Abstract
Objectives. To compare the effectiveness of a (CEP) versus a technical assistance approach (Resources for Services, or RS) to disseminate depression care for low-income ethnic minority women.
Methods. We conducted secondary analyses of intervention effects for largely low-income, minority women subsample (n = 595; 45.1% Latino and 45.4% African American) in a matched, clustered, randomized control trial conducted in 2 low-resource communities in Los Angeles, California, between 2010 and 2012. Outcomes assessed included mental health, socioeconomic factors, and service use at 6- and 12-month follow-up.
Results. Although we found no intervention difference for depressive symptoms, there were statistically significant effects for mental health quality of life, resiliency, homelessness risk, and financial difficulties at 6 months, as well as missed work days, self-efficacy, and care barriers at 12 months favoring CEP relative to RS. CEP increased use of outpatient substance abuse services and faith-based depression visits at 6 months.
Conclusions. Engaging health care and social community programs may offer modest improvements on key functional and socioeconomic outcomes, reduce care barriers, and increase engagement in alternative depression services for low-income, predominantly ethnic minority women.
Depression is expected to be the second-leading cause of adult disability worldwide by 2030.1 Women have 1.5 to 3 times the risk of depression as men.2 In addition, poverty and mental illness interact in a negative spiral,3 especially for low-income minority women, who are exposed to greater environmental stressors and have limited access to resources, which can increase the risk of depression morbidity and mortality.4,5 Thus, depression interventions for low-income, ethnic minority women may benefit from service planning that takes into consideration socioeconomic factors.
Despite the great need, low-income, ethnic minority communities continue to have significant barriers to accessing available mental health services because of low depression literacy, mental health stigma, inconsistent transportation, child care, work schedules, cost, and being uninsured.5,6 In addition, mental health care systems in low-income communities are often underresourced, with provider shortages and highly variable availability of evidence-based and quality depression services.7,8
Primary care–based depression quality improvement (QI) has been recommended to address this gap. Depression QI interventions incorporating screening, care coordination, psychoeducation, and evidence-based treatments have increased access to and the quality of depression care for diverse, low-resource settings worldwide.9,10 However, despite the effectiveness of depression QI, little research exists on the best strategies to disseminate communitywide depression QI in low-income, underresourced communities. Given the barriers to accessing care and the long-standing distrust in low-income ethnic communities of both research and services, community engagement models may support health systems to scale up depression QI to meet Affordable Care Act mandates. For example, current policy initiatives such as Medicaid Behavioral Health Homes and Accountable Care Communities incentivize partnerships across general medical, mental health, and social and community sectors to manage chronic illnesses in low-income communities.11 However, limited systematic evidence exists to inform policymakers on strategies for partnerships across health and community-based agencies to address depression identification and care coordination, while concurrently attending to community context and individual social risk factors such as homelessness.12
Community Partners in Care (CPIC) is the first randomized study to compare communitywide dissemination models for depression care for underresourced, ethnic minority communities in the United States. CPIC expands more traditional QI to engage a larger network of health and community–social sectors for depression identification and care, using community-partnered participatory research,13,14 a community-based participatory research model to address health disparities.15 The trial compared a community engagement and planning participatory network (CEP) approach with a technical assistance approach (Resources for Services, or RS) and found that CEP, which supported the community in implementing a communitywide network for depression care, improved clients’ mental health quality of life and mental wellness, increased physical activity, reduced homelessness risk factors, and reduced rates of behavioral health hospitalization and medication visits among specialty care users at 6-month follow-up. CEP increased primary care and public health visits for depression and use of faith-based and park programs for depression.16 At 12-month follow-up, we found reductions in poor mental health quality of life and reduced hospitalizations in CEP relative to RS, but they were sensitive to statistical modeling.17 These findings suggest the importance of community collaboration, activation of community networks, and, particularly, the role of faith-based and community-trusted organizations to address unmet depression needs in underresourced populations.
CPIC’s CEP dissemination strategy for depression QI focused on activating community networks to develop community-tailored solutions to improve depression services, which we believe to be particularly effective for addressing mental health and social risk factors for low-income, ethnic minority women. The expanded partnerships under CEP may more effectively address financial stressors, provide social support, and overcome barriers to services. This secondary analysis focused on intervention outcomes for women in the CPIC study, to determine whether the added benefits of CEP relative to RS observed for the whole sample also applied specifically to women, in terms of health, functional, and social indicators (financial risk factors, life difficulties) and service utilization at 6 and 12 months.
METHODS
CPIC is a group-level, randomized comparative effectiveness trial designed and implemented using community-partnered participatory research model that promotes equal authority and coleadership of community and academic partners in all research phases, following principles of community engagement. Our process was guided by a partnered and jointly owned formal infrastructure headed by a community–academic council that supported work groups and community forums to build capacity in both community and academic contexts for culturally sensitive, evidence-based practice that could be sustained beyond the study period.15,18 The study’s community-partnered participatory research process, design details, and results at baseline, 6-month follow-up, and 12-month follow-up can be found in previous publications.16,17,19,20
Interventions
The interventions represent 2 dissemination models for depression QI across health, social service, and other community-based programs. Both RS and CEP used the same evidence-based depression QI toolkits, originally developed in We Care21 and Partners in Care,22 which included manuals for cognitive behavioral therapy for depression,23,24 clinician assessment and medication management, care managers to support depression screening, care coordination and treatment adherence, and patient education materials. All materials were available in hard copy, on a Web site, and on flash drives, and were introduced together with the study design to community agencies in kickoff conferences prior to enrollment.
Resources for Services.
RS used culturally competent outreach to engage programs and provide technical assistance to implement QI components, using a “train-the-trainer” approach to build capacity in depression care from December 2009 through July 2010. An expert team of 3 psychiatrists, a nurse care manager, a cognitive behavioral therapy trainer, a QI expert, and support staff worked with a community outreach specialist to offer 12 webinars on team management, cognitive behavioral therapy, care management, and patient education. Site visits were also provided to primary care sites to train providers on medication management.
Community Engagement and Planning.
CEP involved a community-academic partnered process to colead, develop, and implement a written training and implementation plan tailored by community and academic partners for both the South Los Angeles and Hollywood communities between December 2009 and July 2011. CEP promoted community engagement, 2-way capacity building, and shared project participation and ownership. The CEP plans featured multiple community conferences, additional as-needed training sessions for individual programs, webinars and supervision, and webinars on cognitive behavior therapy and case management for therapists, case managers and health workers. The CEP process led to the development of innovations such as adding alternative medicine to medication management, incorporation of provider self-care to trainings, book clubs, and a resiliency intervention. Trainings were also led by program staff, community partners, and study experts. (See Khodyakov et al.25 for more details on CEP features, process, and experiences.) CEP offered more training opportunities, had more staff participation, and provided more total training hours than RS.26
Sample and Randomization
We conducted the CPIC study in 2 communities in Los Angeles County Service Planning Areas—South Los Angeles and Hollywood–Metropolitan—that have high rates of unemployment, homelessness, and avoidable hospitalizations and low rates of insurance.
Agencies and programs.
Using county lists and partner nominations, we recruited agencies and venues offering services identified by community members as relevant to depression (mental health specialty, primary care and public health, substance abuse, social services, faith-based services, park centers, hair salons, and exercise clubs). Eligible agencies offered services to adults or parents of children, were financially stable (i.e., expected to operate 1–3 years), and were selected to oversample 4 community-prioritized subgroups (the homeless, seniors, African Americans, those in substance abuse programs). Eligible programs included those (1) serving 15 or more clients per week, (2) having 2 or more staff members (or 1 or more for senior centers, businesses, and faith-based programs), and (3) not focused on psychotic disorders or home services. Within each community, we paired programs into units based on location, service sector, size, and funding sources, with large agencies as 1 stratum. Within pairs, units were randomized to each intervention by a statistician uninvolved in recruitment. Agency and program enrollment occurred November 6, 2008, through August 17, 2010. Within 60 potentially eligible agencies having 194 programs, we confirmed that 133 programs were potentially eligible and randomized them (65 RS, 68 CEP). To finalize enrollment, postrandomization site visits were conducted by RAND staff blinded to assignment; 20 programs were ineligible, 18 programs refused, and 95 programs from 50 consenting agencies enrolled (46 RS, 49 CEP). Sensitivity analyses found that participating and nonparticipating programs were comparable by age, gender, race, population density, and income by zip code–level census tract data (each P > .10).16,20
Client participants.
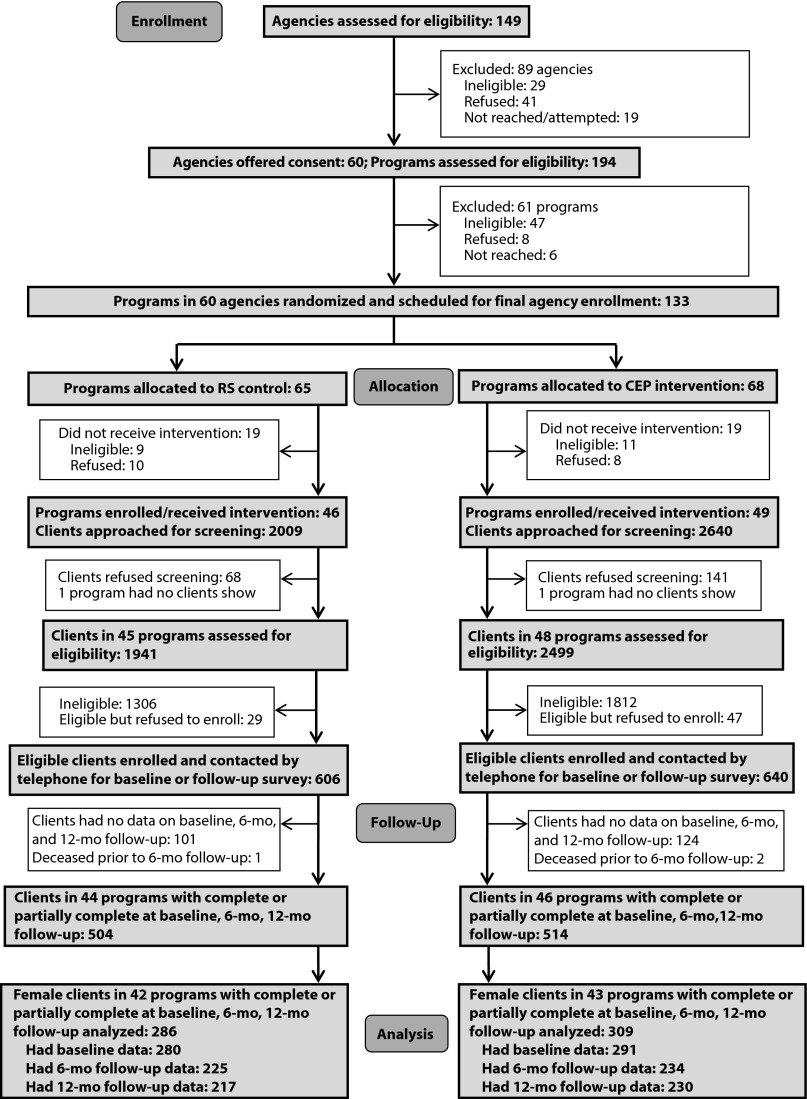
Within programs, between March 2010 and November 2010, clients were screened for eligibility in waiting rooms or at events by community members blinded to intervention condition and supervised by RAND. Staff approached 4649 adults per program over 2 to 3 days; 4440 (95.5%) agreed to screening in 93 enrolled programs. Study eligibility was limited to clients providing contact information and screening positively for depression (i.e., scoring ≥ 10 on the 8-item Patient Health Questionnaire [PHQ-8]).27 Of 4440 screened, 1322 (29.8%) were eligible, and of these, 1246 (94.3%) consented. RAND survey staff blinded to intervention condition conducted telephone surveys on 981 participants at baseline, 759 at 6-month follow-up, and 733 at 12-month follow-up. The study main analytic sample comprised 1018 participants (77% of those eligible, 82% of those enrolled) who completed 1 assessment at baseline or at 6- or 12-month follow-up; the 595 female participants constituted the analytic sample.16,17 Figure 1 shows the study profile.
FIGURE 1—
Trial Profile: Community Partners in Care, Women’s Substudy, Los Angeles, CA, 2010–2012
Note. CEP = Community Engagement and Planning; RS = Resources for Services, or individual program technical assistance.
Baseline and Outcome Assessment
Baseline measures from screener and telephone surveys included demographics (age, gender); the presence of at least 3 of 18 chronic physical health conditions (e.g., diabetes, cancer, heart disease); educational level and race/ethnicity; physical and mental health scores from the 12-item Short Form Health Survey (SF-12)28; and an indicator of meeting census poverty thresholds by size of family and number of children in 2010. Using the Mini International Neuropsychiatric Interview 6,29 an empirically validated structured diagnostic interview,30,31 we created indicators for probable major depressive or dysthymic disorder in the past 12 months, current mania, recent anxiety (in the past month for panic or posttraumatic stress or the past 6 months for generalized anxiety disorder), and alcohol abuse or use of illicit drugs in the past 12 months.
Client outcomes.
Mental health and functioning outcomes included depression symptoms (PHQ-9)32 and poor mental health–related quality of life (i.e., ≤ 40 [1 SD below population mean] on the 12-item Mental Health Component Score28).33
Resilience.
A community-partnered process resulted in outcomes prioritized by community members to assess wellness and resilience. We defined mental wellness as “at least a good bit of time” (score of ≥ 3 on a 6-point Likert scale, range = 1–6) on any of 3 items: feeling calm or peaceful,34 having energy, or being happy in the prior 4 weeks.16 We identified physical activity as an indicator of resiliency; using a single 6-point Likert scale item, we defined it as being at least fairly physically active.16
Socioeconomic indicators.
Employment indicators included single items on working for pay and number of missed work days in the past 30 days among those employed. Homelessness risk included either currently being homeless or living in a shelter, or having multiple risk factors for future homelessness; these included having no place to stay for 2 or more nights in the past 6 months or eviction from primary residence, a financial crisis, or food insecurity in the past 6 months.35,36
We measured life stressors by the presence over the past 12 months of various stressful events, divided into 3 subscales: financial problems (8 items; e.g., laid off or fired from work), loss and trauma (3 items; e.g., “someone close to me died”), and relationship problems (3 items; e.g., serious argument with someone at home).37
Barriers to care included questions about structural barriers (7 items; e.g., high cost, no one at clinic speaking respondent’s language) and logistical barriers (4 items; e.g., not being able to get an appointment, no child care).38
We assessed depression-related self-efficacy by averaging 3 items on a 10-point scale in which respondents indicated (at baseline and 12-month follow-up) how confident they were that they could overcome or control depression, take effective action to treat depression, and manage the side effects of antidepressant medications.39 Only 1 item (“How confident are you in your ability to overcome or control a bout of depression?”) was assessed at 6-month follow-up.
Service use.
We developed service use indicators based on counts in the last 6 months for the following: overnight hospital stays for mental health or substance abuse, emergency department visits, outpatient mental health, self-help groups, outpatient primary care or public health, outpatient substance abuse, overnight substance abuse rehabilitation, social services, faith-based programs, and park community centers. For mental health service utilizers, we developed counts of medication and counseling visits. For other sectors, we developed number of visits at which clients reported receiving information, referral, counseling, or medication management for depression or mental health.
Data Analysis
We examined intervention effects to determine whether CEP was more effective than RS in improving mental health and functioning, resiliency, economic risk, stressors, barriers to care, self-efficacy, and service utilization for low-income minority women. We described baseline differences between CEP and RS using bivariate analyses. We conducted intent-to-treat analyses, in which patients were included in the analysis according to their original assignment, irrespective of whether they received services from the location where they were initiated into care or whether they used intervention resources. We used linear regression for continuously scaled outcome variables, logistic regression for dichotomous measures, and Poisson regression models for counts, with intervention status as the independent variable. Consistent with group-randomized trial recommendations,40 we adjusted for baseline status of dependent variables and covariates (age, education, race/ethnicity, prior 12-month depressive disorder, and community). We adjusted barriers to care—measured only at follow-ups—for baseline insurance status, a proxy for barriers to care.
The CPIC main study used nonresponse weighting41,42 to address missing data for nonenrollment among eligible clients and for attrition. We also used a hot-deck multiple imputation technique for item nonresponse and an approximate Bayesian bootstrap for unit nonresponse among the analytic sample. We conducted imputations for less than 5% for all variables except for baseline income and Mini International Neuropsychiatric Interview variables, which had higher rates of item-level missingness. For all female subpopulation analyses, we used Taylor series linearization with a subpopn statement in SUDAAN version 11.0.1 (RTI International, Research Triangle, NC), accounting for clustering (clients within programs),43 weighting, and multiple imputations.44 Significance of comparisons by intervention status was based on regression coefficients. Results of linear regression models are presented as between-group difference, logistic regression models are presented as odds ratios, and Poisson regression models are presented as incidence rate ratios with 95% confidence intervals; we considered P < .05 to be statistically significant. We illustrate results for intervention groups adjusted for covariates using standardized predictions generated from fitted regression models.45 The detailed procedure, which has been described elsewhere,16,17 is given in the Appendix (available as a supplement to the online version of this article at http://www.ajph.org).
In addition to our primary analyses, we conducted 2 sensitivity analyses to ascertain whether our findings were sensitive to imputation and weighting. We compared results from the final model—using weighted and imputed data adjusted for baseline variables, covariates, and clustering—with results from (1) an unadjusted model using available data without imputation and weighting and (2) an adjusted model accounting for baseline dependent variables and covariates and clustering using unweighted raw data without imputation. Final fully adjusted models reported in our results were robust, as these models produced qualitatively similar results. See the online Appendix for a detailed description.
RESULTS
Table 1 describes the baseline characteristics of women in our sample. At baseline, the sample included 595 women, of whom 45.1% were Latinas, 45.4% African Americans, 7.1% non-Hispanic Whites, and 2.4% of other ethnic groups. Women averaged 45 years old (SD = 13); 24.4% were married or living with a partner, and nearly half had less than a high school education. Three quarters of the women had incomes under the federal poverty level, with 73% reporting a family income of $10 000 or less in the year prior to baseline. Nearly half (46.6%) had no health insurance or were either homeless or had multiple risk factors for homelessness (48.6%). Only 20.8% were working for pay, and among those employed, 61.7% reported missed working days in the last 30 days. We found no differences regarding demographic and socioeconomic variables, mental health, functioning, life difficulties, or depression self-efficacy across the CEP and RS arms.
TABLE 1—
Baseline Sociodemographic, Clinical, and Social Risk Factors: Community Partners in Care, Women’s Substudy, Los Angeles, CA, 2010–2012
| Variable | Overall (n = 595), No. (%) or Mean ±SD | RS (n = 286), No. (%) or Mean ±SD | CEP (n = 309), No. (%) or Mean ±SD |
| Age, y | 45.0 ±13.0 | 44.0 ±12.6 | 45.8 ±13.4 |
| Race/ethnicity | |||
| Latino | 262 (45.1) | 117 (41.5) | 145 (48.2) |
| African American | 283 (45.4) | 141 (48.3) | 142 (42.8) |
| Non-Hispanic White | 38 (7.1) | 18 (7.0) | 20 (7.2) |
| Other | 12 (2.4) | 10 (3.1) | 2 (1.7) |
| Married or living with partner | 146 (24.4) | 76 (26.4) | 70 (22.7) |
| < high school education | 285 (47.9) | 137 (47.7) | 147 (48.0) |
| Income under federal poverty level | 445 (74.8) | 203 (71.2) | 241 (78.0) |
| Family income from work past 12 mo ≤ $10 000 | 438 (73.0) | 208 (73.0) | 230 (73.0) |
| Working for pay | 123 (20.8) | 63 (22.2) | 60 (19.6) |
| Any missed work day in last 30 d among employed (n = 123) | 76 (61.7) | 39 (62.4) | 37 (60.8) |
| Mental health and well-being | |||
| Depressive disorder in past 12 mo | 344 (57.9) | 163 (57.6) | 181 (58.2) |
| Alcohol abuse or use of illicit drugs in past 12 mo | 182 (30.5) | 70 (24.5) | 112 (35.8) |
| PHQ-8 | 14.8 ±4.1 | 15.0 ±4.1 | 14.6 ±4.0 |
| Poor mental health quality of life, MCS-12 ≤ 40 | 311 (51.8) | 155 (54.8) | 156 (49.3) |
| Mental wellness | 240 (40.1) | 110 (37.8) | 130 (42.1) |
| Physical activity | 271 (45.8) | 136 (47.8) | 134 (44.0) |
| Chronic health conditions ≥ 2 | 317 (54.2) | 151 (53.5) | 166 (54.8) |
| Social determinants and risk factors | |||
| Homeless or ≥ 2 risk factors for homelessness | 285 (48.6) | 148 (52.6) | 137 (45.0) |
| No health insurance | 273 (46.6) | 135 (47.1) | 138 (46.2) |
| Life difficulties total score | 3.8 ±2.6 | 4.0 ±2.6 | 3.6 ±2.7 |
| Financial difficulties subscale | 2.3 ±1.8 | 2.5 ±1.8 | 2.2 ±1.8 |
| Loss and trauma subscale | 0.5 ±0.7 | 0.5 ±0.6 | 0.4 ±0.7 |
| Relationship problems subscale | 0.9 ±0.9 | 0.9 ±0.9 | 0.8 ±0.9 |
| Depression treatment self-efficacy | 5.9 ±2.3 | 5.9 ±2.3 | 6.0 ±2.3 |
Note. CEP = Community Engagement and Planning; MCS-12 = 12-item Mental Health Component Summary Score; PHQ-8 = 8-item Patient Health Questionnaire; RS = Resources for Services, or individual program technical assistance. Data were multiply imputed and weighted for eligible sample for enrollment; χ2 test was used for a comparison between the 2 groups, accounting for the design effect of the cluster randomization; P > .05 for all comparisons.
At baseline, 57.9% had probable depressive disorder and 30.5% had alcohol or illicit drug use (both in the past 12 months), and 54.2% had 3 or more current chronic conditions. A total of 51.8% reported poor mental health quality of life, with women on average scoring as moderately depressed (mean PHQ-8 = 14.8; SD = 4.1).
Intervention Effects on Clinical and Social Outcomes
Table 2 describes intervention effects for female clients’ health, functional, and social outcomes at 6- and 12-month follow-up. Intervention effects (CEP vs RS) were not significant for depression symptoms or alcohol use at either 6 or 12 months. However, at 6 months, statistically significant intervention effects were found for poor mental health quality of life, mental wellness, physical activity, homelessness risk, life stressors, and financial difficulties. At 12 months, statistically significant intervention effects were found for poor mental health quality of life, likelihood of missed worked days among working women, barriers to care, and depression self-efficacy. Specifically, at 6 months, relative to RS, CEP reduced the odds of poor mental health quality of life (12-item Mental Health Component Summary Score ≤ 40; odds ratio [OR] = 0.62; 95% confidence interval [CI] = 0.43, 0.88), homelessness risk (OR = 0.52; 95% CI = 0.33, 0.83), having 4 or more life stressors (OR = 0.69; 95% CI = 0.49, 0.99), and number of financial difficulties (group difference = −0.27; 95% CI = −0.054, −0.01). CEP increased the odds of mental wellness (OR = 1.65; 95% CI = 1.10, 2.49) and physical activity (OR = 1.57; 95% CI = 1.06, 2.32). At 12 months, CEP reduced the odds of poor mental health quality of life (OR = 0.69; 95% CI = 0.48, 0.99) and the likelihood of any missed work days among those employed (OR = 0.3; 95% CI = 0.15, 0.95). In addition, relative to RS, CEP reduced the number of structural barriers (group difference = −0.38; 95% CI = −0.72, −0.04) and logistical barriers (group difference = −0.21; 95% CI = −0.41, −0.01), and increased depression self-efficacy (group difference = 0.56; 95% CI = 0.09, 1.04) at 12 months.
TABLE 2—
Clients’ Health, Functional, and Social Outcomes at 6- and 12-Month Follow-Up, by Intervention Status: Community Partners in Care, Women’s Substudy, Los Angeles, CA, 2010–2012
| Variable | RS Estimate, Mean or % (95% CI) | CEP Estimate, Mean or % (95% CI) | Between-Group Difference or OR (95% CI) |
| 6-mo follow-up (n = 595) | |||
| Depression symptoms, PHQ-9 | 12.8 (11.7, 13.8) | 12.4 (11.4, 13.5) | −0.35 (−1.87, 1.17) |
| Total no. life stressors | 2.9 (2.6, 3.3) | 2.6 (2.3, 2.9) | −0.33 (−0.68, 0.01) |
| Financial difficulties | 1.8 (1.6, 2.0) | 1.6 (1.4, 1.8) | −0.27 (−0.54, −0.01) |
| Relationship problems | 0.6 (0.5, 0.7) | 0.6 (0.5, 0.7) | −0.06 (−0.17, 0.06) |
| Loss and trauma | 0.4 (0.3, 0.5) | 0.4 (0.3, 0.4) | −0.04 (−0.13, 0.06) |
| No. structure barriers | 1.5 (1.3, 1.8) | 1.5 (1.3, 1.7) | −0.02 (−0.33, 0.28) |
| No. logistic barriers | 1.1 (0.9, 1.2) | 1.1 (1.0, 1.3) | 0.06 (−0.11, 0.24) |
| Depression self-efficacya | 5.9 (5.5, 6.3) | 6.2 (5.7, 6.7) | 0.29 (−0.40, 0.97) |
| Poor mental health QOL MCS-12 ≤ 40b | 55.1 (48.8, 61.2) | 43.5 (37.0, 50.2) | 0.62 (0.43, 0.88) |
| Hazardous drinker or alcohol use disorderb | 16.0 (10.9, 22.8) | 14.3 (9.5, 20.6) | 0.85 (0.39, 1.87) |
| Mental wellnessb | 34.8 (29.0, 41.1) | 46.0 (39.8, 52.4) | 1.65 (1.10, 2.49) |
| Physical activityb | 38.7 (32.5, 45.4) | 48.5 (41.3, 55.8) | 1.57 (1.06, 2.32) |
| Homelessness riskb | 39.7 (32.9, 46.9) | 26.6 (20.9, 33.1) | 0.52 (0.33, 0.83) |
| Working for payb | 21.9 (17.8, 26.6) | 23.7 (17.9, 30.5) | 1.13 (0.74, 1.73) |
| Any missed work day in last 30 d if workingb,c | 61.8 (46.3, 75.4) | 57.7 (46.2, 68.5) | 0.82 (0.35, 1.94) |
| ≥ 4 life stressorsb,d | 35.2 (29.9, 40.9) | 28.1 (22.1, 34.8) | 0.69 (0.49, 0.99) |
| 12-mo follow-up (n = 593) | |||
| Depression symptoms, PHQ-9 | 12.4 (11.4, 13.4) | 11.8 (11.0, 12.7) | −0.61 (−1.70, 0.49) |
| Total no. life stressors | 2.7 (2.2, 3.1) | 2.5 (2.2, 2.8) | −0.20 (−0.65, 0.25) |
| Financial difficulties | 1.6 (1.4, 1.9) | 1.5 (1.3, 1.7) | −0.11 (−0.40, 0.18) |
| Relationship problems | 0.5 (0.4, 0.7) | 0.5 (0.4, 0.6) | −0.02 (−0.15, 0.11) |
| Loss and trauma | 0.5 (0.4, 0.6) | 0.4 (0.3, 0.5) | −0.10 (−0.24, 0.03) |
| No. structure barriers | 1.6 (1.3, 1.9) | 1.2 (1.0, 1.4) | −0.38 (−0.72, −0.04) |
| No. logistic barriers | 1.0 (0.8, 1.2) | 0.8 (0.7, 1.0) | −0.21 (−0.41, −0.01) |
| Depression self-efficacya | 6.1 (5.8, 6.5) | 6.7 (6.3, 7.1) | 0.56 (0.09, 1.04) |
| Poor mental health QOL MCS-12 ≤ 40 | 53.9 (47.6, 60.2) | 45.0 (37.7, 52.5) | 0.69 (0.48, 0.99) |
| Hazardous drinker or alcohol use disorderb | 14.7 (10.2, 20.5) | 16.0 (10.7, 23.1) | 1.11 (0.65, 1.91) |
| Mental wellnessb | 43.7 (36.3, 51.3) | 47.2 (39.1, 55.5) | 1.17 (0.72, 1.90) |
| Physical activityb | 45.5 (38.2, 52.9) | 43.8 (36.7, 51.1) | 0.93 (0.64, 1.35) |
| Homelessness riskb | 30.3 (23.4, 38.3) | 33.1 (26.2, 40.8) | 1.15 (0.73, 1.80) |
| Working for payb | 22.6 (17.5, 28.6) | 19.4 (14.9, 24.8) | 0.79 (0.48, 1.30) |
| Any missed work day in last 30 d if workingb,c | 65.0 (49.7, 77.9) | 44.2 (28.9, 60.7) | 0.38 (0.15, 0.95) |
| ≥ 4 life stressorsb,d | 31.7 (24.7, 39.6) | 25.1 (19.2, 32.1) | 0.70 (0.44, 1.10) |
Note. CEP = Community Engagement and Planning; CI = confidence interval; MCS-12 = 12-item Mental Health Component Summary Score; OR = odds ratio; PHQ-9 = 9-item Patient Health Questionnaire; QOL = quality of life; RS = Resources for Services, or individual program technical assistance. Adjusted analyses used multiply imputed data, weighted for eligible sample for enrollment; linear regression models for continuous variables and logistic regression models for binary variables adjusted for baseline status of the dependent variable, community, age, education, race/ethnicity, and 12-month depressive disorder, and accounted for the design effect of the cluster randomization.
Six-month self-efficacy was assessed with 1 item: client’s ability to overcome depression (score ranged from 0 = not at all confident to 10 = extremely confident).
Column estimates show percentages and corresponding OR.
n = 137 at 6 months, n = 126 at 12 months.
Median cutpoint for baseline variable.
Intervention Effects in Service Utilization
Table 3 describes intervention effects on service utilization variables at 6- and 12-months follow-up for women. For service use outcomes, for CEP relative to RS, significant intervention effects were found at 6 months only for outpatient substance abuse (incidence rate ratio [IRR] = 3.21; 95% CI = 1.10, 9.34) and faith-based visits for depression (IRR = 2.65; 95% CI = 1.21, 5.82). We found no statistically significant differences between intervention groups for other service sectors or for 12-month follow-up.
TABLE 3—
Clients’ Service Utilization at 6-Month and 12-Month Follow-Up, by Intervention Status: Community Partners in Care, Women’s Substudy, Los Angeles, CA, 2010–2012
| Variable | RS Estimate, Mean or % (95% CI) | CEP Estimate, Mean or % (95% CI) | IRR or OR (95% CI) |
| 6-mo follow-up (n = 595) | |||
| No. hospital nights for alcohol, drugs, mental health | 0.6 (0.2, 1.6) | 1.3 (0.3, 5.2) | 1.93 (0.46, 8.17) |
| No. PC visits with depression service | 1.0 (0.7, 1.4) | 1.1 (0.8, 1.5) | 1.12 (0.75, 1.66) |
| No. MH outpatient visits | 9.9 (6.8, 14.5) | 9.1 (6.3, 13.0) | 0.92 (0.49, 1.71) |
| No. outpatient SA visits for depression | 1.3 (0.5, 3.4) | 4.3 (2.1, 8.6) | 3.21 (1.10, 9.34) |
| No. faith-based visits with depression service | 0.4 (0.2, 0.8) | 1.1 (0.6, 2.0) | 2.65 (1.21, 5.82) |
| Total outpatient contacts for depressiona | 21.6 (15.3, 30.3) | 23.7 (17.2, 32.5) | 1.10 (0.67, 1.79) |
| Any emergency department visits,c | 41.7 (34.8, 48.9) | 39.8 (33.8, 46.1) | 0.91 (0.61, 1.38) |
| ≥ 2 emergency department visitsb,c | 29.1 (22.5, 36.7) | 24.3 (18.7, 30.8) | 0.76 (0.47, 1.24) |
| 12-mo follow-up (n = 593) | |||
| No. hospital nights for alcohol, drugs, mental health | 0.3 (0.1, 0.6) | 0.5 (0.2, 1.2) | 1.71 (0.58, 5.02) |
| No. PC visits with depression service | 0.8 (0.6, 1.2) | 1.0 (0.5, 1.8) | 1.19 (0.57, 2.48) |
| No. MH outpatient visits | 6.8 (4.8, 9.7) | 5.5 (4.1, 7.4) | 0.81 (0.51, 1.28) |
| No. outpatient SA visits for depression | 1.6 (0.5, 4.8) | 2.7 (1.1, 6.3) | 1.70 (0.51, 5.71) |
| No. faith-based visits with depression service | 0.6 (0.2, 1.8) | 0.8 (0.4, 1.5) | 1.30 (0.28, 5.90) |
| Total outpatient contacts for depressiona | 20.1 (14.1, 28.7) | 18.6 (13.6, 25.3) | 0.92 (0.60, 1.43) |
| Any emergency department visits,c | 35.1 (29.9, 40.6) | 36.5 (30.3, 43.1) | 1.07 (0.75, 1.51) |
| ≥ 2 emergency department visitsb,c | 26.9 (21.8, 32.6) | 21.3 (17.4, 25.8) | 0.72 (0.51, 1.02) |
Note. CEP = Community Engagement and Planning; CI = confidence interval; IRR = incidence rate ratio; MH = mental health; OR = odds ratio; PC = primary care; RS = Resources for Services, or individual program technical assistance; SA = substance abuse. Adjusted analyses used multiply imputed data, weighted for eligible sample for enrollment; logistic regression models for binary variables (presented as odds ratios) or Poisson regression models for count variables (presented as incidence rate ratios) adjusted for baseline status of the dependent variable, community, age, education, race/ethnicity, and depressive disorder in the past 12 months, and accounted for the design effect of the cluster randomization.
Including emergency department visits for alcohol, drug, and mental health problems, mental health specialty visits with depression services from primary care provider, mental health outpatients, substance abuse, self-help, and social–community services.
Median cutpoint for baseline variable.
Column estimates show percentages and corresponding OR.
DISCUSSION
CPIC is one of the first studies to use a community-based participatory research approach to conduct a randomized study of alternative approaches to disseminate depression QI in underresourced communities,46 offering insight into strategies to support improved outcomes for depressed ethnic minority women. Our secondary analyses of intervention effects for women confirmed similar intervention effects found for the whole sample (improved mental health quality of life, reduction in homelessness risk factors at 6 months); it also confirmed additional enduring effects on functional and socioeconomic outcomes for women at 12 months relative to findings for the entire sample.16,17 Although CEP relative to RS did not improve depression symptoms, there were gains for women in mental health–related quality of life, mental wellness, physical activity, and in reductions in life stressors, financial difficulties, and missed work days. We also found significant intervention differences on several potential explanatory factors such as depression-related self-efficacy as well as logistical and structural barriers to care (e.g., being able to get an appointment, having someone speak your language at the clinic) by 12 months. These effects were not found at 6 months, suggesting that service system improvements may require time to translate into reduction in barriers to care and depression-related self-efficacy.
Consistent with findings for the overall sample, CEP relative to RS shifted depression care toward use of community settings, increasing visits for depression care to substance abuse, faith-based, and park settings by 6 months. The increase in substance abuse visits under CEP is noteworthy given that 30.5% of women had comorbid substance use. However, the benefits of shifting depression care to community-based settings may have been limited by the resource constraints to implement intensive evidence-based QI components, such as electronic outcome tracking systems and licensed care managers.47,48 Community sectors may have offered other alternatives through nonlicensed staff; therefore, it may be important to strengthen depression treatment access and individual-level support to providers to achieve a greater effect on depression outcomes.
This study has important limitations, including its focus on 2 Los Angeles communities; reliance on self-report measures, some of which are not empirically validated; lack of clinical diagnoses of depression; small sample size for subanalyses involving low-occurrence characteristics (e.g., lost work days, because of the small number of employed in our sample); and lack of a usual-care comparison group. In addition, the subanalyses were inherently exploratory in nature, useful for informing directions for future research.
Despite these limitations, our analyses suggest that, compared with more standard technical assistance, CEP was successful at implementing depression QI in low-resource minority settings; it also led to a broad range of improvements for women, such as resiliency, employment, less risk of homelessness, and other factors that could result in markedly better quality of life, services access, and social risk disparities. The benefits of CEP are particularly significant given the challenges of engaging the most vulnerable low-income women (i.e., ethnic minority women with average incomes of less than $10 000, homelessness risk, or more than 3 chronic conditions) into depression care and improving individual social risk factors associated with poor health outcomes. Activation of informal support systems, task shifting, and the sharing of depression care tasks between health care and community-based agencies may have created a “village” for depression care and provided an opportunity for women to get some depression-informed care in settings they already frequent. The improvements in individual social risk factors, such as reductions in homelessness, may have been the result of the improved capacity of social services agencies to engage depressed clients or to give more attention to their social concerns within and across health care sectors. The CPIC study results may be relevant to existing policy initiatives such as Medicaid Behavioral Health Homes and Accountable Care Communities, which incentivize health care and community agency partnerships to improve population-based health outcomes. In conclusion, the use of community-based, locally tailored, multisector service partnership strategies, such as those in CEP, can improve quality of life, services access, and social risk disparities for low-income ethnic minority women.
ACKNOWLEDGMENTS
Community Partners in Care was funded by the National Institute of Mental Health (awards R01MH078853, P30MH082760, and P30MH068639), the Robert Wood Johnson Foundation (64244), the California Community Foundation, the National Library of Medicine (award G08LM011058), and the NIH/UCLA Clinical Translational Science Institute (award UL1TR000124). The preparation of this article was supported by the National Institute of Minority Health and Health Disparities (R01MD007721) and in part by the Implementation Research Institute, George Warren Brown School of Social Work, Washington University, St. Louis, through an award from the National Institute of Mental Health (R25 MH080916-01A2) and the Department of Veterans Affairs, Health Services Research & Development Service, Quality Enhancement Research Initiative.
We thank the Los Angeles programs, providers, staff, and clients who participated and the RAND Survey Research Group and community members who conducted client data collection. We also thank Loretta Jones for her study leadership and vision, Esmeralda Pulido, Ana Ramos, Rosie Cardenas, and Liz Lizaola for project management support, Lily Zhang for statistical programming support, and Enola Proctor for feedback on implementation science methods. We also thank the 25 participating agencies of the CPIC Council and their representatives.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was received by RAND.
REFERENCES
- 1.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74(1):5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- 3.Patel V, Lund C, Hatherill S, Plagerson S, Corrigall J, Funk M. Social Determinants of Mental Disorders. Priority Public Health Conditions: From Learning to Action on Social Determinants of Health. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
- 4.McLeod JD, Kessler RC. Socioeconomic status differences in vulnerability to undesirable life events. J Health Soc Behav. 1990;31(2):162–172. [PubMed] [Google Scholar]
- 5.Alegria M, Canino G, Rios R et al. Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatr Serv. 2002;53(12):1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- 6.US Surgeon General releases report on mental health: culture, race, and ethnicity. Public Health Rep. 2001;116(4):376. [PMC free article] [PubMed] [Google Scholar]
- 7.Hu TW, Snowden LR, Jerrell JM, Nguyen TD. Ethnic populations in public mental health: services choice and level of use. Am J Public Health. 1991;81(11):1429–1434. doi: 10.2105/ajph.81.11.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chow JC, Jaffee K, Snowden L. Racial/ethnic disparities in the use of mental health services in poverty areas. Am J Public Health. 2003;93(5):792–797. doi: 10.2105/ajph.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ekers D, Murphy R, Archer J, Ebenezer C, Kemp D, Gilbody S. Nurse-delivered collaborative care for depression and long-term physical conditions: a systematic review and meta-analysis. J Affect Disord. 2013;149(1–3):14–22. doi: 10.1016/j.jad.2013.02.032. [DOI] [PubMed] [Google Scholar]
- 10.Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006;166(21):2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 11. Behavioral Health Homes for People With Mental Health and Substance Use Conditions: The Core Clinical Features. Washington, DC: SAMHSA–HRSA Center for Integrated Health Solutions; May 2012.
- 12.Hughes LS, Peltz A, Conway PH. State innovation model initiative: a state-led approach to accelerating health care system transformation. JAMA. 2015;313(13):1317–1318. doi: 10.1001/jama.2015.2017. [DOI] [PubMed] [Google Scholar]
- 13.Smedley BD, Syme SL. Promoting Health: Intervention Strategies From Social and Behavioral Research. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 14.Thomas SB, Quinn SC, Butler J, Fryer CS, Garza MA. Toward a fourth generation of disparities research to achieve health equity. Annu Rev Public Health. 2011;32:399–416. doi: 10.1146/annurev-publhealth-031210-101136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones L, Wells K. Strategies for academic and clinician engagement in community-participatory partnered research. JAMA. 2007;297(4):407–410. doi: 10.1001/jama.297.4.407. [DOI] [PubMed] [Google Scholar]
- 16.Wells KB, Jones L, Chung B et al. Community-partnered cluster-randomized comparative effectiveness trial of community engagement and planning or resources for services to address depression disparities. J Gen Intern Med. 2013;28(10):1268–1278. doi: 10.1007/s11606-013-2484-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chung B, Ong M, Ettner SL et al. 12-month outcomes of community engagement versus technical assistance to implement depression collaborative care: a partnered, cluster, randomized, comparative effectiveness trial. Ann Intern Med. 2014;161(10) suppl:S23–S34. doi: 10.7326/M13-3011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones L, Wells K, Norris K, Meade B, Koegel P. The vision, valley, and victory of community engagement. Ethn Dis. 2009;19(4) suppl 6:S6. [PMC free article] [PubMed] [Google Scholar]
- 19.Miranda J, Ong MK, Jones L et al. Community-partnered evaluation of depression services for clients of community-based agencies in under-resourced communities in Los Angeles. J Gen Intern Med. 2013;28(10):1279–1287. doi: 10.1007/s11606-013-2480-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stockdale SE, Tang L, Pudilo E et al. Sampling and recruiting community-based programs using community-partnered participation research. Health Promot Pract. 2016;17(2):254–264. doi: 10.1177/1524839915605059. [DOI] [PubMed] [Google Scholar]
- 21.Miranda J, Chung JY, Green BL et al. Treating depression in predominantly low-income young minority women: a randomized controlled trial. JAMA. 2003;290(1):57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- 22.Wells KB, Sherbourne C, Schoenbaum M et al. Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA. 2000;283(2):212–220. doi: 10.1001/jama.283.2.212. [DOI] [PubMed] [Google Scholar]
- 23.Muñoz RF, Miranda J. Group Therapy Manual for Cognitive Treatment of Depression. San Francisco, CA. San Francisco, CA: San Francisco General Hospital, University of California; 1993. [Google Scholar]
- 24.Muñoz RF, Miranda J, Aguilar-Gaxiola S. Individual Therapy Manual for Cognitive-Behavioral Treatment of Depression. Santa Monica, CA: Rand Corp; 2000. [Google Scholar]
- 25.Khodyakov D, Sharif MZ, Dixon EL et al. An implementation evaluation of the community engagement and planning intervention in the CPIC Depression Care Improvement Trial. Community Ment Health J. 2014;50(3):312–324. doi: 10.1007/s10597-012-9586-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chung B, Ngo VK, Ong MK et al. Participation in training for depression care quality improvement: a randomized trial of community engagement or technical support. Psychiatr Serv. 2015;66(8):831–839. doi: 10.1176/appi.ps.201400099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 28.Ware J, Jr, Kosinski M, Keller SDA. 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Sheehan DV, Lecrubier Y, Sheehan KH et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(suppl 20):22–33. quiz, 34–57. [PubMed] [Google Scholar]
- 30.Sheehan DV, Lecrubier Y, Sheehan KH et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry. 1997;12(5):232–241. [Google Scholar]
- 31.Lecrubier Y, Sheehan DV, Weiller E et al. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry. 1997;12(5):224–231. [Google Scholar]
- 32.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ware JEJ, Kosinski M, Turner-Bowker DM, Gandek B. User’s Manual for the SF-12v2® Health Survey: With a Supplement Documenting SF-12® Health Survey. Lincoln, RI: Quality Metric Inc; 2002. [Google Scholar]
- 34.Wong MD, Sarkisian CA, Davis C, Kinsler J, Cunningham WE. The association between life chaos, health care use, and health status among HIV-infected persons. J Gen Intern Med. 2007;22(9):1286–1291. doi: 10.1007/s11606-007-0265-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Apicello J. A paradigm shift in housing and homeless services: applying the population and high-risk framework to preventing homelessness. Open Health Serv Policy J. 2010;3:41–52. [Google Scholar]
- 36.Gundersen C, Weinreb L, Wehler C, Hosmer D. Homelessness and food insecurity. J Hous Econ. 2003;12(3):250–272. [Google Scholar]
- 37.Sherbourne CD, Edelen MO, Zhou A, Bird C, Duan N, Wells KB. How a therapy-based quality improvement intervention for depression affected life events and psychological well-being over time: a 9-year longitudinal analysis. Med Care. 2008;46(1):78–84. doi: 10.1097/MLR.0b013e318148478d. [DOI] [PubMed] [Google Scholar]
- 38.Wells KB, Tang L, Miranda J, Benjamin B, Duan N, Sherbourne CD. The effects of quality improvement for depression in primary care at nine years: results from a randomized, controlled group-level trial. Health Serv Res. 2008;43(6):1952–1974. doi: 10.1111/j.1475-6773.2008.00871.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ludman E, Katon W, Bush T et al. Behavioural factors associated with symptom outcomes in a primary care-based depression prevention intervention trial. Psychol Med. 2003;33(6):1061–1070. doi: 10.1017/s003329170300816x. [DOI] [PubMed] [Google Scholar]
- 40.Murray DM. Design and analysis of group-randomized trials. In: Kelsey JL, Marmot MG, Stolley PD, Vessey MP, editors. Monographs in Epidemiology and Biostatistics. New York, NY: Oxford University Press; 1998. pp. 77–176. [Google Scholar]
- 41.Groves RM, Dillman D, Eltinge JL, Little RJA. Survey Nonresponse. Hoboken, NJ: Wiley-Interscience; 2002. [Google Scholar]
- 42.Korn EL, Graubard BI. Analysis of health surveys. In: Groves RM, Kalton G, Rao JNK, Schwarz N, Skinner C, editors. Wiley Series in Probability and Statistics: Survey Methodology Section. New York, NY: Wiley; 1999. pp. 159–185. [Google Scholar]
- 43.Binder DA. On the variances of asymptotically normal estimators from complex surveys. Int Stat Rev. 1983;51(3):279–292. [Google Scholar]
- 44.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley & Sons; 1987. [Google Scholar]
- 45.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55(2):652–659. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- 46.Anderson LM, Adeney KL, Shinn C, Safranek S, Buckner-Brown J, Krause LK. Community coalition-driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database Syst Rev. 2015;6:CD009905. doi: 10.1002/14651858.CD009905.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Solberg LI, Crain AL, Jaeckels N et al. The DIAMOND initiative: implementing collaborative care for depression in 75 primary care clinics. Implement Sci. 2013;8:135. doi: 10.1186/1748-5908-8-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Whitebird RR, Solberg LI, Jaeckels NA et al. Effective Implementation of collaborative care for depression: what is needed? Am J Manag Care. 2014;20(9):699–707. [PMC free article] [PubMed] [Google Scholar]