Abstract
Annular pancreas is a developmental anomaly that can be associated with other conditions such as Down syndrome, duodenal atresia, and Hirschsprung disease. A band of pancreatic tissue, in continuity with the pancreatic head, completely or incompletely encircles the descending duodenum, sometimes assuming a “crocodile jaw” configuration. We present the case of an adult who presented with epigastric pain and vomiting and was found to have annular pancreas.
Annular pancreas is an uncommon and infrequently reported anomaly. The malformation was given its descriptive name in 1862 by Ecker (1). The prevalence ranged from 5 to 15 per 100,000 adults in a cadaveric case series and was 1 in 250 on an endoscopic retrograde cholangiopancreatography (ERCP) study (2). Annular pancreas presents differently in neonates and adults. In neonates, it usually causes duodenal obstruction and may be associated with other congenital abnormalities such as Down syndrome. In adults, however, it can present as pancreatitis and associated biliary obstruction. Symptoms can occur when either a complete or incomplete ring of pancreatic tissue encircles the second portion of the duodenum. We report a case of annular pancreas that was diagnosed in an adult based on radiologic tests and was treated surgically. If the condition is not diagnosed quickly, it can lead to severe morbidity and mortality. Contrast-enhanced computed tomography (CT), magnetic resonance imaging (MRI), endoscopic ultrasonography, and laparoscopic ultrasonography are used as advanced imaging techniques even in asymptomatic patients (3).
CASE REPORT
A 42-year-old man presented with severe epigastric pain, vomiting after meals, and significant weight loss. Abdominal ultrasound showed gross dilatation of the stomach and duodenum with suspicion of annular pancreas (Figure 1). Contrast-enhanced CT revealed pancreatic tissue partially encircling the duodenum with gastric outlet obstruction (Figure 2). On axial T1-weighted MRI, partial annular pancreas was seen with a “crocodile jaw” appearance (Figure 3). Based on the imaging findings, partial annular pancreas with gastric outlet obstruction was diagnosed. The patient underwent duodenoduodenostomy with relief of symptoms. At 6-month follow-up, he had no complaints.
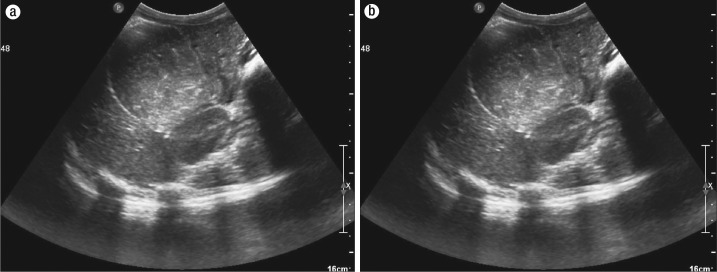
Figure 1.
Axial ultrasound images showing (a) a grossly dilated stomach and (b) at the inferior level, pancreatic tissue encircling the duodenum.
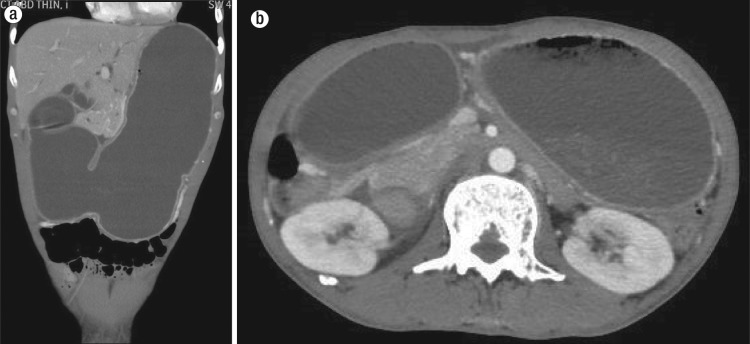
Figure 2.
Contrast-enhanced CT images with 4 mm slice thickness. (a) A coronal multiplanar reconstruction showing duodenal obstruction as a result of annular pancreas. (b) An axial image showing the dilated stomach and pancreatic tissue extending anteromedially to the second part of the duodenum.
Figure 3.
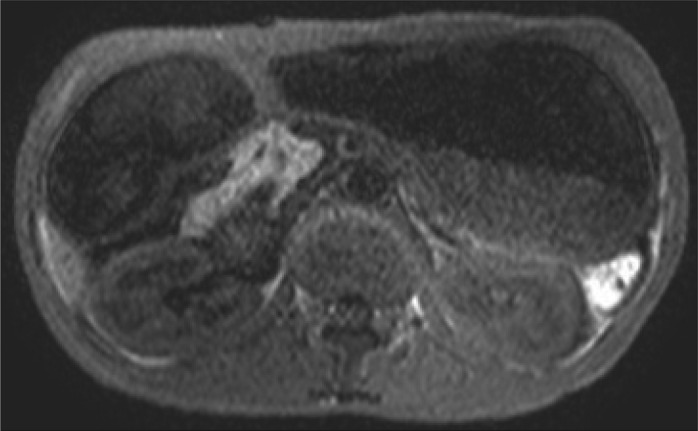
An MRI gradient echo sequence (T2 FFE) of the same patient showing hyperintense pancreatic tissue extending anteromedially to the duodenum with the crocodile jaw sign.
DISCUSSION
Pancreatic development starts with two ventral buds and one dorsal bud, which appear at about the fifth week of gestation. The two ventral buds unite and then rotate with the duodenum at about the seventh week of gestation. The ventral bud forms the uncinate process and the head of the pancreas, and the dorsal bud forms the body and tail of the pancreas. Failure of the ventral and dorsal buds to fuse results in entrapment of the duodenum (mostly the posterior part) by the pancreas and leads to formation of annular pancreas (1, 2, 4).
Annular pancreas can be complete or incomplete. In complete annular pancreas, a complete ring of pancreatic tissue surrounds the duodenum. In incomplete annular pancreas, an incomplete ring of pancreatic tissue surrounds a portion of the circumference of the duodenum, giving a “crocodile jaw” appearance. Complete annular pancreas is a well-known entity; however, incomplete annular pancreas is often poorly recognized and may be undetected, especially in patients who do not present with duodenal obstruction (2).
Preoperative diagnosis has improved considerably with the development of newer techniques such as ERCP and magnetic resonance cholangiopancreatography (MRCP). MRCP has superseded ERCP, as it is noninvasive (3). Annular pancreas can be diagnosed when pancreatic tissue is seen encircling the second part of duodenum. On CT and MRCP, a complete ring of pancreatic tissue surrounding the duodenum suggests complete annular pancreas, and posterolateral extension of pancreatic tissue to the duodenum suggests incomplete annular pancreas. Both MRI and multidetector CT reveal pancreatic tissue encircling the duodenum, which retains the signal intensity and density of normal pancreas even after contrast administration. Treatment consists of bypassing the duodenal obstruction by duodenoduodenostomy or laparoscopic gastrojejunostomy.
References
- 1.Ravitch MM, Woods AC., Jr Annular pancreas. Ann Surg. 1950;132(6):1116–1127. doi: 10.1097/00000658-195012000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sandrasegaran K, Patel A, Fogel EL, Zyromski NJ, Pitt HA. Annular pancreas in adults. AJR Am J Roentgenol. 2009;193(2):455–460. doi: 10.2214/AJR.08.1596. [DOI] [PubMed] [Google Scholar]
- 3.Dalal U, Singal R, Dalal AK, Kumar Y, Gupta S, Mendiratta P, Garg R. Enucleation of the solitary epithelial cyst of pancreatic head in an adult: a case report and review of the literature. Niger J Clin Pract. 2012;15(2):228–230. doi: 10.4103/1119-3077.97327. [DOI] [PubMed] [Google Scholar]
- 4.Choi BI, Yeon KM, Kim SH, Han MC. Caroli disease: central dot sign in CT. Radiology. 1990;174(1):161–163. doi: 10.1148/radiology.174.1.2294544. [DOI] [PubMed] [Google Scholar]