Abstract
Background
The most commonly recommended initial treatment for multidirectional instability is a rehabilitation program. Although there is evidence to support the effect of conservative management on this condition, the published literature provides little information on the exercise parameters of such programs. In addition, current published rehabilitation programs for multidirectional instability do not focus on scapula stability or exercise drills into functional and sports-specific positions, which are often important aspects to consider in this patient population.
Methods
The aim of this paper (Part 1) is to outline the first two stages of a six-stage rehabilitation program for the conservative management of multidirectional instability with a focus on scapula control and exercise drills into functional positions.
Results and Conclusions
This clinical protocol is currently being tested for efficacy as part of a randomized controlled trial (Australian New Zealand Clinical Trials Registry #ACTRN12613001240730). The information in this paper and additional online supplementary files will provide therapists with adequate detail to replicate the rehabilitation program in the clinical setting.
Keywords: exercise, multidirectional instability, scapula, shoulder, rehabilitation
Definition, Aetiology and Management
Multidirectional instability (MDI) of the glenohumeral joint is the symptomatic subluxation or dislocation occurring in two1,2 or three directions.3,4 There is general agreement that the pathology is primarily a result of repetitive micro-trauma imposed on a congenitally lax and redundant joint capsule.5,6 Patients with MDI have reduced muscle strength and altered neuromuscular control compared to controls.1,7 Patients have scapulae that rest in downward rotation and have deficient upward rotation through range,8,9 reducing the contact area between the humeral head (HH) and the glenoid, resulting in excessive HH translation.10,11 Symptoms range from mild reports of pain to apprehension,12 impingement,13 rotator cuff pain14 and neuropathic symptoms.15
The most commonly recommended initial treatment for MDI is a rehabilitation program.16 The rationale is that strengthening the scapula and rotator cuff muscles compensates for the lack of passive stability and assists in active control of the shoulder.2,17 A recent systematic review revealed evidence supporting exercise for MDI;16 however, the quality of the evidence was very low because the literature were confounded by a high level of bias. To date, only one published paper by Rockwood and Burkhead18 has outlined a rehabilitation program for MDI in sufficient detail to enable replication in the clinical setting. Despite the detail provided, the program has little focus on scapula or HH control and lacks exercise drills into higher degrees of shoulder elevation. Considering that patients with MDI often have a need to regain scapula and HH control, especially in overhead activities,9,19 these limitations may result in sub-optimal outcomes for patients using this program.
This paper (Part 1) outlines the first two stages of a six-stage rehabilitation program that has preliminary evidence for improved instability specific outcomes, shoulder muscle strength and scapular upward rotation in patients with MDI.20,21 The program is currently being compared with the Rockwood instability program in a randomized controlled trial (Australian New Zealand Clinical Trials Registry #ACTRN12613001240730).
The Watson MDI program: overview
The Watson Program is primarily based around retraining and maintaining good scapula and HH control through six stages. The program was developed over 25 years of clinical experience in treating patients with MDI,21 with reference to MDI rehabilitation programs in the literature18,22–24 and with consideration of the specific biomechanical deficits often present in MDI.8,11 The program has two primary components: Assessment and Intervention.
The program provides therapists with a set of principles to guide treatment selection. The stages of the program are not strictly sequential and do allow for individualized exercise prescription. The principals of assessment, along with clinical reasoning skills, are used by the therapist to guide treatment decisions. The program duration is 3 months to 6 months, depending on patient presentation.25
The Watson rogram: assessment
Assessment within the context of this section refers to the approach used to determine the appropriate prescription of exercise, not the definitive diagnosis of MDI.
The effect of correction
The effect of manual correction is a key component of the Watson Program because it determines whether rehabilitation is likely to be of benefit, as well as the scapula and/or HH position the patient will need to retrain and maintain throughout the program. The effect of manual correction involves therapist assistance of the scapula and/or HH when the patient performs an objective test to determine whether the assisted position improves the result of that test.21,26–31 Poor scapula positioning through range and altered muscle patterning are predominant characteristics of nontraumatic MDI32,33 and so an immediate improvement with manual assistance is likely to confirm the presence of these characteristics and indicate that the patient is appropriate for treatment with exercise.31 Although the reliability and validity of some shoulder corrective techniques have been established,34,35 to date, research on the reliability and validity and on establishing normative values for shoulder corrective tests in MDI is incomplete.
The steps for assessing the effect of correction are as follows:
The patient performs an objective test (i.e. movement test, strength test) and the therapist notes scapula dyskinesis, symptoms onset, range of motion or strength deficits, and/or HH subluxation, depending on the objective test chosen.
The therapist manually assists the scapula, then HH, and then a combination of both into a position that corrects the faulty biomechanics (e.g. correction into scapula upward rotation if downward rotation was observed) at the same time as reassessing the objective test; noting any improvements in pain levels, range of motion, strength, patient apprehension or HH subluxation.
The correction position that most improves the patient's symptoms is the one that is retrained and adopted throughout the Watson Program.
If none of the patient’s objective tests improve with correction, the therapist must consider whether there are other factors contributing to the patient’s presentation, such as a structural lesion or an inflammatory component. Further investigations or medical management may be warranted prior to commencing rehabilitation in such cases.
Scapula correction
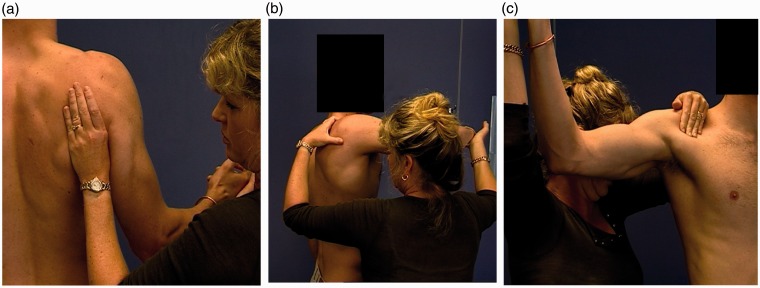
Scapula correction is performed by supporting the patient’s scapula, under the axilla through range or during an isometric strength testing (Figure 1a).26,28 Commonly, flexion and abduction range of motion or isometric external rotation (ER) are used to assess the effect of scapula correction. The most common positions of scapula correction for patients with MDI are one of (or a combination of) slight upward rotation (10°), elevation (1 cm to 2 cm) and posterior tilt (5°).21,27
Figure 1.
(a) Effect of correction into upward rotation when assessing external rotation strength. (b) Anterior to posterior humeral head (HH) correction during resisted external rotation at 90° elevation. Resited internal rotation can also be utilized. (c) Posterior to anterior HH correction during loaded horizontal flexion. Note that variations do exist in the direction of subluxation of the HH in some patients, depending on their primary direction of instability.
Humeral head correction
Humeral head correction is performed by applying a gentle anterior to posterior or posterior to anterior34,35 pressure to the HH.21,31,36 For assessing the correction of anterior translation, the assessment of active ER in varying degrees of abduction3,36 or isometric ER is commonly employed (Figure 1b). For assessing the correction of posterior translation, flexion3 or horizontal flexion range of motion is commonly employed (Figure 1c).
The Watson rogram: intervention
An overview of stages 1 to 2 of the Watson Program is outlined in Table 1 and detailed flow charts of stage 1 to 2 are provided in the Supporting information.
Table 1.
Overview of the Watson MDI Program: Stages 1 to 2.
| Stage | Aims | Potential drills | Dosage/load | Goals | Considerations |
|---|---|---|---|---|---|
| Stage 1 | |||||
| Scapula phase | Develop scapula stability to centre HH | Scapula UR in standing +/– elevation +/– 20° to 30° Abd +/– posterior tilt | 1 to 3 × 20 repetitions (60 repetitions per day) 5-second holds 2 × day 0 kg to 0.5 kg to 1 kg in hand Red- green SR band | Standing UR 3 × 20 repetitions 1 kg +/– green SR band | Side-lying UR if unable to do > 5 repetitions standing 0° Arm Abd if any supraspinatus pain |
| Arc of motion phase | Gain control in 0° to 45° of abduction in coronal plane | For ER/IR/Ext control: ER/IR/Ext isometrics Ext to neutral with TB ER with TB IR with TB For ER strength: Side-lying off support +/– SR band | For ER/IR/Ext control: Isometrics: 5 to 10 × 5 second holds (20% to 30% MVC), 2 to 3 × day TB drills: Dosage:1 to 3 × 20, 2 × day Load: yellow–red TB For ER strength: Dosage: 1 to 3 × 20 repetitions, 2 × day Load: 0 kg to 0.5 kg to 1 kg | 1 or 2 × 20 repetitions ER red/green TB 1 or 2 × 20 repetitions IR, red/green TB 1 or 2 × 20 repetitions Ext row green TB 1 or 2 × 20 repetitions side-lying ER 1 kg | IR after ER control established Isometrics if arc cannot be controlled/drill is pain provoking Side-lying off a support and rolled up towel under arm Palpate anterior HH in ER for unwanted anterior translation |
| Stage 2 | |||||
| Develop posterior musculature for flexion | UR in standing +/posterior tilt/elevation ER with TB Side-lying off support BOR with weight Ext row with TB at 45° Abd +/– SR band | 1 to 3 × 20 repetitions, 1 or 2 times a day TB drills: green Side-lying: 1 kg to 1.5 kg to 2 kg BOR: 0.5 kg to 1 kg to 1.5 kg to 2 kg | 3 × 20 repetitions UR: 2 kg Side-lying: 1.5 kg to 2 kg ER: Green TB BOR: 2 kg Ext Row 45°: Green TB | BOR and standings rows to the side of the body only (neutral extension) |
Repetitions of exercises held for 3 seconds to 5 seconds. Abd, abduction; BOR, bent over row; ER, external rotation; Ext, extension; HH, humeral head; IR, internal rotation; SR, scapula resistance; TB, TheraBand™; UR, upward rotation. *Dosage and load can be progressed from a recruitment and endurance dosage to a dosage and load functionally required by the patient. Exercises may need to be progressed to blue or black bands or heavier weights if functionally required by the patient. For the detailed flow charts for the Watson MDI Program, see the Supporting information.
Stage 1: Scapula control and coronal plane control at 0° to 30° abduction
The aim of stage 1 is to develop scapula and HH control in 0° of abduction. Stage 1 is divided into the scapula setting phase and the arc of motion phase. The scapula setting phase forms the foundation of the Watson Program and needs to be mastered by the patient before moving onto the arc of motion phase.
Scapula setting phase
The aim of the scapula setting phase is to develop adequate scapula stability to centralize the HH,11 and prepare for the arcs of motion. The optimal scapula position is derived from the effect of correction in assessment. The position is commonly upward rotation (10°) and possibly some posterior tilt (5°).27
A scapula upward rotation drill is utilized to retrain the upward rotators.26,37 This drill is performed in standing with the arm by the side and abducted to 20° to 30° (Figure 2a). This position has been shown to recruit the upward rotators of the scapula significantly more compared to the arm by the side.37 Some elevation and/or posterior tilt can be combined with this scapula upward rotation drill if required by the patient. A recruitment dosage is utilized for this stage because altering faulty motor patterns is the aim.38 Ideally, the patient is asked to achieve three sets of 20 repetitions in a 10-minute period, one or two times a day, because there is evidence to suggest that this dosage may assist in motor reorganization.39
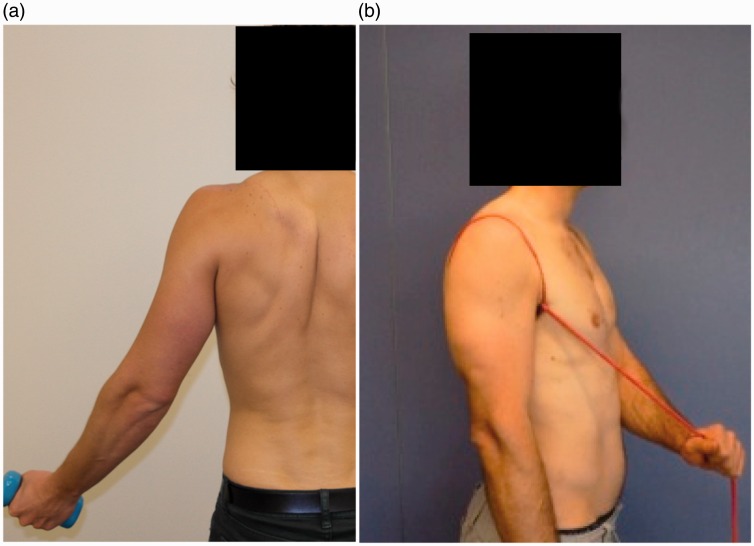
Figure 2.
(a) Standing scapula setting into upward rotation shrug in 20° to 30° of abduction. (b) Scapula setting into upward rotation and posterior tilt, using an scapula resistance band.
Once the patient can achieve this with the weight of the arm, a scapula resistance (SR) band can be utilized to facilitate greater muscle activation. The SR band is placed around the patient’s scapula and resists a setting action and has been shown to significantly activate all components of the trapezius and rhomboids,40 which can enhance scapula stability.20 The SR band can be used to resist upward rotation, elevation and/or posterior tilt depending on where the TheraBand™ (Hygenic Corporation, Akron, OH, USA) is anchored (Figure 2b). Once the patient can achieve three sets of 20 with the SR band, 0.5 kg and then 1 kg weights are added in the hand.
Patients who are unable to perform at least five repetitions when standing as a result of very poor scapula upward rotation or deep cervical flexor strength may need to start this drill in a side-lying position until they can recommence the drill in standing. The patient is generally able to progress to the arc of motion stage when they can perform their scapula drill against a SR band and 1 kg in the hand with three sets of 20 repetitions.
Arc of motion phase
The aim this phase is to gain control in 0° to 45° of abduction in the coronal plane at the same time as maintaining scapula control. The patient typically performs the scapula setting action against a SR band as a small movement prior to executing most exercise drills and through most stages of the program. Patients with MDI can have problems controlling a full arc of motion (e.g. ER to end range);11 therefore, exercises can be progressed from small arcs in the middle of range to larger arcs of motion as the patient gains control.
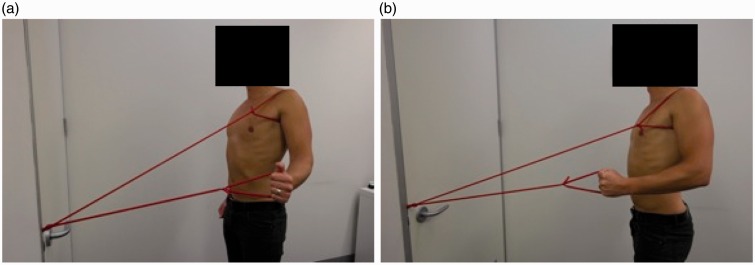
ER, internal rotation (IR) and extension control
These drills are utilized primarily for scapula control with added motion; however, strengthening of rotator cuff and scapula muscles also occurs. ER drills are commenced in standing at 0° with a TheraBand™ (Figure 3a). If the patient has difficulty performing the ER drill, extension is utilized until more control is achieved (Figure 3b). Extension drills are usually performed to neutral only because extension past the side of the body can cause excessive anterior tilt of the scapula. IR often commences once ER control is established (×20 repetitions ER with red TheraBand™) because IR can result in increased anterior tilt of the scapula and increased pectoralis dominance41 if commenced too early.
Figure 3.
(a) External rotation. (b) Both figures show the scapula resistance band for upward rotation and posterior tilt.
ER strengthening
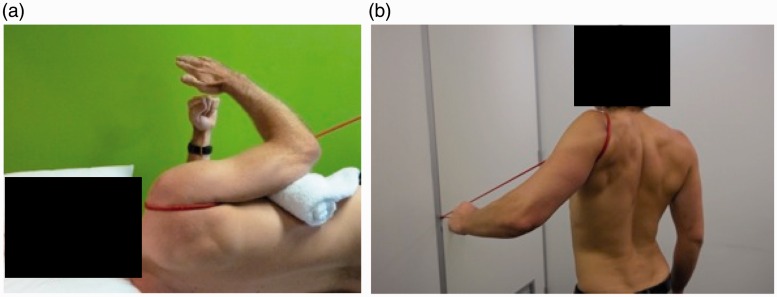
This drill is performed in a side-lying position and is utilized for supraspinatus and infraspinatus strength deficits, as well as for building posterior glenohumeral muscle bulk (Figure 4a). The majority of patients need to perform this drill off a support from neutral to 45° of ER because lowering the arm past neutral may cause posterior translation of the HH.42
Figure 4.
(a) Side-lying external rotation off a support with a scapula resistance band. (b) Extension row to 45° abduction.
Stage 2: Posterior musculature development
The aim of stage 2 is to develop more posterior musculature to act at a buttress to prevent posterior HH translation.43,44 Scapula drills, ER in standing and side-lying are all progressed by an increase in load. Posterior deltoid drills, performed as a bent over row,41 are usually commenced prior to other deltoid drills because the short lever extension may be easier to control and translation of the HH is limited compared to other deltoid drills. In addition, a standing extension row in 45° of abduction is performed to commence control in a higher range of elevation (Figure 4b).
Conclusions
This paper (Part 1) outlines the first two stages of the six-stage Watson MDI Program, which focuses on assessment, regaining scapula and HH control, and beginning arc of motion control in lower ranges of shoulder elevation. These stages are imperative for the MDI patient to master to gain sufficient strength and control to progress to later stages. Part 2 will outline stages 3 to 6, which involve progression of exercises into higher ranges of motion and functional and sports-specific drills. Part 2 will also include further explanation of exercise parameters, including dosage, load, progression of exercises and pathological limitations.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: L. Watson has been teaching physiotherapy shoulder courses for over 25 years. This paper outlines a rehabilitation program that is often taught on these courses; therefore publication may strengthen the rehabilitation programme as a course resource. S. Balster, S. Warby, T. Pizzari, and R. Lenssen are casually employed by L.Watson to assist with her shoulder courses. The authors declare that there are no financial interests in any company or institution that might benefit from the publication of the submitted article. There are no competing interests relevant to this publication.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Barden JM, Balyk R, Raso VJ, Moreau M, Bagnall K. Atypical shoulder muscle activation in multidirectional instability. Clin Neurophysiol 2005; 116: 1846–57. [DOI] [PubMed] [Google Scholar]
- 2.Bahu MJ, Trentacosta N, Vorys GC, Covey AS, Ahmad CS. Multidirectional instability: evaluation and treatment options. Clin Sports Med 2008; 27: 671–89. [DOI] [PubMed] [Google Scholar]
- 3.Neer CS, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. A preliminary report. J Bone Joint Surg Am 1980; 62: 897–908. [PubMed] [Google Scholar]
- 4.Pollock RG, Owens JM, Flatow EL, Bigliani LU. Operative results of the inferior capsular shift procedure for multidirectional instability of the shoulder. J Bone Joint Surg 2000; 82: 919–28. [DOI] [PubMed] [Google Scholar]
- 5.Yamaguchi K, Flatow EL. Management of multidirectional instability. Clin Sports Med 1995; 14: 885–902. [PubMed] [Google Scholar]
- 6.An YH, Friedman RJ. Multidirectional instability of the glenohumeral joint. Orthop Clin North Am 2000; 31: 275–83. [DOI] [PubMed] [Google Scholar]
- 7.Morris AD, Kemp GJ, Frostick SP. Shoulder electromyography in multidirectional instability. J Shoulder Elbow Surg 2004; 13: 24–9. [DOI] [PubMed] [Google Scholar]
- 8.Illyés Á, Kiss RM. Kinematic and muscle activity characteristics of multidirectional shoulder joint instability during elevation. Knee Surg Sports Traumatol Arthrosc 2006; 14: 673–85. [DOI] [PubMed] [Google Scholar]
- 9.Ogston JB, Ludewig PM. Differences in 3-dimensional shoulder kinematics between persons with multidirectional instability and asymptomatic controls. Am J Sports Med 2007; 35: 1361–70. [DOI] [PubMed] [Google Scholar]
- 10.Basmajian JV, Bazant FJ. Factors preventing downward dislocation of the adducted shoulder joint. J Bone Joint Surg 1959; 41: 1182–6. [PubMed] [Google Scholar]
- 11.Ogston JB, Ludewig PM. Differences in 3-dimensional shoulder kinematics between persons with multidirectional instability and asymptomatic controls. Am J Sports Med 2007; 35: 1361–70. [DOI] [PubMed] [Google Scholar]
- 12.McFarland EG, Kim TK, Park HB, Neira CA, Gutierrez MI. The effect of variation in definition on the diagnosis of multidirectional instability of the shoulder. J Bone Joint Surg Am 2003; 85: 2138–44. [DOI] [PubMed] [Google Scholar]
- 13.Salomonsson B, Sforza G, Revay S, Abbaszadegan H, Jonsson U. Atraumatic shoulder instability. Discussion of classification and results after capsular imbrication. Scand J Med Sci Sports 1998; 8: 398–404. [DOI] [PubMed] [Google Scholar]
- 14.Warner JJP, Micheli LJ, Arslanian LE, Kennedy J, Kennedy R. Patterns of flexibility, laxity, and strength in normal shoulders and shoulders with instability and impingement. Am J Sports Med 1990; 18: 366–75. [DOI] [PubMed] [Google Scholar]
- 15.VandenBerghe G, Hoenecke H, Fronek J. Glenohumeral joint instability: the orthopedic approach. Semin Musculoskelet Radiol 2009; 43: 259–64. [DOI] [PubMed] [Google Scholar]
- 16.Warby SA, Pizzari T, Ford JJ, Hahne AJ, Watson L. The effect of exercise-based management for multidirectional instability of the glenohumeral joint: a systematic review. J Shoulder Elbow Surg 2014; 23: 128–42. [DOI] [PubMed] [Google Scholar]
- 17.Guerrero P, Busconi B, Deangelis N, Powers G. congenital instability of the shoulder joint: assessment and treatment options. J Orthop Sports Phys Ther 2009; 39: 124–34. [DOI] [PubMed] [Google Scholar]
- 18.Burkhead WZ, Rockwood CA. Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am 1992; 74: 890–6. [PubMed] [Google Scholar]
- 19.Inui H. Three-dimensional relationship of the glenohumeral joint in the elevated position in shoulders with multidirectional instability. J Shoulder Elbow Surg 2002; 11: 510–5. [DOI] [PubMed] [Google Scholar]
- 20.Watson L. Multidirectional instability of the shoulder: what is it? Does physiotherapy work? What should we be doing? Melbourne: New Moves, Australian Physiotherapy Conference, 2013.
- 21.Watson L. Functional and clinical changes in multidirectional instability of the shoulder after conservative rehabilitation. PhD Thesis: La Trobe University, Bundoora, 2015.
- 22.Ide J, Maeda S, Yamaga M, Morisawa K, Takagi K. Shoulder-strengthening exercise with an orthosis for multidirectional shoulder instability: quantitative evaluation of rotational shoulder strength before and after the exercise program. J Shoulder Elbow Surg 2003; 12: 342–5. [DOI] [PubMed] [Google Scholar]
- 23.Misamore GW, Sallay PI, Didelot W. A longitudinal study of patients with multidirectional instability of the shoulder with seven- to ten-year follow-up. J Shoulder Elbow Surg 2005; 14: 466–70. [DOI] [PubMed] [Google Scholar]
- 24.Tillander B, Lysholm M, Norlin R. Multidirectional hyperlaxity of the shoulder: results of treatment/Hyperlaxite pluridirectionnelle de l ‘ epaule: resultats du traitement. Scand J Med Sci Sports 1998; 8: 421–5. [DOI] [PubMed] [Google Scholar]
- 25.Beasley L, Faryniarz DA, Hannafin JA. Multidirectional instability of the shoulder in the female athlete. Clin Sports Med 2000; 19: 331–49. [DOI] [PubMed] [Google Scholar]
- 26.Watson LA, Pizzari T, Balster S. Thoracic outlet syndrome part 2: conservative management of thoracic outlet. Man Ther 2010; 15: 305–14. [DOI] [PubMed] [Google Scholar]
- 27.Watson L, Pizzari T, Simmonds J, Lewis J. The unstable shoulder. Grieve's modern musculoskeletal physiotherapy, Fourth edition Amserdam: Elsevier, 2015. [Google Scholar]
- 28.Barrett C. The clinical physiotherapy assessment of non-traumatic shoulder instability. Shoulder Elbow 2015; 7: 60–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lewis JS. Rotator cuff tendinopathy/subacromial impingement syndrome: Is it time for a new method of assessment? BJSM 2009; 43: 259–64. [DOI] [PubMed] [Google Scholar]
- 30.Seitz AL, McClure PW, Lynch SS, Ketchum JM, Michener LA. Effects of scapular dyskinesis and scapular assistance test on subacromial space during static arm elevation. J Shoulder Elbow Surg 2012; 21: 631–40. [DOI] [PubMed] [Google Scholar]
- 31.Willmore EG, Smith MJ. Scapular dyskinesia: evolution towards a systems-based approach. Shoulder and Elbow 2016; 8: 61–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lewis A, Kitamura T, Bayley JIL. (ii) The classification of shoulder instability: New light through old windows!. Curr Orthop 2004; 18: 97–108. [Google Scholar]
- 33.Jaggi A, Lambert S. Rehabilitation for shoulder instability. BJSM 2010; 44: 333–40. [DOI] [PubMed] [Google Scholar]
- 34.Farber AJ, Castillo R, Clough M, Bahk M, McFarland EG. Clinical assessment of three common tests for traumatic anterior shoulder instability. J Bone Joint Surg 2006; 88: 1467–74. [DOI] [PubMed] [Google Scholar]
- 35.Lo IKY, Nonweiler B, Woolfrey M, Litchfield R, Kirkley A. An evaluation of the apprehension, relocation, and surprise tests for anterior shoulder instability. Am J Sports Med 2004; 32: 301–7. [DOI] [PubMed] [Google Scholar]
- 36.Magarey ME, Jones MA. Dynamic evaluation and early management of altered motor control around the shoulder complex. Manual Ther 2003; 8: 195–206. [DOI] [PubMed] [Google Scholar]
- 37.Pizzari T, Wickham J, Balster S, Ganderton C, Watson L. Modifying a shrug exercise can facilitate the upward rotator muscles of the scapula. Clin Biomech 2014; 29: 201–5. [DOI] [PubMed] [Google Scholar]
- 38.Adkins DL, Boychuk J, Remple MS, Kleim JA. Motor training induces experience-specific patterns of plasticity across motor cortex and spinal cord. J Appl Physiol 2006; 101: 1776–82. [DOI] [PubMed] [Google Scholar]
- 39.Boudreau SA, Farina D, Falla D. The role of motor learning and neuroplasticity in designing rehabilitation approaches for musculoskeletal pain disorders. Manual Therapy 2010; 15: 410–4. [DOI] [PubMed] [Google Scholar]
- 40.Ganderton C. A novel way to train subscapularis: 17–20 October 2013. Melbourne: New Moves Australian Physiotherapy Association, 2013.
- 41.Kronberg M, Nemeth G, Brostrom LA. Muscle activity and coordination in the normal shoulder: an electromyographic study. Clin Orthops Rel Res 1990; 257: 76–85. [PubMed] [Google Scholar]
- 42.Karduna AR, Williams GR, Iannotti JP, Williams JL. Kinematics of the glenohumeral joint: influences of muscle forces, ligamentous constraints, and articular geometry. J Orthop Res 1996; 14: 986–93. [DOI] [PubMed]
- 43.Wattanaprakornkul D, Halaki M, Cathers I, Ginn KA. Direction-specific recruitment of rotator cuff muscles during bench press and row. J Electromyogr Kinesiol 2011; 21: 1041–9. [DOI] [PubMed] [Google Scholar]
- 44.Day A, Taylor NF, Green RA. The stabilizing role of the rotator cuff at the shoulder – responses to external perturbations. Clin Biomech 2012; 27: 551–6. [DOI] [PubMed] [Google Scholar]