Abstract
To investigate the risk factors for failure of needling revision with 5-fluorouracil (5-FU) and to identify the correlation of outcomes of needling revision and the morphological features of dysfunctional filtration blebs using Moorfields bleb grading system.
This retrospective, nonrandomized, comparative case–control study included 41 consecutive patients (41 eyes) who underwent 5-FU needling revision for failed or failing filtration blebs between July 2012 and August 2014 in Chang Gung Memorial Hospital, a referral center in Taiwan. The main outcome measures were the bleb survival and the correlation factors of bleb morphology before revision. The secondary outcome measure was the identification of any study factor associated with bleb failure.
Forty-one eyes of 41 patients were included in this study. The most frequent glaucoma diagnoses were 10 cases (24%) of neovascular glaucoma and 8 cases (19%) of chronic open-angle glaucoma. Survival of bleb at 6, 12, and 24 months was 42%, 39%, and 23%. Fourteen cases (34%) maintained overall success at the last follow-up, with an average follow-up of 22.7 ± 9.4 months (range: 12–48 months). The central bleb area and height were significantly different between the successful needling group and the failed needling group (P = 0.03 and 0.04, respectively). Further trend test confirmed that smaller central bleb extension and flatter height were associated with a higher chance of failure (P = 0.02 and 0.02, respectively). Time from initial trabeculectomy to needling of less than 4 months and higher intraocular pressure (IOP) in the first postoperative week also led to significantly higher risk for failure (P = 0.01 and 0.03, respectively).
A small central area and the flat height of dysfunctional blebs were more likely to fail after the needle revision. Cautious case selections, taking account of the time from the initial filtering surgery and postoperative IOP, may improve the surgical outcome.
Keywords: 5-fluorouracil, bleb revision, failed trabeculectomy, morphology, needling
1. Introduction
Trabeculectomy is a standard surgical treatment for medically uncontrolled glaucoma. Compared with secondary trabeculectomy or drainage tube implantation, transconjunctival needle revision is an essential and simple technique in the management of failed or failing filtering bleb to restore the aqueous flow through the preexisting sclerectomy into the subconjunctival space with resultant adequate lowering of the intraocular pressure (IOP). Since the introduction of 5-fluorouracil (5-FU) as a therapeutic adjunct to prevent fibroblast proliferation within the subconjunctival space and Tenon's capsule 25 years ago, the success rate and overall pressure lowering effect have been satisfactory, even in some patients who were thought to be at higher risk for surgical failure.[1,2] In some series, the success rates range from 54% to 84% at 1 year, depending on different definitions of success and case selection.[3–7]
However, patients with failure after revision experience a course of IOP fluctuation, which results in further subconjunctival scarring. Therefore, the recognition of the blebs that have a higher chance of success or failure for revision is important to avoid repeat surgery. Several risk factors for failure of 5-FU needle revision were identified, including lack of mitomycin C (MMC) use during the initial filtration surgery,[8] fornix-based trabeculectomies,[9] preneedling IOP >30 mm Hg,[8,10] IOP >10 mm Hg immediately following needling revision,[5,8,10] and elevated bleb with highly vascularized or microcysts.[4] Of these factors, the majority have been reported with little consistency or even contradiction, and a clear picture of which patients benefit from needling revision is yet to emerge.[4] In addition, no objective bleb grading system has been used to describe the morphologic features when evaluating the risk factors for needle revision. Bleb morphology could change over time. Terms such as flat, elevated, localized, diffuse, thin walled, and thick walled are common to describe bleb appearances, but they lack the quantitative measures for bleb morphology during follow-up, and there might be a wide range of variations among different investigators.[11]
Multiple bleb grading systems have been developed. The Moorfields Bleb Grading System (MBGS) is commonly used since it was designed as a single independent grading scales[12]; most of other grading classifications have been proposed to describe bleb appearances among many other parameters as part of filtering surgery studies.[11] The MBGS parameters, including central bleb area, maximal bleb area, bleb height, central bleb vascularity, bleb edge vascularity, and nonbleb vascularity, offer a clear communication and good reproducibility between individuals.
Needling revision often needs to be repeated more than once and is not successful in some patients, even with multiple needling[8]; therefore, it is important to clarify the risk factors for failure of the initial needling revision procedure. Therefore, using MBGS, we conducted this study to identify the predictive factors and to evaluate the morphology of failing or failed trabeculectomy blebs associated with the outcome after needling revision with 5-FU.
2. Methods
2.1. Patient enrollment
This retrospective, observational, case–control study was conducted in Chang Gung Memorial Hospital, Linkou division, a tertiary referral center in Taiwan, from July 1, 2012 to August 31, 2014. All included cases were subjects who had failing or failed trabeculectomy and received needle revision with 5-FU by 2 glaucoma surgeons (SCW and SHLC). Patients who had received intraocular surgery, including cataract extraction or other ocular surface surgery before revision, were also included. Patients with IOP ≤21 mm Hg were included if the clinical findings were consistent with the progression of glaucomatous optic neuropathy. Exclusion criteria were incomplete morphological or clinical records, using another antifibrotic agent, such as MMC, or bleb revision after glaucoma drainage device (GDD) implantation rather than trabeculectomy. The bleb was classified prospectively by a single examiner (SHLC) according to the MBGS before revision.
The study was approved by the Institutional Review Board of Chang Gung Memorial Hospital and conformed to the tenets of the Declaration of Helsinki.
2.2. Surgical technique
All surgery was performed in the operating room. Topical anesthesia with 0.5% proparacaine hydrochloride was applied to the conjunctiva for at least 2 to 3 minutes. A 30-gauge needle was passed 2 to 3 mm from the edge of the failed bleb, underneath the conjunctiva, and parallel to the scleral plane. The needle was used to lyse subconjunctival fibrosis and episcleral scar tissue binding the scleral flap to elevate the scleral flap. Depending on the location and degree of fibrosis of the flap, the needle might be passed through the internal ostium of the sclerectomy to ensure the patency of the sclerectomy. The immediate desired result was egress of aqueous through the trabeculectomy flap, producing diffuse elevation of the bleb and decrease in the IOP. Finally, 5 mg (0.1 mL) 5-FU (Valeant Pharma Intl, Quebec, Canada) was injected around the newly created bleb as the needle was withdrawn.
2.3. Main outcome measures and follow-up
The main outcome measures were the bleb survival and the correlation factors of bleb morphology before revision. The secondary outcome measure was the identification of any other relevant clinical factor, such as the type of glaucoma or prior surgery history associated with bleb failure. All postoperative complications were documented. All patients were followed 1 day, 1 week, 2 weeks, 1 month, 2 months, 3 months, 6 months, 9 months, and 12 months after surgery, and every 3 months thereafter as needed. The minimum of follow-up after revision in this study was 12 months.
Success was defined as follows:
Complete success: IOP ≤21 mm Hg and IOP reduction from baseline of at least 20% without medication.
Qualified success: IOP ≤21 mm Hg and IOP reduction from baseline of at least 20% with medication.
Failure was defined as follows: IOP cannot be controlled under 21 mm Hg with medications on 2 successive visits or a need for further surgery (cyclophotocoagulation, trabeculectomy, revision, GDD implantation) to control IOP. More than 1 5-FU injection procedure was permissible, as long as all injections were performed within a 1-month period.
2.4. Statistics
Snellen acuities were transformed to logarithms of the minimum angle of resolution (logMAR) units before statistical analysis. The continuous variables were presented as the means ± standard deviation (SD), and the categorical variables were presented as frequencies and percentages. Pearson Chi-square and Fisher exact test were used to compare the difference in variables between success groups and failure groups. The Kaplan–Meier plots and Cox proportional hazards regression analysis were used to assess the association between survival and study factors, including bleb morphology. A P-value < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS software, version 20 (IBM, Chicago, IL).
3. Results
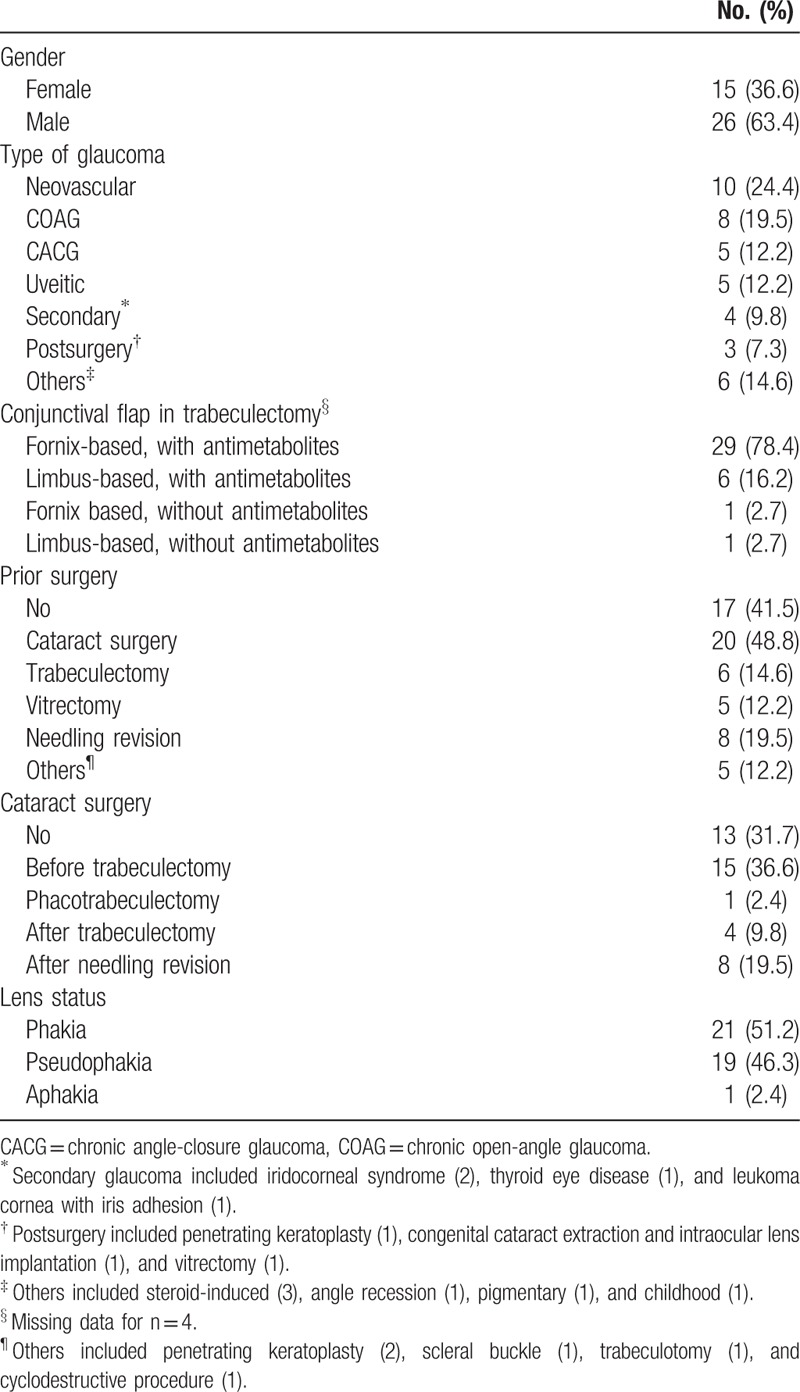
Forty-one eyes of 41 patients were included in this study. Fifteen patients (37%) were female and 26 patients (63%) were male. The patients had a mean age of 52.1 ± 15.8 years old (range: 13–78 years old). The most frequent glaucoma diagnoses were 10 cases (24%) of neovascular glaucoma (NVG), 8 cases (19%) of chronic open-angle glaucoma (COAG), 5 cases (12%) of chronic angle-closure glaucoma (CACG), and 5 cases (12%) of uveitic glaucoma. Thirty patients (81%) underwent initial fornix-based trabeculectomy, and 7 patients (19%) underwent initial limbus-based trabeculectomy. Seventeen patients (41%) did not previously undergo any ocular or intraocular surgery other than the index trabeculectomy, and 12 patients (29%) had undergone at least 2 kinds of surgery. Five patients (12%) had rubeosis iridis before needling. The IOP before needling was 30.3 ± 6.8 mm Hg, and the average number of antiglaucoma medications before needling was 2.9 ± 1.4. The demographics and patient profiles are shown in Table 1.
Table 1.
Demographics and patient profiles.
The median time between initial filtering surgery to revision was 6 months, and the average time was 25.2 ± 49.3 months (range: 1–256 months). Ten cases (24%) achieved complete success, and 6 cases (15%) achieved qualified success in the 1-year follow-up period. Cross-sectional survival at 6, 12, and 24 months was 42%, 39%, and 23%. Fourteen cases (34%) maintained overall success at the last follow-up, and the average follow-up duration was 22.7 ± 9.4 months (range: 12–48 months). Figure 1 shows the overall survival in the present study. Thirteen cases (52%) of 25 failure blebs were revived after repeated needling, with an average 1.8 ± 1.1 times of extra needling. Fifteen eyes (60%) of the failure cases occurred within first 3 months after needling, with a mean time to failure of 3.5 ± 2.6 months.
Figure 1.
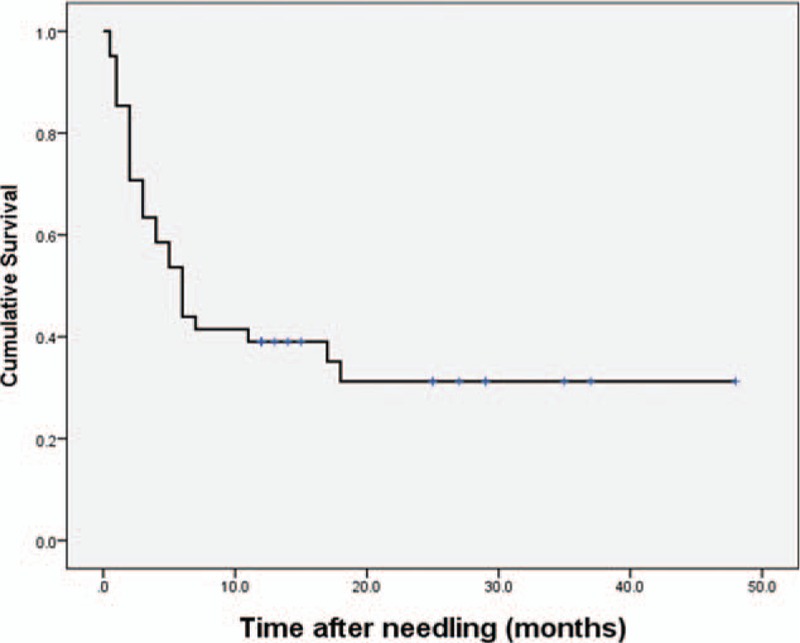
Kaplan–Meier survival plot for the patients in the present study.
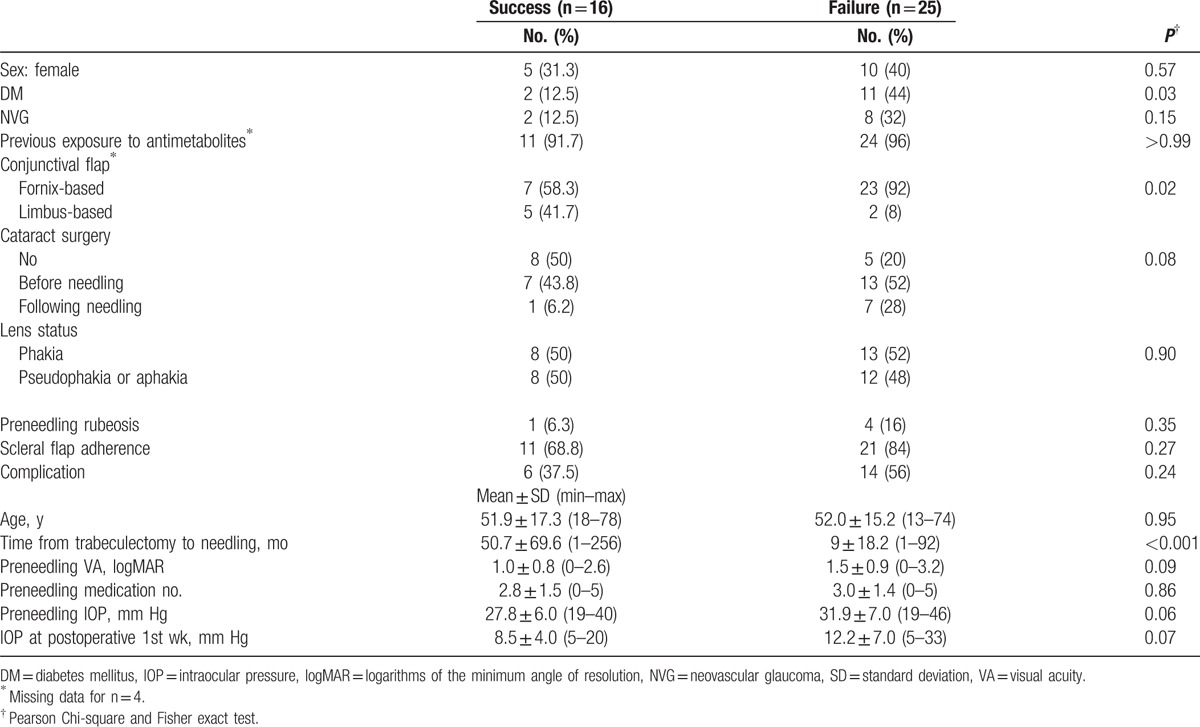
By comparing the characteristics of the successful and failed needling groups, the average time from trabeculectomy to needling was significantly longer in the successful cases (50.7 ± 69.6 months vs 9 ± 18.2 months, P < 0.001), and patients with a history of diabetes mellitus had significantly higher chance of failure (P = 0.03). The IOP in the first postoperative week was also borderline significantly lower in the successful cases (8.5 ± 4.0 mm Hg vs 12.2 ± 7.0 mm Hg, P = 0.07). Other variables, such as gender, exposure to antimetabolites at index trabeculectomy, lens status, preneedling IOP, preneedling medication numbers, scleral flap adherence, and surgical complications, showed no difference between groups. In the failure group, NVG patients had a shorter time to failure after revision than the other cases (2.6 ± 1.6 months vs 3.8 ± 2.8 months). These data are shown in Table 2.
Table 2.
Characteristics of patients following needling revision for failed blebs.
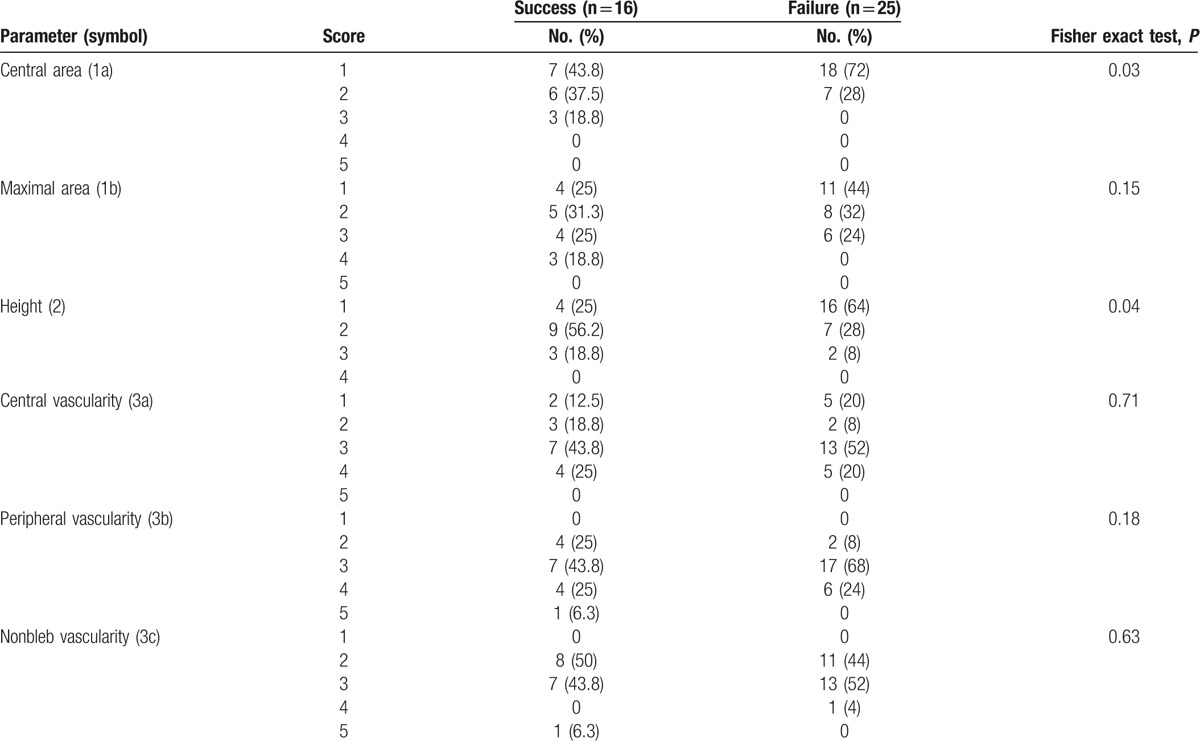
With regards to bleb morphology, the most frequent encountered failing or failed bleb was small and flat with moderate vascularity: 25 cases (61%) were scored as 1 in central bleb area; 28 cases (68%) were scored as 1 to 2 in maximal bleb area; 20 cases (49%) were scored as 1 in height; 20 cases (49%) were scored as 3 in central bleb vascularity; 24 cases (59%) were scored as 3 in peripheral bleb vascularity; 20 cases (49%) were scored as 3 in nonbleb vascularity. The detailed morphology distribution is summarized in Table 3. Central bleb area and height were significantly different between the successful needling group and the failed needling group (P = 0.03 and 0.04, respectively). Further trend test confirmed that smaller central bleb extension and flatter height were associated with a higher chance of failure (P = 0.02 and 0.02, respectively).
Table 3.
Bleb morphology distribution of patients following needling revision for failed blebs.
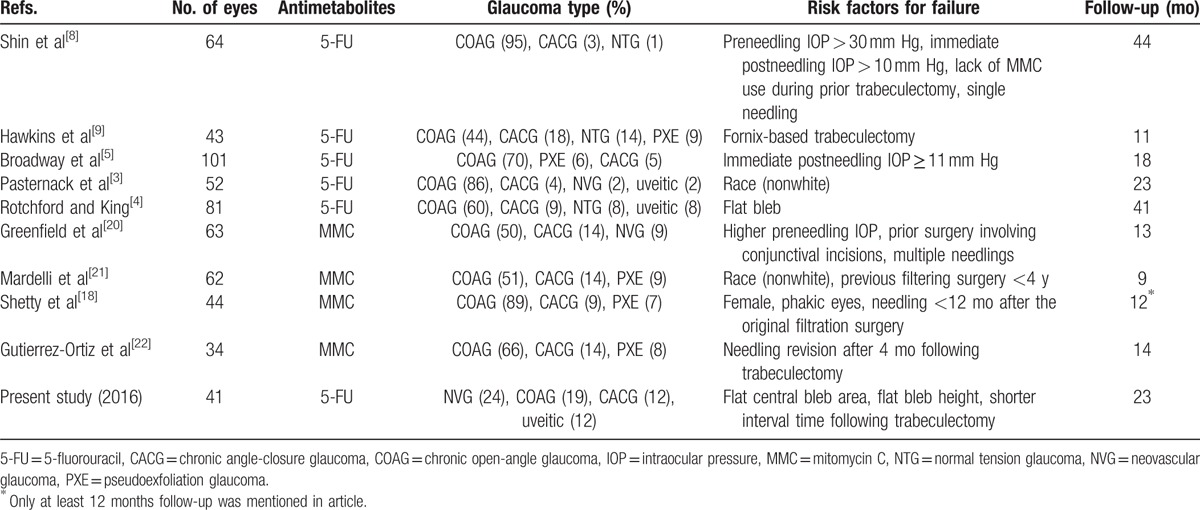
The potential risk factors for failure, using Cox proportional hazards regression analysis, are outlined in Table 4. Time from index trabeculectomy to needling of less than 4 months and higher IOP in the first postoperative week had significantly higher risk for failure (P = 0.01 and 0.03, respectively). Patients with a history of diabetes mellitus, prior fornix-based trabeculectomy, and higher preneedling IOP were also borderline risk factors for failure (P = 0.06, 0.05, and 0.03, respectively). The subgroup risk analysis of bleb morphology was also performed, but the differences were not statistically significant, which was not unexpected because of the reduced statistical power in small subgroup sizes. Further multivariate analysis in Table 5 revealed time from index trabeculectomy to needling of less than 4 months as a risk factor for failure (P = 0.03). Figure 2 depicts the survival of bleb and its relationship with potential risk factors.
Table 4.
Results of the Cox regression analysis.
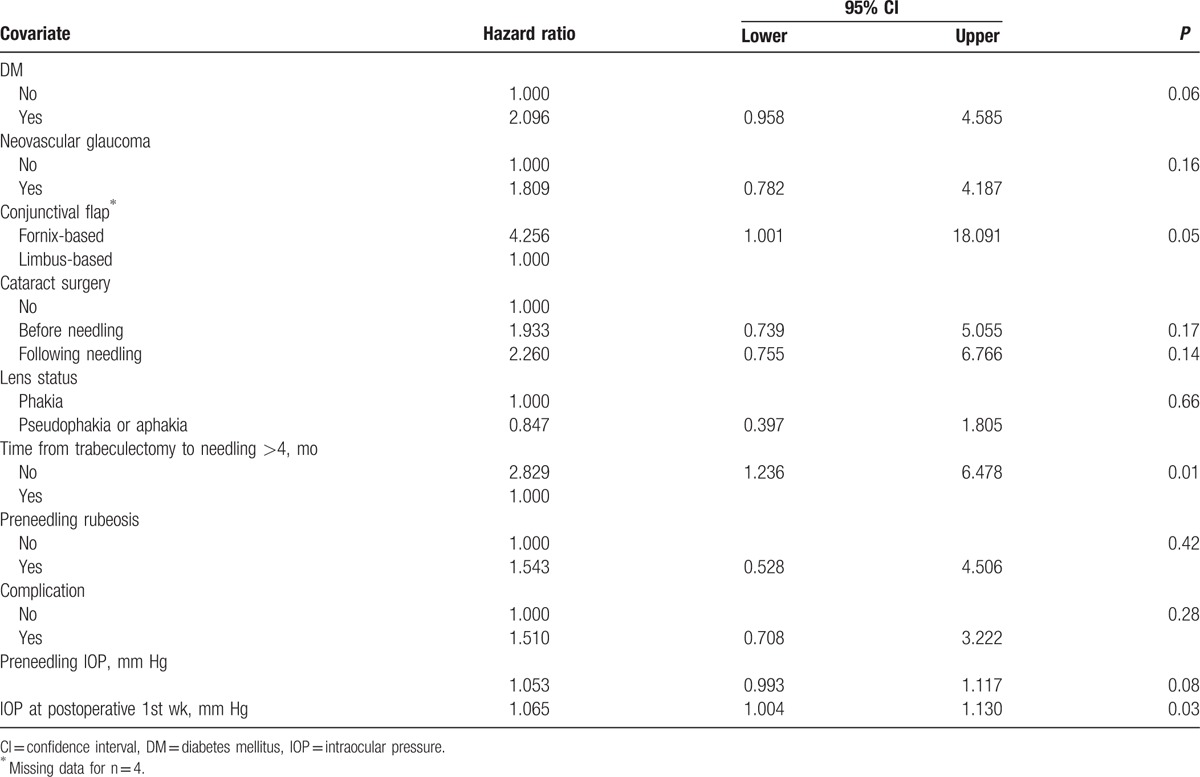
Table 5.
Risk factors for failure in the multivariate Cox regression analysis model.
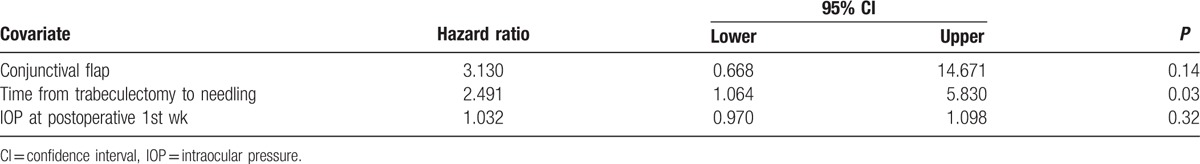
Figure 2.
Kaplan–Meier survival plot for potential risk factors for failure. (A) Different extension of central bleb area (1a) (log-rank test, P = 0.06). (B) Different height of the bleb (log-rank test, P = 0.06). (C) Interval from initial trabeculectomy to needling (log-rank test, P = 0.007). (D) Fornix-based trabeculectomy blebs versus limbus-based blebs (log-rank test, P = 0.02).
Surgical complications were recorded in 20 cases (49%), including 12 cases (29%) of hyphema, 8 cases (19%) of subconjunctival hemorrhage, 7 cases (17%) of shallow anterior chamber, and 1 case (2%) of buttonhole leakage after needling. All of the complications spontaneously resolved within 2 weeks. No diffuse corneal epitheliopathy, hypotony with choroidal effusion, collapsed anterior chamber, or other serious complications were encountered with the procedure. None of the complications that occurred in eyes that had an unsuccessful needling procedure were regarded as directly causative of the failure.
4. Discussion
Our present study used clinical bleb grading systems to classify the bleb morphology and demonstrated that flatter and smaller central area blebs were associated with failure after needling revision. Our results also indicated that cases with a history of diabetes mellitus and shorter interval from initial trabeculectomy to needling had a higher risk for failure. To our knowledge, this is the first paper using a standard grading system to assess the bleb morphology and surgical outcomes.
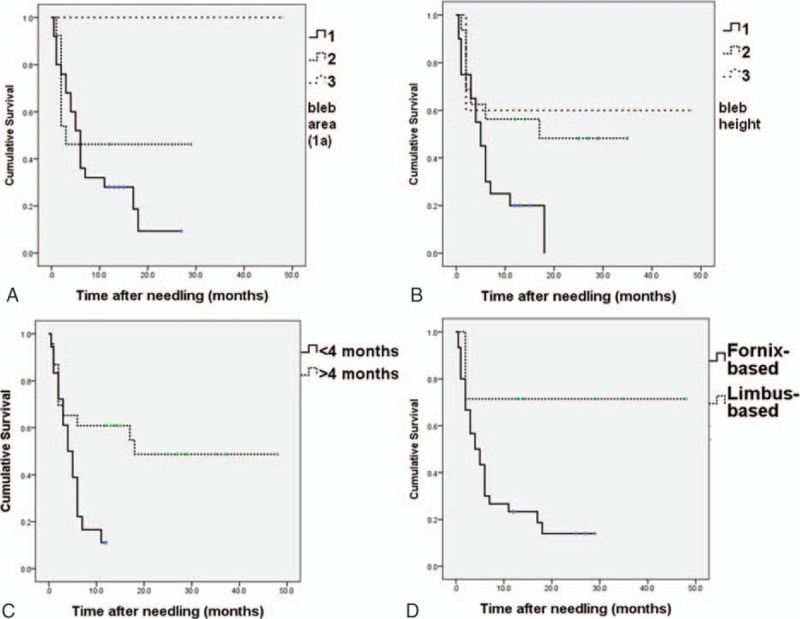
Bleb needling augmented with 5-FU is a safe and effective method to rescue dysfunctional filtration blebs from failure.[5] The intervention of 5-FU needling revision can produce long-term IOP control and avoid further surgery in a high proportion of patients with medically uncontrolled failing blebs.[10,13] No high-quality comparative research to determine the benefit of adjuvant 5-FU and MMC has been conducted because most authors using 5-FU or MMC have believed its use to be justified on a theoretical basis.[5,14] The results of published studies on indicators for failure in needling revision with antimetabolites are summarized in Table 6. Of these risk factors, few studies assessed the association of the morphological features and bleb survival.[4]
Table 6.
Literature review of reported case series of predictive factors in needling revision.
Successful glaucoma filtering surgery is characterized by the passage of aqueous humor from the anterior chamber to the subconjunctival space, which results in the formation of a filtering bleb.[15] Therefore, it is reasonable that appearance of the filtering bleb has an important predictive implication in assessing the survival of glaucoma surgery.[11] Hawkins et al[9] listed 5 preneedling bleb characteristics (encapsulation present or not, thick or thin, vascular or avascular, elevated or low lying, microcysts present or absent) to predict the survival of needle revision, but none of the characteristics showed a significant correlation with success or failure. Rotchford and King[4] reported that preneedling elevated bleb morphology was a predictor of survival in comparison with flat blebs, but the effect was significantly modified by the shorter timing of the needling, injected blebs, and microcystic blebs. However, the clinical pictures of blebs, such as height, vascularity or area, could have different extents, so a clear division of any equivocal clinical feature may not be easy. A vast range of possible interobserver variations within each of these descriptions may also exist.[11] MBGS and the Indiana Bleb Appearance Grading Scale (IBAGS), developed by Wells et al[12] and Cantor et al, respectively,[16] are 2 popular morphologic classifications of filtering blebs. Both methods are reproducible clinically and have high levels of interobserver agreement.[11] We used MBGS to classify the bleb appearance in our patients because of familiarity and the scales of vascularity in different areas of the bleb, which was not described in IBAGS. Our results showed blebs with higher height and larger central bleb extension before needling had a significantly higher chance of long-term success after revision.
The filtering surgery failure is most commonly due to fibrosis involving the episcleral–Tenon–conjunctival interface.[15] Kapetansky and Kapetansky[17] used ultrasonic biomicroscopy to evaluate bleb appearance in 30 eyes before MMC needling. They reported MMC bleb needling was more effective in lowering IOP when there was still a bleb present preoperatively. A bleb with higher height suggested less scarring in the subconjunctival space and was thus a reasonable indicator of success. Smaller bleb area and lower height also indicate the location of outflow obstruction was at the trab door or around the scleral flap. Inadequate flow from the scleral flap area may result in more severe conjunctival scarring. Because the central bleb area is located over the sclera flap controlling the egress of the aqueous outflow, it is not unexpected that a large central bleb area rather than maximal bleb extension is a predictor for success.
The determination of surgical outcomes after needling may be complex and multifactorial. Although many risk factors were previously reported (e.g., female,[18] race,[3] phakic eyes,[18] multiple previous surgical procedures,[19] prior surgery involving conjunctival incisions,[20] prolonged preoperative use of topical adrenergic drugs,[19] high preneedling IOP,[8,20] immediate high IOP after needling,[5,8] the interval between index trabeculectomy and needling,[18,21,22] and needling numbers[8,20]), little consistence was shown in the literature. In the present study, we found higher postneedling IOP at the first week, indicating inadequate aqueous outflow and stronger tendency of scarring, was an indicator for failure. The average IOP in the success group was 8.5 ± 4.0 mm Hg, and the average IOP in the failure group was 12.2 ± 7.0 mm Hg. The result echoes Shin et al[8] and Broadway et al,[5] who reported 10 mm Hg immediately after needling as the threshold between success and failure. We also found needling after fornix-based trabeculectomy was more likely to fail compared with limbus-based trabeculectomy. This risk factor was first proposed by Hawkins et al[9] but showed no significant difference in another study.[4] Hawkins postulated that needling a diffuse bleb with scarring is less effective than needling a focal bleb with scarring.[9] Theoretically, fornix-based with no incision through Tenon's capsule may result in a more diffuse and less encapsulated bleb compared with a limbus-based trabeculectomy.[23,24] Perhaps more scarring around the scleral flap in a dysfunctional fornix-based conjunctival bleb results in less success after needling revision, but more investigations to confirm this hypothesis are needed. Using multivariate analysis, a significantly higher chance of success was found in eyes that were needled more than 4 months after the original filtration surgery. Previous studies also showed a high success rate of revision in cases with long duration from original filtration surgery, but Gutierrez–Ortiz et al reported a contradictory result that needling revision after 4 months following trabeculectomy was associated with failure.[18,21,22] To explain the different results, Shetty el al[18] postulated that the inflammation of the episclera from the original filtering procedure may lead to failure if bleb needling is performed too early. Moreover, the glaucoma surgery in NVG, even augmented with MMC or 5-FU, often has a low success rate in early or long-term follow-up.[25,26] A high proportion of secondary glaucoma, such as NVG and uveitic glaucoma, rather than COAG, was included in our series, compared to previous reports.[4,5,8,9,22] The NVG cases in the current series usually had a shorter time to failure than the other cases in the failure group. Therefore, it is reasonable that a short interval is associated with failure in our study.
Different glaucoma diagnosis in the patient composition, accompanied with different definition of success in each study and criteria to repeat needling, may explain the inconsistent risk factors and success rate in different studies. Rotchford and King[4] reported a cross-sectional survival rate of 54% (IOP ≤21 mm Hg and at least 20% IOP reduction from baseline) at 1 year in 81 eyes, but more than 1 needling procedure was permissible, as long as all needlings were performed within a 6-month period. Kapasi and Birt[10] reported a total success rate of 65% after needling revision in 37 eyes undergoing trabeculectomy after 1 year or more, and repeat needling and laser trabeculoplasty within the 2-year follow-up period were acceptable as qualified success. Zheng et al[6] demonstrated a Kaplan–Meier survival rate of 60% with IOP ≤20 mm Hg at 5 years in 51 eyes, and multiple needle revisions were regarded as success if there was survival of more than 6 months between revisions. In our study, 14 cases (34%) achieved overall success at the last follow-up, with a mean follow-up period of 22.7 ± 9.4 months (range: 12–48 months). We considered the repeat needling or 5-FU application after revision 1 month or more as a new treatment course and classified the cases into the failure group. This stricter criterion may explain the different success rate in our study.
The surgical complications in our patients were usually mild and transient, including a few cases of hyphema, subconjunctival hemorrhage, shallow anterior chamber, and 1 case of buttonhole leakage. Previously reported major complications following needling revision, such as choroidal effusions,[27] suprachoroidal hemorrhages,[28] aqueous misdirection,[29] endothelial decompensation,[30] and endophthalmitis,[31] were not found in our cases.
A limitation of the study was that it was retrospective in study design. There was a greater proportion of fornix-based trabeculectomy compared with limbus-based trabeculectomy. Moreover, the morphological assessment in our series did not include the bleb wall (epithelial microcyst), which may also contribute to the bleb function.[9] Moreover, the clinical decision to perform a needling revision or to reintroduce medication was made without a formal protocol and without randomization.[13] Finally, different patient selection criteria may influence the data interpretation because a greater proportion of NVG and uveitic glaucoma was included in our series. Thus, caution must be exercised in generalizing the results of this study.
In conclusion, using standard bleb grading scales, our present study identified 2 morphological risk factors for failure: smaller central bleb extension and flatter height. Cautious case selections, taking account of the interval from initial filtering surgery and immediate IOP rise following needling, may also help clinicians to improve the overall outcome in 5-FU needling revision.
Footnotes
Abbreviations: 5-FU = 5-fluorouracil, CACG = chronic angle-closure glaucoma, COAG = chronic open-angle glaucoma, GDD = glaucoma drainage device, IBAGS = Indiana Bleb Appearance Grading Scale, IOP = intraocular pressure, logMAR = logarithms of the minimum angle of resolution, MBGS = Moorfields Bleb Grading System, MMC = mitomycin C, NVG = neovascular glaucoma, SD = standard deviation.
The authors have no conflicts of interest to disclose.
References
- 1.Ewing RH, Stamper RL. Needle revision with and without 5-fluorouracil for the treatment of failed filtering blebs. Am J Ophthalmol 1990; 110:254–259. [DOI] [PubMed] [Google Scholar]
- 2.Durak I, Ozbek Z, Yaman A, et al. The role of needle revision and 5-fluorouracil application over the filtration site in the management of bleb failure after trabeculectomy: a prospective study. Doc Ophthalmol 2003; 106:189–193. [DOI] [PubMed] [Google Scholar]
- 3.Pasternack JJ, Wand M, Shields MB, et al. Needle revision of failed filtering blebs using 5-Fluorouracil and a combined ab-externo and ab-interno approach. J Glaucoma 2005; 14:47–51. [DOI] [PubMed] [Google Scholar]
- 4.Rotchford AP, King AJ. Needling revision of trabeculectomies bleb morphology and long-term survival. Ophthalmology 2008; 115:1148.e4–1153.e4. [DOI] [PubMed] [Google Scholar]
- 5.Broadway DC, Bloom PA, Bunce C, et al. Needle revision of failing and failed trabeculectomy blebs with adjunctive 5-fluorouracil: survival analysis. Ophthalmology 2004; 111:665–673. [DOI] [PubMed] [Google Scholar]
- 6.Zheng L, Arvind H, Wechsler D. Outcomes: trabeculectomy bleb needle revision with 5-fluorouracil. J Glaucoma 2016; 25:317–323. [DOI] [PubMed] [Google Scholar]
- 7.Chang SH, Hou CH. Needling revision with subconjunctival 5-fluorouracil in failing filtering blebs. Chang Gung Med J 2002; 25:97–103. [PubMed] [Google Scholar]
- 8.Shin DH, Kim YY, Ginde SY, et al. Risk factors for failure of 5-fluorouracil needling revision for failed conjunctival filtration blebs. Am J Ophthalmol 2001; 132:875–880. [DOI] [PubMed] [Google Scholar]
- 9.Hawkins AS, Flanagan JK, Brown SV. Predictors for success of needle revision of failing filtration blebs. Ophthalmology 2002; 109:781–785. [DOI] [PubMed] [Google Scholar]
- 10.Kapasi MS, Birt CM. The efficacy of 5-fluorouracil bleb needling performed 1 year or more posttrabeculectomy: a retrospective study. J Glaucoma 2009; 18:144–148. [DOI] [PubMed] [Google Scholar]
- 11.Wells AP, Ashraff NN, Hall RC, et al. Comparison of two clinical Bleb grading systems. Ophthalmology 2006; 113:77–83. [DOI] [PubMed] [Google Scholar]
- 12.Wells AP, Crowston JG, Marks J, et al. A pilot study of a system for grading of drainage blebs after glaucoma surgery. J Glaucoma 2004; 13:454–460. [DOI] [PubMed] [Google Scholar]
- 13.Dalvi R, Orzech N, Kranemann C, et al. Five-year results of 5-fluorouracil augmented needling revision of failing blebs. Ophthalmic Surg Lasers Imaging 2012; 43:32–38. [DOI] [PubMed] [Google Scholar]
- 14.Cabourne E, Clarke JC, Schlottmann PG, et al. Mitomycin C versus 5-fluorouracil for wound healing in glaucoma surgery. Cochrane Database Syst Rev 2015; 11:CD006259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Skuta GL, Parrish RK., II Wound healing in glaucoma filtering surgery. Surv Ophthalmol 1987; 32:149–170. [DOI] [PubMed] [Google Scholar]
- 16.Cantor LB, Mantravadi A, WuDunn D, et al. Morphologic classification of filtering blebs after glaucoma filtration surgery: the Indiana Bleb Appearance Grading Scale. J Glaucoma 2003; 12:266–271. [DOI] [PubMed] [Google Scholar]
- 17.Kapetansky FM, Kapetansky SD. Antimetabolite use in revising failing filtering blebs. Semin Ophthalmol 1999; 14:144–151. [DOI] [PubMed] [Google Scholar]
- 18.Shetty RK, Wartluft L, Moster MR. Slit-lamp needle revision of failed filtering blebs using high-dose mitomycin C. J Glaucoma 2005; 14:52–56. [DOI] [PubMed] [Google Scholar]
- 19.Hodge W, Saheb N, Balazsi G, et al. Treatment of encapsulated blebs with 30-gauge needling and injection of low-dose 5-fluorouracil. Can J Ophthalmol 1992; 27:233–236. [PubMed] [Google Scholar]
- 20.Greenfield DS, Miller MP, Suner IJ, et al. Needle elevation of the scleral flap for failing filtration blebs after trabeculectomy with mitomycin C. Am J Ophthalmol 1996; 122:195–204. [DOI] [PubMed] [Google Scholar]
- 21.Mardelli PG, Lederer CM, Jr, Murray PL, et al. Slit-lamp needle revision of failed filtering blebs using mitomycin C. Ophthalmology 1996; 103:1946–1955. [DOI] [PubMed] [Google Scholar]
- 22.Gutierrez-Ortiz C, Cabarga C, Teus MA. Prospective evaluation of preoperative factors associated with successful mitomycin C needling of failed filtration blebs. J Glaucoma 2006; 15:98–102. [DOI] [PubMed] [Google Scholar]
- 23.Wang W, He M, Zhou M, et al. Fornix-based versus limbus-based conjunctival flap in trabeculectomy: a quantitative evaluation of the evidence. PLoS ONE 2013; 8:e83656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Solus JF, Jampel HD, Tracey PA, et al. Comparison of limbus-based and fornix-based trabeculectomy: success, bleb-related complications, and bleb morphology. Ophthalmology 2012; 119:703–711. [DOI] [PubMed] [Google Scholar]
- 25.Takihara Y, Inatani M, Fukushima M, et al. Trabeculectomy with mitomycin C for neovascular glaucoma: prognostic factors for surgical failure. Am J Ophthalmol 2009; 147:912–918.918.e1. [DOI] [PubMed] [Google Scholar]
- 26.Sisto D, Vetrugno M, Trabucco T, et al. The role of antimetabolites in filtration surgery for neovascular glaucoma: intermediate-term follow-up. Acta Ophthalmol Scand 2007; 85:267–271. [DOI] [PubMed] [Google Scholar]
- 27.Potash SD, Ritch R, Liebmann J. Ocular hypotony and choroidal effusion following bleb needling. Ophthalmic Surg 1993; 24:279–280. [PubMed] [Google Scholar]
- 28.Howe LJ, Bloom P. Delayed suprachoroidal haemorrhage following trabeculectomy bleb needling. Br J Ophthalmol 1999; 83:757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mathur R, Gazzard G, Oen F. Malignant glaucoma following needling of a trabeculectomy bleb. Eye (Lond) 2002; 16:667–668. [DOI] [PubMed] [Google Scholar]
- 30.Chalfin S, Memmen JE. Corneal endothelial toxic effect secondary to fluorouracil needle bleb revision. Arch Ophthalmol 1995; 113:1093–1094. [DOI] [PubMed] [Google Scholar]
- 31.Rebolleda G, Munoz-Negrete FJ. Phacoemulsification in eyes with functioning filtering blebs: a prospective study. Ophthalmology 2002; 109:2248–2255. [DOI] [PubMed] [Google Scholar]


