Abstract
Background
Anxiety and depression have each been independently associated with impairments in emotional face recognition. However, little is known about the nature of these impairments when anxiety and depression co-occur.
Methods
This post-hoc analysis evaluated the relationship between anxiety status and performance on the Emotional Expression Multimorph Task within a clinical sample of individuals with major depressive disorder (MDD).
Results
Participants with anxious depression (n=14) and nonanxious depression (n=14) completed the Emotional Expression Multimorph Task. Those with anxious depression required greater intensity of emotion to identify both happy (p=.01) and sad (p=.04) facial expressions than those with nonanxious depression. Severity of anxiety also correlated with greater intensity of emotion required to detect sad faces. Contrary to prediction, hypervigilance to angry and fearful facial expressions was not observed in anxious depression.
Limitations
The present study did not include an anxiety-only group for comparison, and did not assess state anxiety at time of administration. In addition, the extent to which the experimental task correlates with social functioning is not fully understood.
Conclusions
These findings suggest a diminished sensitivity to happy and sad facial expressions specific to anxious depression, but not a hypervigilance toward threatening facial expressions. Further research on the nature of emotion recognition in anxiety and depression may inform improved clinical interventions.
Keywords: anxious depression, anxiety, emotional expressions, emotion recognition
1. Introduction
Anxious depression is a clinically significant subtype of major depressive disorder (MDD) [1-3]. Analyses of a large sample of outpatients with MDD from the Sequenced Treatment Alternatives to Relieve Depression project (STAR*D [1]) defined anxious depression as MDD with co-occurring anxiety symptoms as measured by anxiety-somatization items on the Hamilton Depression Rating Scale (HAM-D [4]). Working from this definition, the STAR-D analyses found: 1) that about half of individuals with MDD have anxious depression, and 2) that anxious depression is associated with a unique demographic and clinical profile, comprising higher unemployment, lower levels of education, more melancholic features, greater severity of illness, and greater suicidal ideation than nonanxious depression [1-3]. Anxious depression is also characterized by poorer response to both psychopharmacologic and cognitive-behavioral treatment [5, 6]. Given the differences in clinical outcomes between anxious and nonanxious depression, and given the central role of emotion processing in both anxiety and depression, investigations into this area may lead to improved treatment strategies for both anxious and nonanxious depression.
Evidence suggests that individuals with MDD may have certain deficits in emotion processing—particularly in recognizing emotional facial expressions—but findings are mixed regarding the specific nature of these deficits. A recent meta-analysis of emotional face recognition in depression found evidence that individuals with MDD may: 1) attribute more sadness to positive or ambiguous facial expressions than controls, and 2) be less accurate than controls when recognizing both sad and happy facial expressions [7]. However, findings in this area vary considerably. For example, Rubinow and Post (1992) found that individuals with MDD had diminished accuracy for both happy and sad facial expressions [8]. Similarly, Gur and colleagues (1992) found that depressed individuals were more likely to misinterpret happy faces as neutral, more likely to misinterpret neutral faces as sad, and less able to recognize ambiguously sad faces than controls [9]. Furthermore, Leppanen and colleagues (2004) found that depressed participants did not differ from controls in accuracy when recognizing happy and sad faces, but were less accurate than controls when recognizing neutral faces, misattributing both sadness and happiness to neutral faces [10]. The use of multiple paradigms to assess emotion recognition may have contributed to the mixed nature of these findings [7]. For example, participants in one study selected one of seven “key” faces representing emotions [8], in another study they selected a numerical value on a scale from very happy to very sad [9], and in another study they selected a verbal label of happy, sad, or neutral [10]. The duration of stimulus presentation also varied, ranging from 200 [10] to 7,000 milliseconds [9]. These methodological differences across the current literature suggest that further research is necessary to investigate emotion recognition deficits in MDD.
A more recent method of assessing emotion recognition involves the use of dynamic photographic facial stimuli (i.e., faces that morph from a neutral to an emotional expression, or from one emotional expression to another), which captures the point at which viewers first recognize an emotion as it emerges. The use of dynamic, rather than static, facial stimuli is thought to be more precise because it yields information about both accuracy (correct or incorrect response) and sensitivity (intensity of emotion required) of recognition [11]. However, studies using dynamic facial stimuli to assess emotion recognition in MDD have also yielded mixed findings. In two such studies, individuals with MDD required a greater intensity of emotion than controls to correctly identify happy (but not sad) expressions [12, 13]. In contrast, Schaefer and colleagues (2010) used a similar dynamic stimulus paradigm and, surprisingly, found no differences in task performance for either happy or sad facial expressions between individuals with MDD and healthy controls [14]. The mixed evidence for emotion recognition biases in depression suggests that the role of specific correlates of MDD, such as anxiety symptoms, may warrant closer investigation. Indeed, despite the common co-occurrence of depression and anxiety, and the maladaptive patterns of emotion recognition associated with each of these separate conditions, little is known about emotion recognition in individuals for whom depression and anxiety co-occur.
Although only a few studies have examined the role of anxiety symptoms in emotion recognition for individuals with MDD, initial evidence suggests that these symptoms may play a role in the negative recognition bias associated with depression. Bouhuys and colleagues (1997) found that increased anxiety in a depressed sample was associated with greater perception of negative emotions when viewing ambiguous facial stimuli [15]. Similarly, Suslow and colleagues (2004) found that individuals with MDD and a comorbid anxiety disorder were slower to respond to positive faces during a face-in-the-crowd task than those without comorbid anxiety, further suggesting diminished reactivity toward positive facial expressions [16]. Furthermore, when anxiety occurs outside the context of depression, it is robustly characterized by heightened vigilance towards threatening faces. For example, compared to healthy controls, individuals with anxiety disorders more often identify neutral or ambiguous facial expressions as negative and/or angry [17], recognize fearful faces more easily [18], and display an attentional bias towards fearful and angry faces [19, 20]. Anxious individuals also require less intensity of emotion than controls to recognize angry expressions [12]. Notably, the studies above that investigated anxiety in MDD samples assessed perception of negative emotions, but did not distinguish fearful and angry expressions from sad expressions [15, 16]. Under these circumstances, more detailed investigation into the recognition of happy, sad, angry, or fearful expressions may help clarify the role of anxiety in emotion recognition for individuals with MDD.
The present study sought to specify the extent to which emotion recognition, as measured by the Emotional Expression Multimorph Task [21], differs between individuals with anxious compared to nonanxious depression. This is a post-hoc analysis of data from a previously analyzed sample [14] that found no significant difference in emotion recognition patterns between MDD participants and healthy controls. In the present study, the MDD group was divided into anxious and nonanxious groups in order to delineate the role of anxiety in emotion recognition.
We hypothesized that compared to the nonanxious group, the group with anxious depression would require less intensity of emotion to recognize angry and fearful faces (which would suggest that this group displays the hypervigilance to threatening stimuli associated with anxiety). We also hypothesized that the group with anxious depression would require more intensity of emotion to recognize happy and sad faces (which would suggest that the diminished sensitivity to subtle happy and sad expressions associated with depression may specifically be associated with anxiety symptoms in MDD). In addition, we hypothesized that severity of anxiety would positively correlate with intensity of emotion required for happy and sad faces and negatively correlate with intensity of emotion required for angry and fearful faces. Assuming differences in anxiety groups, we sought to determine the extent to which either of the depression groups differed from healthy controls. Thus, we hypothesized that only the group with anxious depression would differ substantially from healthy controls.
2. Material and Methods
2.1. Participants
Adults with MDD (n=28) were recruited from ongoing studies in a clinical research setting. These participants met DSM-IV criteria for MDD, as determined by the Structured Clinical Interview for Axis I DSM-IV Disorders – Patient Version (SCID-P [22]), and were free from psychiatric medication for at least two weeks (at least five weeks for fluoxetine) before participation. These participants were also treatment-resistant; that is, they had not responded fully to at least two trials of antidepressant medications.
Healthy participants underwent a screening that included medical history and a physical exam as well as a Structured Clinical Interview for DSM-IV, non-patient version (SCID-NP [22]), in order to confirm that they were free from current or past psychiatric or neurological illness, family history of psychiatric illness, or medical conditions that could affect cognitive performance. All participants were free of acute medical illnesses, current psychotic features, and substance abuse or dependence in the three months prior to participation. The present sample is a subsample of that analyzed by Schaefer and colleagues [14] comprising all healthy control participants and all MDD participants for whom Hamilton Depression Rating Scale (HAM-D [4]) scores were available. The study was approved by the institutional review board (IRB) of the NIMH. All participants gave written informed consent after receiving a detailed explanation of the task procedure.
2.2. Measures
The HAM-D [4], a 17-item clinician-administered scale used to assess severity of depression, was administered to participants with MDD. The anxiety-somatization scale of the HAM-D is derived from a factor analysis and comprises six items: psychic anxiety, somatic anxiety, gastrointestinal somatic symptoms, general somatic symptoms, hypochondriasis, and insight [23]. Anxious depression was defined by a HAM-D anxiety-somatization score ≥ 7, a cutoff score consistent with prior studies [24]. Severity of depression was determined using the sum of the HAM-D items, excluding the six anxiety-somatization factor items. The Matrix Reasoning and Vocabulary subtests of the Wechsler Abbreviated Scale of Intelligence (WASI [25]) were also administered to obtain full-scale IQ (FSIQ-2), an estimate of general cognitive ability.
2.3. Emotional Expression Multimorph Task
The Emotional Expression Multimorph Task is a dynamic stimulus paradigm developed to increase precision in measuring emotion recognition [21]. In this task, participants viewed faces that morphed from a neutral to an emotional expression and were asked to indicate the earliest stage at which they could recognize an emotion. Earlier responses represent better recognition, since an earlier response indicates that the viewer required less intensity of emotion to identify an expression.
2.4. Procedures
As described elsewhere [14], participants completed the Emotional Expression Multimorph Task [21] in which emotional facial stimuli and labels representing six emotions (happy, sad, angry, fearful, surprised, or disgusted; labels displayed in randomized order) were displayed on a computer screen. Each face was presented as a series of 39 stages displayed for 100ms each in order of increasing emotional expression so that the face appeared to be morphing from a neutral expression (0%) to full emotional intensity (100%). Images of three male and three female faces taken from Ekman and Friesen's Pictures of Facial Affect [26] displayed one of six emotional expressions—happy, sad, angry, disgusted, surprised, or fearful—in random order for a total of 36 trials.
During each stimulus presentation, participants were asked to inform the administrator as soon as they recognized the emotion being expressed. The administrator pressed a “stop” button that stopped the face, and the subject selected one of the six emotions displayed on the screen. The face then continued to morph through the remaining stages, during which time participants could ask the administrator to stop the face again in order to change their response at any point. When the face reached 100% intensity, participants were asked to verify their response by selecting the emotion again.
2.5. Statistical Analysis
Group comparisons of clinical and demographic information between the groups with anxious and nonanxious depression used t-tests for continuous variables (age, FSIQ-2, age of onset, severity of depression, and anxiety-somatization score) and chi-square tests for categorical variables (sex). Group comparisons of age, FSIQ-2, and sex were repeated to include the healthy control group using one-way ANOVAs.
The primary dependent variable was response point, or the stage at which a participant correctly identified an emotion. Stages were ordered from 39 (0% of an emotion) to 1 (100% of an emotion). Thus, response to a given stimulus at stage 25 would result in a response point of 25; a lower response point would indicate later recognition, and no response would result in a response point of zero. In a previous analysis of these data, Schaefer and colleagues [14] used three methods of analysis: coding final incorrect responses as no response, using first response regardless of accuracy, and coding final incorrect responses as missing. These methods did not substantially alter the results of that analysis. Thus, in the present analysis the response point was coded as no response for incorrect responses. That is, if an incorrect response was made at stage 25 and corrected at stage 16, the response point for that trial would be 16. If an incorrect response was made at stage 25 and not corrected, or if no response was ever made, response point for that trial would be zero. Accuracy of response was a secondary dependent variable.
Our primary hypothesis was that the anxious depression group would differ from the nonanxious depression group on task performance. To test this, a full factorial linear mixed model with a compound symmetry covariance structure and restricted maximum likelihood estimation was conducted to examine group differences in response point. A similar mixed model was conducted for accuracy; we also calculated mean accuracy for each emotion across the two MDD groups (anxious depression vs nonanxious depression). Group (identified as anxious or nonanxious) was a fixed between-participants factor in the models. Emotion (happy, sad, surprised, angry, disgusted, or fearful) and trial number within each emotion (1 through 6, to account for potential order effects) were included as fixed within-participants factors. A fixed intercept was also included in the models. The models investigated main effects of group, emotion, and trial, as well as interactions among these variables. Bonferroni-adjusted post-hoc tests were used following significant effects. Partial η2 was used to calculate effect size following significant effects.
To examine the effect of anxiety as a continuous variable on response point, a linear mixed model was conducted on a combined group of all depressed participants, with emotion and trial as fixed between-participants factors and anxiety score as a covariate. A similar mixed model was conducted for accuracy. Pearson correlations were calculated following significant effects. Due to the post-hoc and confirmatory nature of these correlations, we did not correct for multiple comparisons.
A secondary hypothesis was that the anxious depression group, but not the nonanxious depression group, would differ from healthy control subjects. To examine the effects of the groups with anxious and nonanxious depression compared to healthy controls, we added controls to the initial mixed model and used Fisher's LSD to make a priori comparisons between each patient group and the control group for each emotion. The full results of this model are reported to be clear about the general outcomes of this model. All statistical analyses were conducted using IBM SPSS version 22. Significance was considered at p < .05, two-tailed.
3. Results
3.1. Demographic and symptom information
Of the 28 individuals with MDD who participated in this study, 14 were classified as anxious and 14 as nonanxious according to HAM-D anxiety-somatization score. The depressed sample was 64% male, and the mean age was 44.45 (SD = 13.20). Mean age of onset was 18 (SD = 10.35) and mean HAM-D score without anxiety items was 14.04 (SD = 3.60). Anxious and nonanxious groups did not differ significantly by age, gender, FSIQ-2, or severity of depression (p's > .10). HAM-D anxiety-somatization scores for the anxious depression group were significantly higher than for the nonanxious group (p < .001).
Demographic characteristics for the 24 healthy controls (50% male, mean age 45.25, SD = 13.91) included as part of the sample did not significantly differ from the MDD groups (p's > .05). See Table 1 for demographic and clinical information.
Table 1.
Group comparisons of demographic information in depressed samples and in controls.
| Nonanxious depression | Anxious depression | Controls | ||||
|---|---|---|---|---|---|---|
| df | X2 | p | ||||
| N | 14 | 14 | 24 | |||
| N (%) Male | 11 (78.57) | 7 (50.00) | 12 (50.00) | 2 | 3.422 | .181 |
| Mean (SD) | Mean (SD) | df | F | p | ||
| Age (yrs) | 43.43 (13.50) | 45.50 (13.30) | 45.25 (13.91) | 2, 49 | .102 | .903 |
| FSIQ-2 | 120.93 (12.38) | 120.62 (9.81) | 118.29(11.03) | 2, 48 | .320 | .728 |
| Age of Onset (yrs) | 19.50 (13.61) | 16.50 (5.69) | - | 1, 26 | .58 | .454 |
| HAM-D | 13.29 (2.84) | 14.79 (4.19) | - | 1, 26 | 1.23 | .278 |
| HAM-D-AS | 4.93 (0.92) | 8.00 (1.04) | - | 1, 26 | 68.87 | < .001 |
Note: One FSIQ-2 score missing for a participant in the anxious depression group.
Abbreviations: FSIQ-2: an estimate of general cognitive ability as assessed by two subtests of the Wechsler Abbreviated Scale of Intelligence. HAM-D: Hamilton Depression Rating Scale, excluding anxiety-somatization items. HAM-D-AS = Hamilton Depression Rating Scale, anxiety-somatization items only.
3.2. Group comparisons: response point and accuracy
In the mixed model examining effects of the groups with anxious versus nonanxious depression on response point, the main effect of emotion was significant. Response point for happy faces was earlier than for the other faces (i.e., less intensity of emotion was required to correctly identify the expression; F(5, 910) = 73.30, p < .001, η2 = .07). A significant emotion by group interaction was observed (F(5, 910) = 2.82, p = .02, η2 = .003); pairwise comparisons revealed that, compared to the group with nonanxious depression, the anxious depression group displayed a significantly later response point for happy (p = .01, η2 = .13) and sad (p = .04, η2 = .07) faces. The groups did not differ in response point for other emotions (p's > .05).
The mixed model examining accuracy revealed no main effect of group (F(2, 49) = 0.92, p = .41, η2 = .02), or group by emotion interaction (F(10, 1715) = 0.86, p = .57, η2 < .001). A significant main effect was observed for emotion (F(5, 1715) = 25.56, p < .001, η2 = .01); pairwise comparisons indicated that participants were significantly more accurate when identifying happy expressions and were significantly less accurate when identifying disgusted expressions compared to other expressions (p’s < .01). Mean accuracy across MDD groups was 100% for happy expressions, 90% for sad expressions, 89% for surprised expressions, 84% for angry expressions, 83% for fearful expressions, and 71% for disgusted expressions. Further information of percent accuracy by group and emotion, with estimated marginal means and standard errors from the mixed model, is presented in Table 2.
Table 2.
Mean accuracy (percent correct) by group for each emotion.
| Nonanxious depression | Anxious depression | Controls | |
|---|---|---|---|
| Mean (SE) | Mean (SE) | Mean (SE) | |
| Disgusted | 68(3.8) | 68(3.8) | 76(2.9) |
| Surprised | 94(3.8) | 86(3.8) | 88(2.9) |
| Angry | 81(3.8) | 83(3.8) | 87(2.9) |
| Fearful | 82(3.8) | 83(3.8) | 83(2.9) |
| Sad | 92(3.8) | 86(3.8) | 92(2.9) |
| Happy | 100(3.8) | 100(3.8) | 100(2.9) |
3.3 Anxiety as a continuous variable: response point and accuracy
In the mixed model examining the effect of anxiety as a continuous variable on response point, the emotion by anxiety interaction approached significance (F(5, 910) = 2.19, p = .053, η2 = .002). Pearson correlations indicated that higher anxiety was associated with later response point for sad faces (r(28) = −.38, p = .05) but not for other emotions (r(28) ranging from −.11 to .09, p's>.05); these correlations were not corrected for multiple comparisons.
In the mixed model examining anxiety as a continuous variable with accuracy, the emotion by anxiety interaction was not significant (F(5, 910) = 1.26, p = .28, η2 = .001).
3.4 Comparisons to control group
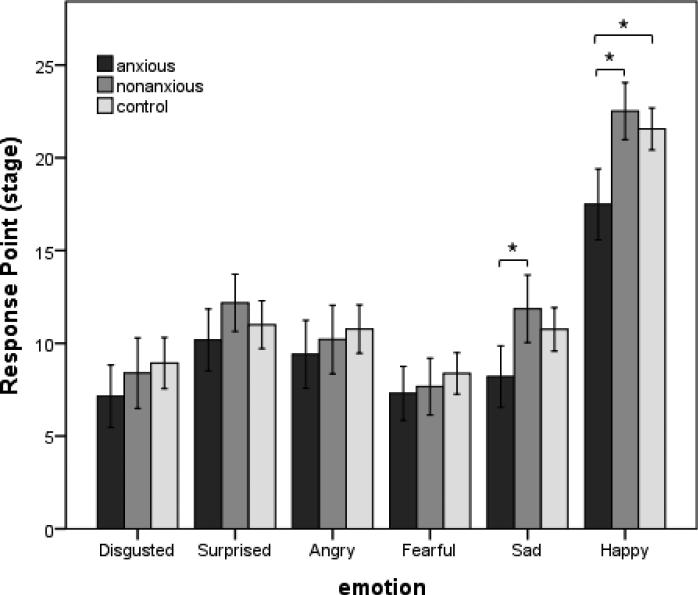
As a final analysis, the anxious and nonanxious depression groups were compared to controls. Specifically, we compared: 1) the response point between the anxious depression group and healthy controls, and 2) the response point between the nonanxious depression group and the control group. Compared to the control group, the anxious depression group displayed a significantly later response point for happy faces (p = .01, η2 = .08). None of the other comparisons by emotion were significant. The nonanxious depression group did not differ from the healthy group on any of the emotions (p's > .1) (See Figure 1). Finally, the full three-way mixed model comparing anxious, nonanxious and healthy controls showed no overall significant difference by group, F(2,49) = 1.98, p = .15, η2 = .04; and the emotion by group interaction did not reach significance, F(10,1715) = 1.65, p = .09, η2 < .001.
Figure 1.
Response point for anxious depressed, nonanxious depressed, and control groups to each emotion. Higher response point indicates earlier recognition. CI = 95%, * p < .05.
4. Discussion
This post-hoc investigation examined emotion-recognition patterns in patients with anxious depression, patients with nonanxious depression, and healthy controls using dynamic facial stimuli. As predicted, the group with anxious depression required a significantly greater intensity of expression, demonstrated by a later response point, to recognize happy and sad faces (but not other faces) than the group with nonanxious depression. In addition, severity of anxiety correlated with later response time to sad faces (but not other faces). When each group was compared to controls, the group with anxious depression required greater intensity of expression to identify happy faces than the control group, but the group with nonanxious depression did not differ from controls in response point to any emotion, however this finding should be interpreted with caution considering that the larger model comparing all three groups did not reach statistical significance.
4.1. Implications for emotion recognition
Results from the present study suggest that anxious depression, compared to nonanxious depression, is associated with diminished recognition of happy and sad faces. Furthermore, greater severity of anxiety is associated with greater impairment in recognizing sad faces; it should be noted, however, that the correlation with sad faces was not corrected for multiple comparisons, and thus this result should be interpreted with caution. While depression-specific patterns of response were not apparent when participants with anxious and nonanxious depression were combined into a single MDD group [14], dividing the sample into anxious and nonanxious groups revealed potential differences. These findings underscore one of the potential negative implications of continuing to study MDD as a heterogeneous disorder rather than as a disease with many subtypes; specifically, initial analyses of heterogeneous samples may fail to find significant group differences that exist within subtypes.
Contrary to hypothesis, greater sensitivity to angry and fearful faces was not found for individuals with anxious depression. This may be due to the presence of MDD in the current sample; however, it should be noted that another possible explanation involves methodological differences between prior research and the present study. Unlike stimuli in the present study, threat-relevant stimuli in some prior investigations have been either backward-masked by neutral faces (e.g. [20]), or presented in an array of other emotional faces (e.g. [19]). Discrepancies between the present findings and previous findings highlight the importance of context in emotion recognition. Specifically, the present methods may be more generalizable to one-on-one social interactions in which interpretation of subtle facial expressions is most important.
4.2. Implications for treatment
Given that the present findings suggest potential differences in emotion recognition between anxious and nonanxious depression, they may also underscore a need to better understand the relationship between depressive and anxiety symptoms during treatment. Individuals with anxious depression (compared to nonanxious depression) have poorer response and higher remission rates following traditional cognitive therapy and interpersonal psychotherapy [5]. Given that the present study suggests deficits in emotion recognition for those with anxious depression, it may be beneficial for psychotherapeutic interventions to address these deficits. Future research is indicated to determine the extent to which interventions that target emotion recognition may be effective for those with anxious depression. Taken together with known differences in clinical outcomes between anxious and nonanxious depression, the results of the present study underscore the importance of considering the role of anxiety in both understanding the neurobiology of depression subtypes and determining treatment strategies for MDD.
4.3. Interpretation of task outcomes
It is notable that the groups did not differ with regard to accuracy: anxious depression was not associated with misinterpretation of facial stimuli, but with a higher threshold between ambiguous and emotional faces. Interpreting this finding requires a precise understanding of the task's outcomes. Response point for a given emotion represents the mean stage at which the correct response was given, coding incorrect responses as zero; accuracy refers to the percentage of trials for which the final response was correct. Thus the present findings indicate that while the group with anxious depression recognized happy and sad faces with equally high accuracy as the group with nonanxious depression, correct responses to these faces came at later stages for the group with anxious depression. During the earlier stages of viewing the happy and sad expressions, it is possible that anxious participants either: 1) did not respond, or 2) gave an incorrect response that was corrected at a later stage. This is consistent with prior data indicating that the depression-related deficits in emotion recognition may be specific to ambiguous expressions [7]; further work is needed to determine whether these deficits may apply to anxious but not nonanxious depression.
4.4. Strengths and limitations
Our study has several strengths. First, we used dynamic facial stimuli to collect information about both accuracy and sensitivity of emotion recognition. Second, unlike previous studies that have used facial stimuli morphing directly from one emotion (e.g., happy) to another (e.g., sad) [27], or static emotional faces, the current study used a paradigm in which faces morphed from neutral to emotional expressions, thus generating precise information about discrete emotions. Third, our clinical sample was not under treatment with any psychiatric medication, so the possibility of medication effects may be ruled out.
The study is also associated with several notable limitations. First, the sample did not include an “anxiety-only” group without depression. Therefore, it is unknown whether the emotion recognition deficits suggested by the current findings are associated with anxious depression specifically, or with anxiety more generally. Future studies in individuals with primary anxiety disorder diagnoses are needed in order to understand how anxiety may influence emotion recognition. Second, use of the HAM-D anxiety-somatization factor score is only one way to define anxious and nonanxious depression [3]. Information about psychiatric comorbidity in the present MDD sample was not available, so any potential effects of comorbidities on task performance are unknown. Research using other methods to define anxious and nonanxious depression—such as the presence or absence of comorbid anxiety diagnosis—may further clarify the role of anxiety in depression. Third, while it is likely that the anxious group was on average more anxious than other groups at the time of task administration, state anxiety at time of administration was not explicitly measured. Fourth, although the Emotional Expression Multimorph Task was designed to test social abilities in a naturalistic setting, the extent to which performance on the task may correlate with social functioning is not fully known. Fifth, because samples were too small to include gender as a factor, we were unable to account for the potential role of gender in emotion recognition. Finally, the task software does not provide information about misclassifications that were later corrected; additional detail about corrected responses may shed further light on the nature of potential emotion recognition deficits in depression.
5. Conclusions
In conclusion, the finding that anxious depression is marked by a diminished sensitivity to happy and sad faces but not heightened sensitivity to angry or fearful faces indicates a need for further research into how anxious depression may differ from either anxiety or depression alone. The present results suggest that recognizing subtle stages of happy and sad facial expressions may be more difficult for individuals with anxious depression. Clinicians should consider the impact and severity of anxiety symptoms on emotion recognition when treating individuals with anxious depression. Further investigations of the phenomena that characterize anxious depression may lead to much-needed improvements in treatments for this condition.
Highlights.
The nature of emotion recognition in anxious depression is not fully understood.
Anxious and nonanxious subjects with MDD completed an emotion recognition task.
Anxious subjects had poorer recognition of happy and sad facial expressions.
Anxious subjects did not display hypervigilance to threatening facial expressions.
Acknowledgements
The authors thank the 7SE research unit and staff for their support. Ioline Henter, MA (NIMH) provided invaluable editorial assistance.
Role of Funding Source
Funding for this work was supported in part by the Intramural Research Program at the National Institute of Mental Health, National Institutes of Health IRP-NIMH-NIH; NCT#00088699; ZIA MH002927), by a NARSAD Independent Investigator to Dr. Zarate, and by a Brain and Behavior Mood Disorders Research Award to Dr. Zarate. These funding sources had no further role in study design; in the collection, analysis, or interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Dr. Zarate is listed as a co-inventor on a patent for the use of ketamine and its metabolites in major depression. He has assigned his rights in the patent to the US government but will share a percentage of any royalties that may be received by the government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
All other authors have no conflict of interest to disclose, financial or otherwise.
References
- 1.Fava M, Alpert J, Carmin CN, Wisniewski SR, Trivedi M, Biggs MM, et al. Clinical correlates and symptom patterns of anxious depression among patients with major depressive disorder in STAR*D. Psychol Med. 2004;34:1299–308. doi: 10.1017/s0033291704002612. [DOI] [PubMed] [Google Scholar]
- 2.Fava M, Rush AJ, Alpert JE, Carmin CN, Balasubramani GK, Wisniewski SR, et al. What clinical and symptom features and comorbid disorders characterize outpatients with anxious major depressive disorder: a replication and extension. Canadian journal of psychiatry. 2006;51:823–35. doi: 10.1177/070674370605101304. [DOI] [PubMed] [Google Scholar]
- 3.Ionescu DF, Niciu MJ, Henter ID, Zarate CAJ. Defining anxious depression: a review of the literature. CNS Spectr. 2013;18:252–60. doi: 10.1017/S1092852913000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farabaugh A, Alpert J, Wisniewski SR, Otto MW, Fava M, Baer L, et al. Cognitive therapy for anxious depression in STAR(*) D: what have we learned? J Affect Disord. 2012;142:213–8. doi: 10.1016/j.jad.2012.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ionescu DF, Niciu MJ, Richards EM, Zarate CAJ. Pharmacologic treatment of dimensional anxious depression: a review. Prim Care Companion CNS Disord. 2014:16. doi: 10.4088/PCC.13r01621. pii: PCC.13r01621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bourke C, Douglas K, Porter R. Processing of facial emotion expression in major depression: a review. Aust N Z J Psychiatry. 2010;44:681–96. doi: 10.3109/00048674.2010.496359. [DOI] [PubMed] [Google Scholar]
- 8.Rubinow DR, Post RM. Impaired recognition of affect in facial expression in depressed patients. Biol Psychiatry. 1992;31:947–53. doi: 10.1016/0006-3223(92)90120-o. [DOI] [PubMed] [Google Scholar]
- 9.Gur RC, Erwin RJ, Gur RE, Zwil AS, Heimberg C, Kraemer HC. Facial emotion discrimination: II. Behavioral findings in depression. Psychiatry Res. 1992;42:241–51. doi: 10.1016/0165-1781(92)90116-k. [DOI] [PubMed] [Google Scholar]
- 10.Leppanen JM, Milders M, Bell JS, Terriere E, Hietanen JK. Depression biases the recognition of emotionally neutral faces. Psychiatry Res. 2004;128:123–33. doi: 10.1016/j.psychres.2004.05.020. [DOI] [PubMed] [Google Scholar]
- 11.Rich BA, Grimley ME, Schmajuk M, Blair KS, Blair RJR, Leibenluft E. Face emotion labeling deficits in children with bipolar disorder and severe mood dysregulation. Dev Psychopathol. 2008;20:529–46. doi: 10.1017/S0954579408000266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Joormann J, Gotlib IH. Is this happiness I see? Biases in the identification of emotional facial expressions in depression and social phobia. J Abnorm Psychol. 2006;115:705–14. doi: 10.1037/0021-843X.115.4.705. [DOI] [PubMed] [Google Scholar]
- 13.LeMoult J, Joorman J, Sherdell L, Wright Y, Gotlib IH. Identification of emotional facial expressions following recovery from depression. J Abnorm Psychol. 2009;118:828–33. doi: 10.1037/a0016944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schaefer KL, Baumann J, Rich BA, Luckenbaugh DA, Zarate CAJ. Perception of facial emotion in adults with bipolar or unipolar depression and controls. J Psychiatr Res. 2010;44:1229–35. doi: 10.1016/j.jpsychires.2010.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bouhuys AL, Geerts E, Mersch PP. Relationship between perception of facial emotions and anxiety in clinical depression: does anxiety-related perception predict persistence of depression. J Affect Disord. 1997;43:213–23. doi: 10.1016/s0165-0327(97)01432-8. [DOI] [PubMed] [Google Scholar]
- 16.Suslow T, Dannlowski U, Lalee-Mentzel J, Donges US, Arolt V, Kersting A. Spatial processing of facial emotion in patients with unipolar depression: a longitudinal study. J Affect Disord. 2004;83:59–63. doi: 10.1016/j.jad.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 17.Winton EC, Clark DM, Edelmann RJ. Social anxiety, fear of negative evaluation and the detection of negative emotion in others. Behav Res Ther. 1995;33:193–6. doi: 10.1016/0005-7967(94)e0019-f. [DOI] [PubMed] [Google Scholar]
- 18.Surcinelli P, Codispoti M, Montebarocci O, Rossi N, Baldaro B. Facial emotion recognition in trait anxiety. J Anxiety Disord. 2006;20:110–7. doi: 10.1016/j.janxdis.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 19.Byrne A, Eysenck MW. Trait anxiety, anxious mood, and threat detection. Cogn Emot. 1995;9:549–62. [Google Scholar]
- 20.Doty TJ, Japee S, Ingvar M, Ungerleider LG. Fearful face detection sensitivity in healty adults correlates with anxiety-related traits. Emotion. 2013;13:183–8. doi: 10.1037/a0031373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blair RJR. Facial expressions, their communicatory functions and neuro-cognitive substrates. Philos Trans R Soc Lond B Biol Sci. 2003;358:561–72. doi: 10.1098/rstb.2002.1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.First MB, Spitzer RL, Gibbon M, Williams AR. Structured Clinical Interview for DSM-IV TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) New York State Psychiatric Institute, Biometrics Research; New York: 2001. [Google Scholar]
- 23.Cleary P, Guy W. Factor analysis of the Hamilton depression scale. Drugs Exp Clin Res. 1977;1:115–20. [Google Scholar]
- 24.Fava M, Rush AJ, Alpert JE, Balasubramani GK, Wisniewski SR, Carmin CN, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. 2008;165:342–51. doi: 10.1176/appi.ajp.2007.06111868. [DOI] [PubMed] [Google Scholar]
- 25.Wechsler D. Wechsler Abbreviated Scale of Intelligence--Second Edition Manual. Pearson; Bloomington, MN: 2011. [Google Scholar]
- 26.Ekman P, Friesen WV. Pictures of facial affect. Human Interaction Laboratory, University of California Medical Center; San Francisco, CA: 1976. [Google Scholar]
- 27.Liu W, Huang J, Wang L, Gong Q, Chan RCK. Facial perception bias in patients with major depression. Psychiatry Res. 2012;197:217–20. doi: 10.1016/j.psychres.2011.09.021. [DOI] [PubMed] [Google Scholar]