (36.8%) | 1.18 (1.11–1.25) | 9797 | 3193 (32.6%) | 1.47 (1.38–1.56) |
| Neurology | 2953 | 526 (17.8%) | 0.60 (0.54–0.68) | 2600 | 265 (10.2%) | 0.46 (0.40–0.53) |
| Ob/gyn | 647 | 280 (43.3%) | 3.72 (3.10–4.47) | 529 | 159 (30.1%) | 2.70 (2.18–3.33) |
| Psychiatry | 341 | 8 (2.3%) | 0.11 (0.05–0.22) | 367 | 3 (0.8%) | 0.06 (0.02–0.19) |
| Provider role | ||||||
| Physician | 25950 | 8023 (30.9%) | Reference | 23169 | 5364 (23.1%) | Reference |
| NP/PA | 7480 | 2019 (27.0%) | 0.75 (0.70–0.81) | 8277 | 1878 (22.3%) | 0.82 (0.76–0.88) |
| Medical student | 90 | 8 (8.9%) | 0.26 (0.12–0.59) | 112 | 5 (4.5%) | 0.27 (0.11–0.68) |
| Order set | ||||||
| No | 27583 | 6700 (24.3%) | Reference | 25957 | 4773 (18.4%) | Reference |
| Yes | 5937 | 3350 (56.4%) | 3.93 (3.65–4.23) | 5601 | 2474 (44.2%) | 2.91 (2.70–3.14) |
| Diet Status | ||||||
| Any diet | 14272 | 1542 (10.8%) | Reference | 14084 | 1052 (7.5%) | Reference |
| NPO | 7859 | 5164 (65.7%) | 14.0 (13.0–15.0) | 6821 | 3812 (55.9%) | 12.0 (11.0–13.0) |
| No order | 11389 | 3344 (29.4%) | 4.07 (3.79–4.38) | 10653 | 2383 (22.4%) | 3.88 (3.57–4.21) |
DISCUSSION
Intravenous PPIs are frequently given in situations where oral PPIs would suffice. We found that implementation of an electronic alert for IV PPI orders was associated with a 23% relative decrease in the proportion of PPIs with IV route of administration. This result was significant after adjusting for the trend in the proportion of PPIs ordered intravenously before implementation of the alert. The decrease in the proportion of PPIs ordered intravenously was immediate, sustained, accompanied by an overall decrease in IV PPI orders, and associated with significant cost savings. There was also a trend towards improved indications for IV PPIs after the alert.
There is little prior data evaluating electronic interventions seeking to improve PPI use.5 In the outpatient setting, pharmacist-based electronic interventions may reduce overall PPI use.6 Inpatient studies have evaluated use of computerized decision support in changing IV to oral medication orders, but have not targeted IV PPIs.7 Our findings suggest that, if providers are educated to make a clearly defined change with a simple but focused alert, oral PPIs will frequently be substituted for IV PPIs. Provider-level factors were also an important determinant of PPI route of administration. Compared to the medical service, the surgical or obstetrics services were more likely to order IV versus oral PPIs. This was true both before and after the alert, and after adjusting for patient diet status; however, this study was not designed to address the reasons underlying these differences. Notably, presence of the IV PPI within an order set strongly predicted IV compared to oral PPI use both before and after alert implementation.
Our study highlights the potential for electronic alerts to alter ordering behavior for IV PPIs. Institutions seeking to decrease IV PPI use should consider removing IV PPIs from order sets, and future studies should test whether additional targeted interventions using clinical decision support systems can improve PPI overuse.
Supplementary Material
Acknowledgments
Funding/Support: Dr Freedberg was supported in part by a grant from the National Center for Advancing Translational Sciences (UL1 TR000040) formerly the National Center for Research Resources (UL1 RR024156) and by a training grant from the National Institute of Diabetes and Digestive and Kidney Diseases (T32 DK083256-0). Dr Salmasian was supported in part by a training grant from the National Library of Medicine (T15 LM007079). Dr Abrams was supported in part by a Career Development Award from the National Cancer Institute (K07 CA 132892).
Additional Contributions: The authors thank Alfred I. Neugut for his thoughtful comments on the manuscript during revision.
Footnotes
Author Contributions: Dr Freedberg had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Freedberg, Abrams, Green. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: Freedberg. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Freedberg, Salmasian, Abrams. Obtained funding: Freedberg, Salmasian, Abrams. Administrative, technical, or material support: All authors. Study supervision: Freedberg, Green.
Conflict of Interest Disclosures: None.
Previous Presentation: This article was presented at the annual conference of the American College of Gastroenterology on October 13, 2013.
Contributor Information
Daniel E. Freedberg, Division of Digestive and Liver Diseases, Columbia University Medical Center, New York, New York.
Hojjat Salmasian, Department of Biomedical Informatics, Columbia University Medical Center, New York, New York.
Julian A. Abrams, Division of Digestive and Liver Diseases, Columbia University Medical Center, New York, New York.
Robert A. Green, Department of Emergency Medicine, Columbia University Medical Center and New York-Presbyterian Hospital, New York, New York.
REFERENCES
- 1.Heidelbaugh JJ, Goldberg KL, Inadomi JM. Overutilization of proton pump inhibitors: a review of cost-effectiveness and risk [corrected] Am J Gastroenterol. 2009;104(Suppl 2):S27–S32. doi: 10.1038/ajg.2009.49. [DOI] [PubMed] [Google Scholar]
- 2.Kaplan GG, Bates D, McDonald D, et al. Inappropriate use of intravenous pantoprazole: extent of the problem and successful solutions. Clin Gastroenterol Hepatol. 2005;3(12):1207–1214. doi: 10.1016/s1542-3565(05)00757-3. [DOI] [PubMed] [Google Scholar]
- 3.Chin HL, Wallace P. Embedding guidelines into direct physician order entry: simple methods, powerful results. Proc AMIA Symp. 1999:221–225. [PMC free article] [PubMed] [Google Scholar]
- 4.Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 5.Smeets HM, Hoes AW, de Wit NJ. Effectiveness and costs of implementation strategies to reduce acid suppressive drug prescriptions: a systematic review. BMC Health Serv Res. 2007;7:177. doi: 10.1186/1472-6963-7-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curtain C, Peterson GM, Tenni P, et al. Outcomes of a decision support prompt in community pharmacy-dispensing software to promote step-down of proton pump inhibitor therapy. Br J Clin Pharmacol. 2011;71(5):780–784. doi: 10.1111/j.1365-2125.2010.03890.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galanter W, Liu XF, Lambert BL. Analysis of computer alerts suggesting oral medication use during computerized order entry of i.v. medications. Am J Health Syst Pharm. 2010;67(13):1101–1105. doi: 10.2146/ajhp090357. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.