Abstract
Research about relationships between place characteristics and racial/ethnic inequities in health has largely ignored conceptual advances about race and place within the discipline of geography.
Research has also almost exclusively quantified these relationships using effect estimates (e.g., odds ratios), statistics that fail to adequately capture the full impact of place characteristics on inequities and thus undermine our ability to translate research into action.
We draw on geography to further develop the concept of “racialized risk environments,” and we argue for the routine calculation of race/ethnicity-specific population-attributable risk percentages.
Despite the Healthy People 2000, 2010, and 2020 goals of attaining health equity, inequities persist between the health of non-Hispanic Black (“Black”) adults and adolescents and that of their non-Hispanic White (“White”) counterparts in the United States.1 Characteristics of the places where people live, work, and play shape these inequities.2–8 Unfortunately, conceptualizations of relationships between place characteristics and Black versus White health inequities have yet to fully engage with key conceptual advances in the discipline of geography.
Moreover, we persist in using effect estimates (e.g., odds ratios [ORs]) to quantify these relationships.These statistics ignore variations in exposure prevalence, a major weakness in studies of place and Black versus White health inequities. Black adults and adolescents in the United States often live in places that are radically different from where their White counterparts live and, thus, have markedly different exposures to place-based hazards and resources.4,7 We seek to catalyze research and interventions rooted in a deeper understanding of the central role that place plays in shaping Black versus White inequities. We achieve this goal by (1) drawing on core constructs from geography to further develop the construct “racialized risk environments,” which was first proposed in 20095; and (2) advocating the routine estimation of race/ethnicity-specific population-attributable risk percentages.
CONCEPTUALIZING RACIALIZED RISK ENVIRONMENTS
Several articles have conceptualized relationships between segregated neighborhoods and Black versus White inequities in health. Collins and Williams have deemed racial/ethnic residential segregation a fundamental determinant of health inequities.2–5,7,8 This work often frames race/ethnicity using critical race theory’s “racialized social systems.” In a racialized social system,
economic, political, social, and ideological [hierarchies] are partially structured by the placement of actors in racial categories. . . . [Whites tend] to receive greater economic remuneration and access to better occupations . . . , [occupy] a primary position in the political system, [and receive] higher social estimation.9(p37)
The racialized risk environments construct extends this past work on racialized social systems, health inequities, and place by integrating core concepts from geography and Rhodes’ risk environment model.10
Public health has extensively mined geographic methods (e.g., geocoding), measures (e.g., floating catchment areas), and software (e.g., ArcGIS) to analyze relationships of place to health and health inequities. We extend the generative engagement of public health with geography to include the latter’s conceptual contributions. Social geography, a subdiscipline of geography, posits that racialized social systems and space are mutually constituted.11–13 This proposition is part of Soja’s “sociospatial dialectic,” in which social relations give shape to space, and interactions in and with space profoundly shape our understanding of our social position.12,13
In the United States, Whites have long established and maintained supremacy by determining the construction and uses of space (the “racialization of space”), and understandings of race/ethnicity have, in turn, been rooted in experiences with these spaces (the “spatialization of race”).11,13 Perhaps the most well-known historical interpenetration of race/ethnicity and space is Jim Crow. Developed by Whites to help maintain supremacy after emancipation, Jim Crow laws allocated physically superior spaces and amenities to White people and physically inferior spaces and amenities to Black people. In turn, the racialized spaces created by Jim Crow informed contemporary meanings of race/ethnicity. Whiteness was constituted, daily, by freedom of movement, the power to control Black movement, and access to physically superior places. Likewise, daily experiences of constrained and surveilled mobility and relegation to physically inferior places constituted race/ethnicity for Black adults and children.
The possibility that Whites could maintain supremacy by racializing neighborhoods only emerged after 1916. This emergence is consistent with two key tenets of social geography: whereas the mutually constituted nature of race/ethnicity and space is constant, its specific manifestation (1) is historically contingent, evolving in response to resistance and other social conditions; and (2) can shift geographic scales.12 For centuries, urban space was undifferentiated; without strong transportation systems, people lived near where they worked, and neighborhoods were racially/ethnically integrated.
New York City ushered in a century of residential segregation in 1916 (not coincidentally, this occurred shortly after the city built its first subway), when it pioneered zoning ordinances that differentiated manufacturing districts from residential districts and created protected neighborhoods for affluent Whites.12,14 Catalyzed by the emergence of zoning and by increasing migrations of Black families to cities, Whites began crafting various strategies to racialize urban (and eventually metropolitan) neighborhoods in an effort to simultaneously exploit and contain Black labor.14,15 These strategies evolved over the past century in response to Black resistance and other dynamics, and they have included restrictive covenants and government-supported redlining, urban renewal, public housing, and gentrification policies.12,16
These strategies have successfully racialized neighborhoods. Metropolitan areas were highly segregated by 1940.15 In 2010 the average White resident of a metro area lived in a census tract where three quarters of other residents were also White, 8% were Black, and 11% were Latino.16 The average Black resident lived in a tract where about half of the other residents were also Black, one third were White, and 15% were Latino.16
As with Jim Crow, the racialization of residential neighborhoods has been highly effective at maintaining racialized social systems. Social, economic, physical, and political resources are disproportionately allocated to predominately White neighborhoods, whereas predominately Black neighborhoods are disproportionately burdened with hazards.2–5,7,15,17 To illustrate, whereas just 5% of White children lived in a high-poverty census tract in 2009 to 2013, 32% of Black children lived in high-poverty tracts.18 A multisite study found that 31% of White households were located in a census tract with one or more supermarkets, compared with just 8% of Black households.19 Predominately Black and poor neighborhoods are stigmatized as “ghettoes,” whereas predominately White neighborhoods are marketed as havens, regardless of resident class.17 Notably, though, predominately Black neighborhoods can also serve as important loci of “congregation,” nurturing Black cultures, resistance, and power.
Social geography also posits that legacies of past efforts to racialize places have shaped current physical landscapes. For example, a highway built during urban renewal that isolated a predominately Black neighborhood will continue to bound the neighborhood after it gentrifies. The meaning of that boundedness, however, may evolve from isolation to exclusivity. These legacies also shape current spatializations of race/ethnicity. Neighborhood loss, for example, may characterize experiences of race/ethnicity for Black families whose members have been serially displaced for generations by urban renewal, public housing, and gentrification policies. By contrast, neighborhood permanence, secured by establishing historic districts and other strategies, may characterize race/ethnicity for White families.
We integrate these elements of social geography with Rhodes’ risk environment model to further develop the racialized risk environments construct. Rhodes’ risk environment model posits that the “risk environment” is the “space . . . [where] factors exogenous to the individual interact to increase the chances of HIV transmission.”10(p1026) In Rhodes’ conceptualization, risk environments have four domains of influence: social, economic, political, and physical.10 These domains can exist at multiple scales and may interact with one another across and within scales to affect HIV.10 Rhodes’ risk environment model posits that social, economic, political, and physical characteristics of places can affect health indirectly, as when they shape networks or norms, or directly, as when they affect immune function.10
The racialized risk environments construct diverges from Rhodes’ risk environment model in that its primary exposures are systematically racialized places and its outcomes are inequities in any health status. A core tenet is that the racialization of space is a primary determinant of Black versus White inequities in health because it is central to the creation and experience of racial/ethnic inequality itself. Presently, White supremacy is maintained, in part, by creating racialized neighborhoods that are both separate and unequal. To the extent that social, economic, political, and physical characteristics of places affect health, racialized risk environments create and perpetuate health inequities, both indirectly and directly.
Social geography teaches us that the strategies that Whites use to configure space to maintain supremacy are historically contingent, often evolving in response to Black resistance. Thus, a focus on racialized risk environments asks us to scan the horizon for emerging configurations of racialized space and consider their implications for equity and to recognize that Black resistance can precipitate these new configurations and buffer their effects. Past racializations of space can influence current health through physical and emotional legacies. The racialized risk environment construct also suggests that diverse spatial scales can be racialized (e.g., activity spaces, metropolitan areas) and that social, economic, political, and physical characteristics of places can interact both across and within scales to affect health inequities.
EFFECT ESTIMATES AND RISK ENVIRONMENTS
Unfortunately, commonly used statistical tools have impeded our ability to understand and intervene in racialized risk environments’ impacts on health inequities. Almost universally, ORs and other effect estimates (e.g., relative risks, hazard ratios [HRs]) are the single metric used to quantify exposure–outcome relationships in analyses of place and health inequities. Relying exclusively on effect estimates creates significant limitations:
(1) Effect estimates provide a dangerously incomplete picture of the impacts of place characteristics on Black versus White inequities in health because they ignore variations in exposure prevalence. These statistics simply quantify the magnitude and direction of change in the outcome variable when values of the exposure variable rise or fall.20 The true public health impact of an exposure, however, is determined by the magnitude of its effect on the outcome in combination with the prevalence of that exposure in the population.21
In a racialized risk environment, these variations in exposure prevalence are crucial determinants of inequities. Investigators routinely test the hypothesis that the relationship between place and health varies by individual race/ethnicity. In the absence of effect modification, the conclusion may be that the exposure’s effect on the outcome is uniform across racial/ethnic groups. In a context of racialized risk environments, however, this conclusion may be incorrect. Even in the absence of effect modification by individual race/ethnicity, a place-based hazard may be responsible for a higher proportion of cases among Black individuals because they experience higher prevalences of the exposure. Likewise, a place-based resource may prevent a higher proportion of cases among Whites because of the systematically higher prevalence of exposure to place-based resources among Whites.
(2) Exclusively relying on effect estimates undermines our capacity to use research to achieve health equity. Intervention priorities and targets may vary across racial/ethnic groups in ways that effect estimates cannot capture because these statistics ignore the racialization of place-based exposures. Several entities have called for place-based interventions to achieve equity,22–24 but our current dependence on effect estimates prevents us from generating findings that can guide the development, prioritization, or targeting of these interventions.
POPULATION-ATTRIBUTABLE RISK PERCENTAGES
We recommend routinely calculating race/ethnicity-specific population-attributable risk percentages (PAR%s) in studies of place and health inequities because they can more comprehensively capture the effects of racialized risk environments. PAR%s estimate the percentage of cases in a population that is attributable to the exposure.20,21 PAR%s integrate information about the effect estimate’s magnitude with information about the population prevalence of the exposure. In a cohort study, the PAR% can be calculated as
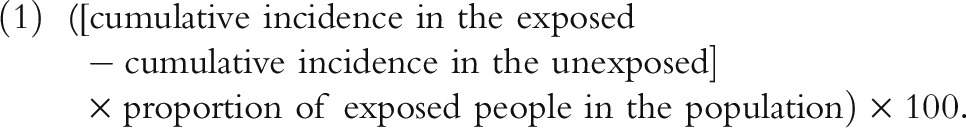 |
A race/ethnicity-specific PAR% is one in which both the effect estimate and the exposure prevalence are calculated for a single racial/ethnic group; confidence intervals can be calculated to determine if PAR%s truly differ across groups (equations are available as a supplement to the online version of this article at http://www.ajph.org). Because of our conceptualization of racialized risk environments, it is significant that race/ethnicity-specific PAR%s (like all PAR%s) can capture time-varying, historical, lagged, and interacting exposures—if variables and models are constructed appropriately.
Our previous work exemplifies the power of race/ethnicity-specific PAR%s. In an analysis of Black women and White women diagnosed with breast cancer who lived in 15 Georgia metropolitan areas, we found that women living in census tracts with “relatively high” percentages of Black residents had higher rates of mortality over time (HR = 1.30).6 Although the HR’s magnitude did not vary across racial/ethnic groups, Black women were much more likely to live in tracts with high percentages of other Black residents (82% of Black women vs 22% of White women).6 Consequently, race/ethnicity-specific PAR%s indicate that the exposure accounted for 19% of the excess mortality among Black women but just 5% of excess mortality among White women.6 The race/ethnicity-specific PAR% revealed the vital story of the consequences of this tract-level exposure, a story that reporting effect estimates alone would have obscured.
Race/ethnicity-specific PAR%s are vital tools for prioritizing intervention targets because they can identify the set of place-based exposures driving inequities in health. If investigators studying place and health inequities routinely calculated race/ethnicity-specific PAR%s, policymakers, community-based organizations, and others could rank the set of place-based exposures relevant to a specific outcome by the percentage of the outcome attributable to each and develop interventions accordingly. Alternatively, they might identify the set of place-based exposures with the highest race/ethnicity-specific PAR%s across several key equity outcomes and design and implement interventions addressing these exposures.
CALCULATION CHALLENGES
Challenges to calculating race/ethnicity-specific PAR%s for place and health inequities research are similar to those for calculating PAR%s for studies of place and health more broadly. PAR%s assume that a causal relationship has been established between the exposure and the outcome.20 Many studies of place, health, and health equity cannot yet make this claim. Longitudinal designs are central to establishing causality. However, longitudinal studies of place and health remain relatively rare, perhaps because it is expensive to gather time-varying data about characteristics of both places and people.
PAR%s also require that samples reflect the underlying population. Studies of inequities in some populations of great interest to public health may not use probability-based methods to generate samples because they lack a sampling frame (e.g., HIV among men who have sex with men). We encourage investigators to generate race/ethnicity-specific PAR%s and critically assess the extent to which PAR% assumptions were met. This strategy of critical transparency is common in other areas of research that routinely violate statistical assumptions (e.g., studies of people who use drugs that calculate P values when samples likely fail to represent the underlying population).
Additionally, PAR% calculations assume that effect estimates were generated in correctly specified statistical models. Effect estimates for relationships of place characteristics to health and health inequities can be artificially low. Place characteristics can influence health inequities through multiple, complex pathways, some of which might have countervailing effects. Also, investigators may unwittingly control for individual-level characteristics that lie in the causal pathway between place and health, thus suppressing effect estimates for the place-based exposures. Directed acyclic graphs can help isolate specific pathways and identify variables that should and should not be included as “controls.”25
CONCLUSIONS
Risk environments are profoundly racialized. Almost all articles quantifying relationships of place characteristics to inequities have exclusively reported effect estimates. Because they ignore exposure prevalence—and thus the racialization of risk environments—effect estimates misrepresent the impact of place on health inequities and undermine our ability to prioritize intervention targets. Routinely calculating race/ethnicity-specific PAR%s, and critically reflecting on violations of assumptions, will allow us to more accurately and comprehensively quantify the implications of place for inequities and identify the highest impact targets for interventions.
ACKNOWLEDGMENTS
This research was supported by the National Institutes of Health (grant “Place Characteristics & Inequities in HIV in IDUS: A Multilevel Analysis of NHBS,” DA035101 to H. L. F. C., principal investigator) and the Emory Center for AIDS Research (grant P30 AI050409).
We want to thank the three reviewers of this article and the editor-in-chief for their insightful comments.
REFERENCES
- 1.Office of Disease Prevention and Health Promotion. Healthy People 2020. Washington, DC: US Department of Health and Human Services; 2012. [Google Scholar]
- 2.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.LaVeist T, Pollack K, Thorpe R, Jr, Fesahazion R, Gaskin D. Place, not race: disparities dissipate in southwest Baltimore when Blacks and Whites live under similar conditions. Health Aff (Milwood) 2011;30(10):1880–1887. doi: 10.1377/hlthaff.2011.0640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper HL, Linton S, Kelley ME et al. Racialized risk environments in a large sample of people who inject drugs in the United States. Int J Drug Policy. 2016;27:43–55. doi: 10.1016/j.drugpo.2015.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper HL, Bossak BH, Tempalski B, Friedman SR, Des Jarlais DC. Temporal trends in spatial access to pharmacies that sell over-the-counter syringes in New York City health districts: relationship to local racial/ethnic composition and need. J Urban Health. 2009;86(6):929–945. doi: 10.1007/s11524-009-9399-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Russell E, Kramer MR, Cooper HL, Thompson WW, Arriola KR. Residential racial composition, spatial access to care, and breast cancer mortality among women in Georgia. J Urban Health. 2011;88(6):1117–1129. doi: 10.1007/s11524-011-9612-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Osypuk TL, Acevedo-Garcia D. Beyond individual neighborhoods: a geography of opportunity perspective for understanding racial/ethnic health disparities. Health Place. 2010;16(6):1113–1123. doi: 10.1016/j.healthplace.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Acevedo-Garcia D, Osypuk TL, McArdle N, Williams DR. Toward a policy-relevant analysis of geographic and racial/ethnic disparities in child health. Health Aff (Milwood) 2008;27(2):321–333. doi: 10.1377/hlthaff.27.2.321. [DOI] [PubMed] [Google Scholar]
- 9.Bonilla-Silva E. White Supremacy and Racism in the Post-Civil Rights Era. Boulder, CO: Lynne Rienner; 2001. [Google Scholar]
- 10.Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61(5):1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 11.Delaney D. The space that race makes. Prof Geogr. 2002;54(1):6–14. [Google Scholar]
- 12.Knox P, Pinch S. Urban Social Geography: An Introduction. New York, NY: Routledge; 2014. [Google Scholar]
- 13.Cooper H, Moore L, Gruskin S, Krieger N. Characterizing perceived police violence: implications for public health. Am J Public Health. 2004;94(7):1109–1118. doi: 10.2105/ajph.94.7.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hankins KB, Cochran R, Derickson KD. Making space, making race: reconstituting White privilege in Buckhead, Atlanta. Soc Cult Geogr. 2012;13(4):379–397. [Google Scholar]
- 15.Massey D, Denton N. American Apartheid: Segregation and the Making of the Underclass. Cambridge, MA: Harvard University Press; 1993. [Google Scholar]
- 16.Logan JR, Stults B. The Persistence of Segregation in the Metropolis: New Findings from the 2010 Census. Providence, RI: Brown University; 2011. [Google Scholar]
- 17.Keene DE, Padilla MB. Race, class and the stigma of place: moving to “opportunity” in Eastern Iowa. Health Place. 2010;16(6):1216–1223. doi: 10.1016/j.healthplace.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kids Count Data Center. Baltimore, MD: Annie E. Casey Foundation; 2015. [Google Scholar]
- 19.Morland K, Wing S, Roux AD. The contextual effect of the local food environment on residents’ diets: the atherosclerosis risk in communities study. Am J Public Health. 2002;92(11):1761–1767. doi: 10.2105/ajph.92.11.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hennekens CH, Buring JE. Epidemiology in Medicine. Boston, MA: Little, Brown; 1987. [Google Scholar]
- 21.Northridge ME. Public health methods—attributable risk as a link between causality and public health action. Am J Public Health. 1995;85(9):1202–1204. doi: 10.2105/ajph.85.9.1202. [Comment in The value of the population attributable risk percentage. Am J Public Health. 1996; Quantifying the expected vs potential impact of a risk-factor intervention program. Am J Public Health. 1997] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White House Office of National AIDS Policy. National HIV/AIDS Strategy. Washington, DC: 2010. [Google Scholar]
- 23.Centers for Disease Control and Prevention. A Practitioner’s Guide for Advancing Health Equity: Community Strategies for Preventing Chronic Disease. Atlanta, GA: US Department of Health and Human Services; 2013. [Google Scholar]
- 24.Smedley B, Amaro H. Advancing the science and practice of place-based intervention. Am J Public Health. 2016;106(2):197. [Google Scholar]
- 25.Fleischer NL, Diez Roux AV. Using directed acyclic graphs to guide analyses of neighbourhood health effects: an introduction. J Epidemiol Community Health. 2008;62(9):842–846. doi: 10.1136/jech.2007.067371. [DOI] [PubMed] [Google Scholar]


