Abstract
Neonatal jaundice (NNJ) is one of the most common neonatal disorders worldwide. It is still a main cause of avoidable brain damage, physical and mental impairment, and probable death in newborns.
We aimed to assess perceptions, practices, and traditional beliefs among Egyptian mothers toward NNJ that may contribute to delayed presentation and inappropriate management of hyperbilirubinemia.
This descriptive, cross-sectional study was conducted from January to May 2015. We interviewed 400 Egyptian mothers who gave birth in <1 month before the study using a structured questionnaire. Participants were recruited from outpatients of Cairo University Teaching Hospital.
This study revealed unexpected moderate knowledge and attitude scores of Egyptian mothers in most domains with a mean of 6.6 and 20.6, respectively, although the majority of them were illiterate or had low educational attainment. In terms of knowledge, 52.3% of participants had adequate knowledge about NNJ in the aspects of awareness, risk factors, management, and complications. Almost all participants exhibited moderate (89.8%) and high levels (10%) of positive attitudes toward NNJ. Maternal sociodemographic factors influenced knowledge level, attitudes, and behaviors related to NNJ in Egypt. Working mothers and those residing in urban areas were significantly more knowledgeable (P = 0.023 and 0.021, respectively), and attained higher attitude scores (P < 0.001 and P < 0.001, respectively) than housewives and rural ones. Moreover, significantly higher attitude scores (P < 0.001) were attained by those who had completed their university [22.3 (SD = 3.1)] or postgraduate education [22.2 (SD = 3.6)].
The majority of Egyptian mothers have a satisfactory level of knowledge and attitudes related to NNJ. However, cultural beliefs and traditional infant care practices still have an impact on mothers regardless of their educational level.
Keywords: attitude, Egypt, knowledge, mothers, neonatal jaundice
1. Introduction
Neonatal jaundice (NNJ) is a condition characterized by yellow discoloration of the skin and sclera of newborn infants. It occurs in approximately 50% to 60% of full-term newborn babies and 80% of preterm newborn babies.[1–3] It is a common disorder worldwide and accounts for 75% of hospital readmissions in the first week of life.[3,4] The jaundice is usually due to unconjugated hyperbilirubinemia. It may be benign if its progression to extreme hyperbilirubinemia is recognized, monitored, and prevented or managed in a timely manner.[5] Nevertheless, it can be neurotoxic and cause kernicterus with diffuse neuronal damage or even death in newborns.[6] Surviving infants may acquire long-term neurodevelopmental sequelae such as cerebral palsy, sensorineural hearing loss, intellectual difficulties, or gross developmental delays.[7,8]
The exact blood level above which unconjugated bilirubin will be neurotoxic is unpredictable.[3,9] However, the incidence of kernicterus increases with serum bilirubin levels exceeding 20 mg/dL in normal birth weight babies who are otherwise healthy.[6] Kernicterus is preventable by early recognition and prompt effective therapy of NNJ. At present, once the early stages of hyperbilirubinemic brain damage occur, therapeutic options are limited to the prompt (<8 hours) use of exchange transfusion, hence the imperative for preventive approaches.[5]
Discharge of newborns from the hospital within 48 hours after birth with relatively short postnatal hospital stay make jaundice unapparent to the health care provider at the time of hospital discharge.[4] Moreover, breast-fed infants may receive relatively suboptimal milk supply in the first few days of life which may participate in inadequate fluid and nutritional intake, thereby increasing the incidence of NNJ.[10] Hence, the role of the parents, in early recognition of NNJ and seeking medical care at the right place, is pivotal. Any action of the parents is influenced by their knowledge, perception of, and their attitude toward the condition.
We are not aware of any study that appraised Egyptian mothers’ knowledge, attitude, or behavior on the subject of NNJ. Therefore, we designed our present study to assess perceptions, practices, and traditional beliefs among Egyptian mothers toward NNJ that may contribute to delayed presentation and inappropriate management of severe hyperbilirubinemia.
2. Methods
2.1. Study design and setting
We conducted a prospective, cross-sectional, interview-based study from January to May 2015. Study participants were recruited from outpatients of Cairo University Teaching Hospital, one of the largest tertiary care referral centers all over the country, Africa, Middle East, and the Arab Region. It incorporates 36 departments, 44 specialized units, 5500 beds over 11 hospitals, which serve approximately >2 million patients a year.[11]
Cairo, capital of Egypt, is one of the most densely populated cities in the world. Administratively, Greater Cairo (catchment area) encompasses 3 adjacent governorates: Cairo, Giza, and Qaluibyia.[12] Based on the 2014 Egypt Demographic and Health Survey (EDHS), the total ever-married female population (15–49 years), potential study respondents, was 21.762 million, with 22.4% were inhabitants of Greater Cairo governorate.[13]
2.2. Study population
A purposeful convenience sample was used to recruit a total of 400 Egyptian mothers who gave birth in <1 month before the study. In the current study, the term “mother” was given for first-time mothers and those who already have children. Participants were selected from mothers attending postnatal clinics, neonatal follow-up clinics, and immunization clinics of Center for Social and Preventive Medicine affiliated with the Medical School, Cairo University.
Excluded from the study were as follows: mothers who had mental disorders, those whose babies died or were admitted to neonatal intensive care units, and also those who refused to respond to the survey.
2.3. Study measurement and data collection
The field staff consisted of 2 well-trained house officers, obstetrics and gynecology (OBGYN) physician, field editor, and field supervisor administered a pretested structured interview questionnaire to collect all relevant data from study participants. Before the final survey, a small pilot study was conducted in 45 mothers to assess the performance characteristics and feasibility of the study. The questionnaire was revised by 3 professionals and expertise from the field of public health, OBGYN, and pediatrics with substantial modifications of some contents. The questionnaire was originally in English and translated into Arabic following an established forward–backward translation procedure. To ensure consistency and quality of the collected data, the completed questionnaires were submitted daily to field supervisor and feedback was disseminated before the next day's survey.
The study instrument consisted of 4 sections obtaining information about maternal sociodemographic data, knowledge, attitude, beliefs, and behaviors related to NNJ. One part included 15 close-ended questions, totally 15 scores, concerned with participants’ knowledge about NNJ. A graded question had a correct and incorrect answer. Based on the total score of the correct answers, mothers were categorized as poor knowledge (0–5), moderate knowledge (6–10), and good knowledge (11–15). Also, a 5-point Likert scale (strongly agree/agree/do not have any idea/disagree/strongly disagree)[14,15] was used to assess the participants’ attitudes about NNJ. The attitude scores were graded to poor (0–12), moderate (13–24), and good (25–35).
Ethical clearance was obtained from Institutional Review Board of Faculty of Medicine, Cairo University, before commencement of the study. Only mothers from whom voluntary informed consent was obtained were enrolled for the study.
2.4. Data analysis
Data were prepared in Microsoft Excel 2010 and analyzed with Statistical Package for the Social Science (SPSS) Version 16 (SPSS for Windows, Version 16.0; SPSS Inc, Chicago, IL). Simple frequency tables were used for the qualitative variables, and we calculated simple statistical parameters, such as mean and standard deviation (SD), for the quantitative variables. The differences between proportions were assessed using the P value for heterogeneity. hi-square and Fisher exact tests were used to estimate differences in qualitative variables. A P < 0.05 was considered statistically significant.
3. Results
During the study period, 400 mothers, who gave birth in <1 month before commencing the study, were interviewed using a structured questionnaire. Sociodemographic characteristics of the study participants are shown in Table 1. The maternal mean age was 27 years (SD = 5.8), with the majority of mothers being aged 19 to 34 years (81.25%).
Table 1.
Sociodemographic data of study participants.
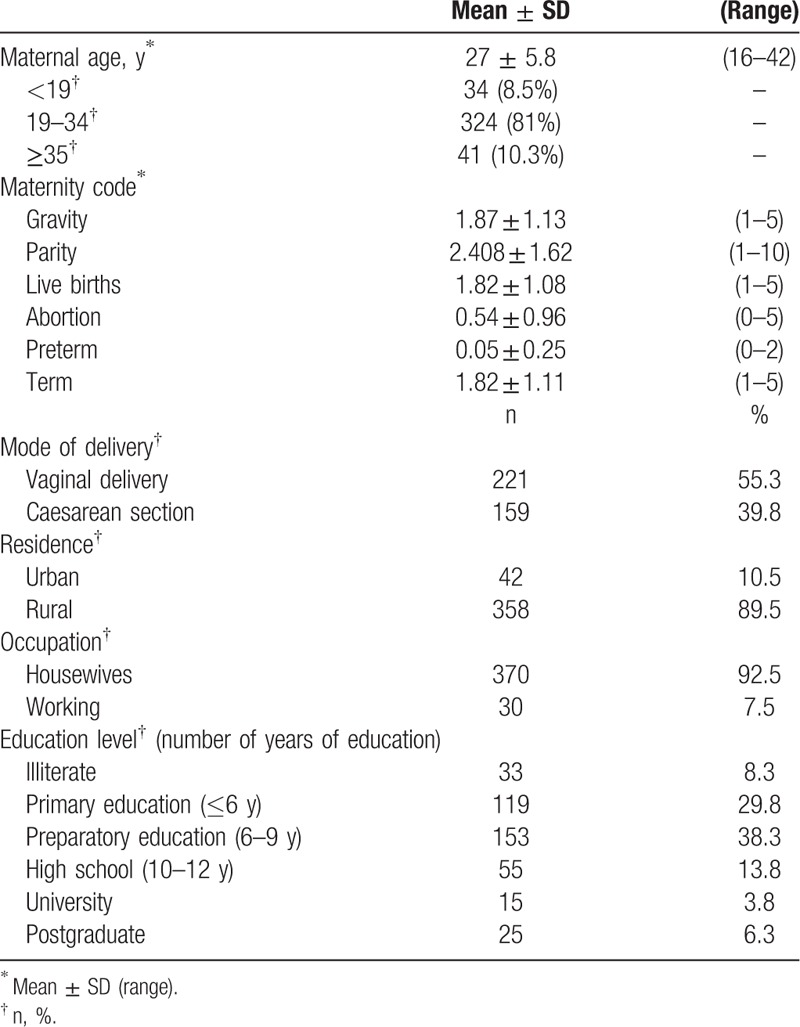
The majority of participants delivered vaginally (59.3%), lived in rural areas (89.5%), had 9 years of full-time education (38.3%), and were housewives (92.5%, n = 370).
Table 2 shows mothers’ experience and perspectives about education of NNJ. Of all 400 participants, 75 had a past history of their infants developing NNJ (18.8%). The group of mothers who received information about NNJ [40%, (n = 160)] comprised all mothers with past experience of jaundiced neonates and those who had no previous experience (n = 85). All participants agreed to be educated about the condition and recognized one-to-one counseling by doctors and antenatal talk sessions as the most favorable methods of health education.
Table 2.
Mothers’ experience and perspectives on education of NNJ.
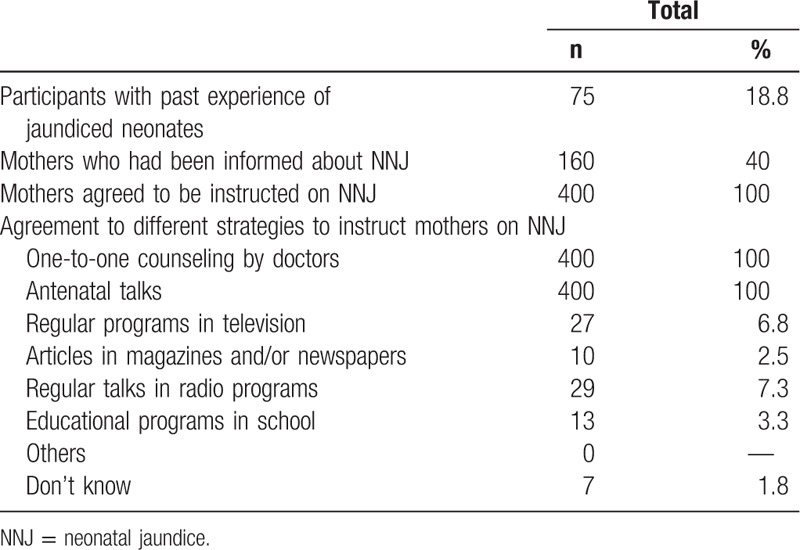
Table 3 shows the results of the assessment of maternal knowledge about NNJ. In terms of basic knowledge, the majority of mothers were able to define NNJ correctly (86%). Yet, only 34% of mothers had considered NNJ > 2 weeks abnormal.
Table 3.
Assessment of maternal knowledge about NNJ.
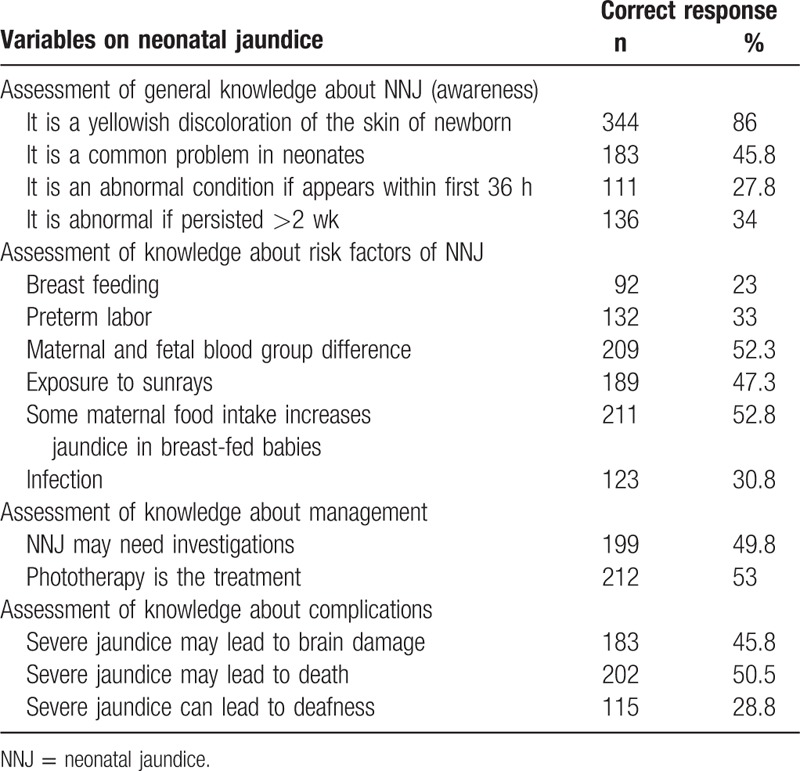
Analysis of maternal perspectives on factors that put infants at risk of NNJ had identified some areas of global concern. Breast feeding, preterm labor, and infection were underestimated as potential risk factors of NNJ, and reported only by 23%, 33%, and 30.8% of mothers, respectively. Approximately half of the participants believed that maternal and fetal blood group difference, some maternal food intake in breast-fed babies, as well as exposure to sunrays, may be risk factors for NNJ (52.3%, 52.8%, and 47.3%, respectively). Almost half of the study participants (n = 212, 53%) exhibited adequate knowledge about phototherapy as the main treatment of hospitalized jaundiced infants. In the same context, sequelae of severe NNJ were adequately recognized among respondents except for deafness (28.8%).
Table 4 shows the results of assessment of maternal practices and beliefs related to NNJ. Approximately half of the mothers combined breast feeding with formula (48%) during the first 3 days after delivery. This percentage increased after the first week of life to involve 77% of the mothers.
Table 4.
Assessment of maternal practices and beliefs related to NNJ.
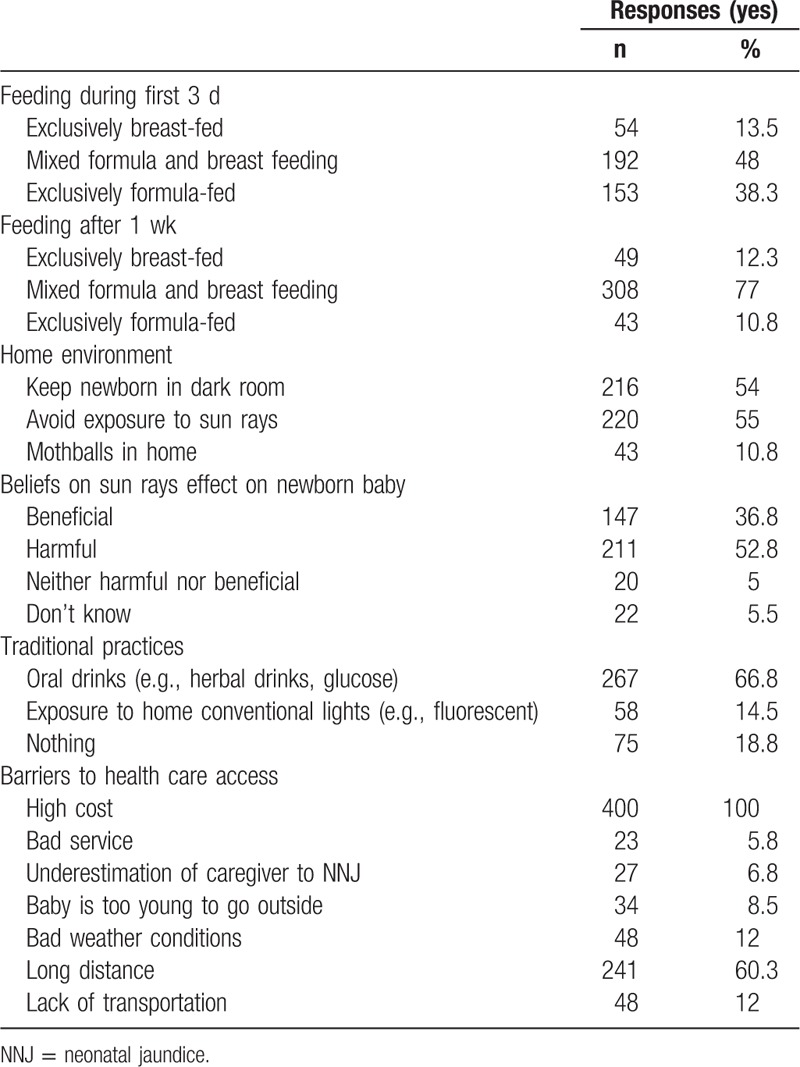
In respect of their beliefs about the benefit of sunlight exposure, 52.8% of mothers deemed that it was harmful for babies; a belief induced 54% of participants to keep infants in a dark room. However, 36.8% (n = 147) emphasized that it was beneficial for NNJ. The traditional practice of giving oral drinks (e.g., herbal drinks and glucose) in case of NNJ was acceptable by approximately two-thirds of our participants (66.8%).
By asking about the possible obstacles that might hinder their access to medical care, all participants were worried about the financial cost of management. Moreover, more than half of them (60.3%, n = 241) believed that distances between their residence and health facilities are long enough to delay proper management of NNJ.
Table 5 shows the different attitudes of the interviewed mothers toward NNJ. More than half of the mothers agreed that NNJ is a worrisome condition (62.3%). On the question whether they consider that investigations of NNJ and frequent blood samples might result in anemia, 66.3% did not agree with that. Meanwhile, only 13.1% (n = 52) gave affirmative answers. In case if jaundice increased, only 25.5% of the participants admitted that they would give herbal drinks as a possible treatment. Nevertheless, all mothers agreed consulting physician if jaundice increased. Of those, approximately two-thirds (62.8%) agreed that it is a serious condition that necessitates early medical consultation. On inquiring about their fear of hospitalization, the majority of mothers (92.8%) gave affirmative answers.
Table 5.
Assessment of maternal attitudes related to NNJ.
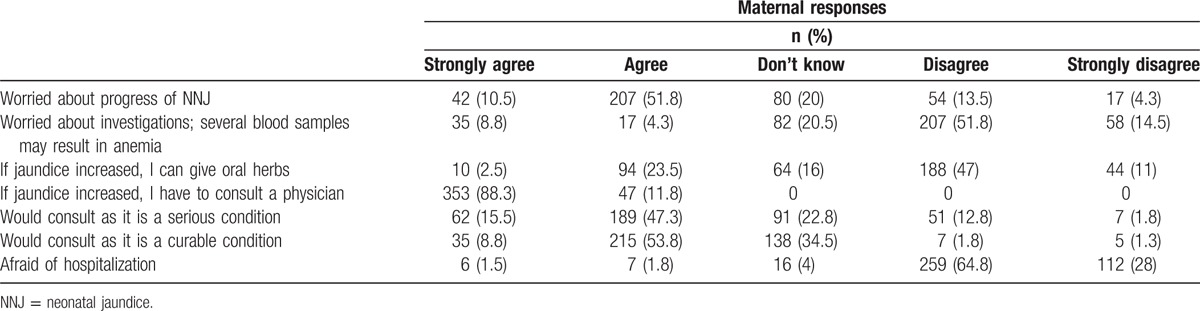
Table 6 shows maternal variables associated with knowledge score. Overall, the total mean knowledge score of participants was 6.6 (SD = 2.8).
Table 6.
Variables associated with maternal knowledge scores related to NNJ.
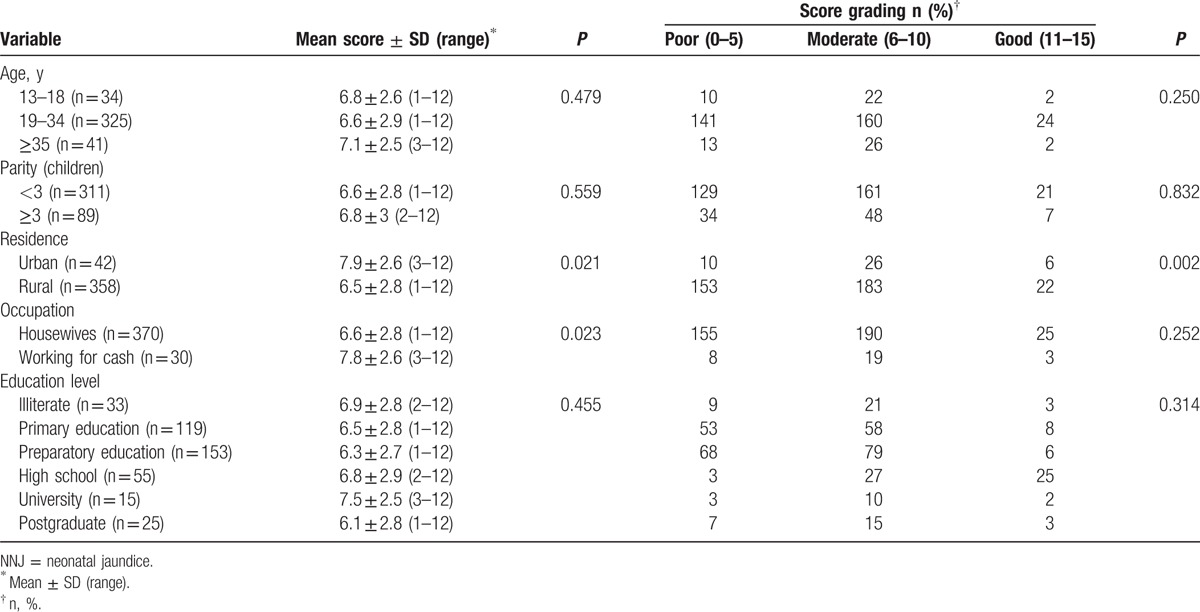
Based on maternal age and education, mothers aged ≥35 years and those who were graduated up to the university level had the highest knowledge score [7.1 (SD = 2.5); 7.5 (SD = 2.5), respectively], despite being statistically nonsignificant. Working mothers and those residing in urban areas were significantly more knowledgeable than housewives and rural ones (P = 0.023 and 0.021, respectively).
Table 7 shows the maternal attitude score in relation to different variables. The total mean attitude score of mothers was 20.6 (SD = 2.8). Similar to knowledge, maternal age and parity had no significant correlation to the attitude score of mothers. However, the highest score was gained by multiparous mothers and those aged ≥ 35 years [20.9 (SD = 2.6), 21.1 (SD = 2.9), respectively]. In addition, mothers residing in rural areas got a significantly lower mean attitude score than those in urban areas [17.4 (SD = 2.7) vs. 22 (SD = 3.5); P < 0.001]. Significantly higher attitude scores (P < 0.001) were attained by working mothers [22.4 (SD = 3.4)] and those who had completed their university [22.3 (SD = 3.1)] or postgraduate education [22.2 (SD = 3.6)].
Table 7.
Variables associated with maternal attitude scores related to NNJ.

4. Discussion
Neonatal severe hyperbilirubinemia represents a significant, yet preventable health problem, particularly in low- and middle-income countries (LMICs).[16,17]
Adequate maternal knowledge, early perception, and care seeking behavior are fundamental components of effective management of NNJ.[18] This study revealed unexpected moderate knowledge and attitude scores of Egyptian mothers in most domains with a mean of 6.6 and 20.6, respectively, although the majority of them were illiterate or had low educational attainment. This may be partly associated with successful implementation of extensive primary care network in Egypt, as well as frequent broadcasting free health messages.[19]
In terms of knowledge, 52.3% of participants had adequate knowledge about NNJ in the aspects of awareness, risk factors, management, and complications. Nonetheless, only 23% and 33% of mothers had addressed breast feeding and preterm labor as risk factors for NNJ, respectively. This warrants adequate antenatal and postnatal dissemination of information on neonatal hyperbilirubinemia to the vast majority of mothers in Egypt. Generally, frequency of correct responses of knowledge related to NNJ was inconsistent across studies conducted in developing world such as Ethiopia (63.5%),[20] Nigeria (57%),[21] Iran (77%),[22] and Turkey (46%).[23] Utilization of different questionnaires, cultural diversity, and traditional beliefs could be factors that might have influenced such difference.
Consistent with previous studies from Nigeria [24] and Sri Lanka, [25] almost all participants exhibited moderate (89.8%) and high levels (10%) of positive attitudes toward NNJ. For example, 88.3% of participants strongly agreed to seek medical care if their babies developed NNJ. A study from Iran[26] reported similar results in perspective of the mean score; however, 63% of their study population had shown higher levels of attitudes. This difference might be attributable to the time lag between the onset of NNJ and seeking medical help, a finding corroborated by other studies.[21,24] This observation is an important reminder that providing education and knowledge is not sufficient itself to change maternal behavior.[27] Thus, more studies are needed to investigate the complexity of influences on maternal health-seeking behaviors in Egypt.
Our study provides insight into maternal sociodemographic factors as determinants of knowledge and attitudes related to NNJ in Egypt. Maternal age, education, working status, parity, and residence had a strong influence on the knowledge level and behavior. Although not statistically significant, we found more accurate knowledge and a relatively safe behavior among mothers with parity of ≥3 and maternal age of ≥35years, a finding replicated in other comparable studies.[18,21,23,28] We also found that working mothers and those residing in urban areas were significantly (P < 0.05) more likely to have perception and attitudes better than housewives and rural mothers. Similar findings were reported in studies conducted in India,[29] Sri Lanka,[25] and Nigeria.[20] A recent Egyptian survey has found that only 49% of women in rural Upper Egypt receiving regular maternal care, compared with 75% in Upper Egypt urban areas.[30] Also, working mothers may acquire more knowledge from participation in the labor market with subsequent interactions with the surrounding community.[31] Several previous studies have found that a high maternal educational level is associated with better outcome of NNJ, which is confirmed by the findings in our study.[24,32]
Consistent with previous work from LMICs,[18,20,32] we reported a substantial number of mothers sustain traditional practices with negative outcomes. For example, only 13.5% of study participants had exclusively breast-fed their infants. A 2008 EDHS found that only 29% of Egyptian infants were exclusively breast-fed.[33] We also found that prelacteal feeding (defined as giving liquids other than breast milk to an infant before mother's milk freely flows)[33] and complementary formula feeding were common during first 3 days after birth.
Although 53% of study participants had identified phototherapy as the standard management of NNJ, many respondents still considered home remedies and exposure to sunlight as initial treatment options. These practices are probably similar in most undeveloped countries from Africa and Asia.[34,35]
At virtually all social classes, mothers have identified information received from health care personnel as the most important intervention the health care system could have offered either through one-to-one counseling or as a part of group antenatal care sessions. Several previous studies have demonstrated significant improvement of maternal knowledge and behavior concerning neonatal care following antenatal visits.[36,37] The health care provider can influence mothers’ attitudes and practices related to NNJ. However, 5.8% of respondents were frustrated with medical personnel due to lack of skills, neglect, or poor medical care. This highlights the need for better handling of patients’ complaints concerning medical staff to identify problems that might interfere with proper utilization of health facilities.[38]
Most of our study participants have acknowledged high cost and limitation of accessibility to health facilities in terms of long distance and lack of transportation as the main barriers to seek medical care services. These findings are consistent with other studies from Egypt and India,[39,40] emphasizing the necessity to put more efforts into overcoming barriers to improve access to health care for mothers and children particularly in rural settings.
5. Implications
Neonatal hyperbilirubinemia has been recognized as a condition which deserves more global health attention.[41] Our study outlined the knowledge, beliefs, attitudes, and practices of Egyptian mothers related to NNJ. Based on our findings, there is a lot to be done in context of health care infrastructures. For example, an implementation of a larger national strategic plan adopting integration of primary health care facilities and social services is required to achieve affordability and sustainability of the health care system.[42] Adequate health education program targeting medical personnel should be applied to ensure delivering quality health services. Also, our data help in understanding how the levels of knowledge and attitudes may correlate with maternal factors such as age, education, and residence. This should be considered in future plans such as effective maternity coverage in rural areas, home visit approach, and mass media campaigns.
6. Limitations
To our best knowledge, this study is the first to investigate maternal knowledge, attitudes, and practice related to NNJ in urban and rural Egyptian communities. Nonetheless, important study limitations should be addressed. First, the nature of voluntary participation in our survey is subject to selection bias. Participants who had infants with NNJ might be more concerned with answering questions about them. Second, we used hospital-based study and thus may limit the representation of the maternal extent of knowledge, attitudes, and practice related to NNJ in the general population. Third, we were restricted in our ability to evaluate all of the factors known to influence awareness, beliefs, and behavior of mothers toward NNJ such as number of antenatal care visits, and socioeconomic factors including household income, and fathers’ education level. In the context of the Egyptian society, such socioeconomic factors could not be assessed because the culture and traditions of the Egyptians, particularly in rural communities, mean they are conservative in providing such information. Finally, the study was conducted on a relatively small scale in purposively one selected governorate, which might limit generalizability of our results.
7. Conclusion
In conclusion, the majority of Egyptian mothers have a satisfactory level of knowledge and attitudes related to NNJ. However, cultural beliefs and traditional infant care practices still have an impact on mothers regardless of their educational level. Health care providers serve as the cornerstone in maternal and infant health promotion. All these factors should be taken into consideration while planning national maternal and child health education program.
Acknowledgments
The authors thank Dr Adel Shabayek, Obstetrics and Gynecology Department, Dr Asma Mohamed Moawad, Dr Hosam Ibraheim, Pediatric Department, Public Health Department, and all house officers, Faculty of Medicine, Cairo University, for their valuable contribution to this study.
Footnotes
Abbreviations: EDHS = Egypt Demographic and Health Survey, LMICs = low- and middle-income countries, NNJ = neonatal jaundice, OBGYN = obstetrics and gynecology, SD = standard deviation, SPSS = Statistical Package for the Social Science.
Authorship: EMIM—substantial contributions to the conception and design of the work, analysis, and interpretation of data for the work; drafting the work; and carried out the statistical analysis. EAAA—substantial contributions to the conception and design of the work, analysis, and interpretation of data for the work; drafting the work. YZAA—substantial contributions to the design of the work; revising it critically for important intellectual content. All authors read and approved the final manuscript, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: This research received no specific grant from any funding agency in the public, commercial, and not-for-profit sectors.
Disclosure: The authors have no conflicts of interest to disclose.
References
- 1.Ip S, Chung M, Kulig J, et al. An evidence-based review of important issues concerning neonatal hyperbilirubinemia. American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Pediatrics 2004; 114:e130–e153. [DOI] [PubMed] [Google Scholar]
- 2.Behrman RE, Kliegman RM, Jenson HB. Nelson Textbook of Pediatrics. 16 th edPhiladelphia, PA: Saunders; 2005. 511–528. [Google Scholar]
- 3.Ogunfowora OB, Adefuye PO, Fetuga MB. What do expectant mothers know about neonatal jaundice? Int Electron J Health Educ 2006; 9:134–140. [Google Scholar]
- 4.Melton K, Akinbi HT. Neonatal jaundice. Strategies to reduce bilirubin-induced complications. Postgrad Med 1999; 106:167–178. [DOI] [PubMed] [Google Scholar]
- 5.Bhutani VK, Zipursky A, Blencowe H, et al. Neonatal hyperbilirubinemia and Rhesus disease of the newborn: incidence and impairment estimates for 2010 at regional and global levels. Pediatr Res 2013; 74 (S1):86–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics. Provisional Committee for Quality Improvement and Subcommittee on Hyperbilirubinemia. Practice Parameter: Management of hyperbilirubinemia in the healthy term newborn. Pediatrics 1994; 94:558–565. [PubMed] [Google Scholar]
- 7.Mwaniki MK, Atieno M, Lawn JE, et al. Long-term neurodevelopmental outcomes after intrauterine and neonatal insults: a systematic review. Lancet 2012; 379:445–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maulik PK, Darmstadt GL. Childhood disability in low-and middle-income countries: overview of screening, prevention, services, legislation, and epidemiology. Pediatrics 2007; 120 (suppl 1):S1–S55. [DOI] [PubMed] [Google Scholar]
- 9.Zupan J. Prenatal mortality in developing countries. N Engl J Med 2005; 352:2047–2048. [DOI] [PubMed] [Google Scholar]
- 10.Blackmon LR, Fanaroff AA, Raju NK. National Institute of Child Health and Human Development. National Institute of Child Health and Human Development. Research on prevention of bilirubin-induced brain Injury and kernicterus: National Institute of Child Health and Human Development conference executive summary 2003. Pediatrics 2004; 114:229–233. [DOI] [PubMed] [Google Scholar]
- 11.El Dib NA. Kasr Al Ainy, the story of a palace that became a medical school. KAMJ 2015; 21:1–7. [Google Scholar]
- 12.Aly MH, Zebker HA, Giardino JR, et al. Permanent Scatterer investigation of land subsidence in Greater Cairo, Egypt. Geophys J Int 2009; 178:1238–1245. [Google Scholar]
- 13.Ministry of Health and Population [Egypt], El-Zanaty and Associates [Egypt], ICF International. Egypt Demographic and Health Survey 2014. Cairo and Rockville, MD: Ministry of Health and Population and ICF International; 2015. [Google Scholar]
- 14.Likert R. A technique for the measurement of attitudes. Arch Psychol 1932; 22:140–155. [Google Scholar]
- 15.Allen IE, Seaman CA. Likert scales and data analyses. Quality progress 2007; 40:64. [Google Scholar]
- 16.Rennie J, Burman-Roy S, Murphy MS. Guideline Development Group. Neonatal jaundice: summary of NICE guidance. BMJ 2010; 340:c2409. [DOI] [PubMed] [Google Scholar]
- 17.Olusanya BO, Emokpae AA, Zamora TG, et al. Addressing the burden of neonatal hyperbilirubinaemia in countries with significant glucose-6-phosphate dehydrogenase deficiency. Acta Paediatr 2014; 103:1102–1109. [DOI] [PubMed] [Google Scholar]
- 18.Ezeaka CV, Ugwu RO, Mukhtar-Yola M, et al. Pattern and predictors of maternal care-seeking practices for severe neonatal jaundice in Nigeria: a multi-centre survey. BMC Health Serv Res 2014; 14:192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. Country Cooperation Strategy for WHO and Egypt 2010–2014. WHO Regional Office for the Eastern Mediterranean, Cairo. www.emro.who. [Google Scholar]
- 20.Adebami OJ. Appraisal of maternal knowledge of neonatal jaundice in Ilesa, Southwestern Nigeria: what implications for persistence of acute bilirubin encephalopathy in developing countries. Basic Res J Med Clin Sci 2015; 4:156–163. [Google Scholar]
- 21.Ogunlesi TA, Abdul AR. Maternal knowledge and care. Seeking behaviors for newborn jaundice in Sagamu, Southwest Nigeria. Niger J Clin Pract 2015; 18:33–40. [DOI] [PubMed] [Google Scholar]
- 22.Amirshaghaghi A, Ghabili K, Shoja MM, et al. Neonatal jaundice: knowledge and practice of Iranian mothers with icteric newborns. Pak J Biol Sci 2008; 11:942–945. [DOI] [PubMed] [Google Scholar]
- 23.Sutcuoglu S, Dursun S, Halicioglu O, et al. Evaluation of maternal knowledge level about neonatal jaundice. J Matern Fetal Neonatal Med 2012; 25:1387–1389. [DOI] [PubMed] [Google Scholar]
- 24.Goodman OO, Kehinde OA, Odugbemi BA, et al. Neonatal jaundice: knowledge, attitude and practices of mothers in Mosan-Okunola community, Lagos, Nigeria. Niger Postgrad Med J 2015; 22:158–163. [DOI] [PubMed] [Google Scholar]
- 25.Rodrigo BK, Cooray G. The knowledge, attitude & behaviour on neonatal jaundice of postnatal mothers in Provincial General Hospital, Badulla. Sri Lanka J Child Health 2011; 40:164–168. [Google Scholar]
- 26.Rabiyeepoor1 S, Gheibi S, Jafari S. To study the knowledge and attitude of postnatal mothers on neonatal jaundice in Motahari Hospital, Iran. J Clin Med Res 2014; 3:1–5. [Google Scholar]
- 27.Mackian S, Bedri N, Lovel H. Up the garden path and over the edge: where might health-seeking behaviour take us? Health Policy Plan 2004; 19:137–146. [DOI] [PubMed] [Google Scholar]
- 28.Egube BA, Ofili AN, Isara AR, et al. Neonatal jaundice and its management: knowledge, attitude, and practice among expectant mothers attending antenatal clinic at University of Benin Teaching Hospital, Benin City, Nigeria. Niger J Clin Pract 2013; 16:188–194. [DOI] [PubMed] [Google Scholar]
- 29.Rama R, Gopalakrishnan S, Udayshankar PM. Assessment of knowledge regarding new-born care among mothers in Kancheepuram district, Tamil Nadu. Int J Community Med Public Health 2014; 1:58–63. [Google Scholar]
- 30.Chaaban J. Youth and development in the Arab countries: The need for a different approach. Middle Eastern Stud 2009; 45:33–55. [Google Scholar]
- 31.Knudsen K, Wærness K. National context, individual characteristics and attitudes on mothers’ employment: a comparative analysis of Great Britain, Sweden and Norway. Acta Sociologica 2001; 44:67–79. [Google Scholar]
- 32.Le LT, Partridge JC, Tran BH, et al. Care practices and traditional beliefs related to neonatal jaundice in northern Vietnam: a population-based, cross-sectional descriptive study. BMC Pediatr 2014; 14:264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.El-Zanaty F, Way A. Egypt Demographic and Health Survey. Cairo: Ministry of Health and Macro International; 2008. [Google Scholar]
- 34.Boo NY, Gan CY, Gian YW, et al. Malaysian mothers’ knowledge & practices on care of neonatal jaundice. Med J Malaysia 2011; 66:239–243. [PubMed] [Google Scholar]
- 35.Aziz NA, Lee K. Malaysian primipara's knowledge and practice on newborn care during the postnatal period. Int J Public Health Clin Sci 2014; 1:132–143. [Google Scholar]
- 36.Weiner EA, Billamay S, Partridge JC, et al. Antenatal education for expectant mothers results in sustained improvement in knowledge of newborn care. J Perinatol 2011; 31:92–97. [DOI] [PubMed] [Google Scholar]
- 37.Dongre AR, Deshmukh PR, Garg BS. A community based approach to improve health care seeking for newborn danger signs in rural Wardha, India. Indian J Pediatr 2009; 76:45–50. [DOI] [PubMed] [Google Scholar]
- 38.Reader TW, Gillespie A, Roberts J. Patient complaints in healthcare systems: a systematic review and coding taxonomy. BMJ Qual Saf 2014; 23:678–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chiang C, Labeeb SA, Higuchi M, et al. Barriers to the use of basic health services among women in rural southern Egypt (Upper Egypt). Nagoya J Med Sci 2013; 75:225–231. [PMC free article] [PubMed] [Google Scholar]
- 40.Singh PK, Rai RK, Alagarajan M, et al. Determinants of maternity care services utilization among married adolescents in rural India. PloS One 2012; 7:e31666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Olusanya BO, Osibanjo FB, Slusher TM. Risk factors for severe neonatal hyperbilirubinemia in low- and middle-income countries: systematic review and meta-analysis. PloS One 2015; 10:e0117229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Valentijn PP, Ruwaard D, Vrijhoef HJ, et al. Collaboration processes and perceived effectiveness of integrated care projects in primary care: a longitudinal mixed-methods study. BMC Health Serv Res 2015; 15:463. [DOI] [PMC free article] [PubMed] [Google Scholar]


