Abstract
This study was conducted to investigate the effects of depression and antidepressant medications on hip fracture. The database of the Taiwan National Health Insurance with medical records of more than 1,000,000 individuals was searched for patients who had hip fracture with or without depression from 1998 to 2009. Patients with the following conditions were excluded: hip fracture due to cancer or traffic accidents, hip fracture that occurred before the diagnosis of depression, and use of antidepressants before the diagnosis of depression. A matched cohort of 139,110 patients was investigated, including 27,822 (17,309 females; 10,513 males) with depression and 111,288 (69,236 females; 42,052 males) without depression (1:4 randomly matched with age, sex, and index date). Among these patients, 232 (158 females and 74 males) had both hip fracture and depression, and 690 (473 females and 217 males) had hip fracture only. The Cox proportional-hazards regression method was used to determine the effect of depression on hip fracture. The hazard ratio (HR) for each clinical parameter was calculated after adjusting for confounders including sex, age, Charlson comorbidity index, urbanization, osteoporosis, and antidepressants. Results showed that patients with major depressive disorder had a 61% higher incidence of hip fracture than those without depression (HR 1.61, 95% confidence interval [CI] 1.19–2.18, P = 0.002). The risk of hip fracture for patients with less severe depressive disorder (dysthymia or depressive disorder, not otherwise specified) was not statistically higher than that of patients with no depression (HR 1.10, 95% CI = 0.91–1.34, P = 0.327). Among the patients with depression, females had a 49% higher incidence for hip fracture than males (HR 1.49, 95% CI 1.30–1.72, P < 0.001). The incidence of hip fracture also increased with age and Charlson comorbidity index scores. Analyses of both all (139,110) patients and only patients (27,822) with depression revealed that antidepressants had no negative impact on the incidence of hip fracture. In conclusion, major depression was found to be a risk factor for hip fracture and that use of antidepressants had no adverse effect on hip fracture in the Taiwanese population.
Keywords: Charlson comorbidity index, defined daily dose, depression, hazard ratio, hip fracture, SNRI, SSRI
1. Introduction
Hip fracture (HF) is a devastating disease with an acute mortality rate of approximately 5% and 1-year mortality rate of 15% to 25%.[1] It has been estimated that 20% of patients who suffer a HF completely lose the ability to walk.[1] Osteoporosis is a major cause of HF. Risk factors for osteoporosis-related HF include age, osteoarthritis, disability before fracture, malnutrition, muscle weakness, arthritis, cognitive deficit, and impaired balance, visual ability, or activity of daily living. Osteoporosis is usually diagnosed by determining bone mineral density (BMD) that is closely related to dietary intake of calcium and protein, serum vitamin D level, and weight-bearing physical activity.[2,3] Many diseases such as those affecting bone mineral homeostasis, imbalance of bone remodeling, and collagen synthesis may also affect BMD.[4]
Similar to osteoporosis, depression (DP) is a common disorder and is a leading cause of disability, affecting at least 120 million people worldwide.[5] Approximately 10% of adults in the United States are prescribed with an antidepressant for more than 6 months.[6] Selective serotonin reuptake inhibitors (SSRIs) are the most widely prescribed antidepressants. On average, antidepressant prescriptions are increased by 10% per year.[7] DP has been implicated as a risk factor for low BMD[8–17] and fracture.[11,18–23] Some studies found that the relationship between DP and low BMD is more pronounced in men,[12,13,24] but another study found such relationship occurs more significantly in women.[14] However, some studies found no association between DP and BMD[25–28] or HF.[28] It is possible that the relationship between DP and BMD or fracture varies with sex or race.
To investigate the effects of DP and use of antidepressants on HF in the Taiwanese population, we analyzed the information extracted from the database of the National Health Insurance (NHI) of Taiwan. This national insurance program was initiated in 1995.[29] Currently, it covers more than 99.5% of the total population of approximately 23 million in Taiwan. The NHI database was established in 1997 by the National Health Research Institute (NHRI) and is updated regularly.[29] This large sample size would minimize the bias in selection of study participants. As this database contains detailed demographic and clinical information of patients, it allows a more accurate assessment of the correlation between diseases and their risk factors. Since results of previous studies on the relationship between DP and HF are inconsistent, we took advantage of this database and conducted 2 prospective cohort studies to clarify the matter. The first one investigated effect of DP on HF rates. The second one investigated whether the use of antidepressants leads to increased incidence of HF.
2. Materials and methods
2.1. Subjects
The NHRI research database of the NHI of Taiwan was searched for patients who were diagnosed with DP (International Classification of Diseases [ICD]-9-CM 296.2 and 296.3 for major depressive disorder [MDD], 300.4 for dysthymia, and 311 for depressive disorder, not otherwise specified [depressive disorder, NOS]) and those who had HF (ICD-9-CM 820) from 1998 to 2009. The ICD-9 coding system was used in this study because the ICD-10 system was not adopted in Taiwan until 2015. Patients with DP were defined as those who had at least 2 clinical visits or 1 hospital admission for DP within 1 year. Major and other depressive disorders were diagnosed as described previously.[30,31] Briefly, patients with at least 5 of the following 9 symptoms were considered as having an MDD: depressed mood or irritable most of the day, decreased interest or pleasure in most activities, significant weight change (5%) or change in appetite, insomnia or hypersomnia, psychomotor agitation or retardation, fatigue or loss of energy, feelings of worthlessness, or excessive or inappropriate guilt, diminished ability to think or concentrate, and thoughts of death or suicide. Other depressive disorders (dysthymia or depressive disorder, NOS) with fewer symptoms than MDD were considered as less severe forms of DP. Patients with the following conditions were excluded: HF due to cancer or traffic accidents, HF that occurred before or within 6 months after the diagnosis of DP, and use of antidepressants before the index date. The diagnosis date of DP was set as the index date. Each patient with DP was compared with at least 4 randomly selected individuals without DP by matching their age and sex. All patients were followed from the index date up to the date of HF or the end of 2009. This study was approved by the Institutional Review Board of Chang Gung Memorial Hospital (approval number: CGMHIRB 103–3585B).
2.2. Charlson comorbidity index
The Charlson comorbidity index (CCI) was determined as described by Charlson et al and Quan et al.[32,33] Patients with the following conditions were given a CCI of 1: myocardial infarct, congestive heart failure, peripheral vascular disease, dementia, cerebrovascular disease, chronic lung disease, connective tissue disease, ulcer, chronic liver disease, or diabetes. Patients with a CCI of 2 included those with hemiplegia, moderate or severe kidney disease, diabetes with end-organ damage, tumor, leukemia, or lymphoma. Patients with moderate or severe liver disease were assigned a CCI of 3, and those with malignant tumor, metastasis, or AIDS were given a CCI of 6.
2.3. Drug evaluation
The use of the following drugs was investigated: selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs), serotonin-norepinephrine reuptake inhibitors (SNRIs), serotonin antagonist and reuptake inhibitors (SARIs, such as trazodone) mirtazapine, bupropion, and monoamine oxidase inhibitors (MAOI). SSRI drugs evaluated in this study included fluoxetine, citalopram, paroxetine, sertraline, fluvoxamine, and escitalopram. Evaluation of drug usage was based on defined daily dose (DDD). A DDD value less than 28 was considered nonuse (level 0). Drug doses were classified into the following 4 levels: level 1, 28 to 83 DDD; level 2: 84 to 167 DDD, level 3, 168 to 335 DDD, and level 4, ≥336 DDD. Only patients who were on any of the aforementioned drugs for more than 180 days were investigated.
2.4. Classification of urbanization
Townships and cities in Taiwan had been classified into 7 urbanization groups, including highly urbanized, moderately urbanized, emerging, ordinary, aging, agricultural, and rural cities.[34] This classification was based on the data of the 2000 Taiwan census, Survey of Health Maintenance Organization, and Health Service Utilization. Variables used for the classification included population density, number of physicians per 100,000 people, and population ratio of farmers, people with college or higher educational levels, and people over 65 years old. In this study, we combined some of these groups together and classified urbanization as very high (highly urbanized), high (moderately urbanized and emerging), moderate (ordinary and aging), and low (agriculture and rural).
2.5. Statistical analyses
Comparisons of differences in demographic characteristics, CCI, osteoporosis, and antidepressants between the cohorts with and without DP were conducted using the Pearson chi-square test and t test. To measure the effect of DP on HF, the multivariate Cox proportional-hazards analysis was performed after adjusting for sex, age, urbanization, CCI, osteoporosis, and antidepressants. Hazard ratios (HRs) of antidepressants on HF were also calculated by the multivariate Cox proportional-hazards method. Cumulative incidence of HF during the entire follow-up period was estimated by the Kaplan–Meier method and compared by the log-rank test. The period for evaluation of CCI was within 1 year before the index date. All analyses were performed with the SAS statistical software (version 9.4).
3. Results
3.1. Patients
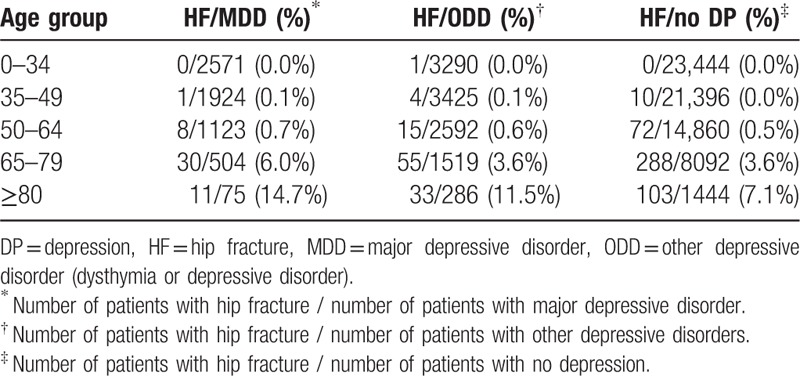
In all, 139,110 patients were investigated in this study, including 27,822 (17,309 females; 10,513 males) with DP and 111,288 (69,236 females; 42,052 males) without DP (Table 1 and Fig. 1). These patients included 232 (158 females and 74 males) with both HF and DP, and 690 (473 females and 217 males) with fracture only. Patients with DP were further classified as having major (MDD) or other depressive disorder (ODD) including dysthymia and depressive disorder, not otherwise specified. The following 6 groups of patients were studied: MDD with HF (77 patients, 27 males and 50 females), MDD without HF (9649 patients), ODD with HF (155 patients, 47 males and 108 females), ODD without HF (17,941 patients), no DP with HF (690 patients), and no DP and no HF (110,598 patients).
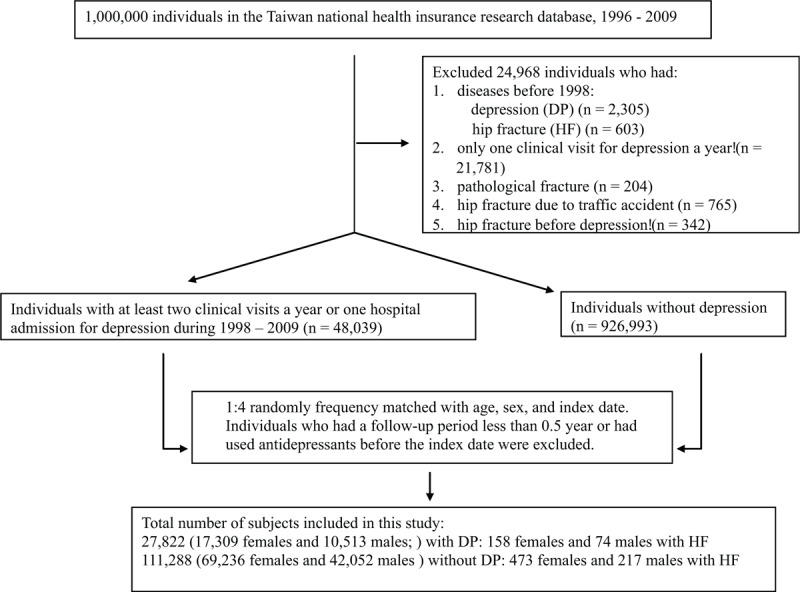
Table 1.
Number and percent of patients in various categories.
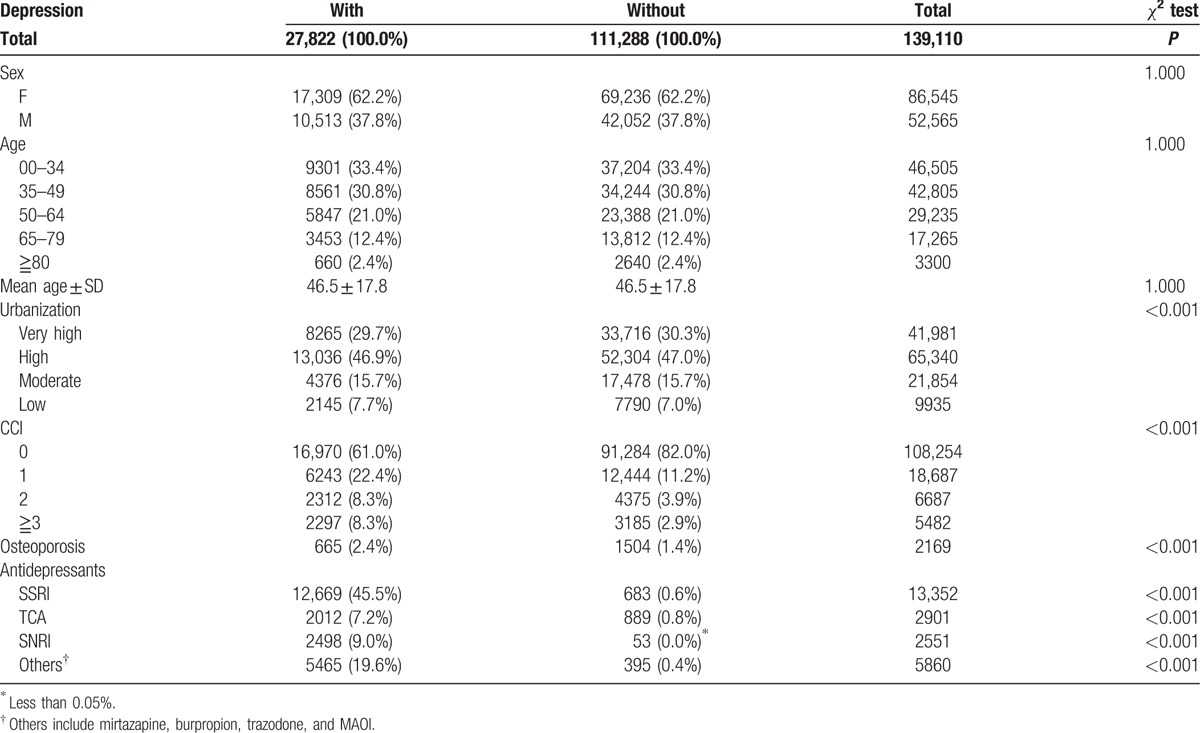
Figure 1.
Selection of patient cohorts for this study. DP = depression, HF = hip fracture, MDD = major depressive disorder, ODD = other depressive disorder.
3.2. Correlation between depression and hip fracture
The cumulative incidence of HF was consistently higher in patients with DP than those with no DP every year during the entire 12 years of follow-up (Fig. 2). Compared with those who had no DP (HR 1), the HR for HF in patients with MDD was 1.61 (95% confidence interval [CI] 1.19–2.18, P = 0.002) after adjusting for confounders (Table 2 and Fig. 3). ODD was found not to be a significant risk factor for HF (multivariate HR 1.10, 95% CI 0.91–1.34, P = 0.327) (Table 2 and Fig. 3).
Figure 2.
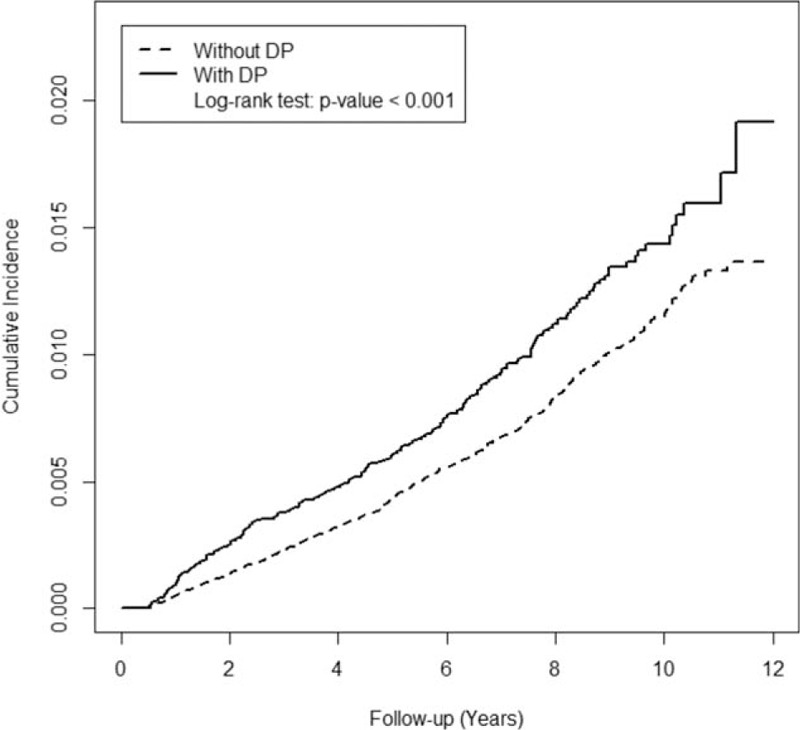
Kaplan–Meier cumulative incidence curves of hip fracture in patients with or without depression.
Table 2.
Unadjusted and adjusted Cox hazard ratios of patients in various categories.
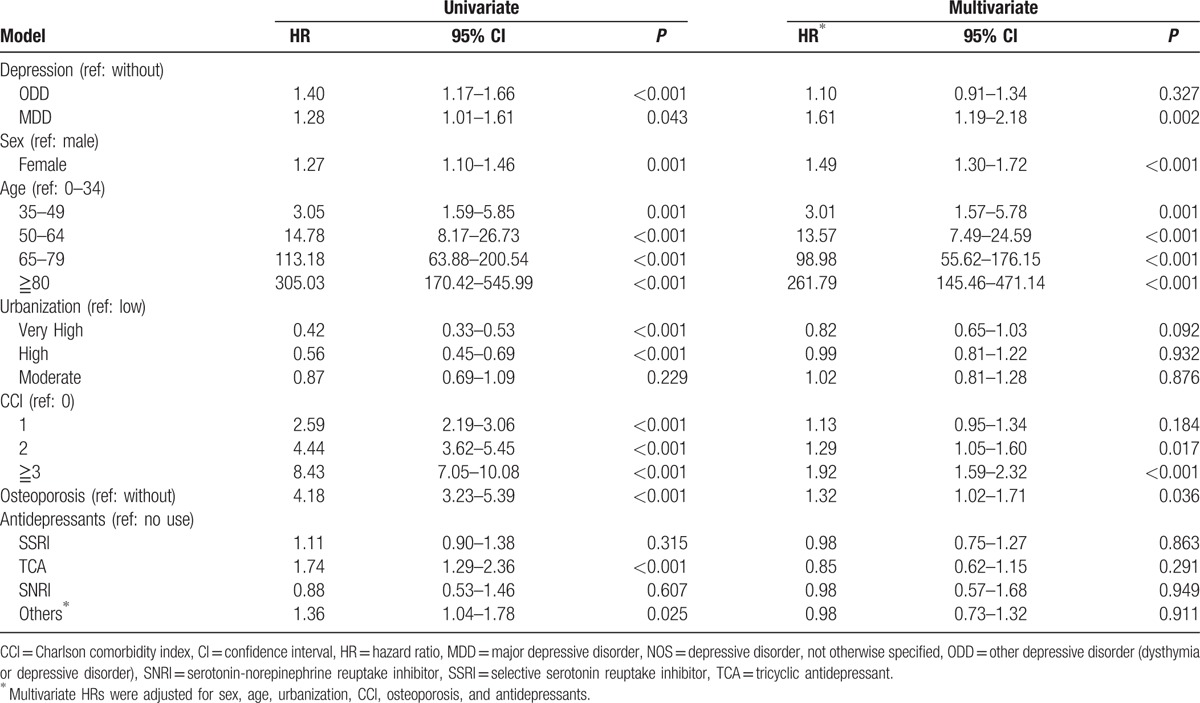
Figure 3.
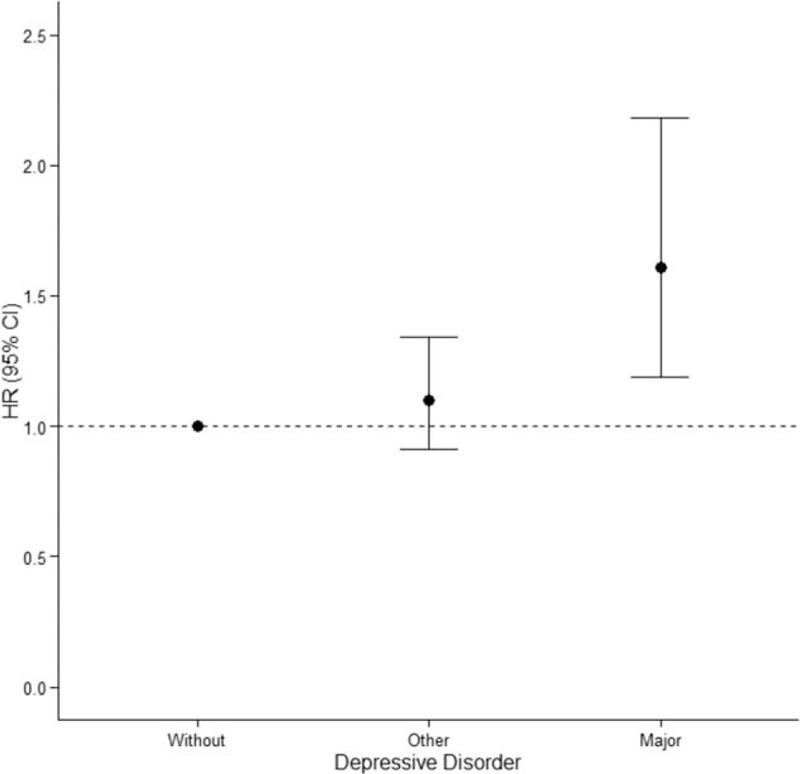
Hazard ratio and 95% confidence interval of patients with no depression (without); dysthymia/depressive disorder, NOS (other); or major depressive disorder (major). Solid circles represent adjusted hazard ratio. Whiskers indicate 95% confidence interval. The multivariate Cox proportional-hazards analysis was performed after adjusting for sex, age, urbanization, CCI, osteoporosis, and antidepressants.
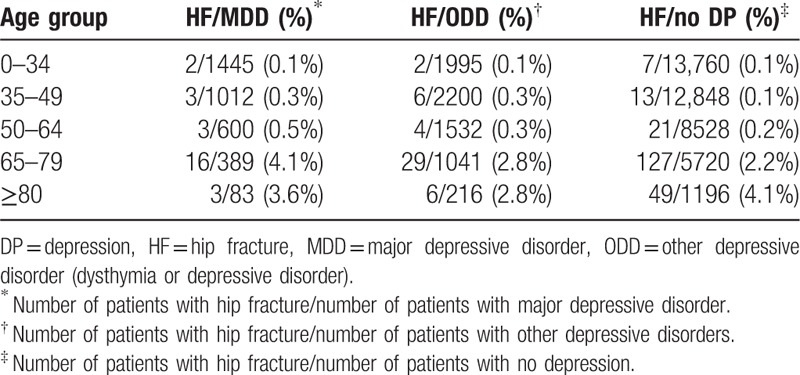
Sex was a risk factor for HF as females had a higher incidence of HF than males (multivariate HR 1.49, 95% CI 1.30–1.72, P < 0.001) (Tables 2–4). Age was also associated with risk of HF as HF rates were increased with age (Tables 2–4). Compared with that of the 0 to 3 age group (HR 1), the multivariate HRs for age groups 35 to 49, 50 to 64, 65 to 79, and >80 were 3.01, 13.57, 98.98, and 261.79, respectively (Table 2).
Table 4.
Number and percentage of males with hip fracture in various age groups of patients with or without depression.
Patients with osteoporosis were found to have a higher risk of HF (multivariate HR 1.32, 95% CI 1.02–1.71, P = 0.036) (Table 2). Urbanization was found to have no effect on HF (Table 2). Patients with a CCI of 2 or greater were found to have a higher incidence of HF (HR 1.29, 95% CI 1.05–1.60, P = 0.017 for CCI = 2; HR 1.92, 95% CI 1.59–2.32, P < 0.001 for CCI ≧3) (Table 2).
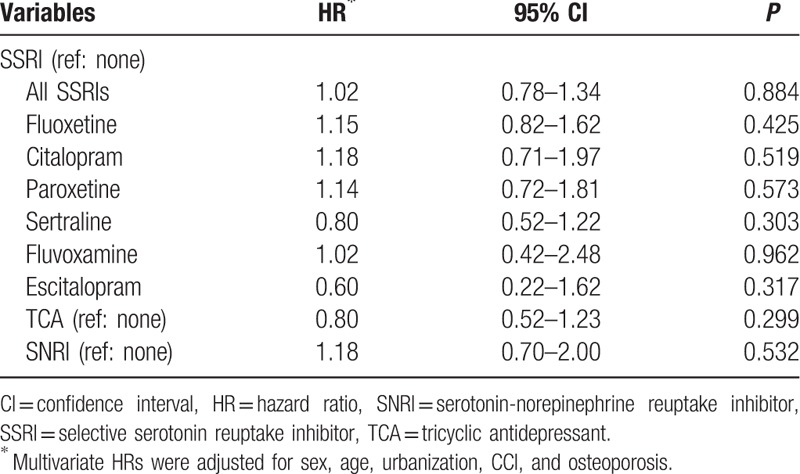
3.3. Effects of antidepressants on hip fracture
The following 4 types of antidepressants were investigated for their effect on HF rates in patients with DP: SSRI, TCA, SNRI, and others (mirtazapine, burpropion, trazodone, and MAOI). Numbers of patients who were on various drugs with different DDDs are shown in Table 5. These drugs were analyzed as a whole on all (139,110) patients (Table 5) and on patients (27,822) with DP (Table 6). SSRI drugs including fluoxetine, citalopram, paroxetine, sertraline, fluvoxamine, and escitalopram were also analyzed individually on the 27,882 patients with DP (Table 6). None of these drugs were found to significantly increase HF rates in patients with DP (Table 6).
Table 5.
Number and per cent of patients with different defined daily dose of various antidepressants∗.
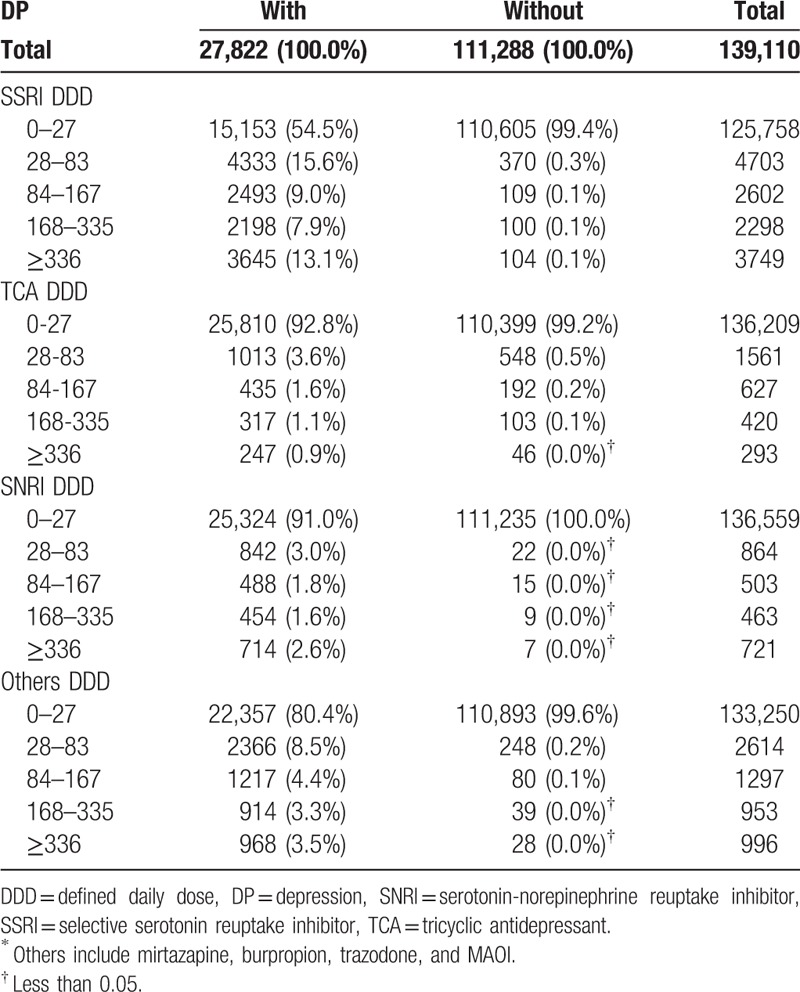
Table 6.
Adjusted hazard ratios of antidepressants on hip fracture.
4. Discussion
The present study is the first population-based study in Taiwan to investigate the relationship between the severity of DP and HF, and effect of antidepressants on HF. Two prospective cohort studies were conducted by analyzing medical records in the NHRI research database of the NHI of Taiwan. In the first study, we investigated the effect of DP on HF. To ensure that the cause-and-effect relationship between DP and HF was determined, we included only patients who had HF 180 days after the diagnosis of DP. In addition, patients with HFs due to cancer or traffic accidents were excluded, and the multivariate Cox proportional-hazards analysis was performed after adjusting for sex, age, urbanization, CCI, osteoporosis, and antidepressants. We found that patients with MDD had a 61% higher incidence of HF than those with no DP (HR 1.61, 95% CI 1.19–2.18) (Table 2 and Fig. 3). This result is highly significant (P = 0.002) and reliable as the CI is relatively narrow. The severity of depressive disorders was correlated with the risk of HF as the HF rate of patients with ODD was not significantly higher than that of patients with no DP (HR 1.10, 95% CI 0.91–1.34, P = 0.327) (Table 2 and Fig. 3). The HF incidence was found to increase with age and CCI scores (Table 2). As expected, osteoporosis was found to be a risk factor of HF (Table 2).
Depression has been shown to decrease BMD.[8,9,12–14,16,35–39] In a population-based prospective cohort study of 2464 community-dwelling men aged 68 years and older, the mean total hip BMD was found to decrease by 0.70% per year in 136 men with a Geriatric Depression Scale (GDS) score of 6 or higher, compared with 0.39% per year in 2328 men with a GDS score less than 6.[16] Similar results were observed in another age-adjusted study of 4177 women aged 69 years and older, in whom the mean total hip BMD was decreased by 0.96% per year in 200 women with a GDS score greater than 6, compared with 0.69% per year in 3977 women with a GDS score less than 6.[35] Another study of 1566 Medicare enrollees aged 65 years and older found that the mean BMD was 40 mg/cm2 lower in those with clinical DP.[14] However, there have also been studies that showed no correlation between DP and low BMD.[11,25,26,28,40]
Patients with DP usually have elevated plasma cortisol that may decrease bone formation and increase resorption, leading to a lower BMD.[41,42] Increased expression of proinflammatory cytokines, such as interleukin (IL)-6 and tumor necrosis factor (TNF)-α, which mediates resorption, has also been observed in patients with DP.[43–45] DP has also been shown to increase addiction to smoking and alcohol consumption, and decrease physical activity.[46] Depressed patients are also more prone to suffer from dietary imbalance or malnutrition, leading to weight loss and development of medical comorbidities that negatively impact BMD. They also have difficulties in taking necessary safety precautions to the environment, and thus have a higher chance of falling, leading to HF.
Our finding that urbanization is not associated with risk of HF in patients with DP is not consistent with that of a meta-study of 15 publications. In that meta-study, rural residents were found to have a 5% higher BMD than urban residents in high-income countries.[47] Another meta-study found that residents in rural regions had a lower incidence of HF compared with urban residents.[48] A study from China found a higher BMD in urban residents[49]; this was postulated to be due to better nutrition. Since the living conditions in rural and urban areas in Taiwan are very similar, it is conceivable that urbanization was found not associated with risk of HF.
In the second prospective cohort study, we investigated HF rates in patients who were on antidepressants with a DDD greater than 28 for more than 180 days. Our results showed that antidepressant medications had no significantly negative impact on HF in patients with DP (Table 2 and Table 4). This result is consistent with that of Diem et al[15] and Ensrud et al.[50] They also found that the use of antidepressants such as SSRI drugs is not associated with an increased risk of HF. Kinjo et al[51] and Spangler et al[28] also found no association between low hip BMD and use of antidepressants. Our findings were similar to those of another recent case-control study in Taiwan by Wang et al.[52] They also did not find an association between the use of SSRI (adjusted OR [aOR] 1.10, 95% CI 0.90–1.24) or SNRI (aOR 1.16, 95% CI 0.95–1.42) drugs and fracture rates, but they found a positive association between combined use of these 2 classes of antidepressants and fracture rates (aOR 1.16, 95% CI 1.05–1.28). This controversial result may be due to their analysis of drug effects based on medication possession ratio (MPR), which was defined as the total prescribing days divided by the total number of follow-up days. Similar to our study, they also found no adverse effects of individual SSRIs such as fluoxetine, sertraline, or paroxetine on fracture. Our results are consistent with those of another recent cohort study in Taiwan by Lee et al[53] in which they found that DP was linked to osteoporosis and that the use of antidepressants lowered the risk of osteoporosis.
Our results regarding the effects of antidepressants on HF differ from some of previous studies from Western countries. These studies showed that antidepressants increased the risk of fracture in patients with DP.[15,35,52,54–66] Epidemiological studies have also linked antidepressants to falls,[67–69] loss of bone density,[70] and fractures.[50,71,72] Antidepressants such as SSRI and TCA drugs have been shown to decrease BMD.[46,73] In a study of a cohort of 2722 older women (mean age 78.5 years), hip BMD was found to decrease by 0.82% in SSRI users compared with 0.47% per year in nonusers.[74] The use of anticonvulsants[51] and glucocorticoids[75,76] have also been associated with low BMD and 25-hydroxyvitamin D levels in patients with DP.[77,78] Therefore, TCA and SSRI drugs are considered as “potentially inappropriate” medications in older adults with a history of falls or fractures in the 2012 American Geriatrics Society Beers Criteria.[79]
Our finding of the lack of adverse effects of antidepressants on HF in patients with DP is probably due to our stringent study design. Since the effect of antidepressants on HF is not immediate, we only examined patients with DP who were on antidepressants with a dose greater than 28 DDD for more than 6 months. Hubbard et al[66] found negative impact of both TCA and SSRI drugs on HF only during the first week of treatment. Another report of similar finding was that of van den Brand et al[55] who found that current use of both SSRIs and TCAs increased hip or femur fracture risk. Arbouw et al[56] also found that current use of dopaminergic drugs (1–30 days before the index date) was associated with an increased risk of hip or femur fractures, but the risk rapidly decreased to baseline levels when treatment was discontinued for more than 1 year. Another reason for the discrepancy in results is that we only examined HF, whereas most of previous studies investigated all fractures.
There were several strengths in our study. We used a large and nationally representative cohort. We determined the relative contribution of both DP and treatment of DP to the incidence of HF. We also explored different classes of antidepressants on HF risk. The cohort study design of our research with a 1:4 case to control match avoided the problem of selection bias. To investigate whether the use of antidepressants increases the risk of HF, we evaluated effects of antidepressants on HF based on DDD not on days of prescription (Table 3), and followed patients up to 12 years (1998–2009). Furthermore, DP in our study was diagnosed by psychiatrists, and not by self-evaluations of patients. A major limitation of our study was that the use of antidepressants was based on prescription records, and not on compliance. This is a common limitation of almost all similar studies as it is very difficult to trace compliance. Another limitation of this study was the lack of information regarding the severity of depressive disorders of patients at the time of fracture. Since the severity of DP is a major confounder in the final outcome, it is not possible to conclude that DP increased HF rates due to apathy, negligence, motor retardation, or adverse effects of antidepressants. As the information on smoking, alcohol consumption, exercise, diet, serum vitamin D levels, and nutrition supplements that may also affect bone health is not in the database, their effects on HF could not be evaluated.
Table 3.
Number and percentage of females with hip fracture in various age groups of patients with or without depression.
Based on the results of this study, we postulate that it is the disease (i.e., DP)—not treatment of the disease—that predisposes patients to HF. Therefore, we propose that Taiwanese patients with MDD should be effectively treated with antidepressants, so that they can become better in managing their food intake, sleep behavior, and physical activities, thus decreasing the chance of falling and incidence of HF.
5. Conclusions
In this study, we found MDD, but not dysthymia or depressive disorder, not otherwise specified, a risk factor for HF. Females and older people had a higher risk of HF. We also found that antidepressants had no effect on HF rates in the Taiwanese population. Since this observation is contrary to those of previous studies in Western countries, additional studies in this regard in the Taiwanese population are needed.
Footnotes
Abbreviations: aOR = adjusted odds ratio, BMD = bone mineral density, CCI = Charlson comorbidity index, CI = confidence interval, DDD = defined daily dose, DP = depression, HF = hip fracture, HR = hazard ratio, ICD = International Classification of Diseases, MAOIs = monoamine oxidase inhibitors, MDD = major depressive disorder, NHI = National Health Insurance, NHRI = National Health Research Institute, ODD = other depressive disorder, SARI = serotonin antagonist and reuptake inhibitor, SNRI = serotonin-norepinephrine reuptake inhibitor, SSRI = selective serotonin reuptake inhibitor, TCA = tricyclic antidepressants.
Funding disclosures: This study was supported by grants CMRGG8D0741 to KEH and COPEG6D0161 to Center of Excellence for Chang Gung Research Data Link from Chang Gung Memorial Hospital, Taiwan.
The authors have no conflicts of interest to disclose.
References
- 1.Rizzoli R, Bruyere O, Cannata-Andia JB, et al. Management of osteoporosis in the elderly. Curr Med Res Opin 2009; 25:2373–2387. [DOI] [PubMed] [Google Scholar]
- 2.Drake MT, Murad MH, Mauck KF, et al. Clinical review. Risk factors for low bone mass-related fractures in men: a systematic review and meta-analysis. J Clin Endocrinol Metab 2012; 97:1861–1870. [DOI] [PubMed] [Google Scholar]
- 3.Bachrach LK. Acquisition of optimal bone mass in childhood and adolescence. Trends Endocrinol Metab 2001; 12:22–28. [DOI] [PubMed] [Google Scholar]
- 4.Unnanuntana A, Rebolledo BJ, Khair MM, et al. Diseases affecting bone quality: beyond osteoporosis. Clin Orthop Relat Res 2011; 469:2194–2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lepine JP, Briley M. The increasing burden of depression. Neuropsychiatr Dis Treat 2011; 7 (suppl 1):3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mojtabai R, Olfson M. National trends in long-term use of antidepressant medications: results from the U.S. National Health and Nutrition Examination Survey. J Clin Psychiatry 2014; 75:169–177. [DOI] [PubMed] [Google Scholar]
- 7.Ilyas S, Moncrieff J. Trends in prescriptions and costs of drugs for mental disorders in England, 1998–2010. Br J Psychiatry 2012; 200:393–398. [DOI] [PubMed] [Google Scholar]
- 8.Schweiger U, Deuschle M, Korner A, et al. Low lumbar bone mineral density in patients with major depression. Am J Psychiatry 1994; 151:1691–1693. [DOI] [PubMed] [Google Scholar]
- 9.Michelson D, Stratakis C, Hill L, et al. Bone mineral density in women with depression. N Engl J Med 1996; 335:1176–1181. [DOI] [PubMed] [Google Scholar]
- 10.Milliken LA, Wilhelmy J, Martin CJ, et al. Depressive symptoms and changes in body weight exert independent and site-specific effects on bone in postmenopausal women exercising for 1 year. J Gerontol A Biol Sci Med Sci 2006; 61:488–494. [DOI] [PubMed] [Google Scholar]
- 11.Whooley MA, Kip KE, Cauley JA, et al. Depression, falls, and risk of fracture in older women. Study of Osteoporotic Fractures Research Group. Arch Intern Med 1999; 159:484–490. [DOI] [PubMed] [Google Scholar]
- 12.Schweiger U, Weber B, Deuschle M, et al. Lumbar bone mineral density in patients with major depression: evidence of increased bone loss at follow-up. Am J Psychiatry 2000; 157:118–120. [DOI] [PubMed] [Google Scholar]
- 13.Halbreich U, Rojansky N, Palter S, et al. Decreased bone mineral density in medicated psychiatric patients. Psychosom Med 1995; 57:485–491. [DOI] [PubMed] [Google Scholar]
- 14.Robbins J, Hirsch C, Whitmer R, et al. The association of bone mineral density and depression in an older population. J Am Geriatr Soc 2001; 49:732–736. [DOI] [PubMed] [Google Scholar]
- 15.Diem SJ, Blackwell TL, Stone KL, et al. Use of antidepressant medications and risk of fracture in older women. Calcif Tissue Int 2011; 88:476–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diem SJ, Harrison SL, Haney E, et al. Depressive symptoms and rates of bone loss at the hip in older men. Osteoporos Int 2013; 24:111–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu Q, Liu J, Gallegos-Orozco JF, et al. Depression, fracture risk, and bone loss: a meta-analysis of cohort studies. Osteoporos Int 2010; 21:1627–1635. [DOI] [PubMed] [Google Scholar]
- 18.Mezuk B, Eaton WW, Golden SH. Depression and osteoporosis: epidemiology and potential mediating pathways. Osteoporos Int 2008; 19:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sogaard AJ, Joakimsen RM, Tverdal A, et al. Long-term mental distress, bone mineral density and non-vertebral fractures. The Tromso Study. Osteoporos Int 2005; 16:887–897. [DOI] [PubMed] [Google Scholar]
- 20.Piirtola M, Vahlberg T, Isoaho R, et al. Predictors of fractures among the aged: a population-based study with 12-year follow-up in a Finnish municipality. Aging Clin Exp Res 2008; 20:242–252. [DOI] [PubMed] [Google Scholar]
- 21.Mussolino ME. Depression and hip fracture risk: the NHANES I epidemiologic follow-up study. Public Health Rep 2005; 120:71–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Forsen L, Meyer HE, Sogaard AJ, et al. Mental distress and risk of hip fracture. Do broken hearts lead to broken bones? J Epidemiol Commun Health 1999; 53:343–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tolea MI, Black SA, Carter-Pokras OD, et al. Depressive symptoms as a risk factor for osteoporosis and fractures in older Mexican American women. Osteoporos Int 2007; 18:315–322. [DOI] [PubMed] [Google Scholar]
- 24.Laudisio A, Marzetti E, Cocchi A, et al. Association of depressive symptoms with bone mineral density in older men: a population-based study. Int J Geriatr Psychiatry 2008; 23:1119–1126. [DOI] [PubMed] [Google Scholar]
- 25.Reginster JY, Deroisy R, Paul I, et al. Depressive vulnerability is not an independent risk factor for osteoporosis in postmenopausal women. Maturitas 1999; 33:133–137. [DOI] [PubMed] [Google Scholar]
- 26.Amsterdam JD, Hooper MB. Bone density measurement in major depression. Prog Neuropsychopharmacol Biol Psychiatry 1998; 22:267–277. [DOI] [PubMed] [Google Scholar]
- 27.Whitson HE, Sanders L, Pieper CF, et al. Depressive symptomatology and fracture risk in community-dwelling older men and women. Aging Clin Exp Res 2008; 20:585–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spangler L, Scholes D, Brunner RL, et al. Depressive symptoms, bone loss, and fractures in postmenopausal women. J Gen Intern Med 2008; 23:567–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hsing AW, Ioannidis JP. Nationwide population science: lessons from the Taiwan National Health Insurance Research Database. JAMA Intern Med 2015; 175:1527–1529. [DOI] [PubMed] [Google Scholar]
- 30.Runeson BS, Rich CL. Diagnostic and statistical manual of mental disorders, 3rd ed. (DSM-III), adaptive functioning in young Swedish suicides. Ann Clin Psychiatry 1994; 6:181–183. [DOI] [PubMed] [Google Scholar]
- 31.Rapaport MH, Judd LL. Minor depressive disorder and subsyndromal depressive symptoms: functional impairment and response to treatment. J Affect Disord 1998; 48:227–232. [DOI] [PubMed] [Google Scholar]
- 32.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40:373–383. [DOI] [PubMed] [Google Scholar]
- 33.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43:1130–1139. [DOI] [PubMed] [Google Scholar]
- 34.Liu CY, Huang YT, Chuang YL, et al. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J Health Manage 2006; 4:1–22. [Google Scholar]
- 35.Diem SJ, Blackwell TL, Stone KL, et al. Depressive symptoms and rates of bone loss at the hip in older women. J Am Geriatr Soc 2007; 55:824–831. [DOI] [PubMed] [Google Scholar]
- 36.Yazici KM, Akinci A, Sutcu A, et al. Bone mineral density in premenopausal women with major depressive disorder. Psychiatry Res 2003; 117:271–275. [DOI] [PubMed] [Google Scholar]
- 37.Kahl KG, Rudolf S, Stoeckelhuber BM, et al. Bone mineral density, markers of bone turnover, and cytokines in young women with borderline personality disorder with and without comorbid major depressive disorder. Am J Psychiatry 2005; 162:168–174. [DOI] [PubMed] [Google Scholar]
- 38.Wong SY, Lau EM, Lynn H, et al. Depression and bone mineral density: is there a relationship in elderly Asian men? Results from Mr. Os (Hong Kong). Osteoporos Int 2005; 16:610–615. [DOI] [PubMed] [Google Scholar]
- 39.Mussolino ME, Jonas BS, Looker AC. Depression and bone mineral density in young adults: results from NHANES III. Psychosom Med 2004; 66:533–537. [DOI] [PubMed] [Google Scholar]
- 40.Whooley MA, Cauley JA, Zmuda JM, et al. Depressive symptoms and bone mineral density in older men. J Geriatr Psychiatry Neurol 2004; 17:88–92. [DOI] [PubMed] [Google Scholar]
- 41.Jilka RL, Hangoc G, Girasole G, et al. Increased osteoclast development after estrogen loss: mediation by interleukin-6. Science 1992; 257:88–91. [DOI] [PubMed] [Google Scholar]
- 42.Nanes MS. Tumor necrosis factor-alpha: molecular and cellular mechanisms in skeletal pathology. Gene 2003; 321:1–15. [DOI] [PubMed] [Google Scholar]
- 43.Dentino AN, Pieper CF, Rao MK, et al. Association of interleukin-6 and other biologic variables with depression in older people living in the community. J Am Geriatr Soc 1999; 47:6–11. [DOI] [PubMed] [Google Scholar]
- 44.Kiecolt-Glaser JK, Glaser R. Depression and immune function: central pathways to morbidity and mortality. J Psychosom Res 2002; 53:873–876. [DOI] [PubMed] [Google Scholar]
- 45.Maes M. Major depression and activation of the inflammatory response system. Adv Exp Med Biol 1999; 461:25–46. [DOI] [PubMed] [Google Scholar]
- 46.Wu Q, Magnus JH, Liu J, et al. Depression and low bone mineral density: a meta-analysis of epidemiologic studies. Osteoporos Int 2009; 20:1309–1320. [DOI] [PubMed] [Google Scholar]
- 47.Matsuzaki M, Pant R, Kulkarni B, et al. Comparison of bone mineral density between urban and rural areas: systematic review and meta-analysis. PLoS One 2015; 10:e0132239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brennan SL, Pasco JA, Urquhart DM, et al. The association between urban or rural locality and hip fracture in community-based adults: a systematic review. J Epidemiol Commun Health 2010; 64:656–665. [DOI] [PubMed] [Google Scholar]
- 49.Gu W, Rennie KL, Lin X, et al. Differences in bone mineral status between urban and rural Chinese men and women. Bone 2007; 41:393–399. [DOI] [PubMed] [Google Scholar]
- 50.Ensrud KE, Blackwell TL, Mangione CM, et al. Central nervous system-active medications and risk for falls in older women. J Am Geriatr Soc 2002; 50:1629–1637. [DOI] [PubMed] [Google Scholar]
- 51.Kinjo M, Setoguchi S, Schneeweiss S, et al. Bone mineral density in subjects using central nervous system-active medications. Am J Med 2005; 118:1414. [DOI] [PubMed] [Google Scholar]
- 52.Wang CY, Fu SH, Wang CL, et al. Serotonergic antidepressant use and the risk of fracture: a population-based nested case-control study. Osteoporos Int 2016; 27:57–63. [DOI] [PubMed] [Google Scholar]
- 53.Lee CW, Liao CH, Lin CL, et al. Increased risk of osteoporosis in patients with depression: a population-based retrospective cohort study. Mayo Clin Proc 2015; 90:63–70. [DOI] [PubMed] [Google Scholar]
- 54.Bolton JM, Metge C, Lix L, et al. Fracture risk from psychotropic medications: a population-based analysis. J Clin Psychopharmacol 2008; 28:384–391. [DOI] [PubMed] [Google Scholar]
- 55.van den Brand MW, Pouwels S, Samson MM, et al. Use of anti-depressants and the risk of fracture of the hip or femur. Osteoporos Int 2009; 20:1705–1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Arbouw ME, Movig KL, van Staa TP, et al. Dopaminergic drugs and the risk of hip or femur fracture: a population-based case-control study. Osteoporos Int 2011; 22:2197–2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gagne JJ, Patrick AR, Mogun H, et al. Antidepressants and fracture risk in older adults: a comparative safety analysis. Clin Pharmacol Ther 2011; 89:880–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Oderda LH, Young JR, Asche CV, et al. Psychotropic-related hip fractures: meta-analysis of first-generation and second-generation antidepressant and antipsychotic drugs. Ann Pharmacother 2012; 46:917–928. [DOI] [PubMed] [Google Scholar]
- 59.Bakken MS, Engeland A, Engesaeter LB, et al. Increased risk of hip fracture among older people using antidepressant drugs: data from the Norwegian Prescription Database and the Norwegian Hip Fracture Registry. Age Ageing 2013; 42:514–520. [DOI] [PubMed] [Google Scholar]
- 60.Moura C, Bernatsky S, Abrahamowicz M, et al. Antidepressant use and 10-year incident fracture risk: the population-based Canadian Multicentre Osteoporosis Study (CaMoS). Osteoporos Int 2014; 25:1473–1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Prieto-Alhambra D, Petri H, Goldenberg JS, et al. Excess risk of hip fractures attributable to the use of antidepressants in five European countries and the USA. Osteoporos Int 2014; 25:847–855. [DOI] [PubMed] [Google Scholar]
- 62.Rossini M, Viapiana O, Adami S, et al. Medication use before and after hip fracture: a population-based cohort and case-control study. Drugs Aging 2014; 31:547–553. [DOI] [PubMed] [Google Scholar]
- 63.Thorell K, Ranstad K, Midlov P, et al. Is use of fall risk-increasing drugs in an elderly population associated with an increased risk of hip fracture, after adjustment for multimorbidity level: a cohort study. BMC Geriatr 2014; 14:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Leach MJ, Pratt NL, Roughead EE. Psychoactive medicine use and the risk of hip fracture in older people: a case-crossover study. Pharmacoepidemiol Drug Saf 2015; 24:576–582. [DOI] [PubMed] [Google Scholar]
- 65.Pacher P, Ungvari Z. Selective serotonin-reuptake inhibitor antidepressants increase the risk of falls and hip fractures in elderly people by inhibiting cardiovascular ion channels. Med Hypotheses 2001; 57:469–471. [DOI] [PubMed] [Google Scholar]
- 66.Hubbard R, Farrington P, Smith C, et al. Exposure to tricyclic and selective serotonin reuptake inhibitor antidepressants and the risk of hip fracture. Am J Epidemiol 2003; 158:77–84. [DOI] [PubMed] [Google Scholar]
- 67.Darowski A, Chambers SA, Chambers DJ. Antidepressants and falls in the elderly. Drugs Aging 2009; 26:381–394. [DOI] [PubMed] [Google Scholar]
- 68.Iaboni A, Flint AJ. The complex interplay of depression and falls in older adults: a clinical review. Am J Geriatr Psychiatry 2013; 21:484–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Thapa PB, Gideon P, Cost TW, et al. Antidepressants and the risk of falls among nursing home residents. N Engl J Med 1998; 339:875–882. [DOI] [PubMed] [Google Scholar]
- 70.Haney EM, Warden SJ, Bliziotes MM. Effects of selective serotonin reuptake inhibitors on bone health in adults: time for recommendations about screening, prevention and management? Bone 2010; 46:13–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu B, Anderson G, Mittmann N, et al. Use of selective serotonin-reuptake inhibitors or tricyclic antidepressants and risk of hip fractures in elderly people. Lancet 1998; 351:1303–1307. [DOI] [PubMed] [Google Scholar]
- 72.Richards JB, Papaioannou A, Adachi JD, et al. Effect of selective serotonin reuptake inhibitors on the risk of fracture. Arch Intern Med 2007; 167:188–194. [DOI] [PubMed] [Google Scholar]
- 73.Takkouche B, Montes-Martinez A, Gill SS, et al. Psychotropic medications and the risk of fracture: a meta-analysis. Drug Saf 2007; 30:171–184. [DOI] [PubMed] [Google Scholar]
- 74.Diem SJ, Blackwell TL, Stone KL, et al. Use of antidepressants and rates of hip bone loss in older women: the study of osteoporotic fractures. Arch Intern Med 2007; 167:1240–1245. [DOI] [PubMed] [Google Scholar]
- 75.Romas E. Bone loss in inflammatory arthritis: mechanisms and therapeutic approaches with bisphosphonates. Best Pract Res Clin Rheumatol 2005; 19:1065–1079. [DOI] [PubMed] [Google Scholar]
- 76.Harpavat M, Keljo DJ, Regueiro MD. Metabolic bone disease in inflammatory bowel disease. J Clin Gastroenterol 2004; 38:218–224. [DOI] [PubMed] [Google Scholar]
- 77.Jorde R, Sneve M, Figenschau Y, et al. Effects of vitamin D supplementation on symptoms of depression in overweight and obese subjects: randomized double blind trial. J Intern Med 2008; 264:599–609. [DOI] [PubMed] [Google Scholar]
- 78.Murphy PK, Wagner CL. Vitamin D and mood disorders among women: an integrative review. J Midwifery Womens Health 2008; 53:440–446. [DOI] [PubMed] [Google Scholar]
- 79.Fick DM, Semla TP. 2012 American Geriatrics Society Beers Criteria: new year, new criteria, new perspective. J Am Geriatr Soc 2012; 60:614–615. [DOI] [PubMed] [Google Scholar]


