Abstract
Mandible fractures have a special place within the injuries of the other bones of the maxillofacial system. In their management, cosmetic issues and functional aspects such as chewing, speaking, and swallowing become very important.
In this study, a retrospective analysis of 419 mandible fractures in 283 patients was performed in relation to epidemiologic factors, treatment strategies, and complications. The average age was 32.14 years (4–69 years). The male/female ratio was 4/1. The most frequent etiologic factor was interpersonal violence (104 patients, 36.7%). The parasymphysis region was the mostly affected site (28.4%). A total of 157 patients (55.5%) were presented with single fracture and the rest with 2, 3, or 4 fracture lines on the mandible. The most common fracture combination was angulus–parasymphysis fracture combination (24.6%). Open reduction and fixation with mini plates and screws was the most preferred treatment strategy (48.2%). Transient short arch bars were not used intraoperatively for any of the patients. There was not any difference in terms of complications between the patients treated with plating systems and plating systems plus intermaxillary fixation.
In conclusion, proper treatment of mandible fractures is critical. Except certain fracture types, the usage of intermaxillary fixation as an adjunct to fixation with plating systems is not necessary.
Keywords: Arch bar, fixation, fracture, mandible, plate
Maxillofacial fractures are one of the most frequent and complicated problems of oral and maxillofacial surgery. Within these fractures, mandibula is one of the most affected bones. When all of the facial bone fractures are evaluated, incidence of the mandible fractures can be detected as ∼38%.1 If mandible fractures are not treated appropriately, they can cause morbidities at a high level. The most important aim of the treatment is to provide healing on both functional and cosmetic aspects. During the determination of treatment strategy, age of the patient, presence of additional injuries, comorbid diseases of the patient, trauma type, and localization of the fracture must be kept in mind. Although there are many developing techniques for the fixation of the fractures, still there is no consensus on the ideal treatment. In this study, it was aimed to evaluate the patients treated for mandible fractures retrospectively from different aspects such as epidemiology, way of treatment, and possible complications.
METHODS
A total of 419 mandible fractures in 283 patients treated at the Ankara Training and Research Hospital from April 2000 to August 2015 were examined retrospectively with the approval of the ethics committee of the hospital. Patients were evaluated according to age, sex, trauma type, season, localization of the fracture, and presence of comorbid injuries. Patients with gunshot wounds and those with bone defects were not included in the study. Obtained data were analyzed by using SPSS program version 15.0 (SPSS Inc, Chicago, IL).
RESULTS
Between 2000 and 2015, a total of 283 patients were operated with the diagnosis of mandible fracture in our clinic. Two hundred twenty eight of these patients were male (80.5%) and the rest 55 were female (19.5%). The male/female ratio was 4/1. The average age was found to be 32.14 years (4–69 years). Eight patients (2.8%) were between 4 and 10 years of age. Five patients (1.7%) were edentulous. The most frequent etiologic factor was detected as interpersonal violence with 36.7% in 104 patients. Traffic accidents (32.9%), falling down (29.3%), and work accidents (1.2%) were the following etiologies with decreasing order (Fig. 1).
FIGURE 1.
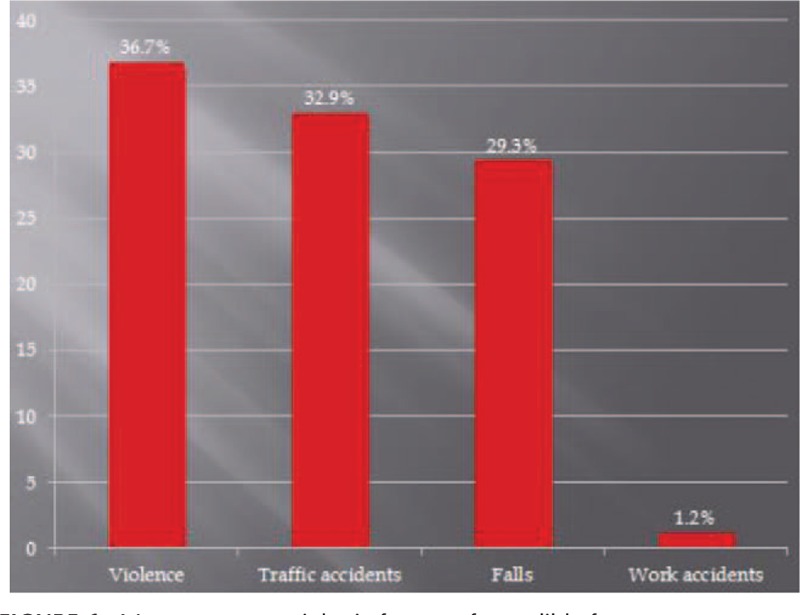
Most common etiologic factors of mandible fractures.
When the seasonal changes were evaluated, it was detected that mandible fractures were seen mostly in summer months (90 patients, 31.8%). Then autumn months (71 patients, 25.1%), spring months (69 patients, 24.4%), and winter months (53 patients, 18.7%) were coming.
Besides single fractures, there were patients with multiple fractures too. Although there were 157 patients (55.5%) with single fracture, 2 fractures were detected in 118 patients (41.7%), 3 fractures were detected in 6 patients (2.1%), and 4 fracture lines were detected in 2 patients (0.7%).
In 58 patients, extra fracture sites were detected besides mandible fracture. These were maxilla fracture in 16 patients, zygoma fracture in 15 patients, upper or lower extremity fracture in 12 patients, Le Fort fracture in 10 patients, orbital fracture in 3 patients, and nasal fracture in 2 patients (Fig. 2).
FIGURE 2.
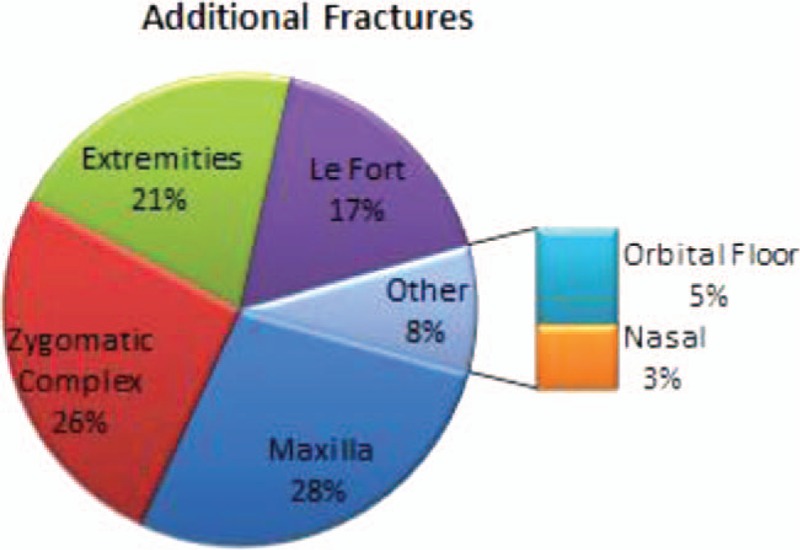
Distribution of additional fracture sites.
When the anatomic distribution of the total number of 419 mandible fractures were investigated, the parasymphysis region was the most affected site with 119 fractures (28.4%). Then comes angulus with 99 fractures (23.6%), subcondyle with 65 fractures (15.5%), symphysis with 44 fractures (10.5%), corpus with 42 fractures (10%), condyle with 25 fractures (6%), ramus with 20 fractures (4.8%), alveol with 4 fractures (1%), and coronoid with 1 fracture (0.2%, Fig. 3).
FIGURE 3.
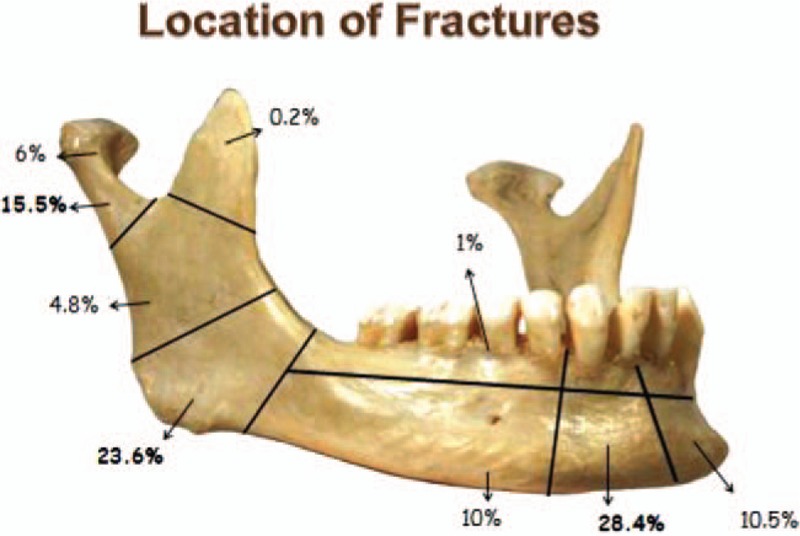
Anatomic distribution of the fracture sites.
When the anatomic distribution of 157 single fractures was investigated, the most affected areas were the parasymphysis region with 48 fractures (30.6%) and the angulus region with 45 fractures (28.7%). The other areas with decreasing order were subcondyle with 26 fractures (16.6%), corpus with 16 fractures (10.2%), symphysis with 12 fractures (7.6%), condyle with 6 fractures (3.8%), ramus with 3 fractures (1.9%), and alveol with 1 fracture (0.6%).
When 126 patients with multiple fractures were evaluated, it was seen that the most frequent fracture combination was combined angulus–parasymphysis fracture in 31 patients (24.6%). This was followed by parasymphysis–subcondyle fracture combination in 17 patients (13.4%).
As treatment modality, fixation with mini plates was used for 202 fractures with 48.2% (53 single, 149 multiple fractures), fixation with mini plates and intermaxillary fixation (IMF) with arch bar wires were used for 125 fractures with 29.8% (83 single, 42 multiple fractures), and only IMF with arch bar wires was performed for 73 fractures with 17.4% (67 single, 6 multiple fractures). Rest 14 fractures (3.3%) were treated with Barton bandage and 5 fractures (1.2%) with fixation with mini plates and IMF with screw (Fig. 4). Arch bar wires were discharged on average 3 weeks after the operation (2–4 weeks).
FIGURE 4.
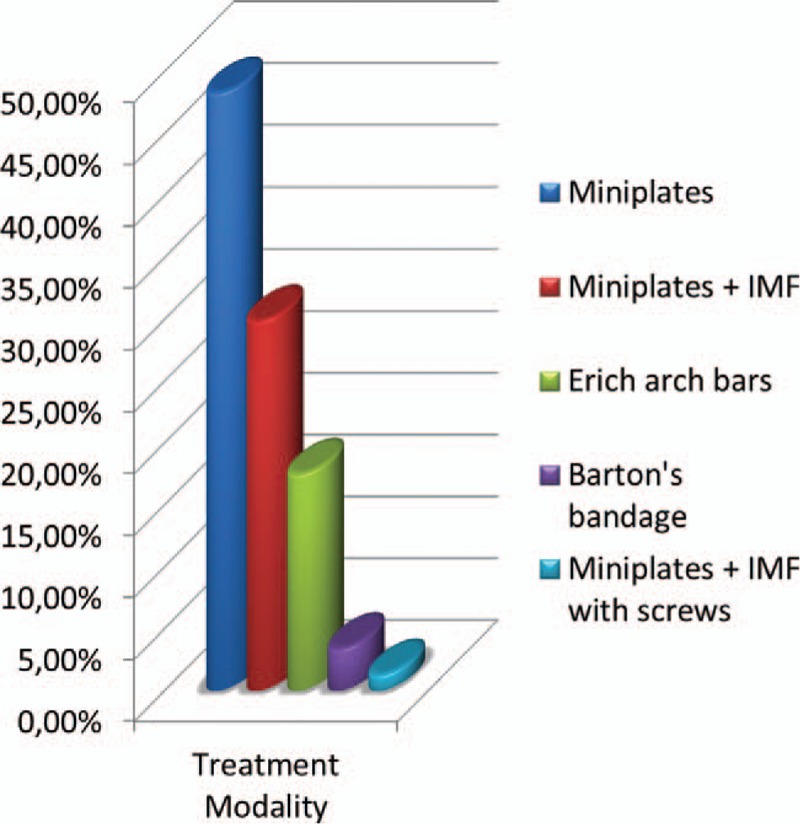
Preferred treatment modalities. IMF, intermaxillary fixation.
Patients were followed up on an average of 7 months (4–13 months). Infection, nonunion, and malunion were not detected in any of the patients in the follow-up period. Signs of paralysis of the frontal branch of the facial nerve were detected in 4 patients with high subcondyle fracture treated with open approach by using preauricular incision. In 1 patient, signs of paralysis of marginal mandibular nerve were detected after the usage of Risdon incision for low subcondyle fracture. In 6 patients with parasymphysis and symphysis fractures, numbness was detected on the sensory tract of the mental nerve after the surgery. All these patients were healed spontaneously 4 to 8 weeks after the surgery without any intervention.
Plate and screws were removed in 68 patients (24%). A total of 44 patients were operated for plate and screw removal in postoperative 6 months to 1 year. Rest 24 patients were operated in between postoperative first and fourth years. Cold intolerance, numbness, and pain were the chief complaints of the 54 patients who had plate and screw removal. For the rest 14 patients, plate and screw exposure is the main complaint. When the fracture localization of the patients with cold intolerance, numbness, and pain were examined, there were mini plates on parasymphysis in 28 patients, on symphysis in 14 patients, on corpus in 8 patients, on angulus in 3 patients, and on subcondyle region in 1 patient. When 14 patients with plate and screw exposure were investigated, plates were on parasymphysis region in 8 patients, on corpus area in 5 patients, and on symphysis region in 1 patient.
DISCUSSION
Mandible fractures can result from many different factors such as interpersonal violence, traffic accidents, gunshot wounds, sports accidents, work accidents, and falls.2 In the literature, although interpersonal violence is the leading cause in rural areas and developing countries, traffic accidents are the major etiologic factor in developed countries.3–6 In our study, similar to the literature, interpersonal violence was the most frequent etiologic factor. This situation can be related to the increasing economic problems of the society and increasing levels of substance addiction. When the age and sex were determined, in our study, patients treated for mandible fracture were mostly young men similar to the literature findings.4,7–9
Trauma type and etiologic factors are important to define the localization of the mandible fractures. For the patients with interpersonal violence, mostly angulus fractures or combined angulus–parasymphysis fractures are detected. On the other hand, the parasymphysis region is mostly affected in traffic accidents.2,7,10
When it is investigated independent from trauma type, different publications are present about the anatomic distribution of fractures. Condyle, angulus, corpus, and symphysis/parasymphysis areas are reported as the most frequent localizations in different studies.1,8,11 At this point, it is important to emphasize that condyle and subcondyle regions are the most difficult areas of the mandible with respect to evaluation, and the diagnosis of the fractures of these regions can be more challenging. In our study, parasymphysis was the most frequently detected localization. Angulus and subcondyle were the other frequent fracture sites. When the combined fractures are determined, the most seen fracture combination was angulus–parasymphysis in our study.
Treatment of isolated mandible fractures can be examined in 2 groups as surgical and nonsurgical.7,9 There are also different ideas about when to perform surgery. It was reported that there are not any difference between the reconstructions performed within the first 72 hours or later in relation to the complication rates.7,12,13 In our clinical practice, 252 patients (89%) were operated within the first 72 hours. A total of 24 patients (8.5%) were operated 3 to 7 days after the trauma, and the rest 7 patients (2.5%) were operated 7 to 14 days after the trauma due to additional injuries of the patients that preclude the surgery. In order to decrease pain and edema, until the operation time, Barton bandages were performed for these patients. When the complication rates were examined, we also did not find any difference between the patients with respect to the duration passed after the trauma until the surgery.
Planning of surgical treatment depends on many factors such as age, trauma type, presence of additional injury, dental profile of the patient, and localization of the fracture. There are many different treatment options such as IMF, open reduction and internal fixation, closed treatment with external fixation, and treatment with Kirschner wires.14 But still there is no consensus about the ideal treatment strategy. Especially for the treatment of condyle and subcondyle fractures, endoscopic reduction with internal fixation techniques are used too.15–17 Many authors have suggested that this technique combines advantages of both open and closed techniques. Most important advantages of this technique are limited scarring and decreased risk of facial nerve damage.18 But it also necessitates high level of technical skill, and possible complications may be higher in unqualified hands. Another limitation is that the technique is not easy to use in every type of fracture.
Today's concept for the treatment is usage of open reduction and internal fixation with rigid or semirigid plates and if necessary to support this treatment with IMF. Through years, plate osteosynthesis became quite popular in the treatment of mandible fractures. It has advantages such as providing a stable anatomic reduction, reducing the displacement on the fracture line in the postoperative period, and decreasing the need for IMF.5,19 Besides these, reduced recovery time and better functional results are the other advantages of the technique. In our clinical practice, we also mostly prefer open reduction and internal fixation with plate and screws as a treatment strategy. Besides this, IMF is also used as an adjunct to open reduction and internal fixation to decrease the displacement between the fracture fragments. We use only IMF in patients with favorable fractures and appropriate subcondyle fractures. In clinical practice, we prefer intraoral approach most of the time, but for the patients with ramus and subcondyle fractures, extraoral approach is also used if necessary.
When the treatment is concerned, we believe that subcondyle fractures necessitate a special interest. In our study, open approach was performed with or without IMF to the 31 of the 65 patients treated for subcondyle fracture (47.6%). A total of 14 of these patients (21.5%) were treated with only mini plates, and 16 of these patients (24.6%) were treated with mini plates and IMF with arch bar wires. One edentulous patient (1.5%) was treated with mini plates and IMF with screws. Twenty-eight of the 65 patients (43.1%) were treated with only IMF with arch bar wires, and the rest 6 patients (9.2%) were followed up by Barton bandages. Patients were classified according to Loukota classification.20 Preauricular and Risdon approaches were used for the 14 patients with high subcondyle fractures who were treated with open technique only. Risdon approach was performed alone for the 17 patients with low condyle fracture according to Loukota classification. In our clinic practice, open approach is preferred for subcondyle fractures when there is displacement into the middle cranial fossa, lateral extracapsular displacement of the condyle and impossibility of obtaining dental occlusion by closed reduction. Except these indications, we prefer the usage of IMF or follow-up with Barton bandages for the treatment.
Position of the teeth is one of the important aspects of diagnosis and treatment of mandible fractures. In the past, prophylactic tooth extraction was accepted as an essential step of the treatment in the presence of tooth on the fracture lines.21,22 But today, possible complications are quite decreased with the usage of rigid fixation with mini plate and screws and the usage of appropriate antibiotics. There are even studies that advocate that fracture reduction can be made more properly by preserving especially the molar teeth on their own places.23,24
In their retrospective analysis of mandibular angle fractures, Zanakis et al25 have not found any difference related to complications between the patients with teeth or without teeth on the fracture lines. In a similar manner, in our study, we did not find any correlation between the presence of teeth on the fracture lines and complication rates. Also, we did not perform prophylactic tooth extraction in any of the patients. Tooth extraction was performed only if there was root fracture or dislocations that prevent proper fracture reduction. We believe that if suitable postoperative care was given after reduction and rigid fixation with plates and screws, preservation of the healthy teeth on fracture lines do not affect the healing process in a negative manner.
Usage of IMF is also a controversial aspect of the treatment of mandible fractures. Although introduction of plating systems decrease the need for IMF, there are reports that suggest its usage intraoperatively to assist in reduction of the fracture sites and postoperatively to assist in fixation.26 For IMF, mostly Erich arch bar wires are used. But it has certain disadvantages such as possible damage to the teeth, difficulty of its placement to the posterior teeth, periodontal tissue injury, poor oral hygiene, and possible risk of needle stick type injuries for surgeons during the application.27,28 Also, the placement of the arch bars increases the operation time significantly and decreases the comfort of the patients to a lower degree. In our study, we did not use arch bars transiently during the operation for any of the patient. We performed fixation with miniplates for 202 fractures and fixation with miniplates and IMF for 125 fractures. Any difference was not detected in between these groups in terms of postoperative complication rates. So, except certain fractures that can be treated with IMF only, we do not use IMF as an adjunct to the fixation with miniplates.
Prevention of the complications after the treatment of mandible fractures is an important issue too. Independent from the usage of open or closed reduction, complication rates are directly related to the type of the injury and localization of the fracture. Especially mandibular angle fractures are prone to high postoperative complication risk.29 Infection, osteomyelitis, nonunion, malunion, and wound dehiscence are possible complications.30,31
In our study, infection was not detected in any of the patients in the follow-up period. This may be related to the routine usage of antibiotics in our clinical practice in the postoperative period. In the literature, antibiotic usage in the follow- up period is a controversial subject. There are reports that advocate antibiotic usage in different dosages and duration.19,32 In contrast to these reports, Abubaker and Rollert33 have reported in their study that postoperative antibiotic usage does not have any advantage to decrease infection. In our practice, besides antibiotic usage, in order to decrease possible contamination, feeding with clear liquid diet and usage of oral antiseptic gargle were also routinely advised to every patient for postoperative 2 weeks.
After the surgery, sensory changes are one of the important problems too. In our study, signs of paralysis of frontal, marginal mandibular and mental nerves were detected after the surgery in 11 patients, and these signs were resolved spontaneously in all of these patients in the postoperative period. Although, it is a frustrating complication, according to our findings, we can say that sensory problems are transient most of the time, and they are mostly related to the traction forces and edema.
Plate and screw removal was performed on 68 patients in our study. Majority of these patients were complaining about numbness, cold intolerance, and pain in the plate area. When these patients were analyzed, it was detected that most of the plates were on the symphysis, parasymphysis, and corpus areas. Besides the decreased amount of soft tissue over the plate and screws at these areas, we may suggest that easy palpation of these plates can be a possible factor for these subjective symptoms. So, psychological factors of the patients are also important about these symptoms. In our study, plate and screw removal was performed mostly within the postoperative 1 year. It must be kept in mind that removal of these plates are very difficult especially after the postoperative second year, and even then the surgeon must be very careful in order not to produce a new fracture during this operation.
Besides these, development of nonunion after the treatment of mandible fractures is an important problem too. Marthog et al34 have stated that there is not a big difference in the nonunion rates although many developed fixation techniques are used for the treatment. Nonunion rates are affected by many factors such as age, sex, trauma type, and fracture localization. Substance addiction is also an important factor that must be taken into account. Passeri et al have defined a positive correlation between chronic alcohol and drug usage and complications.35
In conclusion, proper treatment of mandible fractures is very important in order to obtain satisfactory functional and cosmetic results. Although there are different methods to achieve these goals, we believe that open reduction and fixation with plating systems is the best treatment modality with today's knowledge. According to our experience, addition of IMF with arch bars to the plating systems does not bring any additional profit. Even their usage can cause certain disadvantages such as possible gingival damage, tooth loss due to impaired gingival circulation, and intraoral hygiene problems. So the usage of arch bars must be kept in limited amounts for only certain types of fractures and well-defined indications.
Footnotes
The authors report no conflicts of interest.
REFERENCES
- 1.De Matos FP, Arnez MFM, Sverzut CE, et al. A retrospective study of mandibular fracture in a 40-month period. Int J Oral Maxillofac Surg 2010; 39:10–15. [DOI] [PubMed] [Google Scholar]
- 2.Van den Bergh B, Karagozoglu KH, Heymans MW, et al. Aetiology and incidence of maxillofacial trauma in Amsterdam: a retrospective analysis of 579 patients. J Craniomaxillofac Surg 2012; 40:165–169. [DOI] [PubMed] [Google Scholar]
- 3.Edwards TJ, David JD, Simpson DA, et al. Patterns of mandibular fractures in Adelaide, South Australia. Aust NZ J Surg 1994; 64:307–311. [DOI] [PubMed] [Google Scholar]
- 4.Ellis E, Moos KF, El-Attar A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Med Oral Pathol Oral Surg 1985; 59:120–129. [DOI] [PubMed] [Google Scholar]
- 5.Sakr K, Farag IA, Zeitoun IM. Review of 509 mandibular fractures treated at the University Hospital, Alexandria, Egypt. Br J Oral Maxillofac Surg 2006; 44:107–111. [DOI] [PubMed] [Google Scholar]
- 6.Melmed EP, Koonin AJ. Fractures of the mandible. Plast Reconstr Surg 1975; 56:323–327. [DOI] [PubMed] [Google Scholar]
- 7.Stacey DH, Doyle JF, Mount DL, et al. Management of mandible fractures. Plast Reconstr Surg 2006; 117:48–60. [DOI] [PubMed] [Google Scholar]
- 8.Gutta R, Tracy K, Johnson C, et al. Outcomes of mandible fracture treatment at an academic tertiary hospital: a 5-year analysis. J Oral Maxillofac Surg 2014; 72:550–558. [DOI] [PubMed] [Google Scholar]
- 9.Olson RA, Fonseca RJ, Osbon DB. Fractures of the mandible: a review of 580 cases. J Oral Maxillofac Surg 1982; 40:23–28. [DOI] [PubMed] [Google Scholar]
- 10.Bormann KH, Wild S, Gellrich NC, et al. Five-year retrospective study of mandibular fractures in Freiburg, Germany: incidence, etiology, treatment and complications. J Oral Maxillofac Surg 2009; 67:1251–1255. [DOI] [PubMed] [Google Scholar]
- 11.Chrcanovic BR, Abreu MHNG, Freire-Maia B, et al. 1454 mandibular fractures: a 3-year study in a hospital in Belo Horizonte, Brazil. J Craniomaxillofac Surg 2012; 40:116–123. [DOI] [PubMed] [Google Scholar]
- 12.Anderson T, Alpert B. Experience with rigid fixation of mandibular fractures and immediate function. J Oral Maxillofac Surg 1992; 50:555–560. [DOI] [PubMed] [Google Scholar]
- 13.Maloney PL, Welch TB, Doku HC. Early immobilization of mandibular fractures: a retrospective study. J Oral Maxillofac Surg 1991; 49:698–702. [DOI] [PubMed] [Google Scholar]
- 14.Ellis E, Walker L. Treatment of mandibular angle fractures using two mini-dynamic compression plates. J Oral Maxillofac Surg 1992; 50:958–963. [DOI] [PubMed] [Google Scholar]
- 15.Mueller R. Endoscopic treatment of facial fractures. Facial Plast Surg 2008; 24:78–91. [DOI] [PubMed] [Google Scholar]
- 16.Troulis MJ. Endoscopic open reduction and internal rigid fixation of subcondylar fractures. J Oral Maxillofac Surg 2004; 62:1269–1271. [DOI] [PubMed] [Google Scholar]
- 17.Schubert W, Jenabzadeh K. Endoscopic approach to maxillofacial trauma. J Craniofac Surg 2009; 20:154–156. [DOI] [PubMed] [Google Scholar]
- 18.Hackenberg B, Lee C, Caterson EJ. Management of subcondylar mandible fractures in the adult patient. J Craniofac Surg 2014; 25:166–171. [DOI] [PubMed] [Google Scholar]
- 19.Gabrielli MAC, Gabrielli MFR, Marcantonio E, et al. Fixation of mandibular fractures with 2.0-mm miniplates: review of 191 cases. J Oral Maxillofac Surg 2003; 61:430–436. [DOI] [PubMed] [Google Scholar]
- 20.Loukota RA, Eckelt U, De Bont L, et al. Subclassification of fractures of the condylar process of the mandible. Br J Oral Maxillofac Surg 2005; 43:72–73. [DOI] [PubMed] [Google Scholar]
- 21.Burch RJ. Treatment of displaced fractures of the edentulous mandibular angle. Oral Surg Oral Med Oral Pathol 1951; 4:1101–1107. [DOI] [PubMed] [Google Scholar]
- 22.Bradley RL. Treatment of fractured mandible. Am Surg 1965; 31:289–290. [PubMed] [Google Scholar]
- 23.Rai S, Pradhan R. Tooth in the line of fracture: its prognosis and its effects on healing. Indian J Dent Res 2011; 22:495–496. [DOI] [PubMed] [Google Scholar]
- 24.Chrcanovic BR. Factors influencing the incidence of maxillofacial fractures. Oral Maxillofac Surg 2012; 16:3–17. [DOI] [PubMed] [Google Scholar]
- 25.Zanakis S, Tasoulas J, Angelidis I, et al. Tooth in the line of angle fractures: the impact in the healing process. A retrospective study of 112 patients. J Craniomaxillofac Surg 2015; 43:113–116. [DOI] [PubMed] [Google Scholar]
- 26.Nandini GD, Balakrishna R, Rao J. Self tapping v/s Erich arch bar for intermaxillary fixation: a comparative clinical study in the treatment of mandibular fractures. J Maxillofac Oral Surg 2011; 10:127–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baurmash H, Farr D, Baurmash M. Direct bonding of arch bars in the management of maxillomandibular injuries. J Oral Maxillofac Surg 1988; 46:813–815. [DOI] [PubMed] [Google Scholar]
- 28.Lello JL, Lello GE. The effect of interdental continuous loop wire splinting and intermaxillary fixation on the marginal gingiva. Int J Oral Maxillofac Surg 1988; 17:249–252. [DOI] [PubMed] [Google Scholar]
- 29.Ellis E, Walker L. Treatment of mandibular angle fractures using two noncompression miniplates. J Oral Maxillofac Surg 1994; 52:1032–1036. [DOI] [PubMed] [Google Scholar]
- 30.Iizuka T, Lindqvist C. Rigid internal fixation of fractures in the angular region of the mandible: an analysis of factors contributing to different complications. Plast Reconstr Surg 1993; 91:265–271. [PubMed] [Google Scholar]
- 31.Iizuka T, Lindqvist C, Hallikainen D, et al. Infection after rigid internal fixation of mandibular fractures. J Oral Maxillofac Surg 1991; 49:585–593. [DOI] [PubMed] [Google Scholar]
- 32.Chuong R, Donoff RB, Guralnick WC. A retrospective analysis of 327 mandibular fractures. J Oral Maxillofac Surg 1983; 41:305–309. [DOI] [PubMed] [Google Scholar]
- 33.Abubaker AO, Rollert MK. Postoperative antibiotic prophylaxis in mandibular fractures: a preliminary randomized, double-blind and placebo-controlled clinical study. J Oral Maxillofac Surg 2001; 59:1415–1419. [DOI] [PubMed] [Google Scholar]
- 34.Mathog RH, Toma V, Clayman L, et al. Nonunion of the mandible: an analysis of contributing factors. J Oral Maxillofac Surg 2000; 58:746–752. [DOI] [PubMed] [Google Scholar]
- 35.Passeri LA, Ellis E, Sinn DP. Relationship of substance abuse to complications with mandibular fractures. J Oral Maxillofac Surg 1993; 51:22–25. [DOI] [PubMed] [Google Scholar]


