Abstract
Objectives
The aim of this systematic review was to analyze post‐loading implant loss for implant‐supported prostheses in edentulous jaws, regarding a potential impact of implant location (maxilla vs. mandible), implant number per patient, type of prosthesis (removable vs. fixed), and type of attachment system (screw‐retained, ball vs. bar vs. telescopic crown).
Material and methods
A systematic literature search for randomized‐controlled trials (RCTs) or prospective studies was conducted within PubMed, Cochrane Library, and Embase. Quality assessment of the included studies was carried out, and the review was structured according to PRISMA. Implant loss and corresponding 3‐ and 5‐year survival rates were estimated by means of a Poisson regression model with total exposure time as offset.
Results
After title, abstract, and full‐text screening, 54 studies were included for qualitative analyses. Estimated 5‐year survival rates of implants were 97.9% [95% CI 97.4; 98.4] in the maxilla and 98.9% [95% CI 98.7; 99.1] in the mandible. Corresponding implant loss rates per 100 implant years were significantly higher in the maxilla (0.42 [95% CI 0.33; 0.53] vs. 0.22 [95% CI 0.17; 0.27]; P = 0.0001). Implant loss rates for fixed restorations were significantly lower compared to removable restorations (0.23 [95% CI 0.18; 0.29] vs. 0.35 [95% CI 0.28; 0.44]; P = 0.0148). Four implants and a fixed restoration in the mandible resulted in significantly higher implant loss rates compared to five or more implants with a fixed restoration. The analysis of one implant and a mandibular overdenture also revealed higher implant loss rates than an overdenture on two implants. The same (lower implant number = higher implant loss rate) applied when comparing 2 vs. 4 implants and a mandibular overdenture. Implant loss rates for maxillary overdentures on <4 implants were significantly higher than for four implants (7.22 [95% CI 5.41; 9.64] vs. 2.31 [1.56; 3.42]; P < 0.0001).
Conclusions
Implant location, type of restoration, and implant number do have an influence on the estimated implant loss rate. Consistent reporting of clinical studies is necessary and high‐quality studies are needed to confirm the present results.
Keywords: edentulous mandible, edentulous maxilla, implant‐supported prosthesis, meta‐analysis, systematic review
Introduction and rationale
Complete edentulism still is a common health problem. Although oral health studies illustrated a decrease of individuals suffering from an edentate status, in Germany still 22.6% of 65‐ to 70‐year olds were completely edentulous in the year 2005 (Micheelis & Schiffner 2006).
A complete denture is the classic therapy of full edentulism. Nowadays, this kind of rehabilitation might not be considered as the standard therapy for the lower edentulous jaw any longer. The stabilization of the lower denture with at least two endosseous implants is applied for more than 20 years and was recommended by Feine and co‐workers in the McGill consensus statement as standard therapy in 2002 already (Feine et al. 2002a,b,c).
The diversity of problems caused by complete dentures is not a modern issue. Patients do not only complain about insufficient chewing abilities and articulation problems, but also experience psychic strain and social impairment (Albaker 2013). On the contrary, clinical studies investigating the potential impact of implant‐supported prostheses on the oral health‐related quality of life were able to show clear improvement after implants had been inserted (Zitzmann & Marinello 2000a; Allen & McMillan 2003; Scala et al. 2012; Zembic & Wismeijer 2014). It is worth mentioning that clear evidence of benefits for the patient is merely available for the edentulous lower jaw with two interforaminal implants and an overdenture compared to a complete denture. The few studies concerning patient‐centered outcome for implant‐supported prostheses in the maxilla indicate advantages for the patient. However, considering daily practice, it has to be assumed that the majority of patients with a maxillary complete denture do not articulate major problems.
This systematic review is an update of our own (Schley & Wolfart 2011) and other previously published reviews on the edentulous jaw. As a result of clinical diversity reasons, usually, only a limited number of studies were included in these reviews. Moreover, probably due to a lack of high‐quality studies, most of them also included retrospective studies (Lambert et al. 2009; Slot et al. 2009; Heydecke et al. 2012), which are known to have a lower level of evidence. Furthermore, they either included the edentulous maxilla (Slot et al. 2009) or mandible (Payne & Solomons 2000; Roccuzzo et al. 2012; Papaspyridakos et al. 2013) or pooled the results for both jaws (Papaspyridakos et al. 2012). Two very interesting systematic reviews with meta‐analysis were recently published (Papaspyridakos et al. 2012, 2013). They focused on biologic and technical complications of fixed implant restorations in edentulous mandibles and implant and prosthodontic survival rates of both jaws and reported an implant survival rate of 97.3% after 10 years.
There is still a large variety of opinions on the best rehabilitation of an edentulous patient. The patient's wish and his or her individual circumstances, which also include financial capacities, have first priority in the decision‐making. The anatomic situation and the dentist's knowledge, that is his or her internal evidence, determine the further procedure. Nowadays, the insertion and/or restoration of dental implants in edentulous jaws can considered to be one of the basic treatment modalities in a dentist's everyday practice. Therefore, it seems to be essential to define reproducible treatment protocols that support the individual's expertise and help to establish clear concepts in the sense of an evidence‐based dentistry.
The “optimal” number of implants for edentulous jaws still seems to be debatable. Different reviews tried to address this question (Lambert et al. 2009; Slot et al. 2009; Roccuzzo et al. 2012) and a recently published clinical guideline at least provided key recommendations concerning number of implants and type of implant prosthesis for the edentulous maxilla (Schley & Wolfart 2011; Schley et al. 2013).
To the authors' best knowledge, the potential influence of several factors (not only implant number) on the outcome of dental implants in edentulous patients has not been systematically elaborated, statistically analyzed and compared for both fixed and removable restorations for maxilla and mandible in one review.
Thus, the aim of this systematic review was to address the following focused question:
Is there an impact of implant location (maxilla vs. mandible), implant number, type of prosthesis (fixed vs. removable) and/or different anchorage systems on the implant loss rate concerning the implant‐prosthodontic rehabilitation of edentulous patients?
Material and methods
Protocol
Prior to the systematic literature search, a review protocol was determined with the software Review Manager, version 5.2.
Structure of the review
The systematic review was edited according to the “Preferred Reporting Items for Systematic Reviews and Meta‐Analyses” (PRISMA) (Moher et al. 2009).
Eligibility criteria
The focused question was formulated according to the PICOS format, as suggested by the Center for Evidence‐Based Medicine and served as a basis for the systematic literature search (Askig Focused Questions 2014):
Patients: edentulous patients (both jaws or either upper or lower jaw) with an implant‐retained fixed or removable prosthesis;
Interventions: insertion of either machined or rough‐surfaced endosseous titanium implants with a root‐like or cylindrical form, irrespective of implant number, length, diameter, position, or angulation, into either local or augmented bone, prosthodontic rehabilitation with a fixed full‐arch bridge, segmented reconstructions or a removable overdenture according to an immediate, early or conventional loading protocol.
Comparisons: comparison of different types of prostheses (fixed vs. removable) and/or anchorage systems (ball/locator, bar, telescopic crowns) or fixation mode (screw‐retained/cemented) with different implant numbers, in one or between both jaws.
Outcomes: implant survival rate or number of implant losses after prosthetic loading after an observation period of at least 3 years.
Study design: randomized‐controlled trials (RCTs) or prospective clinical studies as reported by the authors
Definitions: A prosthesis not being detachable by the patient himself was defined as “fixed prosthesis,” that is, screw‐retained or cemented fixed full‐arch or segmented prostheses. An overdenture retained by different anchorage systems (bar, ball/locator or telescopic crown), and accordingly being removable by the patient, was defined as “removable prosthesis.” Regarding different implant surfaces merely a simple distinction between machined and so‐called rough implant surfaces was made. A further differentiation of roughening methods or surface modifications, respectively, was not applicable. The loading protocols were defined according to Esposito et al. (2007), that is, an immediate loading was considered to be within 1 week after implant insertion, an early loading between 1 weeks and 2 months, and a conventional loading after a healing period of more than 2 months.
An implant being still in situ with a bony anchorage after the observation period was defined as “implant survival,” irrespective of hard or soft tissue condition around the implant. Prosthetic loading (immediate or after a conventional healing period) was defined as baseline, meaning, that so‐called early losses, that is losses before prosthetic loading, were noted but not statistically evaluated.
Exclusion criteria: no clinical study, retrospective studies, observation period of <3 years, no mean observation period or detailed information on time of implant loss/dropout, no separate reporting of maxilla and mandible or fixed and removable prostheses, provisional implants, ceramic implants, or implants placed into the pterygomaxillary, zygomatic or palatal region, transmandibular implants, studies reporting on the same patient cohort more than once.
Information sources
The electronic databases of Medline (PubMed), Cochrane Library, and Embase were searched. A supplementary manual search in different German dental journals (Deutsche Zahnärztliche Zeitschrift, Implantologie, Quintessenz, Zeitschrift für Zahnärztliche Implantologie), reference lists of available publications, and private databases (End Note libraries) was conducted. Authors of available studies were contacted per mail in case of unclear data.
May 7, 2014 was the last date of search. (Table 1).
Table 1.
Search strategy
| Information sources | Electronic databases | PubMed, EMBASE, The Cochrane Library |
| Additional sources | German dental journals (not Medline listed), Private databases, reference lists | |
|
Search strategy PubMed |
Population | #1: ((“mouth, edentulous”[MeSH Terms] OR (“mouth”[All Fields] AND “edentulous”[All Fields]) OR “edentulous mouth”[All Fields] OR “edentulous”[All Fields]) OR (completely[All Fields] AND (“mouth, edentulous”[MeSH Terms] OR (“mouth”[All Fields] AND “edentulous”[All Fields]) OR “edentulous mouth”[All Fields] OR “edentulous”[All Fields]))) AND (“maxilla”[MeSH Terms] OR “maxilla”[All Fields])) OR (“mandible”[MeSH Terms] OR “mandible”[All Fields])) AND (“dental implants”[MeSH Terms] OR (“dental”[All Fields] AND “implants”[All Fields]) OR “dental implants”[All Fields] OR (“dental”[All Fields] AND “implant”[All Fields]) OR “dental implant”[All Fields]) |
| Intervention | #2: #1 AND ((implant[All Fields] AND (“denture, overlay”[MeSH Terms] OR (“denture”[All Fields] AND “overlay”[All Fields]) OR “overlay denture”[All Fields] OR “overdenture”[All Fields])) OR (complete[All Fields] AND implant[All Fields] AND removable[All Fields] AND (“dental prosthesis”[MeSH Terms] OR (“dental”[All Fields] AND “prosthesis”[All Fields]) OR “dental prosthesis”[All Fields]))) OR (complete[All Fields] AND fixed[All Fields] AND (“dental prosthesis”[MeSH Terms] OR (“dental”[All Fields] AND “prosthesis”[All Fields]) OR “dental prosthesis”[All Fields]))) OR (full‐arch[All Fields] AND restoration[All Fields])) OR (“dental prosthesis, implant‐supported”[MeSH Terms] OR (“dental”[All Fields] AND “prosthesis”[All Fields] AND “implant‐supported”[All Fields]) OR “implant‐supported dental prosthesis”[All Fields] OR (“implant”[All Fields] AND “supported”[All Fields] AND “dental”[All Fields] AND “prosthesis”[All Fields]) OR “implant‐supported dental prosthesis”[All Fields])) | |
| Comparison | Covered by Population, Intervention and Outcome search | |
| Outcome | #3: #1 AND (“survival rate”[MeSH Terms] OR (“survival”[All Fields] AND “rate”[All Fields]) OR “survival rate”[All Fields]) | |
| Limits (filters) | Clinical trial, humans | |
| Period | No time restriction | |
|
Search strategy EMBASE |
“dental implant”/exp OR “dental implant” AND “edentulous” | |
| Limits (filters) | No | |
|
Search strategy Cochrane Central Register of Controlled Trials |
“dental implant AND edentulous” | |
| Limits (filters) | Trials |
Search strategy
The search strategy is described in Table 1. The PubMed search complied with the PICOS question addressing Patients, Intervention, Comparison, Outcome and Study design.
Study selection
The resulting initial hits of the above‐mentioned search were screened, and a first pre‐selection by title was undertaken. Titles were sequentially excluded if they indicated a non‐relevant content (e.g., no dental implants, animal or in vitro study). In case of any uncertainty, an additional abstract reading was performed. Abstracts of the selected titles were inspected for relevance resulting in a choice of possibly eligible full texts. If studies were published by the same author or institution several times, the according manuscripts were thoroughly read and compared to avoid the inclusion of duplicate data. After full‐text selection and data extraction, it was decided whether the publication was adequate for the intended systematic review.
Study selection and data extraction were performed independently by two reviewers (JSK, TK), and any disagreement was solved by discussion. To assess consistency among the reviewers, the interreviewer reliability using Cohen's Kappa statistic (κ) was analyzed.
Data collection and data items
Extracted data were filled into pre‐defined forms and included the following parameters: author, year, total number of patients/prostheses investigated, observation period, total number of implants, number and time of dropouts on implant level, number of implants per patient, type of implant prosthesis, type of anchorage system, implant survival and implant losses before and after loading. Moreover, implant system, implant surface, loading protocol, and bone augmentation procedures were noted. All variables were pre‐determined and no additional variables were added after the reviewing had started.
Risk of bias within and across studies
A potential risk of bias within the included studies was assessed using the methodology checklists provided by the Scottish Intercollegiate Guidelines Network (SIGN). These lists comprise the critical appraisal of the selection of subjects, the applied assessment, potential confounders, and the statistical analysis, and finally, the overall assessment of the methodological quality of the study:
High quality: (++) Majority of criteria met. Little or no risk of bias. Results unlikely to be changed by further research.
Acceptable quality: (+) Most criteria met. Some flaws in the study with an associated risk of bias, Conclusions may change in the light of further studies.
Low quality: (−) Either most criteria not met, or significant flaws relating to key aspects of study design. Conclusions likely to change in the light of further studies.
Further explanations are shown as footnote of Table 2.
Table 2.
Risk of bias within studies
| Studies in alphabetical order | Study design | Overall assessment of the studya | Level of evidenceb | Sponsoring/support as reported by the authors |
|---|---|---|---|---|
| Agliardi et al. (2012) | Prospective | + | 2+ | n.r. |
| Akca et al. (2010) | Prospective | + | 2+ | Partly supported by State Planning Organization, Prime Ministry, Republic of Turkey |
| Akoglu et al. (2011) | Prospective | ++ | 2++ | n.r. |
| Arvidson et al. (1998) | Prospective | + | 2+ | n.r. |
| Arvidson et al. (2008) | Prospective | ++ | 2++ | Supported and sponsored by Institut Straumann AG, Basel, Switzerland |
| Behneke et al. (2002) | Prospective | + | 2+ | n.r. |
| Bergendal & Engquist (1998) | Prospective | + | 2+ | n.r. |
| Cehreli et al. (2010) | RCT | + | 1+ |
Partly supported by the State Planning Organization, Prime Ministry, Republic of Turkey |
| Chiapasco & Gatti (2003) | Prospective | + | 2+ | n.r. |
| Collaert & De Bruyn (2008) | Prospective | + | 2+ | n.r. |
| Cooper et al. (2008) | Prospective | ++ | 2++ | n.r. |
| Cordioli et al. (1997) | Prospective | + | 2+ | n.r. |
| Covani et al. (2012) | Prospective | + | 2+ | n.r. |
| Crespi et al. (2012) | Prospective | + | 2+ | n.r. |
| De Bruyn et al. (2008) | Prospective | + | 2+ | n.r. |
| De Santis et al. (2012) | Prospective | + | 2+ | n.r. |
| Degidi et al. (2010) | Prospective | + | 2+ | n.r. |
| Ekelund et al. (2003)/Lindquist et al. (1996) | Prospective | + | 2+ | n.r. |
| Eliasson et al. (2010) | Prospective, randomized | + | 2+ | Supported by a grant from Public Dental Health, Örebro County Council, Sweden |
| Elsyad et al. (2012) | RCT | + | 1+ | n.r. |
| Engquist et al. (2005) | Prospective, controlled | ++ | 2++ | n.r. |
| Fischer & Stenberg (2012) | Prospective | + | 2+ | Institut Straumann AG, Basel, Switzerland assisted to prepare the manuscript |
| Gotfredsen & Holm (2000) | Prospective, randomized | + | 2+ | Astra Tech, Sweden supplied implants and implant components |
| Harder et al. (2011) | Prospective | + | 2+ | Supported by a grant from Camlog Biotechnologies AG, Basel, Switzerland |
| Heijdenrijk et al. (2006) | Prospective, randomized | + | 2+ | n.r. |
| Heschl et al. (2013) | Prospective | + | 2+ | n.r. |
| Jemt et al. (1996)/Watson et al. (1997) | Prospective | + | 2+ | Nobelpharma AB, Göteborg, Sweden supported with components |
| Krennmair et al. (2008) | Prospective, randomized | ++ | 2++ | Study was self‐funded by the authors and their institution |
| Krennmair et al. (2011) | Prospective, randomized | ++ | 2++ | n.r. |
| Krennmair et al. (2012) | Prospective, randomized | ++ | 2++ | Study was self‐funded by the authors and their institution |
| Lethaus et al. (2011) | Prospective | + | 2+ | Supported and sponsored by Institut Straumann, Basel, Switzerland |
| Liddelow & Henry (2010) | Prospective | + | 2+ | n.r. |
| Lorenzoni et al. (2013) | Prospective | + | 2+ | n.r. |
| Meijer et al. (2004) | RCT | + | 1+ | n.r. |
| Meijer et al. (2009a, 2009b) | Prospective | + | 2+ | n.r. |
| Meijer et al. (2009a, b) | Prospective | + | 2+ | n.r. |
| Mertens et al. (2012) | Prospective | + | 2+ | Supported by Astra Tech AB, Sweden and Bioscientia, Germany, provided kits for IL‐1 composite genotype tests |
| Murphy et al. (2002) | Prospective | + | 2+ | n.r. |
| Naert et al. (1998) | Prospective | + | 2+ | Ceka NV, Belgium, support with prosthesis components |
| Nyström et al. (2009a,b) | Prospective | + | 2+ | n.r. |
| Nyström et al. (2009a,b) | Prospective | + | 2+ | n.r. |
| Örtorp & Jemt (2012) | Prospective | + | 2+ | Supported by Wilhelm and Martina Lundgren Research Foundation |
| Rasmusson et al. (2005) | Prospective | + | 2+ | n.r. |
| Richter & Knapp (2010) | Prospective | + | 2+ | Biomet 3i supported the study with implants and implant components |
| Romeo et al. (2004) | Prospective | + | 2+ | n.r. |
| Schwarz et al. (2010) | Prospective | + | 2+ | Financially supported by FRIADENT GmbH, Germany |
| Sjöström et al. (2007) | Prospective | + | 2+ | n.r. |
| Stoker et al. (2012) | RCT | + | 1+ | Supported by a grant (188/2000) from the ITI Foundation for the Promotion of Oral Implantology, Switzerland |
| Testori et al. (2004) | Prospective | + | 2+ | n.r. |
| Van de Velde et al. (2007) | Prospective | + | 2+ | n.r. |
| Vroom et al. (2009) | Prospective | + | 2+ | Partly supported by Astra Tech AB, Sweden |
| Weinländer et al. (2010) | Prospective | + | 2+ | Study was self‐funded by the authors and their institution |
| Zitzmann & Marinello (2000a,b) | Prospective | + | 2+ | n.r. |
| Zou et al. (2013) | Prospective | + | 2+ |
Funded by Combined Engineering and Medical Project of Shanghai Jiao Tong University the National Natural Science Foundation of (YG2010MS56), Science and Technology Commission of Shanghai Municipality (13ZR1424000), China (81100788, 31370983, 81371190), the Key Project of Chinese Ministry of Education (212080), Grants for Scientific Research of BSKY (XJ201109), and the Young Top‐notch Talent Support Scheme from Anhui Medical University |
How well was the study performed to minimize the risk of bias or confounding? (++) High quality (+) Acceptable (−) Low quality.
Level of evidence according to SIGN: 1+ = well‐conducted meta‐analyses, systematic reviews, or RCTs with a low risk of bias; 2++ = high‐quality systematic reviews of case–control or cohort studies, high‐quality case–control or cohort studies with a very low risk of confounding or bias and a high probability that the relationship is causal. 2+ = well‐conducted case–control or cohort studies with a low risk of confounding or bias and a moderate probability that the relationship is causal; 2− = case–control or cohort studies with a high risk of confounding or bias and a significant risk that the relationship is not causal; 3 = Non‐analytic studies, for example case reports, case series.
A special assessment of possible publication bias or selective reporting was not performed. There were no clues indicating that data within studies were missing. Several studies were industrially sponsored.
Summary measures and synthesis of results
In the majority of included studies, the investigated patients were subdivided into different groups, for example, to compare different loading protocols, anchorage systems, implant numbers or implant types. Whenever possible, data of these groups were recorded separately so that the statistical analysis incorporated more study populations than indicated by the number of included studies.
The primary outcome of the meta‐analysis was the estimated implant loss rate per 100 implant years in the edentulous maxilla and mandible depending on type of prosthesis (fixed or removable), type of attachment (bar/ball/telescopic crowns, screw‐retained/cemented), and implant number. This rate describes, for example, the risk of an implant loss regarding 100 implants over the course of 1 year or the risk of an implant loss regarding 10 implants over 10 years.
Based on these implant loss rates, 3‐ and 5‐year implant survival rates were estimated.
For simplification, implant numbers were categorized for both jaws. For the mandible, these categories were as follows: one implant, two implants, four implants, and ≥5 implants. For the maxilla, a subdivision was chosen as follows: <4 implants, four implants, and ≥6 implants. Whenever information on the exact implant number per patient could not be extracted, further subcategories were chosen (2–4 implants and 4–6 in the mandible, and 5–6 implants in the maxilla). Data of these overlapping categories were used to strengthen the overall analysis, but were not included for any comparisons. The same applies to missing or not extractable information of other categories (e.g., loading protocol or implant surface, declared as “not applicable”). Tables 3 and 4 illustrate in detail which particular category was “not applicable”. The number of included study populations for each analysis is shown in the Tables, as well.
Table 3.
Study characteristics according to jaw
| Study (Year of publication) | Study design | Jaw | Type of prosthesis | Type of anchorage | Implant system (as reported by the authors) | Loading protocol | Total number of implants | Total number of prostheses | Follow‐up period (years) |
|---|---|---|---|---|---|---|---|---|---|
| Agliardi et al. (2012) | Prospective | Maxilla | Fixed | Screw‐retained | Brånemark, Nobel Speedy (Nobel Biocare) | Immediate | 192 | 32 | 4.6 |
| Collaert & De Bruyn (2008) | Prospective | Maxilla | Fixed | Screw‐retained | TiOblast Astra Tech (Dentsply) | Immediate | 195 | 25 | 3 |
| De Santis et al. (2012) | Prospective | Maxilla | Fixed | Screw‐retained | n.a. | Conventional | 154 | 20 | 4.3 |
| Degidi et al. (2010) | Prospective | Maxilla | Fixed | Screw‐retained | Xive (Dentsply) | Immediate | 210 | 30 | 3 |
| Fischer & Stenberg (2012) | Prospective | Maxilla | Fixed | Screw‐retained | Esthetic Plus SLA (Straumann) | Immediate/conventional | 142 | 24 | 10 |
| Mertens et al. (2012) | Prospective | Maxilla | Fixed | Screw‐retained | Astra Tech, Dentsply | Conventional | 106 | 17 | 11.3 |
| Naert et al. (1998) | Prospective | Maxilla | Fixed | Screw‐retained | Brånemark (Nobel Biocare) | Conventional | 53 | 13 | 3 |
| Nyström et al. (2009b) | Prospective | Maxilla | Fixed | Screw‐retained | Brånemark (Nobel Biocare) | Conventional | 167 | 26 | 13 |
| Nyström et al. (2009a) | Prospective | Maxilla | Fixed | Screw‐retained | Brånemark (Nobel Biocare) | Conventional | 334 | 44 | 11 |
| Richter & Knapp (2010) | Prospective | Maxilla | Removable | Telescopic crown, locator | Osseotite (Biomet 3i) | Conventional | 44 | 27 | 5 |
| Sjöström et al. (2007) | Prospective | Maxilla | Fixed | Screw‐retained | Brånemark (Nobel Biocare) | Conventional | 222 | 29 | 3 |
| Zitzmann & Marinello (2000b) | Prospective | Maxilla | Fixed | Screw‐retained | Brånemark (Nobel Biocare) | Conventional | 84 | 10 | 3.3 |
| Zou et al. (2013) | Prospective | Maxilla | Removable | Telescopic crown, bar, locator | ITI (Straumann) | Conventional | 120 | 30 | 3 |
| Akoglu et al. (2011) | Prospective | Mandible | Removable | Ball | ITI (Straumann), Swiss Plus (Zimmer Dental), Astra Tech (Dentsply) | Conventional | 72 | 36 | 5 |
| Arvidson et al. (1998) | Prospective | Mandible | Fixed | Screw‐retained | Astra Tech (Dentsply) | Conventional | 618 | 107 | 5 |
| Arvidson et al. (2008) | Prospective, multicenter | Mandible | Fixed | Screw‐retained | ITI Monotype SLA (Straumann) | Early | 250 | 61 | 3 |
| Behneke et al. (2002) | Prospective | Mandible | Removable | Bar | ITI (Straumann) | Conventional | 340 | 100 | 5.8 |
| Cehreli et al. (2010) | RCT | Mandible | Removable | Ball | SLA (Straumann), Brånemark TiUnite (Nobel Biocare) | Early | 56 | 28 | 5 |
| Chiapasco & Gatti (2003) | Prospective | Mandible | Removable | Bar | Ha‐Ti (Mathys Dental), ITI (Straumann), Brånemark Conical (Nobel Biocare), Frialoc (Dentsply) | Immediate | 328 | 82 | 5.2 |
| Cooper et al. (2008) | Prospective | Mandible | Removable | Ball | Friatec (Dentsply) | Conventional | 118 | 59 | 5 |
| Cordioli et al. (1997) | Prospective | Mandible | Removable | Ball | Biomet 3i | Conventional | 21 | 21 | 5 |
| De Bruyn et al. (2008) | Prospective | Mandible | Fixed | Screw‐retained | TiOblast Astra Tech (Dentsply) | Immediate | 125 | 25 | 3 |
| Ekelund et al. (2003)/Lindquist et al. (1996) | Prospective | Mandible | Fixed | Screw‐retained | Standard Brånemark (Nobel Biocare) | Conventional | 273 | 47 | 21.5 |
| Eliasson et al. (2010) | Prospective, randomized | Mandible | Fixed | Screw‐retained | Paragon TPS (Zimmer Dental) | Conventional | 168 | 29 | 5 |
| Elsyad et al. (2012) | RCT | Mandible | Removable | Ball | Spectra System Screw Plant (Implant Direct LLC) | Immediate/conventional | 72 | 36 | 3 |
| Engquist et al. (2005) | Prospective, controlled | Mandible | Fixed | Screw‐retained | Standard Brånemark, Brånemark conical 1‐piece, Brånemark Mk II (Nobel Biocare) | Early/conventional | 432 | 108 | 3 |
| Gotfredsen & Holm (2000) | Prospective, randomized | Mandible | Removable | Bar, ball | Astra Tech (Dentsply) | Conventional | 52 | 26 | 5 |
| Harder et al. (2011) | Prospective | Mandible | Removable | Ball | Camlog Promote screw line (Camlog) | Conventional | 11 | 11 | 3.6 |
| Heijdenrijk et al. (2006) | Prospective, randomized | Mandible | Removable | Bar | IMZ TPS, solid screw TPS (Straumann) | Conventional | 120 | 60 | 5 |
| Heschl et al. (2013) | Prospective | Mandible | Removable | Bar | Xive S plus (Dentsply) | Conventional | 156 | 39 | 5 |
| Krennmair et al. (2008) | Prospective, randomized | Mandible | Removable | Bar | IMZ (Dentsply), Frialoc (Dentsply), Camlog root line (Camlog) | Conventional | 204 | 51 | 5 |
| Krennmair et al. (2011) | Prospective, randomized | Mandible | Removable | Ball, telescopic crown | Camlog root line (Camlog) | Conventional | 50 | 25 | 5 |
| Krennmair et al. (2012) | Prospective, randomized | Mandible | Removable | Bar, telescopic crown | Camlog root line/screw line (Camlog) | Conventional | 204 | 51 | 3 |
| Lethaus et al. (2011) | Prospective | Mandible | Removable | Bar | SLA (Straumann) | Early | 70 | 14 | 5 |
| Liddelow & Henry (2010) | Prospective | Mandible | Removable | Ball | Brånemark Mk III TiUnite, Brånemark Mk III machined (Nobel Biocare) | Immediate | 32 | 32 | 3 |
| Lorenzoni et al. (2013) | Prospective | Mandible | Removable | Bar | Xive S Plus (Dentsply) | Immediate/conventional | 160 | 40 | 5 |
| Meijer et al. (2004) | RCT | Mandible | Removable | Bar | IMZ (Dentsply), Brånemark (Nobel Biocare) | Conventional | 122 | 61 | 10 |
| Meijer et al. (2009b) | Prospective | Mandible | Removable | Bar | IMZ TPS (Dentsply), Brånemark (Nobel Biocare), ITI solid screw TPS (Straumann) | Conventional | 180 | 90 | 10 |
| Meijer et al. (2009a) | Prospective | Mandible | Removable | Bar | IMZ TPS (Dentsply) | Conventional | 180 | 60 | 10 |
| Murphy et al. (2002) | Prospective | Mandible | Fixed | Screw‐retained | Astra Tech (Dentsply) | Conventional | 131 | 26 | 5 |
| Schwarz et al. (2010) | Prospective | Mandible | Fixed | Screw‐retained | Frialoc (Dentsply) | Early | 158 | 37 | 4.5 |
| Stoker et al. (2012) | RCT | Mandible | Removable | n.a. | 1‐stage TPS Bonefit (Straumann) | Conventional | 296 | 110 | 8.3 |
| Testori et al. (2004) | Prospective | Mandible | Fixed | Screw‐retained | Osseotite, dual acid‐etched, cylindrical, screw‐shaped (3i) | Immediate | 116 | 19 | 3.2 |
| Van de Velde et al. (2007) | Prospective | Mandible | Fixed | Screw‐retained | Brånemark Mk III/Mk IV (Nobel Biocare) | Immediate | 91 | 18 | 3.8 |
| Vroom et al. (2009) | Prospective | Mandible | Removable | Bar | Astra Tech turned/tioblasted (Dentsply) | Conventional | 80 | 20 | 12 |
| Weinländer et al. (2010) | Prospective | Mandible | Removable | Bar | IMZ cylindric, Frialoc (Denstply), Camlog screw line (Camlog) | Conventional | 252 | 76 | 5 |
| Akca et al. (2010) | Prospective | Both jaws | Removable | Bar | ITI SLA/TPS (Straumann) | Conventional | 124 | 35 | 4.9 |
| Bergendal & Engquist (1998) | Prospective | Both jaws | Removable | Bar, ball | Brånemark (Nobel Biocare) | Conventional | 115 | 50 | 5.2 |
| Covani et al. (2012) | Prospective | Both jaws, only maxilla included | Fixed | Screw‐retained | Ossean (Intra Lock Int) | Immediate | 128 | 16 | 3.6 |
| Crespi et al. (2012) | Prospective | Both jaws | Fixed | Screw‐retained | PAD system (Sweden‐Martina) | Immediate | 176 | 44 | 3 |
| Jemt et al. (1996)/Watson et al. (1997) | Prospective | Both jaws | Removable | Bar | Brånemark (Nobel Biocare) | Conventional | 315 | 133 | 5 |
| Örtorp & Jemt (2012) | Prospective | Both jaws | Fixed | Screw‐retained | Brånemark (Nobel Biocare) | Conventional | 728 | 129 | 10 |
| Rasmusson et al. (2005) | Prospective | Both jaws | Fixed | Screw‐retained | TiOblast Astra Tech (Denstply) | Conventional | 199 | 36 | 10 |
| Romeo et al. (2004) | Prospective | Both jaws | Removable | n.a. | ITI SLA/TPS (Straumann) | Conventional | 126 | 37 | 3.9 |
Table 4.
Estimated implant loss rate and corresponding implant survival for edentulous maxillae with fixed and removable prostheses categorized by number of implants per patient
| Study | Subgroups within study | Number of implants per patient | Total number of implants | Type of prosthesis and anchorage | Number of post‐loading implant losses | Total implant exposure time (implant years) | Estimated implant loss (per 100 implant years) | Estimated implant survival after 5 years (%) |
|---|---|---|---|---|---|---|---|---|
| Richter & Knapp | Locator | <4a | 14 | Removable, BL | 12 | 43.1 | 27.8 | 24.6 |
| Telescopic crowns | <4a | 30 | Removable, TC | 18 | 119.5 | 15.1 | 47.1 | |
| Bergendal & Engquist | Bar | <4a | 29 | Removable, BR | 6 | 140.3 | 4.3 | 80.7 |
| Ball | <4a | 18 | Removable, BL | 7 | 88.0 | 8.0 | 67.2 | |
| Romeo et al. | n.a. | <4a | 42 | Removable | 246.0 | 1.2 | 94.1 | |
| Naert et al. | n.a. | 4 | 53 | Removable, BR | 3 | 135.9 | 2.21 | 89.4 |
| Akca et al. | n.a. | 4 | 44 | Removable, BR | 1 | 210.7 | 0.5 | 97.6 |
| Crespi et al. | n.a. | 4 | 96 | Fixed, SR | 1 | 285.3 | 0.35 | 98.3 |
| Jemt/Watson et al. | n.a. | 4 | 117 | Removable, BR | 21 | 375.5 | 5.6 | 75.0 |
| Zou et al. | Telescopic crowns | 4 | 40 | Removable, TC | 0 | 120.0 | 0 | 100 |
| Bar | 4 | 40 | Removable, BR | 0 | 120.0 | 0 | 100 | |
| Locator | 4 | 40 | Removable, BL | 0 | 120.0 | 0 | 100 | |
| Agliardi et al. | n.a. | ≥6 | 192 | Fixed, SC | 0 | 576.0 | 0 | 100 |
| Fischer & Stenberg | n.a. | 5–6 | 142 | Fixed, SC | 4 | 1095.0 | 0.4 | 98.2 |
| Rasmusson et al. | n.a. | 5–6 | 91 | Fixed, SC | 0 | 787.0 | 0 | 100 |
| Collaert & De Bruyn | n.a. | ≥6 | 195 | Fixed, SC | 0 | 529.0 | 0 | 100 |
| De Santis et al. | n.a. | ≥6 | 154 | Fixed, SC | 0 | 780.0 | 0 | 100 |
| Degidi et al. | n.a. | ≥6 | 210 | Fixed, SC | 1 | 630.1 | 0.2 | 99.1 |
| Mertens et al. | n.a. | ≥6 | 106 | Fixed, SC | 2 | 1050.9 | 0.2 | 99.1 |
| Nytröm et al. | n.a. | ≥6 | 167 | Fixed, SC | 5 | 2132.0 | 0.2 | 98.8 |
| Nyström et al. | n.a. | ≥6 | 334 | Fixed, SC | 4 | 3674.0 | 0.1 | 99.5 |
| Sjöström et al. | n.a. | ≥6 | 222 | Fixed, SC | 8 | 197.5 | 4.1 | 81.3 |
| Zitzmann & Marinello | n.a. | ≥6 | 84 | Fixed, SC | 0 | 820.0 | 0 | 100 |
| Covani et al. | n.a. | ≥6 | 128 | Fixed, SC | 0 | 460.8 | 0 | 100 |
| Örtorp et al. | n.a. | ≥6 | 355 | Fixed, SC | 17 | 2042.5 | 0.8 | 95.9 |
BL, ball; BR, bar; TC, telescopic crown; SC, screw‐retained; n.a., not applicable.
This category was excluded from further statistical analysis.
Ball and locator attachments were summarized in one category (“ball”). The category “bar” included all types of bars. The category “telescopic crowns” included all types of double crowns.
Additional subgroup analyses were carried out to calculate the estimated implant loss rates per 100 implant years with regard to loading protocol (immediate vs. conventional) and implant surface (rough vs. machined).
According to Pjetursson et al. (2007) implant loss rates were calculated by dividing the number of events (loss after loading) by the total exposure time of the implants. The total exposure time consisted of a) the exposure time of the implants being followed for the complete observation period, b) the exposure time of the implants until loss, and c) the exposure time until an implant dropout had occurred (withdrawal for different reasons, patient's death/illness, patient missed recall or moved). If the explicit information on an implant was not provided, that is time of dropout or loss, the total exposure time was calculated by multiplying the number of initially inserted implants (minus losses before loading) by the mean follow‐up time. Implant loss rates were calculated for every study population by dividing the number of events (post‐loading losses) by the total implant exposure time in years.
A Poisson regression models with a logarithmic link function and the logarithm of total exposure time as an offset variable were fitted to the data to obtain a cumulative estimate for the appropriate implant loss rate and a corresponding 95% confidence interval. 3‐ and 5‐year implant survival rates and related 95% confidence limits were derived from the equation S(t) = e λt where t denotes the time and λ the implant loss rate by assuming constant event rates over time. Comparison of loss rates in different subgroups were contrasted by descriptive P‐values resulting from the correspondent Poisson regression model. Factors, which showed significant influence on implant loss in the univariate analysis, were simultaneously analyzed in a multivariate Poisson regression model. To explore possible effect modifiers, all two‐way interactions between factors were evaluated within this model. The final Poisson regression model included all main effects and significant two‐way interactions. P‐values less than or equal to 0.05 were regarded as statistically meaningful. Due to the explorative nature of the study, no adjustment to the significance level was made. All statistical analyses were performed using the software SAS (SAS Institute Inc., Cary, NC, USA, Version 9.3).
Results
Literature search
The search strategy, as described in Figure 1 and Table 1, resulted in an initial number of 4317 titles. 3823 titles could be excluded after screening. The manual search revealed 80 further abstracts.
Figure 1.
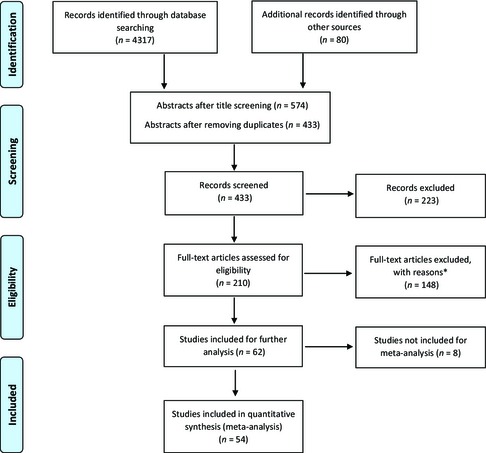
Modified PRISMA flow chart: study selection process. *zygoma, pterygomaxillary, transmandibular or other region, no clinical examination/no regular follow‐up, observation <3 year, no titanium implant, no clinical study, not edentulous, retrospective/study design unclear, no separate reporting of edentulous jaws/removable or fixed prostheses, same patient cohort at earlier stage, case report, no survival rate nor implant loss, different emphasis, study being judged with “2−” according to SIGN (high risk of bias)
After filtering the abstracts and excluding the duplicates, the reviewers decided to conduct a full‐text analysis of 210 publications. Fifty‐six publications, describing 54 studies, could be considered for a quantitative analysis. The interreviewer agreement was found to be κ = 0.9 (SD 0.098) concerning final study selection.
Study characteristics
The included clinical trials were published within an almost 20‐year period (1996–2013). Ten of them investigated the edentulous maxilla, 36 the edentulous mandible, and eight investigated both jaws. Four studies were RCTs, and the rest were prospective clinical studies, sometimes described as “prospective, randomized” or “prospective, controlled” (Table 2).
In the majority of studies, observation periods between 3 and 10 years were stated, and in four studies, 11 or more years of follow‐up were reported (Table 3). Within the 54 included clinical trials, altogether 81 study populations have been investigated. Whenever subgroups were described in a study, this information is shown in Tables 4 and 5. In 30 study populations, patients were restored with fixed full‐arch prostheses, and in the residual 51 study populations, patients received removable overdentures. All of the fixed, definitive prostheses had a metal framework (Au, CoCr, or Ti), veneered with acrylic resin or ceramic and were screw‐retained. None of the studies reported on cemented or adhesively fixed prostheses. The removable prostheses were generally fabricated out of acrylic resin, reinforced with a metal framework or reinforcement (CoCr) and attached by different anchorage systems (ball, locator, telescopic crown as un‐splinted retention elements and different bars enabling a primary splinting).
Table 5.
Estimated implant loss rate and corresponding implant survival for edentulous mandible with fixed and removable prostheses categorized by number of implants per patient
| Study | Subgroups within study | Number of implants per patient | Total number of implants* | Type of prosthesis and anchorage | Number of post‐loading implant losses | Total implant exposure time (implant years) | Estimated implant loss (per 100 implant years) | Estimated implant survival after 5 years (%) |
|---|---|---|---|---|---|---|---|---|
| Cordioli et al. | n.a. | 1 | 21 | Removable, BL | 0 | 95.0 | 0 | 100 |
| Harder et al. | n.a. | 1 | 11 | Removable, BL | 0 | 38.9 | 0 | 100 |
| Liddelow et al. | Machined | 1 | 7 | Removable, BL | 3 | 12.4 | 24.2 | 25.1 |
| Rough | 1 | 25 | Removable, BL | 0 | 36.5 | 0 | 100 | |
| Akoglu et al. | n.a. | 2 | 72 | Removable, BL | 0 | 360.0 | 0 | 100 |
| Cehreli et al. | n.a. | 2 | 56 | Removable, BL | 0 | 230.0 | 0 | 100 |
| Cooper et al. | n.a. | 2 | 118 | Removable, BL | 0 | 557.0 | 0 | 100 |
| Elsyad et al. | Immed. load. | 2 | 36 | Removable, BL | 0 | 96.0 | 0 | 100 |
| Convent. load. | 2 | 36 | Removable, BL | 4 | 92.3 | 4.3 | 80.1 | |
| Gotfredsen & Holm | Bar | 2 | 22 | Removable, BL | 0 | 110.0 | 0 | 100 |
| Ball | 2 | 30 | Removable, BL | 0 | 148.0 | 0 | 100 | |
| Heijdenrijk et al. | 1‐stage | 2 | 40 | Removable, BL | 0 | 381.1 | 0 | 100 |
| 2‐stage | 2 | 80 | Removable, BL | 2 | 192.0 | 1.0 | 94.9 | |
| Krennmair et al. | Ball | 2 | 26 | Removable, BL | 0 | 122.0 | 0 | 100 |
| Telesc. crowns | 2 | 24 | Removable, TC | 0 | 108.0 | 0 | 100 | |
| Meijer et al. | IMZ | 2 | 58 | Removable, BR | 1 | 560.0 | 0.2 | 99.1 |
| Brå | 2 | 64 | Removable, BR | 4 | 536.0 | 0.7 | 96.3 | |
| Meijer et al. | Brå | 2 | 60 | Removable, BR | 0 | 546.0 | 0 | 100 |
| IMZ | 2 | 60 | Removable, BR | 3 | 570.0 | 0.5 | 97.4 | |
| ITI Str | 2 | 60 | Removable, BR | 0 | 562.0 | 0 | 100 | |
| Meijer et al. | 2 implants | 2 | 60 | Removable, BR | 3 | 1008.5 | 0.3 | 98.5 |
| Weinländer et al. | 2 implants | 2 | 48 | Removable, BR | 0 | 216.0 | 0 | 100 |
| Jemt et al./Watson et al. | n.a. | 2 | 198 | Removable, BR | 7 | 880.0 | 0.8 | 96.1 |
| Behneke et al. | n.a. | 2‐4 | 340 | Removable, BR | 0 | 1530.0 | 0 | 100 |
| Stoker et al. | n.a. | 2‐4 | 296 | Removable, n.a. | 9 | 2124.8 | 0.4 | 97.9 |
| Akca et al. | n.a. | 2‐4 | 80 | Removable, BR | 1 | 392.0 | 0.3 | 98.7 |
| Bergendal & Engquist | Bar | 2‐4 | 39 | Removable, BR | 0 | 187.8 | 0 | 100 |
| Ball | 2‐4 | 29 | Removable, BL | 0 | 140.6 | 0 | 100 | |
| Romeo et al. | n.a. | 2‐4 | 84 | Removable, n.a. | 2 | 472.0 | 0.4 | 97.9 |
| Chiapasco et al. | n.a. | 4 | 328 | Removable, BR | 7 | 1704.0 | 0.4 | 98.0 |
| Engquist et al. | 1‐stage Brå/Str | 4 | 120 | Fixed, SC | 3 | 331.0 | 0.9 | 95.6 |
| 2‐stage Brå/Str | 4 | 120 | Fixed, SC | 0 | 347.0 | 0 | 100 | |
| 1‐stage Brå 1‐piece | 4 | 88 | Fixed, SC | 1 | 243.0 | 0.4 | 98.0 | |
| 1‐stage Brå Mk III | 4 | 104 | Fixed, SC | 7 | 299.0 | 2.3 | 88.8 | |
| Heschl et al. | n.a. | 4 | 156 | Removable, BR | 1 | 745.0 | 0.1 | 99.3 |
| Krennmair et al. | n.a. | 4 | 204 | Removable, BR | 0 | 768.0 | 0 | 100 |
| Krennmair et al. | Bar | 4 | 104 | Removable, BR | 0 | 296.0 | 0 | 100 |
| Telesc. crown | 4 | 100 | Removable, TC | 0 | 276.0 | 0 | 100 | |
| Lorenzoni et al. | Convent. load. | 4 | 80 | Removable, BR | 0 | 400.0 | 0 | 100 |
| Immed. load. | 4 | 80 | Removable, BR | 0 | 400.0 | 0 | 100 | |
| Meijer et al. | n.a. | 4 | 120 | Removable, BR | 0 | 586.3 | 0 | 100 |
| Vroom et al. | n.a. | 4 | 80 | Removable, BR | 0 | 852.0 | 0 | 100 |
| Weinländer et al. | n.a. | 4 | 204 | Removable, BR | 0 | 944.0 | 0 | 100 |
| Crespi et al. | n.a. | 4 | 80 | Fixed, SC | 2 | 273.6 | 0.7 | 96.4 |
| Arvidson et al. | n.a. | 4‐6 | 618 | Fixed, SC | 0 | 2809.0 | 0 | 100 |
| Arvidson et al. | n.a. | 4 | 250 | Fixed, SC | 3 | 511.3 | 0.6 | 97.1 |
| De Bruyn et al. | n.a. | ≥5 | 125 | Fixed, SC | 0 | 350.0 | 0 | 100 |
| Ekelund et al./Lindquist et al. | n.a. | ≥5 | 273 | Fixed, SC | 1 | 4835.0 | 0.02 | 99.9 |
| Eliasson et al. | n.a. | ≥5 | 168 | Fixed, SC | 0 | 756.0 | 0 | 100 |
| Lethaus et al. | n.a. | ≥5 | 70 | Removable, BR | 0 | 286.0 | 0 | 100 |
| Murphy et al. | n.a. | ≥5 | 131 | Fixed, SC | 0 | 635.0 | 0 | 100 |
| Schwarz et al. | n.a. | ≥5 | 158 | Fixed, SC | 7 | 693.3 | 1.0 | 95.1 |
| Testori et al. | n.a. | ≥5 | 116 | Fixed, SC | 3 | 284.4 | 1.1 | 94.8 |
| Van de Velde et al. | n.a. | 4–6 | 91 | Fixed, SC | 3 | 302.4 | 1.0 | 95.1 |
| Örtorp et al. | n.a. | ≥5 | 373 | Fixed, SC | 0 | 2200.0 | 0 | 100 |
| Rasmusson et al. | n.a. | ≥5 | 108 | Fixed, SC | 0 | 1054.0 | 0 | 100 |
BL, ball; BR, bar; TC, telescopic crown; SC, screw‐retained; n.a., not applicable.
Altogether 2368 patients received 9267 implants. Various implant types with different surface modifications were used (Table 3). All implants were titanium implants with different lengths and diameters. Implant numbers per patient varied between 1 and 6 implants in the mandible and 2 and 10 in the maxilla. The interforaminal area was the preferred area for implant positioning in the mandible. If only one implant was inserted in the edentulous lower jaw, it was located in the midline symphysis, representing the absolute minimal treatment concept. In the maxilla, implant positions were often not described precisely. Only the following authors described the area of implant placement in more detail: Fischer & Stenberg (2012, 2013) located 5–6 implants from second premolar to second premolar. Agliardi et al. (2012) and Degidi et al. (2010) placed implants in the anterior area and (tilted) implants in the regions of the anterior and posterior sinus wall. De Santis et al. (2012) inserted 6–10 implants in the positions of former incisors, canines, premolars, and molars.
The results for fixed prostheses presented by Romeo et al. (2004) could not be considered, because only three patients had been provided with a fixed prosthesis. In another trial, the observation period was too short, and therefore, the “removable cases” had to be excluded (Zitzmann & Marinello 2000a,b). Covani et al. (2012) merely included six patients with an edentulous lower jaw, and hence, these cases were not regarded in this review. Some authors observed the same study population but reported on different clinical outcomes in different publications (surgical, periodontal, prosthetic) (Jemt et al. 1996; Watson et al. 1997; Fischer & Stenberg 2012, 2013). Their results were summarized.
Generally, criteria for the inclusion or exclusion of patients were pre‐defined. For obvious reasons, these criteria were not consistent among the studies. Mostly, patients with severe diseases or uncontrolled diabetes, psychological problems, and heavy smokers were excluded. In general, the average age of the patients was between 50 and 60 years, although it is worth mentioning that mean ages were not always provided or sometimes not for all indications being investigated in one particular study (e.g., maxilla or mandible, edentulous or partially edentulous).
In the majority of studies, a 2‐stage surgical procedure and a conventional loading protocol were carried out, but non‐submerged healing (1‐stage surgery) followed by immediate prosthetic loading was applied, as well (Table 3). Pre‐implantological or simultaneous bone augmentation was reported in six studies and ranged from rather simple procedures (e.g., filling of post‐extraction sites (Agliardi et al. 2012; Zou et al. 2013) to complex reconstructions such as Le Fort I osteotomies with interpositional bone grafts (Nyström et al. 2009b; De Santis et al. 2012) or onlay osteoplastics (Nyström et al. 2009a). Sjöström et al. (2007) either applied inlay, onlay, or interpositional grafting with free iliac grafts. Covani et al. (2012) partly carried out simultaneous sinus floor elevation with the ostetome technique. Richter & Knapp (2010) performed either bone splitting or bone spreading but no augmentation in case of heavy bone resorption. Three other studies (De Bruyn et al. 2008; Heschl et al. 2013; Lorenzoni et al. 2013) reported not to have applied augmentative or regenerative procedures. The rest of the studies cannot be commented as the authors did not make any statements about bone augmentation.
The examination of patients usually comprised the recording of several indices, that is, plaque indices, bleeding indices, and pocket depth. Implant stability was checked, sometimes by means of radio‐frequency analysis or “damping capacity assessment” (Heschl et al. 2012). In the majority of the included studies, a radiographic examination was performed to measure marginal bone level changes. Several techniques were used for this, for example, standardized radiographic holders to achieve the highest possible reproducibility. In many cases, merely panoramic radiographs were compared.
Overall implant survival and loss
Results of individual patient groups
Estimated implant survival rates after 5 years ranged from 89.0% to 100% for fixed prostheses concerning both jaws (Tables 4 and 5). For removable prostheses, estimated survival rates of 24.9% up to 100% were calculated. The very low survival rate of 24.8%, with an associated annual implant loss rate of 27.8 per 100 implant years, is related to a very small patient group (n = 7) that was restored with merely 2 diameter‐reduced implants and an overdenture in the edentulous maxilla (Richter & Knapp 2010).
Synthesis of results
Comparing the overall implant loss rate per 100 implant years for fixed vs. removable prostheses, a statistically significant difference could be assessed (P < 0.0001) if the category <4 implants (maxilla) was included (Tables 6 and 7). Excluding this latter category, there was also a significantly higher implant loss rate per 100 implant years comparing fixed and removable restorations (0.23 [95% CI 0.18; 0.29] vs. 0.35 [95% CI 0.28; 0.44]; P = 0.0148).
Table 6.
Overall comparison
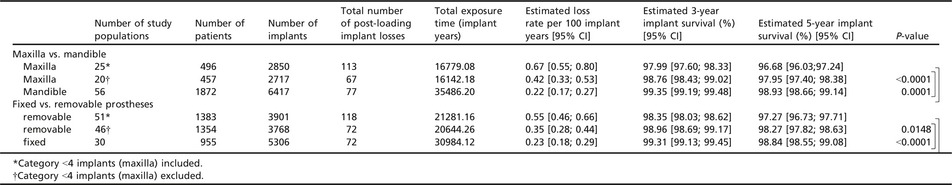
Table 7.
Overall comparison bar vs. ball vs. telescopic crown (category <4 implants excluded)
| Number of study populations | Number of patients | Number of implants | Total number of post‐loading implant losses | Total exposure time (implant years) | Estimated loss rate per 100 implant years [95% CI] | Estimated 3‐year implant survival (%) [95% CI] | Estimated 5‐year implant survival (%) [95% CI] | P‐value | |
|---|---|---|---|---|---|---|---|---|---|
| Ball | 13 | 267 | 507 | 7 | 2048.73 | 0.34 [0.16; 0.72] | 98.98 [97.87; 99.51] | 98.31 [96.46; 99.20] | |
| Bar | 28 | 928 | 2777 | 54 | 15494.73 | 0.35 [0.27; 0.46] | 98.96 [98.64; 99.20] | 98.27 [97.73; 98.66] | 0.9607 |
| Telescopic crown | 3 | 47 | 164 | 0 | 504.0 | Not estimable | |||
| Bar | 28 | 928 | 2777 | 54 | 15494.73 | 0.35 [0.27; 0.46] | 98.96 [98.64; 99.20] | 98.27 [97.73; 98.66] | |
| Ball | 13 | 267 | 507 | 7 | 2048.73 | 0.34 [0.16; 0.72] | 98.98 [97.87; 99.51] | 98.31 [96.46; 99.20] | |
| Telescopic crown | 3 | 47 | 164 | 0 | 504.0 | Not estimable | |||
Regarding different attachment types for overdentures in both jaws, no significant differences could be detected for ball vs. bar anchorage. The estimated implant loss rate per 100 implant years was similar (0.34 [95% CI 0.16; 0.72] vs. 0.35 [95% CI 0.27; 0.46] per 100 implant years; P = 0.9607). The comparison of bar vs. telescopic crown and ball vs. telescopic crown was not possible (no implant losses, merely three study populations included (not regarding the study of Richter & Knapp (2010), as it belonged to the group <4 implants, see below).
Implant survival and loss in the maxilla
Results of individual patient groups
Concerning the estimated 3‐ and 5‐year implant survival rates of both, removable and fixed implant‐supported prostheses, these were higher than 95% for the majority of study populations (Table 4). For five of the investigated groups, the estimated implant survival rate was <90% (67.2–89.4%) and for two groups even <50% (24.8% and 47.2%) after 5 years. The low survival rates were associated with an implant number of <4, and removable overdentures and corresponding annual implant loss rates were between 8.0 and 27.8.
Synthesis of results and subgroup analyses
If fixed and removable implant prostheses were compared, the removable prostheses had a significantly higher implant loss rate (0.28 [95% CI 0.21; 0.38] vs. 2.31 [95% CI 1.56; 3.42]; P < 0.0001) (Table 8). Comparing the implant numbers <4 vs. 4 implants in the “removable group”, the risk of implant loss is more than three times higher with <4 implants (7.22 [95% CI 5.41; 9.64] vs. 2.31 [95% CI 1.56; 3.42]; P < 0.0001). Therefore, this category (<4 implants in the maxilla) was excluded from further statistical analysis.
Table 8.
Comparison in the maxilla
| Number of study populations | Number of patients | Number of implants | Number of post‐loading implant losses | Total exposure time (implant years) | Estimated loss rate per 100 implant years [95% CI] | Estimated 3‐year implant survival (%) [95% CI] | Estimated 5‐year implant survival (%) [95% CI] | P‐value | |
|---|---|---|---|---|---|---|---|---|---|
| Fixed vs. removable prostheses (category <4 implants excluded) | |||||||||
| removable | 6 | 84 | 334 | 25 | 1082.10 | 2.31 [1.56; 3.42] | 93.30 [98.91; 99.41] | 89.09 [84.28; 92.50] | |
| fixed | 14 | 363 | 2383 | 42 | 15060.08 | 0.28 [0.21; 0.38] | 99.17 [98.87; 99.38] | 98.62 [98.13; 98.97] | <0.0001 |
| Removable: <4 implants vs. 4 implants | |||||||||
| <4 | 5 | 49 | 133 | 46 | 636.90 | 7.22 [5.41; 9.64] | 80.52 [74.88; 85.02] | 69.70 [61.75; 76.30] | |
| 4 | 6 | 84 | 334 | 25 | 1082.10 | 2.31 [1.56; 3.42] | 93.30 [90.25; 95.42] | 89.09 [84.29; 92.50] | <0.0001 |
| Fixed: ≥6 (no comparison feasible) | |||||||||
| ≥6 | 11 | 303 | 2057 | 37 | 13099.78 | 0.28 [0.20; 0.39] | 99.16 [98.84; 99.39] | 98.60 [98.07; 98.98] | |
Fixed restorations with six or more implants demonstrated an implant loss rate of 0.28 [95% CI 0.20; 0.39] per 100 implant years. A comparison of this latter category with lower implant numbers was not possible due to a lack of studies.
Implant survival and loss in the mandible
Results of individual patient groups
Estimated implant survival rates after 3 and 5 years for fixed restorations were generally very high (95–100%) (Table 5). For one patient group, implant survival was <90% (88.8%). Also the results for removable prostheses revealed high survival rates. Here, a small study population being treated with one machined implant and an overdenture stands out in a negative sense with an implant loss rate of 24.2 per 100 implant years and a corresponding 5‐year survival estimation of 25.1%.
Synthesis of results
Comparing the estimated implant loss rates per 100 implant years in the mandible for fixed and removable prostheses, no significant difference could be detected (0.19 [95% CI 0.13; 0.27] vs. 0.24 [95% CI 0.18; 0.32]; P = 0.2980) (Tables 9 and 10). Comparing different implant numbers, less implants always resulted in significantly higher implant loss estimations (1 vs. 2, 2 vs. 4 (removable prostheses) 4 vs. ≥5 implants (fixed prostheses)). No statistically significant differences were revealed regarding ball vs. bar attachment (0.34 [95% CI 0.16; 0.72] vs. 0.20 [95% CI 0.14; 0.28]; P = 0.1499). Four implants with a fixed restoration resulted in a significantly higher (P < 0.0001) estimated implant loss rate (0.79 [95% CI 0.49; 1.30]) than with a removable restoration (0.11 [95% CI 0.06; 0.23]).
Table 9.
Comparison in the mandible
| Number of study populations | Number of patients | Number of implants | Total number of post‐loading implant losses | Total exposure time (implant years) | Estimated loss rate per 100 implant years [95% CI] | Estimated 3‐year implant survival (%) [95% CI] | Estimated 5‐year implant survival (%) [95% CI] | P‐value | |
|---|---|---|---|---|---|---|---|---|---|
| Fixed vs. removable prostheses | |||||||||
| Removable | 40 | 1280 | 3494 | 47 | 19562.16 | 0.24 [0.18; 0.32] | 99.28 [99.05; 99.46] | 98.81 [98.41; 99.10] | |
| Fixed | 16 | 592 | 2923 | 30 | 15924.04 | 0.19 [0.13; 0.27] | 99.44 [99.20; 99.61] | 99.06 [98.66; 99.34] | 0.2980 |
| Fixed: 4 implants vs. ≥5implants | |||||||||
| 4 | 6 | 189 | 762 | 16 | 2004.85 | 0.80 [0.49;1.30] | 97.63 [96.17; 98.54] | 96.10 [93.69; 97.59] | |
| ≥5 | 8 | 278 | 1452 | 11 | 10807.77 | 0.10 [0.06;0.18] | 99.70 [99.45; 99.83] | 99.49 [99.10; 99.72] | <0.0001 |
| Removable: 1 implant vs. 2 implants | |||||||||
| 1 | 4 | 66 | 66 | 3 | 182.81 | 1.64 [0.53; 5.09] | 95.20 [85.84; 98.42] | 92.13 [77.53; 97.38] | |
| 2 | 19 | 557 | 1134 | 24 | 7274.90 | 0.33 [0.22; 0.49] | 99.02 [98.53; 99.34] | 98.36 [97.58; 98.91] | 0.0088 |
| Removable: 2 implants vs. 4 implants | |||||||||
| 2 | 19 | 557 | 1134 | 24 | 7274.90 | 0.33 [0.22; 0.49] | 99.02 [98.53; 99.34] | 98.36 [97.58; 98.91] | |
| 4 | 10 | 365 | 1366 | 8 | 6971.25 | 0.11 [0.06; 0.23] | 99.66 [99.31; 99.82] | 99.45 [98.86; 99.70] | 0.0097 |
| 4 Implants: fixed vs. removable | |||||||||
| removable | 10 | 365 | 1366 | 8 | 6971.25 | 0.11 [0.06; 0.23] | 99.66 [99.31; 99.82] | 99.43 [98.86; 99.70] | |
| fixed | 6 | 189 | 762 | 16 | 2004.85 | 0.79 [0.49; 1.30] | 97.63 [96.17; 98.54] | 96.10 [93.69; 97.59] | <0.0001 |
Table 10.
Comparison bar vs. ball vs. telescopic crown for mandible
| Number of study populations | Number of patients | Number of implants | Total number of post‐loading implant losses | Total exposure time (implant years) | Estimated loss rate per 100 implant years [95% CI] | Estimated 3‐year implant survival (%) [95% CI] | Estimated 5‐year implant survival (%) [95% CI] | P‐value | |
|---|---|---|---|---|---|---|---|---|---|
| Ball | 13 | 257 | 467 | 7 | 2048.73 | 0.34 [0.16; 0.72] | 98.98 [97.87; 99.51] | 98.31 [96.46; 99.20] | |
| Bar | 24 | 864 | 2523 | 29 | 14652.63 | 0.20 [0.14; 0.28] | 99.41 [99.15; 99.59] | 99.01 [98.61; 99.30] | 0.1499 |
| Telescopic crown | 2 | 37 | 124 | 0 | 384.0 | Not estimable | |||
| Bar | 24 | 864 | 2523 | 29 | 14652.63 | 0.20 [0.14; 0.28] | 99.41 [99.15; 99.59] | 99.01 [98.61; 99.30] | |
| Ball | 13 | 257 | 467 | 7 | 2048.73 | 0.34 [0.16; 0.72] | 98.98 [97.87; 99.51] | 98.31 [96.46; 99.20] | |
| Telescopic crown | 2 | 37 | 124 | 0 | 384.0 | Not estimable | |||
Further subgroup analyses
Implant surface
Machined implants were more prone to implant loss than rough‐surfaced implants, in almost every subgroup (Table 11). Concerning fixed restorations, no significant difference in post‐loading implant loss could be demonstrated comparing machined vs. rough implant surfaces, although machined implant surfaces tend to result in higher loss rates (0.28 [95% CI 0.21; 0.37] vs. 0.19 [95% CI 0.13; 0.28]; P = 0.1177). Furthermore, in the edentulous mandible, no difference in estimated implant loss per 100 implant years between machined and rough implants could be shown (0.25 [95% CI 0.17; 0.36] vs. 0.21 [95% CI 0.16; 0.27]; P = 0.4518).
Table 11.
Machined implant surface vs. rough implant surface (category <4 implants excluded)
| Number of study populations | Number of patients | Number of implants | Total number of post‐loading implant losses | Total exposure time (implant years) | Estimated loss rate per 100 implant years [95% CI] | Estimated 3‐year implant survival (%) [95% CI] | Estimated 5‐year implant survival (%) | P‐value | |
|---|---|---|---|---|---|---|---|---|---|
| Overall comparison | |||||||||
| Machined | 21 | 657 | 2888 | 87 | 21089.63 | 0.41 [0.33; 0.51] | 98.77 [98.48; 99.00] | 97.63 [97.09; 98.02] | |
| Rough | 53 | 1662 | 6246 | 57 | 29123.75 | 0.20 [0.15; 0.25] | 99.41 [99.24; 99.55] | 99.03 [98.74; 99.25] | <0.0001 |
| Fixed (maxilla and mandible) | |||||||||
| Machined | 12 | 393 | 2240 | 49 | 17423.42 | 0.28 [0.21; 0.37] | 99.16 [98.89; 99.36] | 98.17 [97.67; 98.56] | |
| Rough | 16 | 536 | 1714 | 23 | 12145.70 | 0.19 [0.13; 0.28] | 99.43 [99.15; 99.62] | 99.06 [98.59; 99.37] | 0.1177 |
| Removable (maxilla and mandible) | |||||||||
| Machined | 9 | 264 | 648 | 38 | 3666.21 | 1.04 [0.75; 1.42] | 96.94 [95.82; 97.76] | 94.93 [93.15; 96.32] | |
| Rough | 37 | 1059 | 3180 | 34 | 16978.05 | 0.20 [0.14; 0.28] | 99.40 [99.16; 99.57] | 99.01 [98.61; 99.30] | <0.0001 |
| Maxilla (fixed and removable) | |||||||||
| Machined | 7 | 163 | 1162 | 58 | 9377.40 | 0.62 [0.48; 0.80] | 98.16 [97.63; 98.58] | 96.95 [96.08; 97.64] | |
| Rough | 12 | 241 | 1385 | 9 | 5984.78 | 0.15 [0.08; 0.29] | 99.55 [99.14; 99.77] | 99.25 [98.57; 99.61] | <0.0001 |
| Mandible (fixed and removable) | |||||||||
| Machined | 13 | 451 | 1556 | 29 | 11712.23 | 0.25 [0.17; 0.36] | 99.26 [98.94; 99.49] | 98.76 [98.22; 99.15] | |
| Rough | 41 | 1395 | 4730 | 48 | 23138.97 | 0.21 [0.16; 0.27] | 99.38 [99.17; 99.53] | 98.96 [98.63; 99.22] | 0.4518 |
Loading protocols
Both loading protocols, immediate and conventional, exhibited low implant loss rates per 100 implant years, and no statistically significant differences could be shown concerning fixed restorations in both jaws (0.27 [95% CI 0.15; 0.50] vs. 0.17 [0.12; 0.23]; P = 0.1652) (Tables 12 a, b). However, there was a significantly lower risk of implant loss with a conventional loading protocol concerning the overall analysis, removable prostheses, and the edentulous mandible. Merely for an immediate loading in the maxilla, a significantly lower implant loss rate was shown (0.08 [95% CI 0.02; 0.32] vs. 0.49 [95% CI 0.38; 0.62]; P = 0.0125).
Table 12.
(a) Conventional loading vs. immediate loading (category <4 implants excluded). (b) Comparison of immediate loading vs. conventional loading for mandible/fixed and mandible/removable
| Number of study populations | Number of patients | Number of implants | Total number of post‐loading implant losses | Total exposure time (implant years) | Estimated loss rate per 100 implant years [95% CI] | Estimated 3‐year implant survival (%) [95% CI] | Estimated 5‐year implant survival (%) [95% CI] | P‐value | |
|---|---|---|---|---|---|---|---|---|---|
| (a) | |||||||||
| Overall comparison | |||||||||
| Conventional | 56 | 1773 | 6835 | 99 | 42576.93 | 0.24 [0.19; 0.28] | 99.30 [99.15; 99.43] | 98.66 [98.41; 98.91] | |
| Immediate | 14 | 361 | 1532 | 24 | 5936.87 | 0.40 [0.27; 0.60] | 98.79 [98.21; 99.19] | 97.99 [97.03; 98.65] | 0.0151 |
| Fixed (maxilla and mandible) | |||||||||
| Conventional | 17 | 598 | 3512 | 41 | 24693.90 | 0.17 [0.12; 0.23] | 99.50 [99.33; 99.63] | 98.86 [98.51; 99.10] | |
| Immediate | 9 | 209 | 1143 | 10 | 3691.64 | 0.27 [0.15; 0.50] | 99.19 [98.50; 99.56] | 98.65 [97.51; 99.27] | 0.1652 |
| Removable (maxilla and mandible) | |||||||||
| Conventional | 39 | 1175 | 3323 | 58 | 17883.03 | 0.32 [0.25; 0.42] | 99.03 [98.75; 99.25] | 98.41 [97.92; 98.76] | |
| Immediate | 5 | 152 | 389 | 14 | 2245.23 | 0.62 [0.37; 1.05] | 98.15 [96.89; 98.90] | 96.95 [94.89; 98.17] | 0.0282 |
| Maxilla (fixed and removable) | |||||||||
| Conventional | 14 | 296 | 1847 | 61 | 12566.00 | 0.49 [0.38; 0.62] | 98.55 [98.15; 98.87] | 97.60 [96.93; 98.13] | |
| Immediate | 5 | 127 | 731 | 2 | 2688.18 | 0.08 [0.02; 0.32] | 99.75 [99.04; 99.94] | 99.60 [98.40; 99.90] | 0.0125 |
| Mandible (fixed and removable) | |||||||||
| Conventional | 42 | 1477 | 4988 | 38 | 30010.93 | 0.13 [0.09; 0.17] | 99.62 [99.48; 99.72] | 99.35 [99.15; 99.55] | |
| Immediate | 9 | 234 | 801 | 22 | 3455.69 | 0.64 [0.42; 0.97] | 98.12 [97.14; 98.75] | 96.87 [95.28; 97.93] | <0.0001 |
| (b) | |||||||||
| Mandible/fixed | |||||||||
| Conventional | 9 | 386 | 1999 | 5 | 13210.00 | 0.04 [0.02; 0.09] | 99.89 [99.73; 99.95] | 99.80 [99.55; 99.90] | |
| Immediate | 4 | 82 | 412 | 4 | 1210.46 | 0.66 [0.33; 1.32] | 98.04 [96.11; 99.01] | 96.75 [93.61; 98.36] | <0.0001 |
| Mandible/removable | |||||||||
| Conventional | 33 | 1091 | 2989 | 33 | 16800.93 | 0.20 [0.14; 0.28] | 99.41 [99.17; 99.58] | 99.01 [98.61; 99.30] | |
| Immediate | 5 | 152 | 389 | 14 | 2245.23 | 0.62 [0.37; 1.05] | 98.14 [96.89; 98.90] | 96.93 [94.87; 98.17] | 0.0003 |
Multivariate analysis
To explore the independent effects and interrelation between factors influencing the estimated implant loss rate, a multivariate Poisson regression model was fitted to the data of univariate meaningful factors. The first model included the location of implants, the type of prosthesis, the surface of implants, the loading protocol, and the number of implants per patient and all two‐way interaction terms. Due to the sparse distribution of number of implants across the remaining factors, the Poisson regression model did not converge. Thus, the final model was reduced to the location of implants, the type of prosthesis, the surface of implants, and the loading protocol as main effects. Additionally, the significant two‐way interaction between location and loading protocol remained in the model. Within this model, type of prosthesis (P < 0.0001 fixed vs. removable), surface of implants (P = 0.0001 machined vs. rough), and the interaction term between jaw and loading protocol (P = 0.0006) demonstrated significant influence on the estimated implant loss rate. From the significant interaction between jaw and loading protocol, a significant difference between conventional and immediate loading in the mandible (P < 0.0001) and between mandible and maxilla in the conventional loading protocol (P < 0.0001) followed. The comparisons between conventional and immediate loading in the maxilla (P = 0.1745) and between mandible and maxilla in the immediate loading protocol (P = 0.9886) showed no significant differences (Table 13).
Table 13.
Estimates with corresponding standard errors and P‐values resulting from the multivariate Poisson regression model
| Factor/Interaction | Estimate | Standard Error | P‐value |
|---|---|---|---|
| Intercept | −4.7007 | 0.7327 | <0.0001 |
| Jaw | 0.0108 | 0.7610 | 0.9886 |
| Type of prosthesis | −2.4227 | 0.1921 | <0.0001 |
| Surface of implant | 0.7254 | 0.1913 | 0.0001 |
| Loading protocol | 1.0085 | 0.7427 | 0.1745 |
| Jaw‐loading protocol | −2.6806 | 0.7790 | 0.0006 |
| Conventional vs. immediate (mandible) | −1.6721 | 0.2748 | <0.0001 |
| Conventional vs. immediate (maxilla) | 1.0085 | 0.7427 | 0.1745 |
| Mandible vs. maxilla (conventional) | −2.6698 | 0.2048 | <0.0001 |
| Mandible vs. maxilla (immediate) | −0.9976 | 0.2677 | 0.9886 |
Bone augmentation
The analysis of a potential impact of bone augmentation on implant loss or survival was not a part of the focused question and serves as additional information.
Studies reporting on complex augmentative procedures (e.g., Le Fort I, onlay osteoplastic with iliac graft) were already described. Bone augmentation was reported for the maxilla, exclusively. Assuming that complex procedures would have been reported if executed, a comparison of post‐loading implant loss per 100 implant years revealed a significantly higher rate for non‐augmented (0.93 [95% CI 0.76152; 1.14; 22 study populations) vs. augmented (0.25 [95% CI 0.16; 0.40]; 4 study populations) edentulous maxillae (P < 0.0001). Corresponding 5‐year implant survival estimations were 95.45% [95% CI 94.47; 96.26] for non‐augmented and 98.75% [95% CI 98.00; 99.22] for augmented maxillae. Both groups were pooled for further analyses.
Risk of bias within and across studies
Table 2 shows the risk of bias for each study as identified by the respective SIGN checklist. According to the terms of SIGN, most of the included clinical cohort studies or RCTs were of an acceptable or high quality, meaning “some flaws in the study with an associated risk of bias” or little to no risk of bias. Selective reporting or publication bias cannot be completely ruled out, especially, as some of the studies were sponsored by dental companies or a foundation being associated with a dental company.
Discussion
Summary of evidence
The objective of this systematic review and meta‐analysis was to attend to the focused question: Is there an impact of implant location (maxilla vs. mandible), implant number, type of prosthesis (fixed vs. removable) and/or different anchorage systems on the implant loss rate concerning the implant‐prosthodontic rehabilitation of edentulous patients?
Furthermore, additional analyses were performed to reveal a potential influence of implant surface and loading protocols on the implant loss rate for edentulous jaws.
In summary, the data situation or rather availability of literature concerning the edentulous jaw is comparatively satisfactory. Altogether 54 studies could be included for statistical analysis, although admittedly the majority of clinical studies investigated the edentulous mandible. This fact has also been observed by other authors of systematic reviews over the last 7 years (Sadowsky 2007; Slot et al. 2009; Roccuzzo et al. 2012).
To attain a reasonable level of evidence, retrospective studies were excluded. The overall evidence for the included randomized‐controlled and prospective studies can be rated acceptable. The majority of included studies had an evidence level of 2+, although it must be noted that the little number of included RCTs did not always directly address the focused question, meaning that a high level of evidence can be assumed for certain investigations, exclusively (e.g., different implant types were randomized). (Table 2).
In contrast to a previously published review regarding optimal implant numbers for the completely edentulous maxilla (Schley & Wolfart 2011), the authors decided to perform a statistical analysis. Analyzing non‐randomized, non‐controlled studies raises a complex of problems and does not allow for a classical analysis in form of a forest plot that always intents to compare different intervention groups, that is, randomized‐controlled trials. Furthermore, the inconsistent reporting of results among the studies complicates a meaningful analysis. The absence of exact information on implant/prosthesis loss or dropout and/or the absence of a mean observation period led to the exclusion of several articles. Hence, the authors adopted a frequently applied statistical method, suggested by Pjetursson et al. (2007) and Sailer et al. (2007) using the “total exposure time” of the investigated objects and estimating failure (or loss) and survival rates by Poisson regression. Recently, Pjetursson et al. (2014) applied the same method to describe the implant failure and the survival in a systematic review. Also, the present calculation of the “implant loss rate per 100 implant years” is based on the assumption of a constant event rate over time. The resulting “data distortion” is mainly caused by those studies with a very long or short observation period leading to an extrapolation or adaption of the available data, respectively. From a clinical point of view, this assumption is debatable; however, in the authors' opinion, currently, it is the best method to compare the results of the different clinical studies with each other. To provide full information, the actual implant losses and observation periods are given in Tables 3, 4, 5.
Considering the focused question, it can be stated that all of the mentioned factors (jaw, implant number, type of prosthesis and anchorage system) seem to have an impact on implant survival and implant loss. Generally, estimated implant survival was satisfactory for both, fixed and removable rehabilitation concepts.
The risk for implant loss per 100 implant years in the edentulous mandible is significantly lower than in the maxilla (0.22 [95% CI 0.17; 0.27] vs. 0.41 [95% CI 0.32; 0.52]; P = 0.0001). Regarding the direct comparisons of implant numbers in the mandible, higher numbers showed a clear tendency of resulting in lower implant loss rates. The therapeutic concept of one implant inserted into the midline symphysis in the edentulous lower jaw is an ongoing and intensively discussed topic. The present data of this concept are based on merely three studies and revealed a 5‐year survival estimation of 92.1%, which is satisfactory. Nevertheless, implant loss rates for two and four implants with an overdenture were significantly lower, and data were predicated on 19 and 10 patient groups, respectively. The “gold‐standard concept” of two implants with an overdenture seems to be consolidated by the analyses of this systematic review, regarding post‐loading implant survival, exclusively.
Only 21 studies could be included regarding the edentulous upper jaw, rendering extensive statistical comparisons difficult. However, the present analyses clearly indicate that at least four implants are needed in the edentulous maxilla, irrespective of the type of restoration. Less than four implants have been suggested not to be feasible for the edentulous maxilla in an experts' consensus conference and is not recommendable at the time being (Schley et al. 2013). This fact was proven by the present analysis that revealed unacceptable survival estimations after 5 years (69.7% [95% CI 61.75; 76.30]) and significantly higher implant loss rates per 100 implant years when compared to implant numbers of four and more (7.22 [95% CI 5.41; 9.64] vs. 2.31 [95% CI 1.56; 3.42]; P < 0.0001). Therefore, it was decided to merely include this group for an overall survival analysis, but to exclude it from further statistical evaluations and comparisons. No statistically significant differences for post‐loading implant loss could be assessed when comparing bar or ball anchorage. Estimated implant survival was very high for both attachment types (ball: 98.31% [95% CI 96.46; 99.20]; bar: 98.27 [95% CI 97.73; 98.66]). Telescopic crowns could not be evaluated, as the included number of studies was to low, and no implant losses had occurred after observation periods of 3 years. Furthermore, no statements can be made regarding cemented or adhesively luted fixed restorations as the systematic literature review did not reveal such studies. Considering the so‐called all‐on‐4 concept, meaning four implants being restored with a fixed prosthesis, the existing literature provides sufficient evidence for the edentulous mandible. Crespi et al. (2012) also implemented this concept for the edentulous maxilla and reported an implant survival of 98.96% after 3 years. For obvious reasons, this one study could not be used for statistical comparisons. However, retrospective clinical studies demonstrate comparable results (Malo et al. 2011, 2012).
Additional subgroup analyses were conducted regarding the aspects implants surface (machined vs. rough) and different loading protocols. Different surface roughness values could not be distinguished, and any type of surface modification was summarized under “rough” implant surface.
Comparing immediate vs. conventional loading in general, the estimated implant loss rate was slightly, but still significantly higher for an immediate protocol (P = 0.0151). Regarding fixed restorations, exclusively, implant loss rates did not significantly differ concerning immediate vs. conventional loading (P = 0.1652). This is in accordance with Papaspyridakos et al. (2014) who recently reported estimated survival rates between 99.10% and 99.90% for immediate and conventional loading for fixed prostheses in the edentulous maxilla and mandible in a systematic review. Surprisingly, the present results for fixed reconstructions in the edentulous mandible indicate a better outcome for a conventional loading protocol (P < 0.0001) and a better outcome for an immediate loading protocol for maxilla in general (P = 0.0108). If removable overdentures are planned, a conventional loading protocol still seems to result in a superior outcome concerning post‐loading implant losses per 100 implant years (0.32 [95% CI 0.25; 0.42] vs. 0.62 [95%CI 0.37; 1.05]; P = 0.0282). Also Schimmel et al. (2014) concluded in their systematic review that implant‐supported overdentures tend to have lower 1‐year implant failure rates after application of a conventional loading protocol when compared to an immediate loading protocol. Moreover, they stated a necessity for “well‐designed research protocols”, because they partly experienced contradicting findings in their review.
The superior results for rough implant surfaces in almost all of the subcategories were not surprising. Better osseointegration capabilities of rough‐surfaced implants have been shown in the past (Cordioli et al. 2000; Wennerberg & Albrektsson 2010).
Regarding post‐loading implant loss, the classical implant‐prosthodontic rehabilitation concepts, that is bar‐ or ball‐retained overdentures and screw‐retained full‐arch reconstructions, have shown an excellent outcome according to the present analyses. A certain number of implants seem to ensure a reliable outcome for implants with a fixed or a removable restoration. However, prosthesis‐related technical complications need to be taken into consideration, as well. Therefore, we plan to analyze technical complications and correlated complication‐free rates for implant‐supported prostheses, related to implant location and certain implant numbers, in another systematic review.
Limitations
The presented results have to be interpreted with the following limitations:
The estimated implant loss rates and survival estimations were mostly derived from non‐comparative studies. Due to a lack of high‐quality studies (i.e., RCTs), the currently best option of receiving meaningful results is to analyze the best available evidence (mostly single arm cohort studies). Our focus was on potentially influencing aspects such as implant number, loading protocol and different prosthodontic treatment options. Due to the high degree of separation, a statistical analysis considering all of the potential influencing factors simultaneously was not feasible. However, a multivariate Poisson regression model concerning the location of implants, the type of prosthesis, the surface of implants, and the loading protocol as main effects, was fitted to the data of univariate meaningful factors.
Due to the observational nature of the included studies, confounding of observable, as well as unobservable factors is an intrinsic limitation of our derived results. Of course, a future aim is to analyze which combination of the above‐mentioned factors is decisive, and therefore, more well‐designed RCTs are needed. However, in dentistry and especially in the field of implant dentistry, several aspects such as high treatment costs, long duration of treatment, and limiting inclusion criteria (edentulous patients not being satisfied with complete overdentures) render RCTs difficult at best. It has to be recognized that CONSORT and consequently PRISMA statements or the “Cochrane Handbook” are mainly intended for medical studies and do perfectly fit for study concepts such as placebo vs. active agent. If our analysis strictly adhered to these protocols, merely a few studies would have been included thus setting a limitation, as well. In the authors' opinion, the inclusion of 54 studies with 9267 implants should inherently partly compensate the methodological handicap and thus could represent the best available “compromise”.
The primary outcome was post‐loading implant loss and not implant failure or success, which clearly would be the more accurate approach. However, the inhomogeneous reporting of success and failure among the studies (if reported at all) did not permit a statistical evaluation of success or failure rates.
As a matter of fact, several important aspects could not be considered in the present analyses, setting a limitation to this review. For example, different implant parameters such as length, diameter, form (cylindric, root‐like), implant‐abutment connection, bone‐to‐implant interface, or the difference of one‐ or two‐piece implants could not be assessed. Furthermore, studies investigating implants in either local or augmented bone (four studies) were pooled. However, the analysis of augmented bone in the maxilla did not reveal negative results concerning estimated implant loss and corresponding survival rates. The duration of edentulism as a potential confounder could not be regarded either, but, in most studies, the “typical” completely edentate patient was subject of the investigation.
The analysis of biologic complications was not part of our focused question and explains why these complications were not evaluated in detail.
It is self‐evident that the “best” choice of an implant‐prosthdontic restoration, cannot simply be based on the analyzed and aforementioned aspects. Individual, patient‐based circumstances determine any surgical or prosthodontic procedures. In this context, it was not possible to regard important facts such as patients' preferences, esthetic complexity, maxillomandibular relationship, bone quality and quantity, soft tissue conditions, condition or type of restoration of the opposing jaw, or differences of treatment/manufacturing costs. Even though several authors gave information on the type of restoration in the opposite jaw (full denture, fixed or removable prosthesis), a conclusion, if implant outcome is affected by this factor, could not be evaluated.
Moreover, oral health‐related quality of life (OHRQoL) is an omnipresent topic, and especially, the rehabilitation of the edentulous jaw by means of implant‐prosthodontic procedures can offer a great potential of improving patients' quality of life (Turkyilmaz et al. 2010). For the edentulous maxilla, in particular, there is a huge backlog demand for studies on OHRQoL. In this respect, Zembic & Wismeijer (2014) recently published an interesting approach. Patients received conventional complete dentures in a first step, and 2 months later, two implants were inserted – the implant‐retained overdentures “provided some significant short‐term improvements over conventional dentures in oral‐ and health‐related quality of life”.
Many of the aforementioned parameters demand for a consolidated internal evidence, meaning the dentist's experience, which serves as an important component of evidence‐based medicine/dentistry. In combination with the external evidence (current state of science) and the patient's values and wishes, a participatory decision‐making process can be developed (Türp & Antes 2013). This procedure provides a reasonable degree of safety for both patient and dentist.
Conclusions
Considering the above‐mentioned limitations, the following conclusions can be drawn:
Only four of the included studies report on observation periods of more than 10 years.
The current evaluations show a successful outcome for screw‐retained fixed restorations and bar‐ or ball‐retained overdentures in the completely edentulous jaw. Disregarding more than the included potential confounders (such as anatomic situation, bone quality, jaw relation, implant‐related components) and relating to the estimated post‐loading implant loss, exclusively, the following statements can be made:
- Maxilla:
- The insertion of six or more implants for a fixed reconstruction in the maxilla reveals favorable results. Considering the “all‐on‐4” concept for the maxilla, one study (Crespi et al. 2012) with an acceptable level of evidence was found, revealing a satisfactory outcome. For obvious reasons, this one study could not be used for a meaningful statistical comparison.
- The insertion of four implants for a removable overdenture in the maxilla reveals satisfying results. Data on minimal concepts with <4 implants in the maxilla is scarce and demonstrated significantly worse results, calling for a cautious and controlled application of these therapeutic options.
- Mandible:
- The insertion of four implants for a fixed restoration in the edentulous mandible reveals satisfying results. However, it has to be noticed that five or more implants showed a slightly better outcome.
- The insertion of two implants for a removable overdenture in the mandible shows favorable results. However, it has to be noticed that four implants revealed a slightly better outcome. Furthermore, four implants with a removable prosthesis had a better outcome than four implants with a fixed prosthesis in the mandible. Data on the minimal concept with only 1 implant is scarce and shows promising results. However, the results are negatively influenced when using machined‐surfaced implants and an immediate loading protocol (Liddelow & Henry 2010). The application of this therapeutic option can only be recommended, when the insertion of 2 or more implants is not feasible, e.g. due to economic reasons.
- In general:
- Implants with fixed prostheses show slightly but significantly better results than removable prostheses regarding both jaws.
- Rough‐surfaced implants demonstrated favorable results compared to machined implants.
- In general, conventional loading tended to result in fewer implant losses. However, the implant loss rate for fixed prostheses in maxilla and mandible did not significantly differ concerning immediate and conventional loading. It has to be noted, though, that immediate loading was generally attached to strict conditions (e.g., a pre‐defined insertion torque).
Future research
Consequential suggestions for future research: Future RCTs should investigate different attachment systems with different implant numbers, especially for 1 vs. 2 implants in the mandible and <4 implants in the maxilla. Furthermore, the comparison of 4 implants vs. >4 implants with a fixed prosthesis in the maxilla and mandible would be desirable.
General suggestions for future research: Clinical studies should not only concentrate on implant success rates but also on the patients' benefit with regard to quality of life, improvement of mastication abilities, hygiene capability, psychological aspects, and financial considerations.
Conflict of interest
The authors declare that they have no conflict of interest related to this article.
Source of funding
As this systematic review served as a basis for an experts' consensus conference (7th International Expert Meeting of the CAMLOG Foundation), it was partially supported by the CAMLOG Foundation.
Supporting information
Appendix S1. PRISMA 2009 Checklist.
Acknowledgements
The authors would like to thank Prof. Dr. Jürgen Becker, Prof. Dr. Irena Sailer, Prof. Dr. Frank Schwarz, and Prof. Dr. Dr. Wilfried Wagner for their support.
Kern J‐S, Kern T, Wolfart S, Heussen N. A systematic review and meta‐analysis of removable and fixed implant‐supported prostheses in edentulous jaws: post‐loading implant loss. Clin. Oral Impl. Res. 27, 2016, 174–195 doi: 10.1111/clr.12531
[Corrections added after initial online publication on 9 February, 2015: the word five studies has been changed as 54 studies in the Results section in Abstract.]
References
- Askig Focused Questions (2014) CEBM Center for Evidence Based Medicine www.cebm.net. Oxford: University of Oxford. [Google Scholar]
- Agliardi, E.L. , Pozzi, A. , Stappert, C.F. , Benzi, R. , Romeo, D. & Gherlone, E. (2012) Immediate fixed rehabilitation of the edentulous maxilla: a prospective clinical and radiological study after 3 years of loading. Clinical Implant Dentistry and Related Research 16: 292–302. [DOI] [PubMed] [Google Scholar]
- Akca, K. , Cehreli, M.C. & Uysal, S. (2010) Marginal bone loss and prosthetic maintenance of bar‐retained implant‐supported overdentures: a prospective study. The International Journal of Oral and Maxillofacial Implants 25: 137–145. [PubMed] [Google Scholar]
- Akoglu, B. , Ucankale, M. , Ozkan, Y. & Kulak‐Ozkan, Y. (2011) Five‐year treatment outcomes with three brands of implants supporting mandibular overdentures. The International Journal of Oral and Maxillofacial Implants 26: 188–194. [PubMed] [Google Scholar]
- Albaker, A.M. (2013) The oral health‐related quality of life in edentulous patients treated with conventional complete dentures. Gerodontology 30: 61–66. [DOI] [PubMed] [Google Scholar]
- Allen, P.F. & McMillan, A.S. (2003) A longitudinal study of quality of life outcomes in older adults requesting implant prostheses and complete removable dentures. Clinical Oral Implants Research 14: 173–179. [DOI] [PubMed] [Google Scholar]
- Arvidson, K. , Bystedt, H. , Frykholm, A. , von Konow, L. & Lothigius, E. (1998) Five‐year prospective follow‐up report of the Astra Tech Dental Implant System in the treatment of edentulous mandibles. Clinical Oral Implants Research 9: 225–234. [DOI] [PubMed] [Google Scholar]
- Arvidson, K. , Esselin, O. , Felle‐Persson, E. , Jonsson, G. , Smedberg, J.I. & Soderstrom, U. (2008) Early loading of mandibular full‐arch bridges screw retained after 1 week to four to five monotype implants: 3‐year results from a prospective multicentre study. Clinical Oral Implants Research 19: 693–703. [DOI] [PubMed] [Google Scholar]
- Behneke, A. , Behneke, N. & d'Hoedt, B. (2002) A 5‐year longitudinal study of the clinical effectiveness of ITI solid‐screw implants in the treatment of mandibular edentulism. The International Journal of Oral and Maxillofacial Implants 17: 799–810. [PubMed] [Google Scholar]
- Bergendal, T. & Engquist, B. (1998) Implant‐supported overdentures: a longitudinal prospective study. The International Journal of Oral and Maxillofacial Implants 13: 253–262. [PubMed] [Google Scholar]
- Cehreli, M.C. , Uysal, S. & Akca, K. (2010) Marginal bone level changes and prosthetic maintenance of mandibular overdentures supported by 2 implants: a 5‐year randomized clinical trial. Clinical Implant Dentistry and Related Research 12: 114–121. [DOI] [PubMed] [Google Scholar]
- Chiapasco, M. & Gatti, C. (2003) Implant‐retained mandibular overdentures with immediate loading: a 3‐ to 8‐year prospective study on 328 implants. Clinical Implant Dentistry and Related Research 5: 29–38. [DOI] [PubMed] [Google Scholar]
- Collaert, B. & De Bruyn, H. (2008) Immediate functional loading of TiOblast dental implants in full‐arch edentulous maxillae: a 3‐year prospective study. Clinical Oral Implants Research 19: 1254–1260. [DOI] [PubMed] [Google Scholar]
- Cooper, L.F. , Moriarty, J.D. , Guckes, A.D. , Klee, L.B. , Smith, R.G. , Almgren, C. & Felton, D.A. (2008) Five‐year prospective evaluation of mandibular overdentures retained by two microthreaded, TiOblast nonsplinted implants and retentive ball anchors. The International Journal of Oral and Maxillofacial Implants 23: 696–704. [PubMed] [Google Scholar]
- Cordioli, G. , Majzoub, Z. & Castagna, S. (1997) Mandibular overdentures anchored to single implants: a five‐year prospective study. The Journal of Prosthetic Dentistry 78: 159–165. [DOI] [PubMed] [Google Scholar]
- Cordioli, G. , Majzoub, Z. , Piattelli, A. & Scarano, A. (2000) Removal torque and histomorphometric investigation of 4 different titanium surfaces: an experimental study in the rabbit tibia. The International Journal of Oral and Maxillofacial Implants 15: 668–674. [PubMed] [Google Scholar]
- Covani, U. , Orlando, B. , D'Ambrosio, A. , Sabattini, V.B. & Barone, A. (2012) Immediate rehabilitation of completely edentulous jaws with fixed prostheses supported by implants placed into fresh extraction sockets and in healed sites: a 4‐year clinical evaluation. Implant Dentistry 21: 272–279. [DOI] [PubMed] [Google Scholar]
- Crespi, R. , Vinci, R. , Cappare, P. , Romanos, G.E. & Gherlone, E. (2012) A clinical study of edentulous patients rehabilitated according to the “all on four” immediate function protocol. The International Journal of Oral and Maxillofacial Implants 27: 428–434. [PubMed] [Google Scholar]
- De Bruyn, H. , Van de Velde, T. & Collaert, B. (2008) Immediate functional loading of TiOblast dental implants in full‐arch edentulous mandibles: a 3‐year prospective study. Clinical Oral Implants Research 19: 717–723. [DOI] [PubMed] [Google Scholar]
- De Santis, D. , Trevisiol, L. , D'Agostino, A. , Cucchi, A. , De Gemmis, A. & Nocini, P.F. (2012) Guided bone regeneration with autogenous block grafts applied to Le Fort I osteotomy for treatment of severely resorbed maxillae: a 4‐ to 6‐year prospective study. Clinical Oral Implants Research 23: 60–69. [DOI] [PubMed] [Google Scholar]
- Degidi, M. , Nardi, D. & Piattelli, A. (2010) Immediate loading of the edentulous maxilla with a definitive restoration supported by an intraorally welded titanium bar and tilted implants. The International Journal of Oral and Maxillofacial Implants 25: 1175–1182. [PubMed] [Google Scholar]
- Ekelund, J.A. , Lindquist, L.W. , Carlsson, G.E. & Jemt, T. (2003) Implant treatment in the edentulous mandible: a prospective study on Branemark system implants over more than 20 years. The International Journal of Prosthodontics 16: 602–608. [PubMed] [Google Scholar]
- Eliasson, A. , Narby, B. , Ekstrand, K. , Hirsch, J. , Johansson, A. & Wennerberg, A. (2010) A 5‐year prospective clinical study of submerged and nonsubmerged Paragon system implants in the edentulous mandible. The International Journal of Prosthodontics, 23: 231–238. [PubMed] [Google Scholar]
- Elsyad, M.A. , Al‐Mahdy, Y.F. & Fouad, M.M. (2012) Marginal bone loss adjacent to conventional and immediate loaded two implants supporting a ball‐retained mandibular overdenture: a 3‐year randomized clinical trial. Clinical Oral Implants Research 23: 496–503. [DOI] [PubMed] [Google Scholar]
- Engquist, B. , Astrand, P. , Anzén, B. , Dahlgren, S. , Engquist, E. , Feldmann, H. , Karlsson, U. , Nord, P.G. , Sahlholm, S. & Svärdström, P. (2005) Simplified methods of implant treatment in the edentulous lower jaw: a 3‐year follow‐up report of a controlled prospective study of one‐stage versus two‐stage surgery and early loading. Clinical Implant Dentistry and Related Research, 7: 95–104. [DOI] [PubMed] [Google Scholar]
- Esposito, M. , Grusovin, M.G. , Willings, M. , Coulthard, P. & Worthington, H.V. (2007) The effectiveness of immediate, early, and conventional loading of dental implants: a Cochrane systematic review of randomized controlled clinical trials. The International Journal of Oral & Maxillofacial Implants 22: 893–904. [PubMed] [Google Scholar]
- Feine, J.S. , Carlsson, G.E. , Awad, M.A. , Chehade, A. , Duncan, W.J. , Gizani, S. , Head, T. , Heydecke, G. , Lund, J.P. , MacEntee, M. , Mericske‐Stern, R. , Mojon, P. , Morais, J.A. , Naert, I. , Payne, A.G. , Penrod, J. , Stoker, G.T. , Tawse‐Smith, A. , Taylor, T.D. , Thomason, J.M. , Thomson, W.M. & Wismeijer, D. (2002a) The McGill consensus statement on overdentures. Mandibular two‐implant overdentures as first choice standard of care for edentulous patients. Gerodontology 19: 3–4. [PubMed] [Google Scholar]
- Feine, J.S. , Carlsson, G.E. , Awad, M.A. , Chehade, A. , Duncan, W.J. , Gizani, S. , Head, T. , Lund, J.P. , MacEntee, M. , Mericske‐Stern, R. , Mojon, P. , Morais, J. , Naert, I. , Payne, A.G. , Penrod, J. , Stoker, G.T., Jr , Tawse‐Smith, A. , Taylor, T.D. , Thomason, J.M. , Thomson, W.M. & Wismeijer, D. (2002b) The McGill consensus statement on overdentures. Montreal, Quebec, Canada. May 24–25, 2002. The International Journal of Prosthodontics 15: 413–414. [PubMed] [Google Scholar]
- Feine, J.S. , Carlsson, G.E. , Awad, M.A. , Chehade, A. , Duncan, W.J. , Gizani, S. , Head, T. , Lund, J.P. , MacEntee, M. , Mericske‐Stern, R. , Mojon, P. , Morais, J. , Naert, I. , Payne, A.G. , Penrod, J. , Stoker, G.T. , Tawse‐Smith, A. , Taylor, T.D. , Thomason, J.M. , Thomson, W.M. & Wismeijer, D. (2002c) The McGill consensus statement on overdentures. Mandibular two‐implant overdentures as first choice standard of care for edentulous patients. Montreal, Quebec, May 24–25, 2002. The International Journal of Oral and Maxillofacial Implants 17: 601–602. [PubMed] [Google Scholar]
- Fischer, K. & Stenberg, T. (2012) Prospective 10‐year cohort study based on a randomized controlled trial (RCT) on implant‐supported full‐arch maxillary prostheses. Part 1: sandblasted and acid‐etched implants and mucosal tissue. Clinical Implant Dentistry and Related Research 14: 808–815. [DOI] [PubMed] [Google Scholar]
- Fischer, K. & Stenberg, T. (2013) Prospective 10‐year cohort study based on a randomized, controlled trial (RCT) on implant‐supported full‐arch maxillary prostheses. part II: prosthetic outcomes and maintenance. Clinical Implant Dentistry and Related Research 15: 498–508. [DOI] [PubMed] [Google Scholar]
- Gotfredsen, K. & Holm, B. (2000) Implant‐supported mandibular overdentures retained with ball or bar attachments: a randomized prospective 5‐year study. The International Journal of Prosthodontics 13: 125–130. [PubMed] [Google Scholar]
- Harder, S. , Wolfart, S. , Egert, C. & Kern, M. (2011) Three‐year clinical outcome of single implant‐retained mandibular overdentures – results of preliminary prospective study. Journal of Dentistry 39: 656–661. [DOI] [PubMed] [Google Scholar]
- Heijdenrijk, K. , Raghoebar, G.M. , Meijer, H.J. , Stegenga, B. & van der Reijden, W.A. (2006) Feasibility and influence of the microgap of two implants placed in a non‐submerged procedure: a five‐year follow‐up clinical trial. Journal of Periodontology 77: 1051–1060. [DOI] [PubMed] [Google Scholar]
- Heschl, A. , Payer, M. , Clar, V. , Stopper, M. , Wegscheider, W. & Lorenzoni, M. (2013) Overdentures in the edentulous mandible supported by implants and retained by a Dolder bar: a 5‐year prospective study. Clinical Implant Dentistry and Related Research 15: 589–599. [DOI] [PubMed] [Google Scholar]
- Heschl, A. , Payer, M. , Platzer, S. , Wegscheider, W. , Pertl, C. & Lorenzoni, M. (2012) Immediate rehabilitation of the edentulous mandible with screw type implants: results after up to 10 years of clinical function. Clinical Oral Implants Research 23: 1217–1223. [DOI] [PubMed] [Google Scholar]
- Heydecke, G. , Zwahlen, M. , Nicol, A. , Nisand, D. , Payer, M. , Renouard, F. , Grohmann, P. , Mühlemann, S. & Joda, T. (2012) What is the optimal number of implants for fixed reconstructions: a systematic review. Clinical Oral Implants Research 23(Suppl. 6): 217–228. [DOI] [PubMed] [Google Scholar]
- Jemt, T. , Chai, J. , Harnett, J. , Heath, M.R. , Hutton, J.E. , Johns, R.B. , McKenna, S. , McNamara, D.C. , van Steenberghe, D. , Taylor, R. , Watson, R.M. & Herrmann, I. (1996) A 5‐year prospective multicenter follow‐up report on overdentures supported by osseointegrated implants. The International Journal of Oral and Maxillofacial Implants 11: 291–298. [PubMed] [Google Scholar]
- Krennmair, G. , Krainhofner, M. & Piehslinger, E. (2008) The influence of bar design (round versus milled bar) on prosthodontic maintenance of mandibular overdentures supported by 4 implants: a 5‐year prospective study. The International Journal of Prosthodontics 21: 514–520. [PubMed] [Google Scholar]
- Krennmair, G. , Seemann, R. , Weinlander, M. & Piehslinger, E. (2011) Comparison of ball and telescopic crown attachments in implant‐retained mandibular overdentures: a 5‐year prospective study. The International Journal of Oral and Maxillofacial Implants 26: 598–606. [PubMed] [Google Scholar]
- Krennmair, G. , Suto, D. , Seemann, R. & Piehslinger, E. (2012) Removable four implant‐supported mandibular overdentures rigidly retained with telescopic crowns or milled bars: a 3‐year prospective study. Clinical Oral Implants Research 23: 481–488. [DOI] [PubMed] [Google Scholar]
- Lambert, F.E. , Weber, H.P. , Susarla, S.M. , Belser, U.C. & Gallucci, G.O. (2009) Descriptive analysis of implant and prosthodontic survival rates with fixed implant‐supported rehabilitations in the edentulous maxilla. Journal of Periodontology 80: 1220–1230. [DOI] [PubMed] [Google Scholar]
- Lethaus, B. , Kälber, J. , Patrin, G. , Brandstätter, A. & Weingart, D. (2011) Early loading of sandblasted and acid‐etched titanium implants in the edentulous mandible: a prospective 5‐year study. The International Journal of Oral and Maxillofacial Implants 26: 887–892. [PubMed] [Google Scholar]
- Liddelow, G. & Henry, P. (2010) The immediately loaded single implant‐retained mandibular overdenture: a 36‐month prospective study. The International Journal of Prosthodontics 23: 13–21. [PubMed] [Google Scholar]
- Lindquist, L.W. , Carlsson, G.E. & Jemt, T. (1996) A prospective 15‐year follow‐up study of mandibular fixed prostheses supported by osseointegrated implants. Clinical results and marginal bone loss. Clinical Oral Implants Research 7: 329–336. [DOI] [PubMed] [Google Scholar]
- Lorenzoni, M. , Stopper, M. , Vogl, S. & Wegscheider, W.A. (2013) Sofort und konventionell versorgte Implantate im zahnlosen Unterkiefer. Zeitschrift für Zahnärztliche Implantologie 29: 130–138. [Google Scholar]
- Malo, P. , de Araujo Nobre, M. , Lopes, A. , Francischone, C. & Rigolizzo, M. (2012) “All‐on‐4” immediate‐function concept for completely edentulous maxillae: a clinical report on the medium (3 years) and long‐term (5 years) outcomes. Clinical Implant Dentistry and Related Research 14(Suppl. 1): e139–e150. [DOI] [PubMed] [Google Scholar]
- Malo, P. , Nobre, M. & Lopes, A. (2011) The rehabilitation of completely edentulous maxillae with different degrees of resorption with four or more immediately loaded implants: a 5‐year retrospective study and a new classification. European Journal of Oral Implantology 4: 227–243. [PubMed] [Google Scholar]
- Meijer, H.J. , Raghoebar, G.M. , Batenburg, R.H. , Visser, A. & Vissink, A. (2009a) Mandibular overdentures supported by two or four endosseous implants: a 10‐year clinical trial. Clinical Oral Implants Research 20: 722–728. [DOI] [PubMed] [Google Scholar]
- Meijer, H.J. , Raghoebar, G.M. , Batenburg, R.H. & Vissink, A. (2009b) Mandibular overdentures supported by two Branemark, IMZ or ITI implants: a ten‐year prospective randomized study. Journal of Clinical Periodontology 36: 799–806. [DOI] [PubMed] [Google Scholar]
- Meijer, H.J. , Raghoebar, G.M. , Van't Hof, M.A. & Visser, A. (2004) A controlled clinical trial of implant‐retained mandibular overdentures: 10 years' results of clinical aspects and aftercare of IMZ implants and Branemark implants. Clinical Oral Implants Research 15: 421–427. [DOI] [PubMed] [Google Scholar]
- Mertens, C. , Steveling, H.G. , Stucke, K. , Pretzl, B. & Meyer‐Bäumer, A. (2012) Fixed implant‐retained rehabilitation of the edentulous maxilla: 11‐year results of a prospective study. Clinical Implant Dentistry and Related Research 14: 464–472. [DOI] [PubMed] [Google Scholar]
- Micheelis, W. & Schiffner, U. (2006) Vierte Deutsche Mundgesundheitsstudie (DMS IV). Ergebnisse zu oralen Erkrankungsprävalenzen, Risikogruppen und zum zahnärztlichen Versorgungsgrad in Deutschland 2005. In: (IDZ) IdDZ, ed. Vol. Materialienreihe Band 31 Deutscher Zahnärzte Verlag DÄV, Köln: 1‐502.
- Moher, D. , Liberati, A. , Tetzlaff, J. , Altman, D.G. & Group, P. (2009) Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Medicine 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy, W.M. , Absi, E.G. , Gregory, M.C. & Williams, K.R. (2002) A prospective 5‐year study of two cast framework alloys for fixed implant‐supported mandibular prostheses. The International Journal of Prosthodontics 15: 133–138. [PubMed] [Google Scholar]
- Naert, I. , Gizani, S. & van Steenberghe, D. (1998) Rigidly splinted implants in the resorbed maxilla to retain a hinging overdenture: a series of clinical reports for up to 4 years. Journal of Prosthetic Dentistry 79: 156–164. [DOI] [PubMed] [Google Scholar]
- Nyström, E. , Nilson, H. , Gunne, J. & Lundgren, S. (2009a) A 9–14 year follow‐up of onlay bone grafting in the atrophic maxilla. The International Journal of Oral and Maxillofacial Surgery 38: 111–116. [DOI] [PubMed] [Google Scholar]
- Nyström, E. , Nilson, H. , Gunne, J. & Lundgren, S. (2009b) Reconstruction of the atrophic maxilla with interpositional bone grafting/Le Fort I osteotomy and endosteal implants: a 11–16 year follow‐up. The International Journal of Oral and Maxillofacial Surgery 38: 1–6. [DOI] [PubMed] [Google Scholar]
- Örtörp, A. & Jemt, T. (2012) CNC‐milled titanium frameworks supported by implants in the edentulous jaw: a 10‐year comparative clinical study. Clinical Implant Dentistry and Related Research 14: 88–99. [DOI] [PubMed] [Google Scholar]
- Papaspyridakos, P. , Chen, C.J. , Chuang, S.K. & Weber, H.P. (2014) Implant loading protocols for edentulous patients with fixed prostheses: a systematic review and meta‐analysis. The International Journal of Oral and Maxillofacial Implants 29(Suppl.): 256–270. [DOI] [PubMed] [Google Scholar]
- Papaspyridakos, P. , Chen, C.J. , Chuang, S.K. , Weber, H.P. & Gallucci, G.O. (2012) A systematic review of biologic and technical complications with fixed implant rehabilitations for edentulous patients. The International Journal of Oral and Maxillofacial Implants 27: 102–110. [PubMed] [Google Scholar]
- Papaspyridakos, P. , Mokti, M. , Chen, C.J. , Benic, G.I. , Gallucci, G.O. & Chronopoulos, V. (2013) Implant and prosthodontic survival rates with implant fixed complete dental prostheses in the edentulous mandible after at least 5 years: a systematic review. Clinical Implant Dentistry and Related Research 16: 705–717. [DOI] [PubMed] [Google Scholar]
- Payne, A.G. & Solomons, Y.F. (2000) The prosthodontic maintenance requirements of mandibular mucosa‐ and implant‐supported overdentures: a review of the literature. The International Journal of Prosthodontics 13: 238–243. [PubMed] [Google Scholar]
- Pjetursson, B.E. , Asgeirsson, A.G. , Zwahlen, M. & Sailer, I. (2014) Improvements in implant dentistry over the last decade: comparison of survival and complication rates in older and newer publications. The International Journal of Oral and Maxillofacial Implants 29(Suppl.): 308–324. [DOI] [PubMed] [Google Scholar]
- Pjetursson, B.E. , Bragger, U. , Lang, N.P. & Zwahlen, M. (2007) Comparison of survival and complication rates of tooth‐supported fixed dental prostheses (FDPs) and implant‐supported FDPs and single crowns (SCs). Clinical Oral Implants Research 18(Suppl. 3): 97–113. [DOI] [PubMed] [Google Scholar]
- Rasmusson, L. , Roos, J. & Bystedt, H. (2005) A 10‐year follow‐up study of titanium dioxide‐blasted implants. Clinical Implant Dentistry and Related Research 7: 36–42. [DOI] [PubMed] [Google Scholar]
- Richter, E.J. & Knapp, W. (2010) Auf zwei Eckzahnimplantaten abgestützte Oberkiefer‐Coverdentureprothesen ‐ Ergebnisse einer klinischen Studie. Implantologie 18: 165–174. [Google Scholar]
- Roccuzzo, M. , Bonino, F. , Gaudioso, L. , Zwahlen, M. & Meijer, H.J. (2012) What is the optimal number of implants for removable reconstructions? A systematic review on implant‐supported overdentures. Clinical Oral Implants Research 23(Suppl. 6): 229–237. [DOI] [PubMed] [Google Scholar]
- Romeo, E. , Lops, D. , Margutti, E. , Ghisolfi, M. , Chiapasco, M. & Vogel, G. (2004) Long‐term survival and success of oral implants in the treatment of full and partial arches: a 7‐year prospective study with the ITI dental implant system. The International Journal of Oral and Maxillofacial Implants 19: 247–259. [PubMed] [Google Scholar]
- Sadowsky, S.J. (2007) Treatment considerations for maxillary implant overdentures: a systematic review. Journal of Prosthetic Dentistry 97: 340–348. [DOI] [PubMed] [Google Scholar]
- Sailer, I. , Pjetursson, B.E. , Zwahlen, M. & Hammerle, C.H. (2007) A systematic review of the survival and complication rates of all‐ceramic and metal‐ceramic reconstructions after an observation period of at least 3 years. Part II: fixed dental prostheses. Clinical Oral Implants Research 18(Suppl. 3): 86–96. [DOI] [PubMed] [Google Scholar]
- Scala, R. , Cucchi, A. , Ghensi, P. & Vartolo, F. (2012) Clinical evaluation of satisfaction in patients rehabilitated with an immediately loaded implant‐supported prosthesis: a controlled prospective study. The International Journal of Oral and Maxillofacial Implants 27: 911–919. [PubMed] [Google Scholar]
- Schimmel, M. , Srinivasan, M. , Herrmann, F.R. & Muller, F. (2014) Loading protocols for implant‐supported overdentures in the edentulous jaw: a systematic review and meta‐analysis. The International Journal of Oral and Maxillofacial Implants 29(Suppl.): 271–286. [DOI] [PubMed] [Google Scholar]
- Schley, J.S. , Terheyden, H. , Wolfart, S. , Boehme, P. , Gómez‐Róman, G. , Keese, E. , Kern, M. , Pilgrim, C. , Reinhardt, S. , Weber, A. & Schütte, U. (2013) Implantatprothetische Versorgung des zahnlosen Oberkiefers ‐ S3 Leitlinie. Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V. (AWMF) AWMF‐Registernr. 083‐010.
- Schley, J.S. & Wolfart, S. (2011) Which prosthetic treatment concepts present a reliable evidence‐based option for the edentulous maxilla related to number and position of dental implants? European Journal of Oral Implantology 4: 31–47.21594217 [Google Scholar]
- Schwarz, S. , Gabbert, O. , Hassel, A.J. , Schmitter, M. , Seche, C. & Rammelsberg, P. (2010) Early loading of implants with fixed dental prostheses in edentulous mandibles: 4.5‐year clinical results from a prospective study. Clinical Oral Implants Research 21: 284–289. [DOI] [PubMed] [Google Scholar]
- Sjöström, M. , Sennerby, L. , Nilson, H. & Lundgren, S. (2007) Reconstruction of the atrophic edentulous maxilla with free iliac crest grafts and implants: a 3‐year report of a prospective clinical study. Clinical Implant Dentistry and Related Research 9: 46–59. [DOI] [PubMed] [Google Scholar]
- Slot, W. , Raghoebar, G.M. , Vissink, A. , Huddleston Slater, J.J. & Meijer, H.J. (2009) A systematic review of implant‐supported maxillary overdentures after a mean observation period of at least 1 year. Journal of Clinical Periodontology 37: 98–110. [DOI] [PubMed] [Google Scholar]
- Stoker, G. , van Waas, R. & Wismeijer, D. (2012) Long‐term outcomes of three types of implant‐supported mandibular overdentures in smokers. Clinical Oral Implants Research 23: 925–929. [DOI] [PubMed] [Google Scholar]
- Testori, T. , Fabbro, M. , Galli, F. , Francetti, L. , Taschieri, S. & Weinstein, R. (2004) Immediate occlusal loading the same day or the after implant placement: comparison of 2 different time frames in total edentulous lower jaws. The Journal of Oral Implantology 30: 307–313. [DOI] [PubMed] [Google Scholar]
- Turkyilmaz, I. , Company, A.M. & McGlumphy, E.A. (2010) Should edentulous patients be constrained to removable complete dentures? The use of dental implants to improve the quality of life for edentulous patients. Gerodontology 27: 3–10. [DOI] [PubMed] [Google Scholar]
- Türp, J.C. & Antes, G. (2013) Evidenzbasierte Zahnmedizin –aktueller Stand; evidence‐based dentistry – status quo. Deutsche Zahnärztliche Zeitschrift 68: 72–74. [Google Scholar]
- Van de Velde, T. , Collaert, B. & De Bruyn, H. (2007) Immediate loading in the completely edentulous mandible: technical procedure and clinical results up to 3 years of functional loading. Clinical Oral Implants Research 18: 295–303. [DOI] [PubMed] [Google Scholar]
- Vroom, M.G. , Sipos, P. , de Lange, G.L. , Grundemann, L.J. , Timmerman, M.F. , Loos, B.G. & van der Velden, U. (2009) Effect of surface topography of screw‐shaped titanium implants in humans on clinical and radiographic parameters: a 12‐year prospective study. Clinical Oral Implants Research 20: 1231–1239. [DOI] [PubMed] [Google Scholar]
- Watson, R.M. , Jemt, T. , Chai, J. , Harnett, J. , Heath, M.R. , Hutton, J.E. , Johns, R.B. , Lithner, B. , McKenna, S. , McNamara, D.C. , Naert, I. & Taylor, R. (1997) Prosthodontic treatment, patient response, and the need for maintenance of complete implant‐supported overdentures: an appraisal of 5 years of prospective study. The International Journal of Prosthodontics 10: 345–354. [PubMed] [Google Scholar]
- Weinländer, M. , Piehslinger, E. & Krennmair, G. (2010) Removable implant‐prosthodontic rehabilitation of the edentulous mandible: five‐year results of different prosthetic anchorage concepts. The International Journal of Oral & Maxillofacial Implants 25: 589–597. [PubMed] [Google Scholar]
- Wennerberg, A. & Albrektsson, T. (2010) On implant surfaces: a review of current knowledge and opinions. The International Journal of Oral and Maxillofacial Implants 25: 63–74. [PubMed] [Google Scholar]
- Zembic, A. & Wismeijer, D. (2014) Patient‐reported outcomes of maxillary implant‐supported overdentures compared with conventional dentures. Clinical Oral Implants Research 25: 441–450. [DOI] [PubMed] [Google Scholar]
- Zitzmann, N.U. & Marinello, C.P. (2000a) Treatment outcomes of fixed or removable implant‐supported prostheses in the edentulous maxilla. Part I: patients' assessments. Journal of Prosthetic Dentistry 83: 424–433. [DOI] [PubMed] [Google Scholar]
- Zitzmann, N.U. & Marinello, C.P. (2000b) Treatment outcomes of fixed or removable implant‐supported prostheses in the edentulous maxilla. Part II: clinical findings. Journal of Prosthetic Dentistry 83: 434–442. [DOI] [PubMed] [Google Scholar]
- Zou, D. , Wu, Y. , Huang, W. , Wang, F. , Wang, S. , Zhang, Z. & Zhang, Z. (2013) A 3‐year prospective clinical study of telescopic crown, bar, and locator attachments for removable four implant‐supported maxillary overdentures. The International Journal of Prosthodontics 26: 566–573. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. PRISMA 2009 Checklist.


