This column series compares neurological conditions that pose differential challenges in diagnoses.
Fahr’s disease and Fahr’s syndrome are two conditions characterized by calcification in certain areas of the brain that results in neurological and/or psychiatric sequelae in patients. While the symptoms and signs of both conditions may resemble one another, there are distinct, critical differences that exist regarding the etiology, location of lesions, prognosis, and treatment. Thus, it is important for clinicians to be familiar with the similarities and differences between Fahr’s disease and Fahr’s syndrome, so that an accurate diagnosis can be made and appropriate therapy initiated.
A diagnosis of either Fahr’s disease or Fahr’s syndrome should be considered if some or all of the following symptoms are present:
|
Consider a diagnosis of Fahr’s disease if
|
Consider a diagnosis of Fahr’s syndrome if
and Presence of any of the following endocrinopathies:
or Presence of any of the following:
|
|
Treatment If Fahr’s disease—
If Fahr’s syndrome—
|
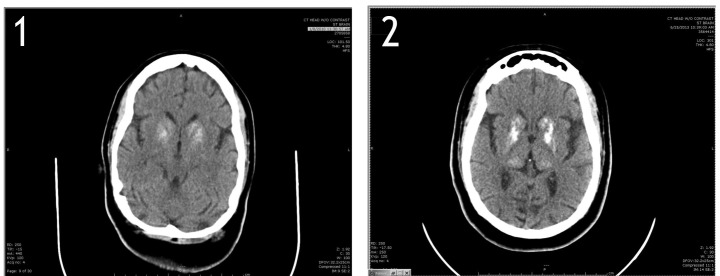
FIGURES 1 and 2.
Computerized tomographic scans of the head in 2010 (Figure 1) and 2013 (Figure 2) reveal coarse bilateral, symmetrical calcifications in the basal ganglia, with progression in 2013.
Images reprinted with permission. Goyal et al. Would you recognize Fahr’s disease if you saw it? Innov Clin Neurosci. 2014;11(1–2):26–28
Footnotes
FUNDING:No funding was provided for the preparation of this article.
FINANCIAL DISCLOSURES:The authors have no conflicts of interest relevant to the content of this article.
REFERENCES
- 1.Asokan AG, D’souza S, Jeganathan J, Pai S. Fahr’s syndrome: an interesting case presentation. J Clin Diagn Res. 2013;7(3):5302–5303. doi: 10.7860/JCDR/2013/4946.2814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saleem S, Aslam HM, Anwar M, et al. Fahr’s syndrome: literature review of current evidence. Orphanet J Rare Dis. 2013;8:156. doi: 10.1186/1750-1172-8-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goyal D, Mashal Khan M, Quereshi B, et al. Would you recognize Fahr’s disease if you saw it? Innov Clin Neurosci. 2014;11(1-2):26–28. [PMC free article] [PubMed] [Google Scholar]
- 4.Faye AD, Gawande S, Tadke R, et al. A case of psychosis due to Fahr’s syndrome and response to behavioral disturbances with risperidone and oxcarbazepine. Indian J Psychiatry. 2014;56(2):188–190. doi: 10.4103/0019-5545.130506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manyam BV, Walters AS, Narla KR. Bilateral striopallido dentate calcinosis: clinical characteristics of patients seen in a registry. Mov Disord. 2001;16(2):258–264. doi: 10.1002/mds.1049. [DOI] [PubMed] [Google Scholar]
- 6.Ramen C. Basak. A case report of basal ganglia calcification: a rare finding of hypoparathyroidism. Oman Med J. 2009;24(3):220–222. doi: 10.5001/omj.2009.44. [DOI] [PMC free article] [PubMed] [Google Scholar]