Abstract
The purpose of this report is to describe our experience with the implementation of a practice quality improvement (PQI) project in thoracic imaging as part of the American Board of Radiology Maintenance of Certification process. The goal of this PQI project was to reduce the effective radiation dose of routine chest CT imaging in a busy clinical practice by employing the iDose4 (Philips Healthcare) iterative reconstruction technique. The dose reduction strategy was implemented in a stepwise process on a single 64-slice CT scanner with a volume of 1141 chest CT scans during the year. In the first annual quarter, a baseline effective dose was established using the standard filtered back projection (FBP) algorithm protocol and standard parameters such as kVp and mAs. The iDose4 technique was then applied in the second and third annual quarters while keeping all other parameters unchanged. In the fourth quarter, a reduction in kVp was also implemented. Throughout the process, the images were continually evaluated to assure that the image quality was comparable to the standard protocol from multiple other scanners. Utilizing a stepwise approach, the effective radiation dose was reduced by 23.62 and 43.63 % in quarters two and four, respectively, compared to our initial standard protocol with no perceived difference in diagnostic quality. This practice quality improvement project demonstrated a significant reduction in the effective radiation dose of thoracic CT scans in a busy clinical practice.
Keywords: Quality improvement, Iterative reconstruction, Computed tomography, Dose reduction
Introduction
As radiology departments grow in complexity, the process of improving and maintaining excellence becomes more challenging than ever before. Systematic quality improvement projects are important for upholding the overall department quality [1]. The Maintenance of Certification (MOC) Program for radiology, which began in 2007, was designed to ensure ongoing self-assessment and lifelong learning. The program consists of four parts, the last of which entails practice quality improvement (PQI) projects [2, 3]. These projects may be completed by individuals or by a group. In 2012, the American Board of Radiology (ABR) mandated one new PQI project every 3 years as part of continuous certification, a change from the 2008 requirement of three PQI projects every 10 years [4–7]. Ultimately, these projects not only benefit patients, but may also come with the added incentive of higher reimbursement from the Centers for Medicare and Medicaid Services (CMS) [6, 8].
The ABR states that each PQI project should incorporate a Plan-Do-Study-Act (PDSA) process [9, 10]. First, an area within one’s practice that could benefit from quality improvement is identified and a plan with a set of measureable goals and methods for data collection are established. The plan is then tested, and problems are documented. Next, data from the plan is compared to the established goal. If the goal is not achieved, a root cause analysis is performed. Finally, a plan is set in motion from which a new improvement plan is devised for the next PDSA cycle [3, 11].
Medical radiation safety is a growing concern as the use of CT increases. Despite the debate over potential health risks, there remains evidence to suggest that we should be vigilant in the use of imaging that employs ionizing radiation [12–14]. Over the past several years, there has been increased emphasis on maintaining the principle of using radiation doses as low as reasonably achievable (ALARA principle) for diagnostic imaging. Recently, iterative reconstruction (IR) algorithms have demonstrated significant dose reduction while preserving or enhancing CT image quality [15–23].
The fourth generation iterative reconstruction technique, iDose4 (Philips Healthcare), was recently adopted at our institution. Previous studies demonstrated significant radiation dose reduction with iDose4 compared to filtered back projection (FBP), which had been our standard protocol [24–26]. The introduction of the iDose4 technique created an opportunity to develop a PQI project using the PDSA process. Over a 1-year period, we executed a plan for decreasing the radiation dose of our thoracic CT scans in a stepwise process. In this report, we describe our experience with conducting a successful radiation dose reduction PQI project in a busy academic clinical radiology practice.
Materials and Methods
Patients
This was a quality improvement initiative utilizing retrospective medical record review to analyze effective radiation dose trends before and after the implementation of an IR technique. Institutional review board approval was obtained for this Health Insurance Portability and Accountability Act-compliant study. Informed consent was waived for retrospective medical records review. All CT scans evaluated in this study were performed on a single CT machine at a tertiary medical care center. Both standard-resolution (5-mm axial slice thickness) and high-resolution (1-mm axial slice thickness) scans were reviewed. During the 1-year study period, 1141 thoracic CT scans were performed. Patient ages ranged from 18 to 91 years of age with a median age of 61 years.
Practice Quality Improvement Initiative
Our goal was to implement a thoracic CT dose reduction quality initiative using the iDose4 IR technique in clinical practice. This plan was instituted systematically over the course of 1 year following the PDSA formula. Effective radiation dose and image quality were reviewed in 3-month intervals, and adjustments to the iDose4 algorithm were made accordingly. The team of thoracic radiologists, radiology nurses, and radiology technicians were made aware of the protocol changes at each quarterly interval.
CT Protocol
All 1141 CT scans were performed on a single 64-section multidetector CT machine (Philips Brilliance 64, Cleveland, OH). At annual quarterly intervals, adjustments were made to the scanning protocol. In quarter one (Q1), all scans were performed with the FBP algorithm in the absence of IR with a standard tube voltage of 120 kVp. This was done to establish an effective dose baseline. At the start of quarter two (Q2), iDose4 was implemented with an IR strength of level 4 and a tube voltage of 120 kVp. These settings were continued until the end of quarter three (Q3). At the start of quarter four (Q4), the IR strength was increased to level 5 and the tube voltage was decreased to 100 kVp. We allowed for variable mAs including tube modulation in the z-axis in all scans in order to accommodate variable patient size.
CT Radiation Dose Assessment
Radiation dose-related parameters were retrieved from CT scan dose sheets using the Radiation Dose Intelligent Analytics for CT Examinations (RADIANCE) software (Philadelphia, PA) database [27]. Dose-length products (DLP) for each scan was recorded and used to estimate effective radiation dose (E) in mSv using the DLP to E conversion coefficient of 0.014.
Image Quality
The image quality of scans obtained on the iDose4 machine was closely monitored. Images were compared side-by-side on a daily basis in a single reading room workstation by a group of five subspecialty-trained thoracic radiologists to assure the image quality remained comparable to the prior exams from the non-iDose4 CT scans. Our practice sees a large number of cancer patients who require multiple follow-up CT scans. This provided the opportunity to make comparisons to prior images obtained on machines that use FBP when available. There was no perceived difference in diagnostic image quality during this project.
Statistical Analysis
Statistical analyses were performed using commercially available statistical software (SPSS, version 17.0; SPSS Inc., Chicago, IL). Radiation dose data was summarized as mean, standard deviation, median, 25th and 75th percentiles. The Student t test with the Bonferroni multiple comparisons correction was used to measure differences in effective radiation dose at 3-month intervals. A Bonferroni corrected P value of <0.05 was considered to be statistically significant.
Results
A total of 1141 chest CT scans were performed on a single CT scanner over 1 year. A standard FBP protocol was used for the first 3 months, and an iDose4 protocol was used for the remaining 9 months. Table 1 summarizes the number of thoracic CT scans per quarter.
Table 1.
Distribution CT scans per annual quarter. High resolution CT scans were performed with 1-mm axial slice thickness. Standard resolution CT scans were performed with 5-mm axial slice thickness
| Q1 | Q2 | Q3 | Q4 | |
|---|---|---|---|---|
| High resolution CT | 8 | 5 | 6 | 5 |
| Standard resolution CT | 303 | 231 | 275 | 308 |
| Total | 311 | 236 | 281 | 313 |
Following the PDSA method for implementing PQI projects, we successfully instituted an effective radiation dose reduction protocol. The estimated effective doses from each annual quarter are summarized in Table 2. The baseline dose obtained in Q1 using the standard FBP algorithm was 12.01 mSv (median 7.67 mSv; interquartile range 5.47–18.66 mSv). In Q2, the iDose4 IR technique was implemented with an iteration level of 4. The tube voltage remained constant at 120 kVp. The mean effective dose in this quarter was 9.18 mSv (median, 5.21 mSv; interquartile range 3.44–10.84 mSv), which was a 23.62 % reduction in effective dose from Q1 (P = 0.003). The CT protocol was unchanged during Q3, and the effective dose was 9.06 mSv (median, 5.84 mSv; interquartile range 3.77–10.98 mSv). This was a 24.60 % reduction in effective dose compared to Q1 (P < 0.001).
Table 2.
Descriptive summary of effective radiation dose in each annual quarter
| Annual quarter | Mean (SD) effective dose (mSv) | Median effective dose (mSv) | 25th percentile | 75th percentile | P value* |
|---|---|---|---|---|---|
| 1 | 12.01 (9.48) | 7.67 | 5.47 | 18.66 | |
| 2 | 9.18 (9.23) | 5.21 | 3.44 | 10.84 | 0.003 |
| 3 | 9.06 (8.81) | 5.84 | 3.77 | 10.98 | <0.001 |
| 4 | 6.77 (7.01) | 4.47 | 2.84 | 8.21 | <0.001 |
*Changes in mean effective dose for quarters 2-4 were compared to baseline dose from quarter 1
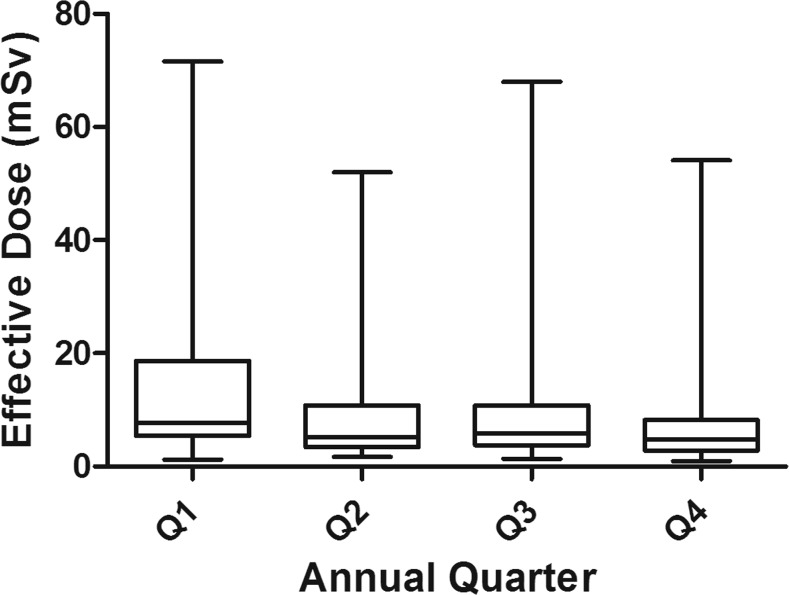
At the end of Q3, we reevaluated our plan with respect to dose reduction. We determined that we had successfully reduced radiation dose with the iDose4 protocol while maintaining high quality diagnostic images. However, based on the CT parameters at the time, further dose reduction seemed achievable. Therefore, the tube voltage was reduced from 120 to 100 kVp, and the iteration strength was increased from 4 to 5 at the start of Q4. The CT parameter modifications resulted in a mean effective dose of 6.77 mSv (median, 4.47; interquartile range 2.84–8.21 mSv). This was a 43.63 % reduction in effective dose from Q1 (P < 0.001). Figure 1 demonstrates the distribution of effective dose per quarter.
Fig. 1.
Boxplots demonstrating the effective radiation dose per annual quarter. CT scans from quarter 1 were performed at 120 kVp with the FBP algorithm. In quarters 2 and 3, images were acquired with the iDose4 technique (iterative strength of 4 and a tube voltage of 120 kVp). In quarter 4, images were acquired at 100 kVp and iterative strength was increased to 5
Discussion
The establishment of a clear, concise, and easily measurable PQI system will help radiologists effectively meet the part IV requirement of MOC. Practice quality improvement endeavors can be time consuming, and surveys among radiologists have demonstrated mixed opinions on the subject [28]. However, MOC demonstrates dedication to the delivery of high quality health care for patients. It is here to stay; therefore, formulating efficient and effective systems to execute the MOC process will help radiologists maintain department excellence.
The efficacy of the iDose4 technique has been validated in prior studies, which have demonstrated significant effective dose reduction with simultaneously improved image quality compared to FBP, particularly in low-dose comparisons [25, 29]. Rather, the radiation dose reduction initiative launched at our institution provides a model for implementing a systematic PQI project in a busy academic clinical practice. After confirming our goal to reduce radiation dose by implementing a new IR system, a baseline effective dose using the FBP algorithm was established. Significant effective dose reduction was then demonstrated following the introduction of the iDose4 technique. Next, we showed that we could maintain diagnostic image quality while further reducing effective dose by decreasing the tube voltage from 120 to 100 kVp and simultaneously increasing the iterative setting. By utilizing measureable outcomes in our project, we were able to quantitatively appraise the benefits of the IR technique. This was especially valuable as we optimized our imaging protocol in Q4. This PQI method can serve as a framework for addressing dose reduction initiatives in other sections of our radiology department for the next PDSA cycle.
Throughout our PQI process, there was subjective image quality evaluation by a small group of subspecialized thoracic radiologist. The images obtained with IR were compared to the images acquired with FBP on the same machine as well as to prior comparison images acquired on different FBP scanners. No subjective difference in diagnostic image quality was detected between FBP and IR during the project.
Several CT scans in our analysis were performed with additional acquisitions, such as multiple timing phases. The total effective dose for each scan, including the dose of all additional sequences, was recorded for our calculations. As a result, some of the CT exams in our PQSA cycle had relatively high effective doses despite iDose4 utilization. We intentionally included these studies in our analysis since our goal was to capture all clinical CT exams performed on the same scanner without introducing a selection bias and to simulate what may be seen in clinical practice.
Conclusion
In conclusion, we demonstrated an effective systematic PQI project for reducing thoracic CT radiation dose. Our method for assessing dose reduction may serve as a model to facilitate future dose reduction initiatives in other areas of CT imaging within the department.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no competing interests.
Contributor Information
Edwin A. Takahashi, Phone: 507-284-2511, Email: takahashi.edwin@mayo.edu
Marc D. Kohli, Phone: 317-715-6402, Email: mkohli@iu.edu
Shawn D. Teague, Phone: 303-398-1547, Email: teagues@njhealth.org
References
- 1.Hawkins CM, Alsip CN, Pryor RM, et al. Quality improvement and confirmation projects: facilitating rapid, measurable performance improvement. Radiographics. 2013;33(7):e225–35. doi: 10.1148/rg.337135058. [DOI] [PubMed] [Google Scholar]
- 2.Strife JL, Kun LE, Becker GJ, et al. The American board of radiology perspective on maintenance of certification: part IV—practice quality improvement for diagnostic radiology. Radiology. 2007;243(2):309–13. doi: 10.1148/radiol.2432061954. [DOI] [PubMed] [Google Scholar]
- 3.American Board of Radiology. MOC: Maintenance of certification. Available from: http://www.theabr.org/moc-landing. Accessed: May 8, 2014.
- 4.Griffith B, Brown ML, Jain R. Improving imaging utilization through practice quality improvement (maintenance of certification part IV): a review of requirements and approach to implementation. AJR Am J Roentgenol. 2014;202(4):797–802. doi: 10.2214/AJR.13.11607. [DOI] [PubMed] [Google Scholar]
- 5.Kouo T. Experience with a practice quality improvement system in a university radiology department. J Am Coll Radiol. 2012;9(11):814–9. doi: 10.1016/j.jacr.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 6.Keegan J, Miglioretti DL, Gould R, et al. Radiation dose metrics in CT: assessing dose using the National Quality Forum CT patient safety measure. J Am Coll Radiol. 2014;11(3):309–15. doi: 10.1016/j.jacr.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 7.Choudhery S, Richter M, Anene A, et al. Practice quality improvement during residency: where do we stand and where can we improve? Acad Radiol. 2014;21(7):851–58. doi: 10.1016/j.acra.2013.11.021. [DOI] [PubMed] [Google Scholar]
- 8.Silva E., 3rd MOC for dollars. J Am Col Radiol. 2011;8(11):746–8. doi: 10.1016/j.jacr.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 9.Tamm EP, Szklaruk J, Puthooran L, et al. Quality initiatives: planning, setting up, and carrying out radiology process improvement projects. Radiographics. 2012;32(5):1529–42. doi: 10.1148/rg.325125013. [DOI] [PubMed] [Google Scholar]
- 10.Lee CS, Larson DB. Beginner’s guide to practice quality improvement using the model for improvement. J Am Coll Radiol. 2014;11(12ptA):1131–6. doi: 10.1016/j.jacr.2014.08.033. [DOI] [PubMed] [Google Scholar]
- 11.Hirsch JA, Becker GJ, Derdeyn CP, et al. Maintenance of certification: part 2-continuous certification. J Neurointerv Surg. 2014;6(2):156–60. doi: 10.1136/neurintsurg-2013-010693. [DOI] [PubMed] [Google Scholar]
- 12.Smith-Bindman R. Is computed tomography safe? N Engl J Med. 2010;363(1):1–4. doi: 10.1056/NEJMp1002530. [DOI] [PubMed] [Google Scholar]
- 13.Brenner DJ, Doll R, Goodhead DT, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. PNAS. 2003;100(24):13761–6. doi: 10.1073/pnas.2235592100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Takahashi EA, Yoon HC. Four-year cumulative radiation exposure in patients undergoing computed tomography angiography for suspected pulmonary embolism. Radiol Res Pract. 2013;2013:482403. doi: 10.1155/2013/482403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beister M, Kolditz D, Kalender WA. Iterative reconstruction methods in X-ray CT. Phys Med. 2012;28(2):94–108. doi: 10.1016/j.ejmp.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalez-Guindalini FD, Ferreira Botelho MP, Tore HG, et al. MDCT of chest, abdomen, and pelvis using attenuation-based automated tube voltage selection in combination with iterative reconstruction: an intrapatient study of radiation dose and image quality. AJR Am J Roentgenol. 2013;201(5):1075–82. doi: 10.2214/AJR.12.10354. [DOI] [PubMed] [Google Scholar]
- 17.Christe A, Heverhagen J, Ozdoba C, et al. CT dose and image quality in the last three scanner generations. World J Radiol. 2013;5(11):421–9. doi: 10.4329/wjr.v5.i11.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee SW, Kim Y, Shim SS, et al. Image quality assessment of ultra low-dose chest CT using sonogram-affirmed iterative reconstruction. Eur Radiol. 2014;24(4):817–26. doi: 10.1007/s00330-013-3090-9. [DOI] [PubMed] [Google Scholar]
- 19.Ning P, Zhu S, Shi D, et al. X-ray dose reduction in abdominal computed tomography using advanced iterative reconstruction algorithms. PLoS One. 2014;9(3):e92568. doi: 10.1371/journal.pone.0092568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matsuki M, Murakami T, Juri H, et al. Impact of adaptive iterative dose reduction (AIDR) 3D on low-dose abdominal CT: comparison with routine-dose CT using filtered back projection. Acta Radiol. 2013;54(8):869–75. doi: 10.1177/0284185113488576. [DOI] [PubMed] [Google Scholar]
- 21.Kim M, Lee JM, Yoon JH, et al. Adaptive iterative dose reduction algorithm in CT: effect on image quality compared to filtered back projection in body phantoms of different sizes. Korean J Radiol. 2014;15(2):195–204. doi: 10.3348/kjr.2014.15.2.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prakash P, Kalra MK, Digumarthy SR, et al. Radiation dose reduction with chest computed tomography using adaptive statistical iterative reconstruction technique: initial experience. J Comput Assist Tomogr. 2010;34(1):40–5. doi: 10.1097/RCT.0b013e3181b26c67. [DOI] [PubMed] [Google Scholar]
- 23.Noel PB, Renger B, Fiebich M, et al. Does iterative reconstruction lower CT radiation dose: evaluation of 15,000 examinations. PLoS One. 2013;8(11):e81141. doi: 10.1371/journal.pone.0081141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arapakis I, Efstathopoulos E, Tsitsia V, et al. Using “iDose4” iterative reconstruction algorithm in adults’ chest-abdomen-pelvis CT examinations: effect on image quality in relation to patient radiation exposure. Br J Radiol. 2014;87:20130613. doi: 10.1259/bjr.20130613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lagmani A, Buhk JH, Henes FO, et al. Impact of a 4th generation iterative reconstruction technique on image quality in low-dose computed tomography of the chest in immunocompromised patients. Rofo. 2013;185(8):749–57. doi: 10.1055/s-0033-1335577. [DOI] [PubMed] [Google Scholar]
- 26.Li Q, Yu H, Zhang L, et al. Combining low tube voltage and iterative reconstruction for contrast-enhanced CT imaging of the chest—initial clinical experience. Clin Radiol. 2013;68(5):e249–53. doi: 10.1016/j.crad.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 27.Cook TS, Zimmerman S, Maidment AD, et al. Automated extraction of radiation dose information for CT examinations. J Am Coll Radiol. 2010;7(11):871–7. doi: 10.1016/j.jacr.2010.06.026. [DOI] [PubMed] [Google Scholar]
- 28.Yousem DM, Nidecker A. Maintenance of certification: update on attitudes of members of the American Society of Neuroradiology. AJNR Am J Neuroradiol. 2010;31(8):1369–72. doi: 10.3174/ajnr.A2029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khawaja RD, Singh S, Gilman M, et al. Computed tomography (CT) of the chest at less than 1 mSv: an ongoing prospective clinical trial of chest CT at submillisievert radiation doses with iterative model image reconstruction and iDose4 technique. J Comput Assist Tomogr. 2014;38(4):613–9. doi: 10.1097/RCT.0000000000000087. [DOI] [PubMed] [Google Scholar]