Abstract
Introduction
One of the most common late complications following stoma construction is prolapse. Although the majority of prolapse can be managed conservatively, surgical revision is required with incarceration/strangulation and in certain cases laparotomy and/or stoma reversal are not appropriate. This report will inform surgeons on safe and effective approaches to revising prolapsed stomas using local techniques.
Presentation of case
A 58 year old female with an obstructing rectal cancer previously received a diverting transverse loop colostomy. On completion of neoadjuvant treatment, re-staging found new lung metastases. She was scheduled for further chemotherapy but incarcerated a prolapsed segment of her loop colostomy. As there was no plan to resect her primary rectal tumor at the time, a local revision was preferred. Linear staplers were applied to the prolapsed stoma in step-wise fashion to locally revise the incarcerated prolapse. Post-operative recovery was satisfactory with no complications or recurrence of prolapse.
Discussion
We detail in step-wise fashion a technique using linear stapler devices that can be used to locally revise prolapsed stoma segments and therefore avoid a laparotomy. The procedure is technically easy to perform with satisfactory post-operative outcomes. We additionally review all previous reports of local repairs and show the evolution of local prolapse repair to the currently reported technique.
Conclusion
This report offers surgeons an alternative, efficient and effective option for addressing the complications of stoma prolapse. While future studies are needed to assess long-term outcomes, in the short-term, our report confirms the safety and effectiveness of this local technique.
Keywords: Stoma, Prolapse, Local revision, Stapler, Case report
Highlights
-
•
Local repair of stoma prolapse avoids the consequences of a major laparotomy.
-
•
Step-wise application of linear staplers effectively repairs prolapsed stomas.
-
•
Patient outcomes are satisfactory after local repairs.
1. Introduction
Stoma prolapse is one of the most common late complications after stoma construction with reported incidence of 2–26% [1]. Although prolapse is observed with any type of ostomy, loop ostomies have a higher incidence of prolapse [1]. In these cases, the prolapsed segment typically involves the distal limb of the loop ostomy [1], [2], [3]. Prolapsed segments are usually not life-threatening but may lead to alterations in cosmesis and difficulty in fitting stoma appliances. In cases of prolapse where manual reduction is difficult due to edema, local osmotic therapy using sugar can decrease the edema and facilitate reduction of the prolapsed segment [4]. When prolapse cannot be reduced, bowel incarceration and strangulation can occur. In these situations, exploratory laparotomy may be necessary with revision of the stoma, stoma reversal if appropriate, or complete relocation of the stoma [4].
For certain patients, laparotomy may be associated with significant morbidity and therefore additional surgical options are needed. In this report, we describe a technique for local revision of stoma prolapse using stapler devices that avoids the need for a laparotomy. While this technique has been partly described by other surgeons [5], [6], [7], [8], [9], [10], previous reports are heterogeneous in detail and visual descriptions are quite limited. We therefore reviewed all reported cases of local prolapse revisions and comprehensively detail a summary technique in a step-by-step graphical manner.
2. Presentation of case
2.1. Patient presentation
A 58 year old African American female with rectal cancer was referred for further management. She had been initially diagnosed with a near-obstructing rectal mass at 10 cm from the anal verge and underwent a diverting transverse loop colostomy at an outside hospital. She was staged by endorectal ultrasound (ERUS) and magnetic resonance imaging (MRI) to be T3N1 and pathology from biopsies were consistent with adenocarcinoma. The patient underwent chemo-radiotherapy and was found on re-staging to have new multiple lung lesions suspicious for metastatic disease. This was subsequently confirmed on wedge biopsy. As she underwent evaluation for further chemotherapy, she presented with an acutely incarcerated, prolapsed distal segment of the transverse loop colostomy. Attempts at reduction were unsuccessful. Local revision of the prolapsed segment was planned as there was no intention to resect the lung lesions or primary rectal tumor at this time. Informed consent was obtained for local revision with possible conversion to laparotomy.
2.2. Intervention
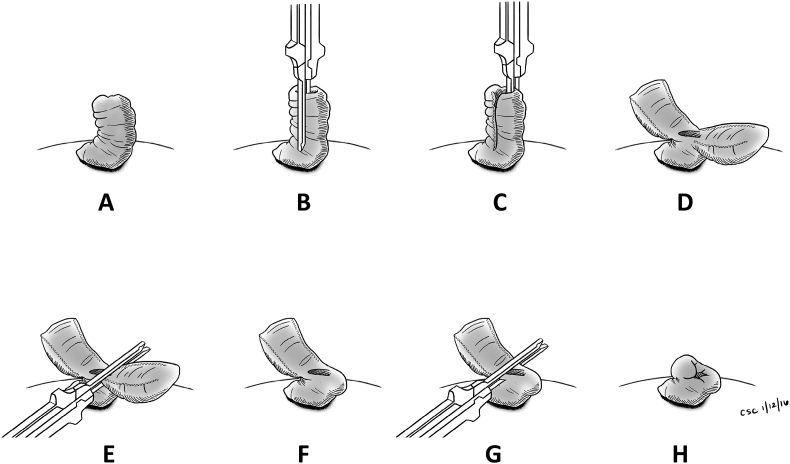
The patient underwent general anesthesia and was placed in the supine position. After administration of preoperative antibiotics, the prolapse segment was examined and confirmed to be the distal limb of the loop transverse colostomy (Fig. 1, Fig. 2). The segment was incarcerated and could not be reduced even under general anesthesia. At this point, a gastrointestinal linear stapler (GIA 100; Covidien, Mansfield, MA, USA) was inserted into the lumen of the stoma and used to transect the prolapsed stoma in a longitudinal fashion at the superior, twelve o'clock position to approximately 1-cm from the skin (Fig. 2B). A second GIA stapler was used to transect the prolapsed stoma at the inferior, six o'clock position (Fig. 2C). These two staple lines bisected the prolapsed segment into two halves (Fig. 2D). The base of each half was then transected at approximately 1 cm above the skin level in a perpendicular fashion with two additional GIA stapler loads (Fig. 2E–G). A total of four staple loads (two for the bisection and two for the base of each half) were thus used in the entire procedure. On final appearance, the circumferential margin of the stoma was reconstructed with complete removal of the prolapsed segment and a 1-cm bud above the skin level (Fig. 2, Fig. 3). There was minimal blood loss and the lumen of both proximal and distal ends of the loop colostomy were widely patent. After application of a stoma appliance the patient was awoken and taken to the recovery area.
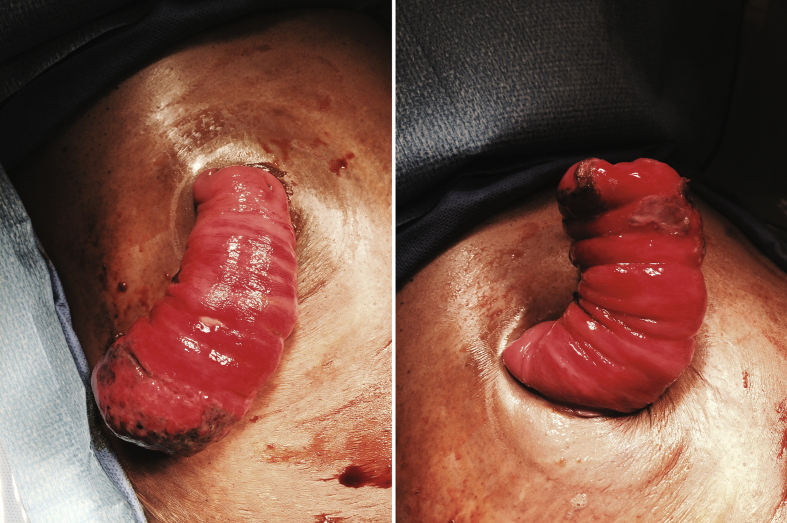
Fig. 1.
Photograph of incarcerated stoma prolapse. Visualized is an incarcerated segment of the distal aspect of a loop transverse colostomy.
Fig. 2.
Schematic illustrating the complete step-by-step local revision of stoma prolapse using linear stapling devices. A. Prolapsed segment. B. First application of linear stapler in the longitudinal plane. C. Second application of linear stapler on the opposite side but in the longitudinal plane. D. Bisection of the prolapsed segment. E. Third application of the linear stapler at a perpendicular angle to transect the base of one half. F. Appearance after transection of one half. G. Fourth application of the linear stapler to transect the remaining bisected half. H. Final appearance of revised stoma.
Fig. 3.
Final appearance of stoma after local revision.
3. Results
No intraoperative or postoperative complications occurred. Entry into the abdomen was completely avoided. In the recovery phase, no narcotic medications were required as the patient had minimal pain requirements and oral intake was resumed the day of surgery. Stoma function returned and she was dismissed on post-operative day one. On four-week post-operative follow-up, she had no evidence for recurrent prolapse, obstruction or other complications. The patient was satisfied with her care and is currently receiving additional chemotherapy for progression of disease with new lung metastasis.
4. Discussion
In this report, we describe a technically easy, safe and effective approach to locally revise complications of stoma prolapse. This technique uses commonly available linear staplers to remove incarcerated segments of prolapsed intestine and avoids a laparotomy. After four applications of the stapler to the prolapsed segment, the final appearance of the revised stoma was satisfactory (Fig. 3). Functional outcome was also excellent with rapid recovery of bowel function. The entire procedure was completed in less than thirty minutes with no intra-operative or post-operative complications. The local revision technique described in this report should be part of the armamentarium of any surgeon who manages stomas and their potential complications.
Stoma construction is an important and often under-appreciated technique for many surgical specialties. Both early and late complications may occur with stomas. Early complications, which occur within 30-days of stoma construction, include vascular compromise, stoma retraction, skin irritation secondary to poor stoma siting, peristomal abscess/fistula, parastomal hernias and early postoperative bowel obstruction. Errors such as maturation of the wrong end of the stoma are also possible. Of the late complications that can occur, stoma prolapse is one of the most common and has a reported incidence between 2 and 26% [1]. Presence of prolapse itself is not an indication for surgical repair; however, it can alter quality of life for patients and may incarcerate (as in our case) or even strangulate.
Many surgical techniques have been used to address stoma prolapse [2]. These techniques can be broadly classified into abdominal or local approaches. The abdominal approach involves reversing, re-doing or re-siting the stoma; each of these procedures carries the morbidities associated with intraabdominal entry, potential anastomoses and re-operative surgery. The local approach to revising stoma prolapse intends to avoid these morbidities. Initial reports of local revisions applied the principles of the Altemeier [11] and Delorme techniques [12] to remove prolapsed intestinal segments. More recently, revisions have been performed with stapler devices, which allow for fewer steps and less operative time [5], [6], [7], [8], [9], [10].
A review of all reported cases of local prolapse revisions are summarized in Table 1. The earliest description was reported by Trentin et al. [10] in Italy using a curved stapler to resect the prolapsed mucosal stoma. Ferguson et al. [6] also used a curved stapler in addition to a straight one to resect a prolapsed end colostomy. In their description, a straight stapler was applied to the stoma at oblique angles along the bowel. This was followed by application of a curved stapler (CONTOUR; Ethicon, Somerville, NJ, USA) to amputate the two remaining halves above the mucocutaneous junction. The remainder of the case reports on local revision apply variations of these staplers. Maeda et al. [9] made a full thickness incision through one side of the prolapsed ostomy prior to transverse resection of the redundant tissue via the straight stapler. Masumori et al. [5] were able to reduce the application of the straight stapler to only one firing across the entire ostomy in a transverse fashion. All cases reviewed involved ostomies of various configurations including end colostomy, loop colostomy, end ileostomy and mucus fistula. Operative times ranged from twenty minutes [7] to fifty-nine minutes [9]. Several of these case reports used local anesthesia [5], [6], [7], [8], [10]. In all reported cases thus far, no complications or recurrences were reported with local techniques.
Table 1.
Summary of reported local revisions of stoma prolapse.
| Year | Journal/Location | Authors | Number of patients | Type of ostomy | Method | Outcomes |
|---|---|---|---|---|---|---|
| 2003 | Chirurgia Italiana Presidio Ospedaliero Di Vittorio Veneto Italy |
Trentin G, De Simone P, Mainente P, Agresta F, Bedin N | 1 | Mucus fistula | Circular stapler applied to prolapse mucosal stoma | No complications |
| 2004 | Techniques in Coloproctology Fujita Health University Toyoake, Japan |
Maeda K, Maruta M, Utsumi T et al. | 2 | Loop colostomy | Linear stapler applied to each side of one limb of ostomy via longitudinal incisions | No complications |
| 2005 | Digestive Surgery Sapporo Medical University Sapporo, Japan |
Hata F, Kitagawa S, Nishimori H et al. | 6 | Ileostomy and ascending colostomy | Linear stapler with two vertical and horizontal applications | No complications |
| 2005 | Techniques in Coloproctology University Hospital of Larissa Larissa, Greece |
Tepetes K, Spyridakis M, Jatzitheofilou C | 1 | Loop colostomy | Linear stapler with two vertical and horizontal applications | Patient discharged without issue; died 3 months later without stomal complications |
| 2010 | Techniques in Coloproctology City Hospital Birmingham, UK |
Ferguson HJM, Bhalerao S | 1 | End colostomy | Straight stapler applied at oblique angles followed by curved stapler | No complication |
| 2012 | Techniques in Coloproctology Fujita Health University Toyoake, Japan |
Masumori K, Maeda K, Koide Y, Hanai T, Sato H, Matsuoka H, Katsuno H, Noro T | 2 | Distal limb of loop colostomy | Linear stapler applied to whole ostomy transversely | One patient with stoma closure and one without recurrence 4 years later |
5. Conclusion
Surgeons who construct stomas and manage their complications should be familiar with local approaches to addressing stoma prolapse. When laparotomy and/or stoma reversal is not appropriate, local revision of stoma prolapse provides a low-risk and high-benefit alternative solution. Our comprehensive review of all reported cases of local stoma revision shows that patient outcomes are very favorable with satisfactory function and appearance. Local techniques have gravitated towards the application of linear staplers to remove prolapsed intestinal segments. Our report confirms the safety and effectiveness of this local technique and furthermore summarizes the step-by-step process in an easy-to-follow visual description (Fig. 2) to assist with future application of this technique. Future studies are needed to assess long-term outcomes of local revisions, but in the short-term, the local technique described in this study provides surgeons with an alternative and effective option for addressing the complications of stoma prolapse.
Ethical approval
All procedures followed were in accordance with the ethical standards of the institution.
Sources of funding
No funding.
Author contribution
All authors contributed equally to the study design, data collection, analysis/interpretation, writing and drafting of this manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Acknowledgements
We would like to thank Christine S. Chen for her medical illustrations.
References
- 1.Husain S., Ctaldo T. Late stomal complications. Clin. Colon Rectal Surg. 2008;21:31–40. doi: 10.1055/s-2008-1055319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim J., Kumar R. Reoperation for stoma-related complications. Clin. Colon Rectal Surg. 2006;19(4):207–212. doi: 10.1055/s-2006-956441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Geisler D., Glennon E. Intestinal stomas and their complications. Colorectal Surg. 2013;28:440–455. [Google Scholar]
- 4.Park J., Del Pino A., Orsay C. Stoma complications. Dis. Colon Rectum. 1999;42:1575–1580. doi: 10.1007/BF02236210. [DOI] [PubMed] [Google Scholar]
- 5.Masumori K., Maeda K., Koide Y., Hanai T., Sato H., Matsuoka H., Katsuno H., Noro T. Simple Excision and closure of a distal limb of loop colostomy prolapse by stapler device. Tech. Coloproctol. 2012;16:143–145. doi: 10.1007/s10151-011-0785-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferguson H., Bhalerao S. Correction of end colostomy prolapse using a curved surgical stapler, performed under sedation. Tech. Coloproctol. 2010;14:165–167. doi: 10.1007/s10151-010-0568-1. [DOI] [PubMed] [Google Scholar]
- 7.Tepetes K., Spyridakis M., Jatzitheofilou C. Local treatment of loop colostomy prolapse with a linear stapler. Tech. Coloproctol. 2005;9:156–158. doi: 10.1007/s10151-005-0217-2. [DOI] [PubMed] [Google Scholar]
- 8.Hata F., Kitagawa S., Nishimori H. A novel, easy, and safe technique to repair a stoma prolapse using a surgical staple device. Dig. Surg. 2005;22:306–310. doi: 10.1159/000088626. [DOI] [PubMed] [Google Scholar]
- 9.Maeda K., Maruta M., Utsumi T. Local correction of a transverse loop colostomy prolapse by stapler device. Tech. Coloproctol. 2004;8:45–46. doi: 10.1007/s10151-004-0051-y. [DOI] [PubMed] [Google Scholar]
- 10.Trentin G., De Simone P., Mainente P., Agresta F., Bedin N. Repair of mucosa stomal prolapse with circular stapler. Chir. Ital. 2003;55(1):141–143. [PubMed] [Google Scholar]
- 11.Corman M.L. fifth ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2005. Colon and Rectal Surgery. [Google Scholar]
- 12.Abulafi A.M., Sherman I.W., Fiddian R.V. Delorme operation for prolapsed colostomy. Br. J. Surg. 1989;76:1321–1322. doi: 10.1002/bjs.1800761234. [DOI] [PubMed] [Google Scholar]