Abstract
Introduction
The evidence is mixed on the HIV knowledge, attitude, and practices of youth in Iran. The aim of the current study was to assess knowledge, attitudes, and practices of Iranian youth towards HIV through a national survey.
Materials and Methods
Through a cross-sectional study with multistage cluster sampling, we administered a pilot-tested standard questionnaire to assess the levels of HIV knowledge, attitudes and practices of individuals aged 15–29 years old. Participants were recruited from 13 provinces in Iran and consisted of 2456 men and 2412 women.
Results
Only 37.3% of the participants had a high knowledge score. Most participants knew the main routes of HIV transmission; however, misconceptions existed about the transmission of HIV through mosquito bites across all age groups (31.7% correct response). Positive levels of attitude wereobserved among 20.7% of the participants. Most participants believed that people living with HIV (PLHIV) should be supported (88.3%) while only 46.3% were ready to share a table with them. Among those aged 19–29 years old, the main source of HIV information was mass media (69.1%), only 13.1% had ever tested for HIV, around 20.8% had ever had extramarital sex (31.7% male vs. 9.6% female),1.8% ever injected drugs (2.9% male vs. and 0.7% female). Among sexually active subjects in this age group, only 21.8% (26.1% male vs. 7.1% female) were consistent condom users.
Conclusions
The findings showed that Iranian youth and young adults have relatively insufficient overall knowledge and negative attitudes about HIV and PLHIV. Novel strategies involving schools and youth’s networks could be employed to deliver a culturally sensitive sexual health program.
Introduction
While the Middle East and North Africa (MENA) region has the lowest number of people living with HIV (PLHIV), the epidemic is expanding at a rapidly increasing rate. In the case of Iran, the estimated prevalence in the general population remains low (i.e., 0.14%), and the concentrated HIV epidemic continues to be mainly driven by injection drug use with a prevalence of 13.8% among people who inject drugs (PWID) [1, 2]. Nevertheless, the modes of transmission for HIV in Iran are changing, and rates of infection through unsafe sexual practices are increasing [2, 3].
Youth are at an increased risk of HIV and account for about half of the new HIV infections in many nations [4, 5]. Being an important period for social development, the adolescent and young adulthood stages are critical for promoting healthy attitudes and behaviors to protect young people from HIV. Their elevated risk of HIV infection has been attributed to their lack of knowledge and engagement in risky sexual and injection behaviors; calling for targeted educational interventions in improving their HIV knowledge and decreasing their risky behaviors [6]. Increasing HIV knowledge has been suggested as an effective HIV preventive behavioral intervention across different contexts. Elevating HIV knowledge creates motivation for risk reduction and has been associated with increased safe sex practices and HIV testing and treatment uptake [7].
The evidence is mixed on the HIV knowledge, attitude, and practice (KAP) of Iranian general population. A systematic review of HIV KAP studies across different sub-populations in 2011, reports relatively high scores of knowledge and attitude among various populations [8]. However, most studies in that review were heterogeneous and came from studies with small sample sizes with limited generalizability to the general Iranian population. Indeed, most previous HIV KAP studies among Iranian youth aged 15–29 that indicate a high level of knowledge and positive attitude towards HIV, are mainly limited to high school [9–12] and medical students [13, 14] in certain provinces. On the other hand, a considerable number of studies on HIV KAP among some demographics of the general and young population, suggest fairly low scores [15–18]. Therefore, given that data on youth’s KAP towards HIV play an important role indestigmatizing HIV and reducing their risky behaviors that can endure into adulthood [19] and the controversial estimates across different studies, it is critical to inform health policy makers and HIV prevention programs with reliable estimates. Therefore, through a population-based large national survey, this study tries to examine Iranian youth’s KAP towards HIV. Findings of this study have important implications for future HIV preventive efforts and policies targeting Iranian youth.
Materials and Methods
Study population
This cross-sectional survey was conducted in 13 (out of 31) provinces in Iran between January and March 2013. In a multistage sampling scheme, 4950 young men and women aged 15–29 years old were recruited proportionate to population size of provinces, meaning that larger provinces had larger samples.
Sampling and data collection
Based on the Statistical Center of Iran’s provincial literacy rates [20], all 31 provinces were categorized into three strata of literacy level: low, moderate, and high. Four provinces from low literacy level, three provinces from the moderate level, and six provinces from the high literacy level were selected. Within each stratum, provinces were considered as clusters. The province of Tehran was treated as three clusters, due to its large population, and other provinces were considered as a single cluster. Therefore, considering the geographic distribution of the provinces, a total of 13 provinces (15 clusters) were purposefully selected for data collection. Assuming that 65% of the general population had a good level of HIV knowledge [8], the power of 80%, and a design effect of 5 (due to the convenient nature of the sample), and a precision level of 0.03, a sample size of 4855 was calculated. Allowing for a non-response rate of 10% (4855/(1–0.10) = 5395) andinformed by expert opinions within Ministry of Health, the calculated sample size was adjusted to 4950.
In each cluster, 330 participants were selected. Based on the population distributions reported in the 2011 census [20], 70% of the participants were recruited from the capital and 30% from the non-capital cities within province. Furthermore, within each city, 70% and 30% of the participants were selected from the urban and rural regions, respectively. Urban regions were divided into five areas (i.e., north, east, west, south, and central) and in each area, two public places were randomly chosen. Rural areas were divided into three strata based on development indicators, and one village was randomly selected from each stratum. Using quota sampling, trained interviewers selected participants from different crowded streets and public places at differenttimes of the day. This was guided by our previous research that suggested people are more likely to disclose sensitive information (e.g., sexual health-related topics) in street-based surveys compared to household- or telephone-based surveys [21].
Survey instrument
The questionnaire was developed through a review of the HIV/AIDS literature [22, 23] and focus group discussions with HIV experts and key informants at the Ministry of Health. The questionnaire consisted of 14 questions/statements on knowledge of HIV modes of transmission, 10 questions on knowledge of HIV diagnosis, prevention, and treatment, as well as 12 questions/statements on attitudes towards HIV/AIDS. We also asked participates about high-risk sexual and drug use behaviors and their sources of HIV/AIDS knowledge. The last section of the questionnaire collected data on participants’ socio-demographic background.
The questionnaire was pilot-tested with 150 participants in three provinces across different strata to ensure clarity, relevance, and accessibility. The content validity was assessed by expert opinion, and the internal reliability was assessed by measuring the Cronbach alpha coefficient; 0.781 for knowledge of HIV modes of transmission, 0.751 for knowledge of HIV diagnosis, prevention, and treatment, and 0.867 for attitudes towards HIV/AIDS. Knowledge questions were scored by “yes”, “no”, and “don’t know”. Overall knowledge was determined by aggregating correct answers from all questions (0–24 for questions on HIV/AIDS knowledge). Based on previous research in this field [6], three levels including (I) low (≤12), (II) medium (13–18), and (III) high (19–24) were specified to assess participants’HIV/AIDS knowledge. Attitudes statements were scored by “agreed”, “disagreed”, and “no idea”. Overall attitudes were determined by aggregating all positive responses ranging from 0 to 12. Levels of (I) negative (0–6 positive responses), (II) neutral (7–9 positive responses) and (III) positive (10–12 positive responses) were quantified.
Statistical analysis
Data were entered via double data entry into Stata v.11 software (StataCorp; College Station, Texas, USA), cleaned, and checked for errors before coding. As participants were recruited from different regions, clustering effects were adjusted using Stata survey package. Data were presented as relative frequencies and 95% confidence intervals (CI) for categorical variables and means with 95% CI for quantitative variables. Participants’ knowledge, attitude, and behaviors in different age groups were compared using chi-square tests. All P-values were two-sided and values less than 5% were considered as statistically significant.
Ethical considerations
Verbal informed consent forms were obtained from all eligible subjects. Given the sensitivity of the topic and the street-based nature of the sample, acquiring written informed consent was not feasible. However, the interviewers explained the informed consent form to the participants and signed the data collection forms to confirm that they had obtained verbal informed consent for all participants. Participants were also briefed about the objectives of the survey and the anonymous nature of data. For minor participants, verbal informed consent was obtained from their caretaker. The ethics committee of the Kerman University of Medical Sciences approved the study protocol and waived the need for written informed consent (Reference Number: K/93/205).
Results
Demographic information
A total of 4950 (2456 men and 2412 women) individuals were approached, out of which 4868 participants completed the survey. The mean (standard deviation (SD)) age was 21.8 (5.6) years; 33.4% (n = 1622) were 15–18 years old, 35.6% (n = 1733) were 19–24 years old, and 31% (n = 1507) were 25–29 years old. Most participants were single (70.7%), had some levels of university educations (58.4%), and around 7.3% reported to be unemployed (Table 1).
Table 1. Socio-demographic characteristics of the study population (N = 4868).
| Variable | n (%) |
|---|---|
| Age | |
| 15–18 | 1622 (33.4) |
| 19–24 | 1733 (35.6) |
| 25–29 | 1507 (31.0) |
| Mean (±SD)* | 21.8 (±5.6) |
| Sex | |
| Male | 2456 (50.5) |
| Female | 2412 (49.6) |
| Marital status | |
| Single | 3407 (70.7) |
| Married | 1350 (28.0) |
| Widowed/Divorced | 63 (1.3) |
| Education | |
| Primary or less | 1573 (32.5) |
| Secondary | 440 (9.1) |
| University student or graduate | 2824 (58.4) |
| Employment Status | |
| Pupil | 1356 (28.0) |
| University student | 838 (17.3) |
| Self-employed | 744 (15.4) |
| Housekeeper | 640 (13.2) |
| Government employee | 371 (7.7) |
| Unemployed | 355 (7.3) |
| Laborer | 332 (6.9) |
| Other | 204 (4.2) |
*SD: Standard Deviation.
HIV/AIDS knowledge
HIV knowledge was assessed in two parts and participants’ responses are presented in Table 2.
Table 2. Knowledge of HIV/AIDS transmission and prevention (N = 4868).
| Statements (correct response) | 15–18 years | 19–24 years | 25–29 years | Total | P-value |
|---|---|---|---|---|---|
| Knowledge of modes of transmission* | |||||
| Sharing food and water utensils with PLHIVa | 1028 (63.8) | 1212 (70.5) | 1141 (76.4) | 3381 (70.1) | <0.001 |
| HIV-infected pregnant woman to her baby (i.e., pregnancy)b | 1246 (77.0) | 1365 (79.6) | 1233 (83.1) | 3844 (79.8) | 0.006 |
| HIV-infected pregnant woman to her baby (i.e., breastfeeding)b | 884 (55.0) | 876 (51.8) | 694 (47.4) | 2454 (51.5) | 0.014 |
| Using the personal belongings and toiletries of PLHIVa | 1108 (69.0) | 1251 (73.5) | 1123 (76.6) | 3482 (72.9) | 0.005 |
| Using the haircut kit of PLHIVa | 1208 (75.1) | 1437 (84.2) | 1297 (88.4) | 3942 (82.4) | <0.001 |
| Piercing with HIV-infected equipmentb | 1277 (79.1) | 1454 (85.0) | 1328 (90.3) | 4059 (84.6) | <0.001 |
| Using dental instruments used for PLHIVb | 1119 (69.9) | 1314 (77.1) | 1253 (85.1) | 3686 (77.1) | <0.001 |
| Using public bathroomsa | 974 (60.8) | 1137 (66.4) | 1046 (70.7) | 3157 (65.9) | <0.001 |
| Using unsterile equipment of tattoo and bloodlettingb | 1242 (78.3) | 1417 (83.8) | 1307 (88.6) | 3966 (83.4) | <0.001 |
| Mosquito/insect bitea | 542 (33.9) | 531 (31.2) | 442 (29.9) | 1515 (31.7) | 0.121 |
| Kissing and/or hugging PLHIVa | 1035 (64.5) | 1226 (71.9) | 1106 (74.7) | 3367 (70.3) | <0.001 |
| Sharing injection needles/syringes with PLHIVb | 1377 (85.4) | 1515 (88.3) | 1359 (91.1) | 4251 (88.2) | 0.003 |
| Contacting sneeze, cough or saliva of PLHIVa | 764 (47.5) | 926 (54.1) | 854 (57.5) | 2544 (52.9) | <0.001 |
| Unprotected sex (i.e., without condom) with PLHIVb | 1334 (82.5) | 1545 (89.4) | 1380 (91.9) | 4259 (87.9) | <0.001 |
| Knowledge of HIV prevention, diagnosis, and treatment | |||||
| One can identify PLHIV, by their physical appearancea | 1167 (72.0) | 1396 (80.7) | 1249 (83.2) | 3812 (78.6) | <0.001 |
| Treatment can reduce the chance of HIV transmissionb | 585 (36.4) | 589 (34.3) | 526 (35.3) | 1700 (35.3) | 0.611 |
| Early diagnosis/treatment increases PLHIV’s life expectancyb | 972 (60.6) | 1168 (68.0) | 1128 (75.7) | 3268 (67.9) | <0.001 |
| Blood testing is the only definite diagnosis of HIV infectionb | 1102 (68.4) | 1262 (73.2) | 1185 (79.4) | 3549 (73.5) | <0.001 |
| There exists a cure for AIDSa | 1104 (68.6) | 1185 (69.2) | 1107 (74.4) | 3396 (70.6) | 0.010 |
| Using condom reduces the chance of HIV transmissionb | 1038 (64.4) | 1216 (71.0) | 1167 (78.2) | 3421 (71.0) | <0.001 |
| PLHIV can have a normal life by following a healthy diet and life style, and taking their treatmentsb | 753 (46.8) | 947 (55.2) | 955 (64.1) | 2655 (55.2) | <0.001 |
| There exists a vaccine that prevents AIDSa | 777 (48.4) | 929 (54.0) | 941 (63.1) | 2647 (55.0) | <0.001 |
| Having multiple sex partners increases the chance of HIV infectionb | 1118 (69.2) | 1290 (75.0) | 1191 (79.3) | 3599 (74.4) | <0.001 |
| Presence of an STD (e.g., genital ulcers) increases the chance of HIV infectionb | 1016 (62.8) | 1229 (71.3) | 1142 (75.9) | 3387 (69.9) | <0.001 |
*PLHIV: people living with HIV; STD: sexually transmitted diseases; Data are n (%)
aFor these questions, “No” is the correct answer
bFor these questions, “Yes” is the correct answer.
Part I: Knowledge of HIV modes of transmission
Participants aged 25–29 years were significantly more knowledgeable about HIV modes of transmission compared to other age groups. Most participants knew the main routes of HIV transmission and could correctly identify the risk of piercing (84.6%) and tattoo (83.4%) with HIV-infected equipment, sharing injection needles/syringes (88.2%), and unprotected sex with PLHIV (87.9%) in transmitting HIV. However, only around half of the participants knew that HIV can be transmitted through breastfeeding (51.5%), or that it cannot be spread through the sneeze, cough or saliva of PLHIV (52.9%). Moreover, misconceptions existed about the transmission of HIV through mosquito/insect bites across all age groups (31.7% correct response).
Part II: Knowledge of HIV prevention, diagnosis, and treatment
Most participants knew that PLHIV cannot be identified by their appearance (78.6%), and HIV testing is the only diagnostic measure (73.5%). Around 70% knew that condom use reduces the chance of HIV transmission. Most participants knew that having multiple sexual partners and pre-existence of sexually transmitted diseases (STD) could increase the chance of HIV infection (74.4% and 69.9%, respectively). Participants’ knowledge about HIV treatment was relatively low, and 55.0% believed that an HIV vaccine exists. More than one-third (35.3%) of the participants knew that antiretroviral therapy could reduce the chance of HIV transmission. Around two-third (67.9%) of them knew that early diagnosis and treatment increases the life expectancy of PLHIV (Table 2).
Attitudes towards HIV/AIDS
Overall, only 38.4% declared tolerance for working or studying with PLHIV. More than half of the participants rejected the misconceptions of viewing HIV as a fair punishment for the sins of the past (57.0%) or quarantining PLHIV as the best HIV preventative intervention (61.8%). Most participants believed that PLHIV should be supported and receive treatments (88.3%), and 47.7% revoked feelings of disgust when thinking about kissing or hugging PLHIV. Around two-third (61.7%) of the participants declared that AIDS is not only exclusive to high-risk populations such as PWID or female sex workers, and 51.4% would not break up their contacts with PLHIV. The poorest attitudes were observed towards sharing a table with PLHIV (46.3% positive attitudes) and feelings of despair in the case of testing positive for HIV (40.1% positive attitudes) (Table 3).
Table 3. Attitudes towards people living with HIV (n = 4868).
| Statements (response for positive attitude)* | 15–18 years | 19–24 years | 25–29 years | Total | P-value |
|---|---|---|---|---|---|
| Attitude towards PLHIV | |||||
| I can work/study with an HIV-infected colleague/classmateb | 550 (34.0) | 712 (41.2) | 603 (40.1) | 1865 (38.4) | 0.006 |
| HIV is not a punishment for the sins and immoralities of the pasta | 820 (50.7) | 1030 (60.0) | 904 (60.4) | 2754 (57.0) | 0.001 |
| Quarantine of PLHIV is not the best way to prevent HIVa | 909 (56.3) | 1142 (66.4) | 934 (62.4) | 2985 (61.8) | <0.001 |
| We should not avoid/stay away from a family with an HIV-infected memberb | 1013 (62.6) | 1194 (69.4) | 1012 (67.8) | 3219 (66.6) | 0.002 |
| PLHIV have to be supported and receive treatmentb | 1393 (86.5) | 1503 (87.2) | 1364 (91.4) | 4260 (88.3) | 0.005 |
| PLHIV do not like to infect othersb | 953 (59.6) | 976 (56.9) | 838 (56.7) | 2767 (57.8) | 0.229 |
| Kissing or hugging people living with HIV is not disgustingb | 719 (44.6) | 856 (50.2) | 717 (48.1) | 2292 (47.7) | 0.005 |
| I prefer not to break my contacts with PLHIVb | 767 (47.6) | 942 (54.9) | 767 (51.5) | 2476 (51.4) | 0.013 |
| PLHIV do not bring disgrace and shame of their familyb | 926 (57.6) | 1104 (64.4) | 896 (60.1) | 2926 (60.8) | 0.002 |
| I can share a table PLHIVb | 673 (42.1) | 847 (49.3) | 705 (47.3) | 2225 (46.3) | 0.007 |
| AIDS is not only the problem of people who inject drugs and people with unrestrained sexual practices (e.g., female sex workers)b | 888 (55.0) | 1046 (60.8) | 1045 (70.0) | 2979 (61.7) | <0.001 |
| If I become infected with HIV, my life is not overb | 665 (41.1) | 682 (39.6) | 594 (39.6) | 1941 (40.1) | 0.667 |
*PLHIV: people living with HIV; Data are n (%)
aFor these questions, “No” shows a positive attitude
bFor these questions, “Yes” shows a positive attitude.
Overall knowledge and attitude
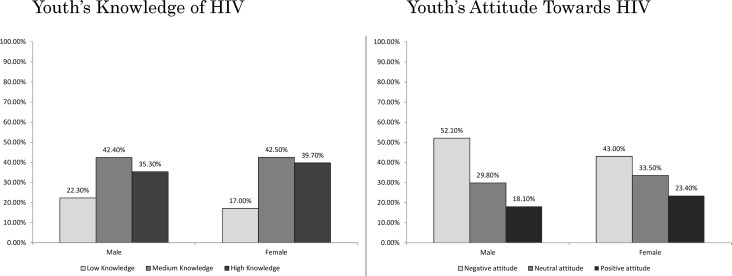
Details of knowledge and attitude scores stratified by age, residence type, and type of cities are presented in Table 4. Moreover, gender differences in knowledge and attitude scores are presented in Fig 1.
Table 4. Overall knowledge and attitude towards HIV/AIDS.
| Knowledge | Attitude | |||||||
|---|---|---|---|---|---|---|---|---|
| Low (12 or less) | Medium (13–18) | High (19 or more) | P-value | Negative (6 or less) | Neutral (7–9) | Positive (10 or more) | P-value | |
| Total* | 958 (19.7) | 2095 (43.0) | 1815 (37.3) | — | 2317 (47.6) | 1542 (31.7) | 1009 (20.7) | — |
| Age groups | <0.001 | 0.005 | ||||||
| 15–18 | 418 (25.8) | 769 (47.4) | 435 (26.8) | 856 (52.8) | 504 (31.1) | 262 (16.2) | ||
| 19–24 | 334 (19.3) | 748 (43.2) | 651 (37.6) | 777 (44.8) | 545 (31.4) | 411 (23.7) | ||
| 25–29 | 205 (13.6) | 577 (38.3) | 725 (48.1) | 682 (45.3) | 490 (32.5) | 335 (22.2) | ||
| Residence type | <0.001 | <0.001 | ||||||
| Rural | 338 (24.6) | 609 (44.4) | 426 (31.0) | 751 (54.7) | 377 (27.5) | 245 (17.8) | ||
| Urban | 620 (17.7) | 1486 (42.5) | 1389 (39.7) | 1566 (44.8) | 1165 (33.3) | 764 (21.9) | ||
| Type of cities | 0.745 | 0.051 | ||||||
| Capital cities | 592 (20.1) | 1259 (42.9) | 1087 (37.0) | 1457 (49.6) | 914 (31.1) | 567 (19.3) | ||
| Non-capital cities | 366 (19.0) | 836 (43.3) | 728 (37.7) | 860 (44.6) | 628 (32.5) | 442 (22.9) | ||
*Data are n (%).
Fig 1. HIV-related Knowledge and attitude scores among young men and women in Iran.
A total of 19.7%, 43.0%, and 37.3% of the participants had low, medium, and high levels of HIV knowledge, respectively. Older (48.1% vs. 26.8%; P-value<0.001), female (39.1% vs. 35.3%; P-value = 0.006), and urban (39.7% vs. 31.0%; P-value<0.001) participants were significantly more knowledgeable about HIV. Moreover, 47.6%, 31.7%, and 20.7% of the participants had negative, neutral, and positive attitudes towards PLHIV, respectively. Attitudes were also significantly better among older (23.7% vs. 16.2%; P-value<0.005), female (23.4% vs. 18.1%; P-value<0.001), and urban (21.9% vs. 17.8%; P-value<0.001) participants.
HIV/AIDS risk behaviors
Data on HIV-related risk behaviors was only collected for subjects aged 19–29 years. Ever drug injection was reported by 1.8% (95% CI: 1.2, 2.7) of participants (2.9% male vs. 0.7% female) and ever needle/syringe sharing was reported by 0.4% (95% CI: 0.2, 1.0) of the participants. Extramarital sex or temporary marriage was reported by 20.8% (95% CI: 16.3, 26.2) of the youth (31.7% male vs. 9.6% female) and mean age at the first extramarital sex among sexually active participants was 19.0 (95% CI: 18.5, 19.5) years. Only 21.8% were consistent condom users (26.1% male vs. 7.1% female) and 27.6% had never or rarely used condoms (24.4% male vs. 38.3% female). While younger participants reported lower condom use practices, there was no significant difference between the two age groups (P-value = 0.177). Main reasons for non-condom use were inaccessibility (38.4%), unnecessity (32.3%), and disinterest (28.8%). Around one-third of the participants (35.4%; 95% CI: 30.1, 41.1) reported condom use in their last sexual encounter (38.2% male vs. 25.9% female). About 40% had ever used alcohol or drugs during or before sex (39.8% male vs. 40.3% female). A total of 86.9% (95% CI: 84.4, 89.1) had never tested for HIV, and only 6.5% (8.1% male vs. 4.9% female) had tested for HIV during the previous year. Media (69.1%), acquaintances (40.9%), and the web (39.9%) were reported as principal sources of obtaining information about HIV (Table 5).
Table 5. HIV/AIDS risky behavior practices in a survey among young people in Iran.
| Variables (number of valid responses) | 19–24 years | 25–29 years | Total | P-valueƗ |
|---|---|---|---|---|
| Ever injected illicit or stimulants drugs (n = 3000) | 1.9 (1.2, 3.0)* | 1.7 (1.0, 2.9) | 1.8 (1.2, 2.7) | 0.721 |
| Male (n = 1491) | 2.9 (1.9, 4.6) | 2.8 (1.6, 5.0) | 2.9 (1.9, 4.3) | 0.895 |
| Female (n = 1504) | 0.9 (0.3, 2.5) | 0.6 (0.2, 2.0) | 0.7 (0.3, 1.8) | 0.536 |
| Ever used shared/unsterile syringes/needles (n = 3240) | 0.5 (0.2, 1.1) | 0.3 (0.1, 1.3) | 0.4 (0.2, 1.0) | 0.495 |
| Male (n = 1628) | 0.8 (0.3, 1.9) | 0.7 (0.2, 2.6) | 0.7 (0.3, 1.9) | 0.658 |
| Female (n = 1612) | 0.1 (0.0, 1.0) | 0.0 | 0.1 (0.0, 0.5) | 0.371 |
| Extramarital sex or temporary marriage (n = 3040) | 19.8 (15.3,25.1) | 22.0 (16.7,28.3) | 20.8 (16.3,26.2) | 0.214 |
| Male (n = 1537) | 30.0 (23.2,37.8) | 33.5 (25.0,43.2) | 31.7 (24.7,39.6) | 0.291 |
| Female (n = 1503) | 9.5 (6.6,13.7) | 9.8 (6.4,14.7) | 9.6 (6.7,13.7) | 0.872 |
| Mean age at the first extramarital sex (n = 413) | 18.4 (17.8, 18.9) | 20.4 (19.6, 21.1) | 19.3 (18.8, 19.8) | <0.001 |
| Male (n = 303) | 18.0 (17.3, 18.7) | 20.2 (19.5, 20.9) | 19.0 (18.5, 19.5) | <0.001 |
| Female (n = 109) | 19.5 (18.6, 20.5) | 20.9 (19.8, 22.0) | 20.2 (19.6, 20.8) | 0.022 |
| Using condom during sex (n = 616) | 0.177 | |||
| Always | 19.0 (14.1,25.1) | 24.5 (19.5,30.4) | 21.8 (17.4,26.8) | |
| Often | 14.2 (9.3,21.1) | 16.7 (11.2,24.2) | 15.4 (11.3,20.8) | |
| Sometimes | 35.8 (29.5,42.6) | 34.6 (27.9,42.1) | 35.2 (29.9,41.0) | |
| Rarely/Never | 31.0 (26.6,35.7) | 24.2 (20.1,28.8) | 27.6 (24.2,31.3) | |
| Male (n = 475) | 0.351 | |||
| Always | 23.0 (16.8,30.6) | 29.2 (23.1,36.1) | 26.1 (20.8,32.2) | |
| Often | 16.2 (10.7,23.7) | 15.8 (10.2,23.8) | 16.0 (11.3,22.2) | |
| Sometimes | 34.0 (26.9,42.0) | 32.9 (25.5,41.3) | 33.5 (26.9,40.7) | |
| Rarely/Never | 26.8 (21.8,32.5) | 22.1 (17.4,27.6) | 24.4 (20.9,28.3) | |
| Female (n = 141) | ||||
| Always | 6.7 (2.0,20.3) | 7.6 (3.5,15.8) | 7.1 (3.4,14.4) | 0.189 |
| Often | 8.0 (3.5,17.1) | 19.7 (9.6,36.1) | 13.5 (7.4,23.3) | |
| Sometimes | 41.3 (28.4,55.6) | 40.9 (27.2,56.2) | 41.1 (30.6,52.6) | |
| Rarely/Never | 44.0 (32.9,55.8) | 31.8 (23.8,41.1) | 38.3 (31.1,46.0) | |
| Reasons for inconsistent condom use (n = 632) | ||||
| It was not accessible | 40.6 (35.6,45.8) | 36.3 (30.6,42.5) | 38.4 (33.8,43.3) | 0.134 |
| It is too expensive | 10.1 (6.1,16.0) | 4.1 (2.2,7.6) | 7.1 (4.3,11.6) | <0.001 |
| My partner objected | 20.8 (17.4,24.6) | 9.2 (4.8,16.9) | 15.0 (10.9,20.4) | 0.024 |
| I do not like it | 28.3 (21.8,35.9) | 29.3 (23.9,35.4) | 28.8 (23.8,34.4) | 0.773 |
| I used something else | 4.4 (2.9,6.6) | 4.5 (2.6,7.5) | 4.4 (3.3,5.9) | 0.971 |
| I did not think it was necessary | 32.4 (25.4,40.3) | 32.2 (26.4,38.6) | 32.3 (26.7,38.4) | 0.947 |
| Using condom in the last sexual contact (n = 616) | 0.090 | |||
| Yes | 31.8 (25.0,39.5) | 39.0 (33.7,44.5) | 35.4 (30.1,41.1) | |
| No | 59.1 (53.9,64.1) | 48.4 (42.8,54.0) | 53.7 (48.9,58.5) | |
| I do not remember | 9.1 (5.6,14.5) | 12.7 (8.7,18.0) | 10.9 (8.5,13.8) | |
| Male (n = 477) | 0.277 | |||
| Yes | 35.0 (26.9,44.2) | 41.2 (34.4,48.2) | 38.2 (32.5,44.2) | |
| No | 55.6 (49.5,61.4) | 46.5 (39.9,53.2) | 50.9 (45.5,56.3) | |
| I do not remember | 9.4 (5.2,16.4) | 12.3 (8.3,18.0) | 10.9 (8.5,13.8) | |
| Female (n = 139) | 0.321 | |||
| Yes | 21.6 (14.1,31.7) | 30.8 (19.0,45.8) | 25.9 (19.8,33.1) | |
| No | 70.3 (57.6,80.5) | 55.4 (38.8,70.8) | 63.3 (51.3,73.8) | |
| I do not remember | 8.1 (1.9,28.3) | 13.8 (6.0,28.7) | 10.8 (4.9,22.3) | |
| Ever used alcohol or drugs during/before sex (n = 614) | 0.620 | |||
| Yes | 40.8 (35.6,46.3) | 39.0 (31.7,46.8) | 39.9 (34.6,45.4) | |
| No | 53.9 (47.9,59.8) | 54.5 (47.3,61.6) | 54.2 (48.6,59.7) | |
| I do not remember | 5.2 (2.8,9.4) | 6.5 (4.1,10.1) | 5.9 (3.7,9.3) | |
| Male (n = 475) | ||||
| Yes | 42.2 (35.2,49.6) | 37.4 (29.6,46.0) | 39.8 (33.4,46.5) | 0.210 |
| No | 53.0 (45.7,60.2) | 55.6 (48.7,62.2) | 54.3 (48.2,60.3) | |
| I do not remember | 4.7 (2.7,8.2) | 7.0 (3.8,12.4) | 5.9 (3.5,9.6) | |
| Female (n = 139) | ||||
| Yes | 36.5 (22.3,53.5) | 44.6 (28.3,62.1) | 40.3 (28.1,53.9) | 0.712 |
| No | 56.8 (41.5,70.9) | 50.8 (32.3,69.0) | 54.0 (40.4,67.0) | |
| I do not remember | 6.8 (2.3,18.2) | 4.6 (0.9,19.9) | 5.8 (2.5,12.9) | |
| HIV testing (n = 3074) | <0.001 | |||
| Never tested | 89.9 (87.7,91.7) | 83.4 (79.4,86.8) | 86.9 (84.4,89.1) | |
| Tested in the past 12 months | 5.2 (4.1,6.5) | 8.0 (6.4,9.9) | 6.5 (5.5,7.6) | |
| Tested before the past 12 month | 4.9 (3.5,6.8) | 8.6 (6.2,11.8) | 6.6 (5.0,8.7) | |
| Male (n = 1549) | ||||
| Never tested | 88.0 (84.8,90.6) | 80.1 (74.6,84.6) | 84.2 (81.0,87.1) | 0.003 |
| Tested in the past 12 months | 6.1 (4.3,8.6) | 10.2 (7.3,14.1) | 8.1 (6.2,10.5) | |
| Tested before the past 12 month | 5.9 (4.4,7.8) | 9.7 (6.8,13.6) | 7.7 (6.0,9.9) | |
| Female (n = 1525) | ||||
| Never tested | 91.8 (89.7,93.4) | 87.0 (81.9,90.8) | 89.6 (86.5,92.0) | 0.008 |
| Tested in the past 12 months | 4.2 (3.3,5.4) | 5.6 (4.0,7.8) | 4.9 (3.9,6.1) | |
| Tested before the past 12 month | 4.0 (2.5,6.4) | 7.4 (4.8,11.4) | 5.6 (3.8,8.2) | |
| Source of obtaining information about HIV (n = 3240) | ||||
| Family, friends and acquaintances | 40.8 (36.5,45.2) | 41.1 (36.2,46.1) | 40.9 (36.6,45.4) | 0.831 |
| Media (e.g., TV, radio, newspaper) | 65.8 (61.4,70.1) | 72.9 (67.0,78.2) | 69.1 (64.6,73.4) | 0.012 |
| Internet | 42.2 (37.9,46.6) | 37.4 (33.3,41.6) | 39.9 (36.3,43.7) | 0.037 |
| Health centers and hospitals | 31.3 (27.6,35.3) | 36.5 (32.8,40.4) | 33.7 (30.6,37.0) | 0.018 |
| Schools or universities | 40.6 (37.1,44.3) | 29.5 (26.5,32.6) | 35.4 (32.5,38.5) | <0.001 |
| Do not know much about HIV | 11.0 (8.8,13.7) | 9.8 (7.5,12.8) | 10.5 (8.6,12.6) | 0.436 |
| Other | 1.6 (0.9,2.7) | 1.7 (1.1,2.6) | 1.6 (1.1,2.3) | 0.843 |
*Data are % (95% CI)
Ɨ P-values were obtained from Chi-Square test.
Discussion
This study revealed that a considerable subgroup of Iranian youth know little about HIV. While most identified the basic routes of transmission, approximately half of the participants did not know that HIV cannot be transmitted through sneezes of PLHIV, and a large proportion of them falsely indicated that mosquito bites can transmit the HIV. Moreover, youth’s knowledge of HIV treatment was similarly low as most did not know that HIV treatment reduces the chances of transmission and around 55% believed that an HIV vaccine exists. Our findings indicate a lower knowledge score compared to most previous studies in Iran. A systematic review on the knowledge and attitude of Iranians (2011) towards HIV, reported a mean knowledge score of 67.5, and attitude score of 68 (on a scale of 100) [8]. This high level of knowledge and positive attitude, in comparison with our study, could be due to their large sample of high school and medical students, university professors, and nurses that may have a higher level of HIV knowledge and a better attitude towards PLHIV. Other population-based studies that have recruited young participants and reported higher HIV knowledge and attitude scores are also limited to western provinces [24], and convenience volunteer samples [25].
HIV knowledge and attitudes scores were higher in urban settings. This could be explained by the uneven distribution of HIV educational campaigns across different regions with urban areas receiving more attention. It could also be related to the overall higher knowledge level of urban residents. We also observed that women were significantly more knowledgeable that men and had more positive attitudes towards HIV and PLHIV. Such findings have been reported in several studies elsewhere [26–29] and been attributed to women’s higher health consciousness and levels of empathy compared to men. As expected, knowledge and positive attitudes about HIV increased with age which could be attributed to older people’s larger interest in seeking sexual health information or higher exposure to sexual health education (e.g., premarital mandatory trainings on sexual health and HIV).
Participants’ limited knowledge about HIV could be attributed to their lack of access to sexual health information. Media was reported as our participants’ main source of seeking HIV-related sexual health information. However, similar to other conservative contexts where open discussions of sexually-related topics are challenging and sensitive [6], Iranian media has not taken a proactive role in educating the public about HIV and other sexually transmitted infections (STI). While a recent increase in the number of HIV-related documentaries (e.g., Shock, Red Ribbon) is promising and the media has started conversations on destigmatizing HIV-related topics, there is much room for improvement. Similar to other studies [30], family members were reported as the second most significant source of information on HIV-related topics. Worldwide, youth are often viewed as immature individuals who are not ‘ready’ to make the ‘right’ decisions regarding their sexual lives, and parents are expected to monitor and inform their decision about sexual and reproductive health [31]. However, in the context of Iran and several other conservative settings, parents often try to stick to the socio-cultural norms around sexuality (e.g., abstinence, delaying first sexual experience) and discussions around such topics remain very limited if they ever take place [31, 32]. Moreover, many parents are often not equipped with sufficient knowledge to provide their children with sexual health education in the context of HIV [33]. Additionally, only one-third of youth reported school as a source of information on HIV, which points to youth’s limited exposure to sexual health education in school settings. Indeed, Iranian youth’s primary official exposure to sexual health information including HIV areas, has been either through very limited topics in school curricula, pre-marital mandatory courses, a one-credit undergraduate level course on family planning—which was recently suspended—or the various interventions of the HIV/STI office at the Ministry of Health (MOH).
Unfortunately, youth’s low knowledge of HIV had translated into negative attitudes whereas only one-fifth of the participants had a positive attitude towards PLHIV. Studies in Iran have indicated how insufficient knowledge of HIV transmission and prevention leads to less positive attitudes towards HIV and PLHIV [16]. It seems that while youth were empathetic towards PLHIV, they still preferred to avoid close contact with them. This could be illustrated by participants’ favorable attitudes on the rights of PLHIV to access treatment or disapproval of shunning behaviors towards PLHIV and their families, but not wanting to kiss them or share a table or workspace with them. Such poor attitudes have been reported in similar studies in Iran [16] where out of 4641 high school students, around half disapproved of PLHIV’s presence at schools saying that they would avoid any physical contact with them. Similar negative attitudinal problems have been reported among youth from other Middle Eastern countries such as United Arab Emirates [34], where 85% of university students had a negative attitude towards PLHIV. This could be attributed to the similar conservative atmosphere of these countries regarding HIV education, and also highlights the importance of considering such attitudes in developing future HIV strategic plans.
While poor attitudes towards PLHIV can lead to PLHIV’s experiences of discrimination across various settings, positive attitudes towards PLHIV have been associated with a willingness for HIV testing [35, 36]. This was also evident in our study where poor attitudes towards PLHIV was observed next to a very low ever HIV testing prevalence. While barriers to HIV testing among Iranian youth are complicated and not yet fully understood, low uptakes of HIV testing among them could be attributed to several reasons such as confidentiality concerns, anticipated stigma, low HIV risk perceptions in youth, and clinic locations and hours of operation [37]. Such low HIV testing prevalence is very concerning as frequent HIV testing practices have been associated with a reduced risk of HIV transmission and lower risky behavior profiles among youth [16].
Moreover, despite youth’s knowledge about reduced risk of HIV transmission via safe sex practices, less than one-third of them had used a condom in their last sexual encounter, and only 21.8% were consistent condom users. Moreover, around 30% of the participants perceived consistent condom use as unnecessary. Although condoms are widely accessible in pharmacies with a relatively affordable price, accessibility was reported as the main reason for youth’s inconsistent condom use. While barriers to condom use among Iranian youth are less understood, profound levels of anticipated or enacted stigma associated with obtaining condoms among Iranian youth could create a reluctance in purchasing condoms. Such stigmas could be rooted in the religious and socio-cultural norms around sexual practices of youth—unmarried youth in particular—that do not welcome youth’s engagement in extramarital sexual practices.
Young men were much more likely to use a condom compared to young women. This calls for further gender-sensitive condom promotion interventions and could be due to young women’s lower negotiation skills or self-perceived risk of HIV compared to men [38, 39]. Moreover, around one-fifth of participants reported having extramarital or pre-marital relationships with a significantly higher prevalence among young men. Studies have shown how existing gender inequalities around youth sexuality may lead to different sexual expectations for young men and women. For example, young men may be expected to gain sexual experience by starting sexual relationships at an earlier age or having multiple sexual partners; behaviors that may be celebrated among their peers or fathers [31].
We would like to acknowledge the limitations of this study. Although a large national sample of adults was recruited through a cluster randomized sampling approach, the street-based nature of the sample may introduce bias to our findings and limit its generalizability to some extent. However, our prior research in Iran indicates that in the context of asking culturally sensitive question, more accurate responses are obtained through street-based surveys compared with household-level and telephone-based surveys [21, 40]. Moreover, we used a three-point scale to assess attitudes towards HIV and PLHIV. While five-point scales may reflect a more precise view of the participants, fearing participants’ inability to think in such wider scale, a three-point scale was used. Lastly, social desirability bias could not be ruled out due to the self-reported nature of the data. However, the anonymity of the questionnaires and using experienced interviewers may have encouraged the participants to provide honest responses. Overall, given the scope of the study, we believe our findings have important implications for both research and policy.
Conclusions
Our study re-emphasizes the findings of the previous body of evidence suggesting that despite being a crucial foundation in addressing the epidemic, knowledge of HIV among Iranian youth is insufficient in positively influencing their attitudes and risky sexual practices. We observed a low knowledge of HIV and fairly negative attitudes towards PLHIV among our participants. Given their limited knowledge, youth with risky sexual practices at an early age are being sent off to the society without adequate and accurate knowledge of STI and sexual health. Low levels of condom use and HIV testing among our participants are also concerning and call for targeted gender-sensitive interventions to increase condom use and HIV testing availability and acceptability among young men and women. Schools and universities are of utmost importance in reaching this goal and should be able to take a more prominent and proactive role in educating youth about sexual health and HIV-related risky behaviors. Healthcare providers and teachers, in particular, should be equipped with required training and knowledge on HIV-related topics and should take on an active responsibility in providing quality sexual educations to youth. Future research and intervention on HIV health promotion should focus on the further understanding of how socio-cultural and religious value systems affect youth’s sexual lifestyle and information access. Strategic plans should also prioritize involving the key individuals in youth’s networks (e.g., parents, teachers, and peers) in HIV education programs.
Data Availability
Data are owned by the Ministry of Health and Medical Education. Data will be available upon request from the senior author (Hamid Sharifi; hsharifi@kmu.ac.ir) for researchers who meet the criteria for access to confidential data in the Ministry of Health of Iran.
Funding Statement
The survey was financially supported by the Ministry of Health of Iran in 2013. However, the authors received no funding for this specific paper.
References
- 1.Khajehkazemi R, Osooli M, Sajadi L, Karamouzian M, Sedaghat A, Fahimfar N, et al. HIV prevalence and risk behaviours among people who inject drugs in Iran: the 2010 National Surveillance Survey. Sexually transmitted infections. 2013;89 Suppl 3:iii29–32. Epub 2013/09/17. 10.1136/sextrans-2013-051204 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National AIDS Committee Secretariat. Islamic Republic of Iran AIDS Progress Report. In: office HS, editor. Tehran: Ministry of Health and Medical Education; 2015. [Google Scholar]
- 3.Nasirian M, Doroudi F, Gooya MM, Sedaghat A, Haghdoost AA. Modeling of human immunodeficiency virus modes of transmission in Iran. Journal of research in health sciences. 2012;12(2):81–7. Epub 2012/12/18. . [PubMed] [Google Scholar]
- 4.UNAIDS. The GAP report, 2014.http://www.unaids.org/sites/default/files/en/media/unaids/contentassets/documents/unaidspublication/2014/UNAIDS_Gap_report_en.pdf.
- 5.UNAIDS. All In to #EndAdolescentAIDS, 2015. Available at: http://www.unaids.org/sites/default/files/media_asset/20150217_ALL_IN_brochure.pdf.
- 6.Ganczak M, Barss P, Alfaresi F, Almazrouei S, Muraddad A, Al-Maskari F. Break the silence: HIV/AIDS knowledge, attitudes, and educational needs among Arab university students in United Arab Emirates. The Journal of adolescent health: official publication of the Society for Adolescent Medicine. 2007;40(6):572.e1–8. Epub 2007/05/29. 10.1016/j.jadohealth.2007.01.011 . [DOI] [PubMed] [Google Scholar]
- 7.Tulloch HE, Balfour L, Kowal J, Tasca GA, Angel JB, Garber G, et al. HIV knowledge among Canadian-born and sub-Saharan African-born patients living with HIV. Journal of immigrant and minority health / Center for Minority Public Health. 2012;14(1):132–9. Epub 2011/06/07. 10.1007/s10903-011-9480-7 . [DOI] [PubMed] [Google Scholar]
- 8.Haghdoost AA, Pourkhandani A, Motaghipisheh S, Farhoudi B, Fahimifar N, Sadeghirad B. Knowledge and Attitude concerning HIV/AIDS among Iranian Population: a Systematic Review and Meta-Analysis. Iranian Journal of Epidemiology. 2011;6(4):8–20. [Google Scholar]
- 9.Behjati M, Ayatollahi J. Knowledge of high schools students in Yazd city about AIDS. Iranian Journal of Pediatrics. 2005;15(4):321–6. [Google Scholar]
- 10.Taheri JB, Maleki Z, Baharvand M, Tabatabaei FM. Knowledge and attitude of Tehran high school students in HIV/AIDS, 2005. Journal of Dental School. 2009;26(3):303–12. [Google Scholar]
- 11.Mazloumi MS, Abbasi SM. Knowledge and attitude survey of high school students of Yazd province of Iran about HIV/AIDS. Zahedan Journal of Research in Medical Sciences.2006;8(1):53–63. [Google Scholar]
- 12.Tavoosi A, Zaferani A, Enzevaei A, Tajik P, Ahmadinezhad Z. Knowledge and attitude towards HIV/AIDS among Iranian students. BMC public health. 2004;4(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Askarian M, Honarvar B, Tabatabaee H-R, Assadian O. Knowledge, practice and attitude towards standard isolation precautions in Iranian medical students. Journal of Hospital Infection. 2004;58(4):292–6. 10.1016/j.jhin.2004.07.004 . [DOI] [PubMed] [Google Scholar]
- 14.Askarian M, Assadian O. Infection control practices among dental professionals in Shiraz Dentistry School, Iran. Archives of Iranian medicine. 2009;12(1):48–51.. [PubMed] [Google Scholar]
- 15.Montazeri A. AIDS knowledge and attitudes in Iran: results from a population-based survey in Tehran. Patient education and counseling. 2005;57(2):199–203. Epub 2005/05/25. 10.1016/j.pec.2004.05.014 . [DOI] [PubMed] [Google Scholar]
- 16.Ghabili K, Shoja MM, Kamran P. The Iranian female high school students' attitude towards people with HIV/AIDS: a cross-sectional study. AIDS research and therapy. 2008;5(1):1 10.1186/1742-6405-5-15 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taj SS, Roushan DM. A survey on the knowledge and attitude of Iranian recruits about HIV/AIDS during the training course of their military service conducted in Tehran (2004).Annals of military and health sciences research. 2005;3(2): 565–73. [Google Scholar]
- 18.Sadeghipour Roudsari H, Sherafat Kazemzadeh R, Rezaeie M, Derakhshan M. Reproductive health knowledge, attitudes and practices of Iranian and Afghan men in Tehran province.East Mediterr Health J. 2006;12(6):862–72.. [PubMed] [Google Scholar]
- 19.Gao X, Wu Y, Zhang Y, Zhang N, Tang J, Qiu J, et al. Effectiveness of school-based education on HIV/AIDS knowledge, attitude, and behaviour among secondary school students in Wuhan, China. PLoS one. 2012;7(9):e44881 Epub 2012/09/13. 10.1371/journal.pone.0044881 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Statistical centre of Iran. Selected findings of the 2011 national population and housing census. 2011.
- 21.Nasirian M, Karamouzian M, Kamali K, Nabipour AR, Maghsoodi A, Nikaeen R, et al. Care Seeking Patterns of STIs-Associated Symptoms in Iran: Findings of a Population-Based Survey. International journal of health policy and management. 2015;5(1):5–11. Epub 2015/12/18. 10.15171/ijhpm.2015.146 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Research in nursing & health. 2001;24(6):518–29. Epub 2001/12/18. . [DOI] [PubMed] [Google Scholar]
- 23.USAID. Demographic and Health Surveys Toolkit. 2012. Available at: https://www.k4health.org/toolkits/dhs.
- 24.Tehrani FR, Malek-Afzali H. Knowledge, attitudes and practices concerning HIV/AIDS among Iranian at-risk sub-populations. Eastern Mediterranean health journal. 2008;14(1):143. [PubMed] [Google Scholar]
- 25.Hedayati-Moghaddam M. Knowledge of and attitudes towards HIV/AIDS in Mashhad, Islamic Republic of Iran. East Mediterr Health J. 2008;14(6):1321–32. [PubMed] [Google Scholar]
- 26.Eastwood SV, Hill PC. A gender-focused qualitative study of barriers to accessing tuberculosis treatment in The Gambia, West Africa. The international journal of tuberculosis and lung disease: the official journal of the International Union against Tuberculosis and Lung Disease. 2004;8(1):70–5. Epub 2004/02/21. . [PubMed] [Google Scholar]
- 27.Gustafson PE. Gender differences in risk perception: theoretical and methodological perspectives. Risk analysis. 1998;18(6):805–11. Epub 1999/02/11. . [DOI] [PubMed] [Google Scholar]
- 28.Martin RJ, Chaney BH, Vail-Smith K, Gallucci AR. Hazardous Drinking and Weight-Conscious Drinking Behaviours in a Sample of College Students and College Student Athletes. Substance abuse. 2016:0. Epub 2016/01/29. 10.1080/08897077.2016.1142922 . [DOI] [PubMed] [Google Scholar]
- 29.Ross CE, Bird CE. Sex stratification and health lifestyle: consequences for men's and women's perceived health. Journal of health and social behaviour. 1994;35(2):161–78. Epub 1994/06/01. . [PubMed] [Google Scholar]
- 30.Mosavi SA, Babazadeh R, Najmabadi KM, Shariati M. Assessing Iranian adolescent girls' needs for sexual and reproductive health information. The Journal of adolescent health. 2014;55(1):107–13. Epub 2014/02/25. 10.1016/j.jadohealth.2013.11.029 . [DOI] [PubMed] [Google Scholar]
- 31.Wood K, Aggleton P. Promoting young peoples sexual and reproductive health Stigma discrimination and human rights. Thomas Coram Research Unit; Institute of Education, University of London, 2002. Available at: http://r4d.dfid.gov.uk/PDF/Outputs/HSafeGoodstigma.pdf. [Google Scholar]
- 32.O'Byrne P, Watts J. Include, differentiate and manage: gay male youth, stigma and healthcare utilization. Nursing inquiry. 2014;21(1):20–9. Epub 2012/12/13. 10.1111/nin.12014 . [DOI] [PubMed] [Google Scholar]
- 33.Karamouzian M, Shokoohi M. Sexual and reproductive health education in Iranian schools. The Journal of adolescent health. 2014;55(1):149–50. Epub 2014/05/03. 10.1016/j.jadohealth.2014.04.009 . [DOI] [PubMed] [Google Scholar]
- 34.Haroun D, El Saleh O, Wood L, Mechli R, Al Marzouqi N, Anouti S. Assessing Knowledge of, and Attitudes to, HIV/AIDS among University Students in the United Arab Emirates. Eugenin EA, ed. PLoS One. 2016;11(2):e0149920 10.1371/journal.pone.0149920 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kakoko DC, Lugoe WL, Lie GT. Voluntary testing for HIV among a sample of Tanzanian teachers: a search for socio-demographic and socio-psychological correlates. AIDS care. 2006;18(6):554–60. Epub 2006/07/13. 10.1080/09540120500259779 . [DOI] [PubMed] [Google Scholar]
- 36.Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town, South Africa. Sexually transmitted infections. 2003;79(6):442–7. Epub 2003/12/10. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shoveller J, Johnson J, Rosenberg M, Greaves L, Patrick DM, Oliffe JL, et al. Youth’s experiences with STI testing in four communities in British Columbia, Canada. Sexually Transmitted Infections. 2009;85(5):397–401. 10.1136/sti.2008.035568 [DOI] [PubMed] [Google Scholar]
- 38.Farahani FK, Shah I, Cleland J, Mohammadi MR. Adolescent males and young females in tehran: differing perspectives, behaviours and needs for reproductive health and implications for gender sensitive interventions. Journal of reproduction & infertility. 2012;13(2):101–10. Epub 2012/04/01. . [PMC free article] [PubMed] [Google Scholar]
- 39.Terry PE, Mhloyi M, Masvaure TB, Adlis SA. Gender equity and HIV/AIDS prevention: comparing gender differences in sexual practice and beliefs among Zimbabwe university students. International quarterly of community health education. 2005;24(1):29–43. Epub 2007/08/11. 10.2190/f5vv-jpne-71at-8fuh . [DOI] [PubMed] [Google Scholar]
- 40.Haghdoost AA, Baneshi MR, Eybpoosh S, Khajehkazemi R. Comparison of three interview methods on response pattern to sensitive and non-sensitive questions. Iranian Red Crescent medical journal. 2013;15(6):500–6. Epub 2013/12/19. 10.5812/ircmj.7673 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are owned by the Ministry of Health and Medical Education. Data will be available upon request from the senior author (Hamid Sharifi; hsharifi@kmu.ac.ir) for researchers who meet the criteria for access to confidential data in the Ministry of Health of Iran.