Abstract
Research has consistently shown that alcohol use is a problem in rural communities and access to substance abuse treatment, particularly evidence-based treatment is limited. Because telemedicine has been shown to be effective in delivering services, this article presents a novel and innovative way of using telemedicine technology in the form of videoconferencing to deliver an evidence-based alcohol intervention (motivational enhancement therapy) with at-risk alcohol users in real-world settings (rural probation and parole offices). This article focuses on: (a) creating a profile of an at-risk group of rural alcohol users; (b) describing the evidence-based intervention; and (c) describing the innovative telemedicine-based service delivery approach.
Keywords: videoconferencing, real-world setting, alcohol use, rural offenders, treatment need
Research has consistently shown that alcohol use is a problem in rural communities (Helzer, Burnam, & McEvoy, 1991; McAuliffe, LaBrie, Woodworth, Zhang, & Dunn, 2003; Van Gundy, 2006). One national study found that heavy drinking among rural residents increased significantly over urban areas between 1995 and 2003 (Jackson, Doescher, & Hart, 2006). Rural drinkers are more likely than urban drinkers to meet criteria for an alcohol use disorder, as defined by the Diagnostic and Statistical Manual of Mental Disorders-IV (Booth, Kirchner, Fortney, Ross, & Rost, 2000). In fact, rural participants were more likely to have a current alcohol use disorder and regularly exceed recommended weekly limits of alcohol use compared to both urban and suburban participants (Borders & Booth, 2007). The prevalence of alcohol problems in rural areas has been acknowledged by treatment providers. In particular, one study found that a significantly higher percentage of health care and social service providers in rural areas reported clients on their caseloads with alcohol use problems compared to urban providers (Brems, Johnson, Warner, & Roberts, 2007).
A primary correlate of the problem of alcohol use in rural areas is the limited access to and availability of health and behavioral services (Booth & Curran, 2006). Limited access to services in rural areas is characterized by transportation difficulties, long travel distances to existing services, and service costs (Brems, Johnson, Warner, & Roberts, 2006). Rural problem drinkers believe that there are fewer services available for alcohol use than urban drinkers (Fortney & Booth, 2001), and those who seek services typically have to travel to larger cities, which can be a barrier (Fortney, Booth, Blow, & Bunn, 1995). Rural drinkers have been shown to have increased barriers to service access, including affordability, availability, and acceptability compared to urban drinkers, although there were only moderate differences in these measures predicting actual service utilization (Booth et al., 2000). One study also suggested that the barriers to service access may vary by rurality, with clients in more remote areas facing greater challenges than clients in small rural areas that are closer to metropolitan areas (Brems et al., 2006). In addition to the service access barriers, rural alcohol users are also likely to perceive negative community stigma associated with entering treatment (Brems et al., 2006; Fortney et al., 2004).
One at-risk group affected by alcohol use and limited services in rural areas is offenders on community supervision. Community supervision is defined as being on “parole” (returning to the community from prison) or “probation” (being monitored by an officer in the community rather than serving time in a jail or prison). Rates of alcohol abuse and dependence have been estimated at 4.7% and 3.8% among the general population (Grant et al., 2004), but are considerably higher among the offender population. Specifically, offender reports of alcohol abuse and dependence have ranged from 18%–30%, with variation attributed to sampling method and custody status of offenders (Fazel, Bains, & Doll, 2006). In addition to the prevalence rates of abuse and dependence, a number of offenders report hazardous drinking patterns that led to adverse consequences (Conklin, Lincoln, & Tuthill, 2000; Greenfeld, 1998), including alcohol use prior to the offense that led to their current incarceration (Jones & Hoffman, 2006; Mumola, 1999; Visher, LaVigne, & Travis, 2004). Martin, Bryant, and Fitzgerald (2001) examined the association between alcohol use and crime, in a sample of arrestees using Arrestee Drug Abuse Monitoring (ADAM) data and found that 54% of men and 43% of women reported using alcohol during the 72 hours prior to arrest. In addition, Zhang (2003) reported that 29% of male and 24% of female arrestees in the arrestee dataset reported problem drinking behavior prior to arrest that placed them at risk for alcohol dependence. Study data from Kentucky on rural probationers found that alcohol was the most common substance reported in the past 30 days (Oser et al., 2006), and nearly half had a history of an arrest for driving under the influence (DUI; Webster et al., 2009).
In the absence of accessible and effective treatment opportunities that target alcohol abstinence, offenders with a history of hazardous drinking patterns are at increased risk for subsequent relapse and recidivism. Studies reporting that offenders with a history of hazardous drinking are more likely to violate parole, compared to nonalcohol abusers, date back to the 1960s (Guze & Cantwell, 1965). This increased risk is due in part to the fact that alcohol use is a parole or a probation violation. Also, significant risk exists for the offender as well in that continued alcohol consumption adversely affects health (e.g., Brumback, Cao, & King, 2007; Durazzo et al., 2007; Prat, Adan, Pérez-Pàmies, & Sànches-Turet, 2008) and leads to social consequences (e.g., Miller, Cohen, & Wiersema, 1996; Widom, White, Czaja, & Marmorstein, 2007). Thus, there is a critical need for establishing community alcohol interventions for offenders with a history of hazardous drinking, particularly in communities where alcohol treatment is limited.
One of the National Institutes of Health research priorities is to increase access to care for individuals in need of alcohol services, with particular attention on services that may be delivered in nontraditional, real-world settings that are easily accessible for hazardous drinkers (National Institute on Alcohol Abuse and Alcoholism, 2008). Telemedicine technology is one approach that has been used more frequently to increase access to care for rural individuals (Bashshur, Reardon, & Shannon, 2000; Myers, Swan-Kriemeier, Wonderlich, Lancaster, & Mitchell, 2004; Shore, Brooks, Savin, Manson, & Libby, 2007; Shore & Manson, 2005). Telemedicine services have been acknowledged for time and cost savings both to patients, who do not have to invest the time and the money to travel long distances, and to institutions, which do not have funds to cover travel costs for providers (Hartley, Britain, & Sulzbacher, 2002; Shore et al., 2007). Videoconferencing, as a form of telemedicine, permits patients and therapists to see and hear each other through video cameras and television monitors (Miller, 1995; Tschirch, Walker, & Calvacca, 2006).
While commonly used for health care services, telemedicine has emerged in recent years as an approach for behavioral health services, with promising outcomes. Although much of the telemedicine literature is focused on psychiatric counseling, it has also been used to deliver manualized evidence-based practices (Bakke, Mitchell, Wonderlich, & Erickson, 2001; Nelson, Barnard, & Cain, 2003). Research on telemedicine videoconferencing indicates greater treatment adherence and medication compliance compared to nontreated controls in a sample of individuals with mental illness (D’Souza, 2002). Telemedicine videoconferencing has also demonstrated benefits for people in the criminal justice system, specifically individuals with substance use and mental health issues, by providing a way to monitor inmates’ psychotropic medications and by reducing the need for inmate transport to distant clinics (Manfredi, Shupe, & Batki, 2005). Studies have also examined the clinical efficacy of telemedicine compared to same room face-to-face sessions with no differences reported in treatment outcomes (Zaylor, 1999; Nelson et al., 2003). These studies suggest that telemedicine, when delivered using videoconferencing, is a feasible and viable method of behavioral health service delivery. However, studies on technology-driven interventions in real-world settings (outside traditional clinical or therapeutic environments) are limited.
In summary, this literature suggests that alcohol use is a problem in rural communities, that offenders who engage in hazardous alcohol use may be at increased risk for relapse and recidivism, that the existing treatment structure in rural communities is limited in addressing the needs of this at-risk population, and that telemedicine has been shown to be effective in delivering services. This article describes a new and innovative program designed to use telemedicine technology to deliver an evidence-based alcohol intervention (motivational enhancement therapy [MET]) with a sample of at-risk rural offenders in real-world settings (rural probation and parole offices). The purposes of this study are: (a) to create a profile of an at-risk group of rural alcohol users; (b) to describe the evidence-based intervention; and (c) to describe an innovative telemedicine-based service delivery approach.
Profile of Rural Alcohol Users
Participants in this study were 75 rural alcohol users on community supervision (probation or parole) who entered a study focused on the delivery of MET via videoconferencing technology in rural probation and parole offices. Participants were recruited from the probation and parole offices of three rural Kentucky districts. Eligibility criteria included (a) a history of at least hazardous use of alcohol, as indicated by an Alcohol Use Disorders Identification Test (AUDIT) Babor et al. (2001), score of 8 or higher, (b) willingness to enroll in alcohol services, (c) referral to the social service clinician (SSC), a trained substance abuse professional employed to assess probationers or parolees and to refer for the appropriate level of treatment, (d) self-report of alcohol as a primary substance of choice, (e) self-reported active drinking during the past year before incarceration, and (f) willingness to attend telemedicine sessions if randomized. Exclusion criteria included indications of cognitive impairment, psychosis, and evidence of physical withdrawal from a recent episode of alcohol use. There was no minimal amount of time participants were required to be out of custody to be considered eligible for the study.
As seen in Table 1, participants were mostly male, mostly White (one participant was African American), and they had an average age of 32.1 years. The majority of participants in the study were reentering the community from prison and were considered to be on parole status in the community. More than half of them reported working full-time during the year before incarceration, with an average of about 35 days working during the 3 months before incarceration.
Table 1.
Profile of the Target Group20
| Variable | M or % | SD | Range |
|---|---|---|---|
| Demographics | |||
| Community supervision status: parole | 93.3% | — | — |
| Race: White | 97.4% | — | — |
| Average age of participants | 32.1 | 9.2 | 19–57 |
| Sex: male | 90.8% | — | — |
| Alcohol Use | |||
| Average AUDIT score | 23.9 | 8.7 | 8–40 |
| Average number of days of alcohol use in 3 months before incarceration | 48.8 | 35.5 | 1–90 |
| Average number of drinks per day in 3 months before incarceration | 15.3 | 10.5 | 2–48 |
| Average number of days a week drinking to intoxication in 3 months before incarceration | 3.7 | 2.6 | 0–7 |
| Average number of years of regular use | 8.2 | 8.4 | 0–34 |
| Alcohol Treatment | |||
| Percent of participants treated for alcohol abuse in their lifetime | 33.3% | — | — |
| Average number of times participants treated for alcohol abuse | 0.6 | 1.1 | 0–6 |
| Other Substance Use (other than alcohol) | |||
| Percent reporting any drug use in 3 months before incarceration | 80.0% | — | — |
| Average number of days of drug use in 3 months before incarceration | 70.1 | 33.1 | 0–90 |
| Criminal History | |||
| Mean number of lifetime convictions | 15.0 | 14.4 | 1–75 |
| Average number of lifetime months spent incarcerated | 31.7 | 46.6 | 0–225 |
| Average number of months of most recent incarceration | 21.3 | 18.4 | 1–90 |
| Percent of participants under the influence of alcohol when committing crime that lead to last incarceration | 64.0% | — | — |
Note. AUDIT = Alcohol Use Disorders Identification Test.
Alcohol use was measured using the Drug/Alcohol Use subscale of the Addiction Severity Index (McLellan et al., 1992) and was based on self-report before incarceration. Rural offenders on community supervision reported an average of 48.8 days of alcohol use in the 3 months prior to incarceration—meaning that they consumed alcohol on 54% of the available drinking days during that time. By comparison, the average number of drinking days per month for a group of DUI offenders was 7.5 (25.0% of the available drinking days) (Nochajski & Stasiewicz, 2005). The sample of rural offenders in this study reported an average of 15.3 drinks per day. The same group of DUI offenders noted above reported a mean of 1.2 drinks per day (Nochajski & Stasiewicz, 2005), suggesting that the frequency and intensity of use among rural offenders in this sample is considerably higher than another notable at-risk group—which is also consistent with the self-reported average number of 3.7 days per week of drinking to intoxication, and an average number of 8.2 years of regular alcohol use.
The AUDIT score was served as an additional indicator of treatment need (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001). The AUDIT has been shown to detect between 75% and 90% of hazardous drinkers in different settings (Gordon et al., 2001; Moore, Beck, Babor, Hays, & Reuben, 2002; Saunders & Lee, 2000) and with diverse populations (De Silva, Jayawardana, & Pathmeswaran, 2008; Reinert & Allen, 2007). The average AUDIT score among rural offenders on community supervision in this study was 23.9. This AUDIT score is considerably higher than the mean score for rural and urban DUI offenders in Kentucky referred for assessment (7.4; Webster, Dickson, Duvall, & Clark, 2010) and for offenders convicted of multiple DUIs (14.5; Conley, 2001). In fact, the average AUDIT score in this study is consistent with other studies of individuals identified as alcohol-dependent entering outpatient treatment (Connor et al., 2008; Donovan, Kivlahan, Doyle, Longabaugh, & Greenfield, 2006) and psychiatric inpatient treatment (Bácskai, Czobor, & Gerevich, 2008).
Despite these rates of alcohol use, only about one third of study participants reported ever receiving alcohol treatment. Of those, more than half reported only being in treatment once. In addition, most participants also reported not using self-help groups such as Alcoholics Anonymous in the 3 months prior to their arrest. Also, more than one third of the sample indicated that they did not think they needed alcohol treatment. Although these findings are surprising in light of the extensive alcohol use among these rural offenders, studies have shown individuals at risk for or currently experiencing hazardous drinking patterns or alcohol use disorders typically do not seek formal treatment (Fleming & Manwell, 1999; National Institute on Alcohol Abuse and Alcoholism, 2008), despite research that indicates that alcohol treatment is associated with positive outcomes (e.g., Weisner, Matzger, & Kaskutas, 2003). In the absence of accessible and effective treatment opportunities that target alcohol abstinence, rural offenders with a history of hazardous drinking are clearly at increased risk for relapse and recidivism in the community.
This risk is exacerbated by the finding that the majority of these individuals also used illicit substances during the time just before incarceration (see Table 1), and they used illicit drugs with significant frequency (an average of 70 out of 90 days). Specifically, about two thirds reported illicit use of prescription opiates including Lortab (acetaminophen and hydrocodone), Percodan (aspirin and oxycodone), and Oxycontin (oxycodone). Half of the sample reported illicit use of prescription sedatives and tranquilizers as well as and marijuana. This rate of prescription opiate misuse is increasingly common in the Appalachia area targeted for this project, and more common than other types of illicit substances of abuse such as crack or powder cocaine. However, the majority of participants were polysubstance users, with 87% reporting use of more than one substance in the same day (including alcohol).
As shown in Table 1, nearly three quarters of participants had a lifetime criminal history of charges for driving while intoxicated and disorderly conduct or public intoxication, while two thirds had a history of drug possession or trafficking. They reported an average of 15 lifetime convictions, and their most recent incarceration was for nearly two years (an average of 21.3 months). About two thirds reported that the crime that led to their most recent incarceration was committed while under the influence of alcohol.
Description of Evidence-Based Intervention
Evidence-based, structured, therapist-guided approaches that enhance motivation for and commitment to change have been used successfully with offenders with a history of hazardous drinking. One such approach—MET—was initially developed for use in the National Institute on Alcohol Abuse and Alcoholism’s multisite trial Project MATCH (Miller, Zweben, DiClemente, & Rychtarik, 1992) and has been recognized as an evidence-based intervention for alcohol users (DiClemente, Bellino, & Neavins, 1999; Fuller & Hiller-Strumhofel, 1999). MET was also recognized by Fletcher and Chandler (2006) in the National Institute on Drug Abuse’s publication Principles of Drug Abuse Treatment for Criminal Justice Populations as an evidenced-based practice for substance users involved in the criminal justice system. MET is a manualized therapeutic approach grounded in key principles of motivational interviewing, with the overall goal of motivating a client to draw on his or her own internal resources for change (Miller, 1995; Sinha, Easton, Renee-Aubin, & Carroll, 2003). Therapists aid the participant in achieving change and creating an environment in which self-efficacy, rather than resistance and argumentation, is supported (Carroll et al., 2006; Sinha et al., 2003).
Studies have consistently shown reductions in alcohol use following MET participation (Adamson & Sellman, 2008; Brown & Miller, 1993; Donovan, Kadden, DiClemente, & Carroll, 2002; Miller, Benefield, & Tonigan, 1993; Project MATCH Research Group, 1997; Sellman, Sullivan, Dore, Adamson, & MacEwan, 2001; Thevos, Thomas, & Randall, 2001), including reduction in alcohol consumption among rural hazardous drinkers seeking treatment in community health clinics (Beckham, 2007). In addition to changes in alcohol use, motivational counseling (the basis of MET) has also shown promise as a tool to engage clients in alcohol services (Saitz et al., 2007). MET is currently being tested in a number of National Institutes of Health Clinical Trials Network (CTN) protocols, including one study testing the therapeutic usefulness of incorporating MET to improve treatment engagement, retention, and outcome (Carroll et al., 2002). Therefore, MET was used in this study based on the literature to support its effectiveness in reducing the frequency and intensity of alcohol use in a number of different samples. In addition, the brevity of the intervention and the suggested timeframe (4 sessions over 12 weeks) corresponds with the risky timeframe of 3 months postrelease for reentering offenders. In this study, MET was delivered to rural offenders in the enhanced treatment condition using telemedicine videoconferencing linkages to confidential settings adjacent to their local parole offices.
Training for MET study therapists consisted of a 1-day overview of the MET study manual with the study clinical supervisor who was a trained clinical expert in motivational interviewing and MET practices. All study therapists had to have a minimum bachelor’s degree in psychology or social work with related clinical experience, and most had a master’s degree. Training also consisted of role plays, videos of motivational interviewing and MET vignettes and case examples, and practice exercises. Each of the clinical sessions was videotaped (with permission of participants) and watched with the clinical supervisor to provide ongoing supervision on fidelity to the MET intervention and motivational interviewing principles. Each taped session was also separately coded by a trained research assistant using the Behavior Change Counseling Index, Criminal Justice Version (Walters, 2002) to monitor core components of motivational interviewing (i.e., the therapist used reflective listening statements) in order to ensure fidelity with the intervention.
Description of Telemedicine-Based Delivery Approach
In the current study, potential participants were identified after their initial visit with their probation or parole officer if they received a referral for a substance abuse assessment by the SSC. Kentucky is unique in that it places SSCs in each state probation and parole district to conduct substance abuse assessments and referrals to treatment for offenders on community supervision. Using a standardized recruiting script, the research coordinator met with each potential participant immediately after the SSC meeting to invite that person to participate in the study. Recruitment flyers were also placed in the probation and parole offices. Once the individual showed interest in participating, each was asked to complete a face-to-face screening session with the research coordinator within 3 days. The research coordinator met with potential participants in a private room to complete an eligibility screening session, which lasted about 20 minutes. Informed consent was obtained during this session. Information about all participants was kept confidential, and officers were not notified who participated in the study. A federal certificate of confidentiality was also obtained, to protect participants’ information.
Of those screened for study inclusion, 75 eligible participants completed a baseline interview within one week. With institutional review board and Kentucky Department of Corrections approval, all participants were paid $20 for completing a face-to-face baseline interview in a private, confidential setting in the parole office. The baseline interview focused on alcohol use, alcohol treatment history and barriers, other drug use, criminal justice involvement, and related issues. Participants were then randomized using a computerized program (http://www.randomizer.org) into one of two groups: MET via telemedicine in combination with services as usual or services as usual.
If randomized to services as usual, study participants in this group received the “usual” referral for services by the SSC but did not receive the MET telemedicine intervention. The SSC provided transitional case management services, including assessment and linkages to needed outpatient services in the local communities, for both study conditions, including crisis intervention. If assigned to the MET group, the sessions were initiated within 2 weeks of the baseline interview. From the participant’s perspective, MET sessions took place in a private, confidential setting adjacent to the rural parole office, and each participant was remotely connected with the therapist using portable, desktop videoconferencing equipment (Tanberg MXP150, http://www.solutionzinc.com/Video-Conferencing/Video-Desktop/TANDBERG-150-MXP-TANDBERG-150-MXP.html). The videoconferencing equipment included an 8-in. screen and a regular Internet cable and modem (see Figure 1). The equipment is portable and can be used in regular offices or conference rooms throughout the parole building or adjacent office to ensure participant confidentiality. Either the research coordinator or the SSC assisted with equipment set up, but left the room before each counseling session, to ensure privacy. The therapist used Polycom PVX software (http://www.polycom.com) on a regular personal computer in the urban-based, university office. The PVX software was used because it allows for connections with multiple user interfaces (Tanbergs) in the different rural parole offices.
Figure 1.
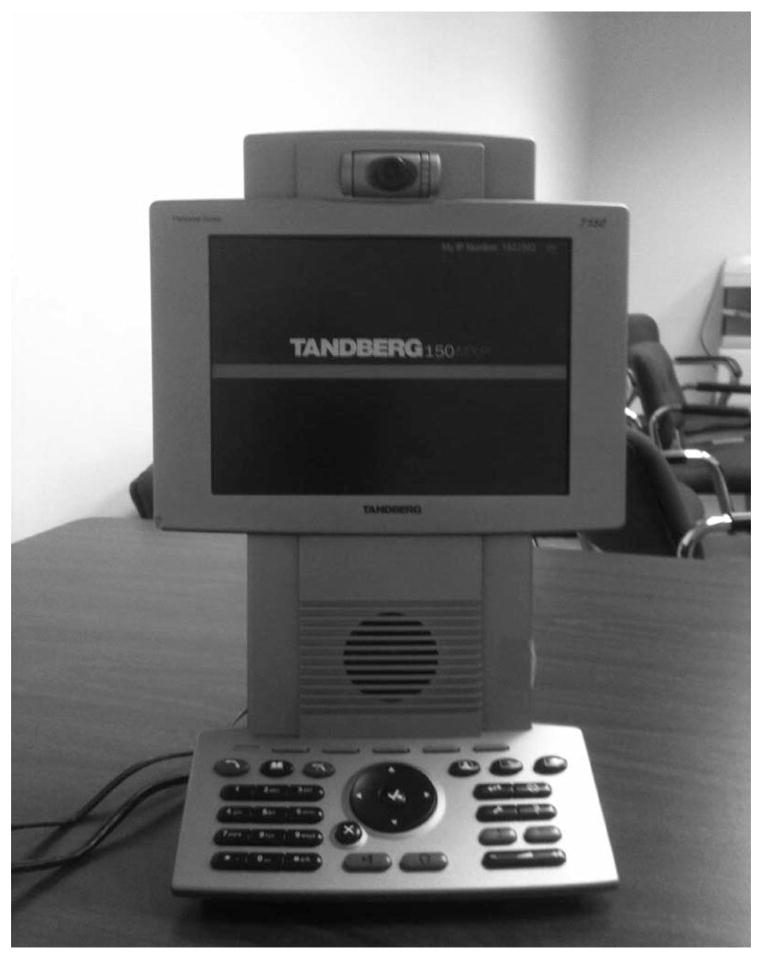
Tanberg MXP150.
The initial MET session included a telemedicine-based assessment conducted by the study therapist using a computerized version of Drinker’s Checkup (DCU) (Hester & Squires, 2008) to ascertain the participant’s level of drinking risk behavior, the participant’s concerns about drinking behavior, and the potential risks for relapse. The computerized version of the DCU has been shown to perform similarly to the face-to-face version of the DCU in assessing drinking behavior and drinking risk (Walker, Roffman, Picciano, & Stephens, 2007). The initial telemedicine session (or Session 2) also included a review of the DCU to discuss the assessment to provide feedback about a participant’s risk behaviors and to determine if there were any particular areas of concern that he or she would like to discuss during the sessions. The goal of the first two sessions was to establish a baseline assessment of the participant’s risks and to develop a plan for change over the next few weeks.
Subsequent MET sessions (3– 4) examined the client’s current motivation for staying sober and worked with the client to progress him or her through a series of stages to reduce relapse stressors (Miller, 1995). Up to four MET sessions were conducted over 12 weeks, which is consistent with the MET approach (DiClemente et al., 1999). Sessions were scheduled on the same day as the client’s visit to the parole officer in order to eliminate the need for additional travel. To increase session confidentiality, participants are asked to sign in separately to see the SSC after meeting with their parole officers to ensure that the therapy sessions remained independent of correctional supervision and monitoring.
Of the 75 participants who completed a baseline interview, 33 were randomized to the MET telemedicine condition. Of the 33 randomized to receive MET sessions, 24 participants (72.7%) have successfully engaged in the intervention by completing the first session, which consisted of the DCU and feedback session. Of the 9 participants who did not engage in the intervention, reasons for not doing so included transportation concerns (n = 3), securing employment (n = 4), returning to custody (n = 1), and unknown or lost contact (n = 1). To date, of the 24 participants who are participating in the intervention, eight participants have completed 1–2 sessions, four participants have completed three sessions, and 12 participants have completed the targeted four sessions. Consistent with other telemedicine-based studies, session engagement and session completion are indicators of the feasibility of the telemedicine approach to delivery services (Dorsey et al., 2010). Because this trial is ongoing, these feasibility measures are intended to be preliminary, because some participants who have been enrolled but have not participated in telemedicine sessions may engage in the trial before it concludes.
The Next Steps
This ongoing project will continue to address whether telemedicine-based videoconferencing can be a feasible option for delivering evidence-based practices in rural communities. The use of telemedicine videoconferencing to provide services for substance use and mental health issues in criminal justice populations has produced benefits including monitoring psychotropic medications (Manfredi, Shupe, & Batki, 2005). Using technology, however, is limited in real-world settings. Thus, feasibility becomes critically important when these settings do not have a traditional clinical focus or purpose—such as a probation or a parole office. Preliminary findings from this study suggest that telemedicine may be a viable option. With nearly three quarters of the participants in this study (72.7%) engaging in the MET intervention in this nontraditional, real-world setting, which is not intended as a therapeutic milieu, using telemedicine in real-world settings to reach substance users who may not otherwise frequent formal treatment programs could be a component of a future treatment plan. Of those who have engaged in the intervention, half (50%) have already completed the majority of scheduled MET sessions. Future research from this study will focus on intervention effectiveness in reducing alcohol use and related problems, as well as on other indicators of treatment process, including intervention engagement and counselor rapport. Future research will also examine treatment outcomes in the context of satisfaction with the telemedicine-based services, including the extent to which participants feel comfortable with counseling using videoconferencing, how well the technology performs (volume level, picture quality), and if the intervention is a good fit for the service-delivery mechanism.
Study Limitations
This study has limitations. First, due to the sensitive nature of the interview questions and the content of the therapy sessions, the probation and parole office environment may threaten the integrity of the data. To increase confidentiality, each screening session, interview, and therapy session took place in a private, confidential office (usually a group room or conference room). The study team also obtained a federal certificate of confidentiality, as an extra layer of participant protection. Despite efforts to protect confidentiality, it is possible that the community corrections environment influenced enrollment, retention, and self-report accuracy. Second, the study sample includes primarily White men. Although this sample makeup is fairly reflective of the demographics of offenders on probation and parole in the targeted rural communities, the generalizability of study findings is limited. Finally, because the trial is ongoing, outcome data are not currently available to examine intervention effectiveness in reducing alcohol use and related problems. Outcome analysis will be forthcoming.
Conclusion
Despite these limitations, the findings from this study demonstrate significant treatment need and limited treatment utilization, which provide evidence for the need to link offenders who have a history of hazardous and problem drinking with innovative and evidence-based services. Because alcohol use is legal, criminal activity is often viewed as a consequence of alcohol use and only brought to the attention of the criminal justice system when the crime leads to a public health concern, such as drinking and driving or abuse of a partner and/or children. The public health problem associated with hazardous drinking among offenders may be overlooked in policy priorities and substance abuse treatment (Farabee, Prendergast, & Cartier, 2002; Martin, Bryant, & Fitzgerald, 2001). Therefore, a significant number of individuals who engage in hazardous drinking enter the criminal justice system, do not get treatment, and return to the community under supervision with limited treatment resources. Without accessible and effective treatment opportunities that specifically target alcohol abstinence, rural offenders with a history of hazardous drinking are at increased risk in the community. This study demonstrates that telemedicine is a feasible and acceptable option to deliver services in real-world, accessible settings for offenders with a history of hazardous drinking. This approach holds promise to eliminate some of the barriers to access and utilization of effective, evidenced-based treatment for rural alcohol users.
Acknowledgments
Supported by the National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health (Grant R21-AA017937).
Contributor Information
Michele Staton-Tindall, University of Kentucky College of Social Work and University of Kentucky Center on Drug and Alcohol Research.
Elizabeth Wahler, University of Kentucky College of Social Work and University of Kentucky Center on Drug and Alcohol Research.
J. Matthew Webster, University of Kentucky Center on Drug and Alcohol Research and Department of Behavioral Science, University of Kentucky.
Theodore Godlaski, University of Kentucky College of Social Work.
Rebecca Freeman, University of Kentucky College of Social Work.
Carl Leukefeld, University of Kentucky Center on Drug and Alcohol Research and Department of Behavioral Science, University of Kentucky.
References
- Adamson SJ, Sellman JD. Five-year outcomes of alcohol dependent persons treated with motivational enhancement. Journal of Studies on Alcohol and Drugs. 2008;69:589–593. doi: 10.15288/jsad.2008.69.589. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guidelines for use in primary care. 2. Geneva, Switzerland: Department of Mental Health and Substance Dependence, World Health Organization; 2001. [Google Scholar]
- Bácskai E, Czobor P, Gerevich J. Heavy drinking as a differential predictor of physical aggression in clinical and general populations. Progress in Neuro-Psychopharmacology & Biological Psychology. 2008;32:668–672. doi: 10.1016/j.pnpbp.2007.11.016. [DOI] [PubMed] [Google Scholar]
- Bakke B, Mitchell J, Wonderlich S, Erickson R. Administering cognitive-behavioral therapy for bulimia nervosa via telemedicine in rural settings. International Journal of Eating Disorders. 2001;30:454–457. doi: 10.1002/eat.1107. [DOI] [PubMed] [Google Scholar]
- Bashshur RL, Reardon TG, Shannon GW. Telemedicine: A new health care delivery system. Annual Review of Public Health. 2000;21:613–637. doi: 10.1146/annurev.publhealth.21.1.613. [DOI] [PubMed] [Google Scholar]
- Beckham N. Motivational interviewing with hazardous drinkers. Journal of the American Academy of Nurse Practitioners. 2007;19:103–110. doi: 10.1111/j.1745-7599.2006.00200.x. [DOI] [PubMed] [Google Scholar]
- Booth BM, Curran GM. Variations in drinking patterns in the rural south: Joint effects of race, gender, and rural residence. The American Journal of Drug and Alcohol Abuse. 2006;32:561–568. doi: 10.1080/00952990600920409. [DOI] [PubMed] [Google Scholar]
- Booth BM, Kirchner J, Fortney J, Ross R, Rost K. Rural at-risk drinkers: Correlates and one-year use of alcoholism treatment services. Journal of Studies on Alcohol. 2000;61:267–277. doi: 10.15288/jsa.2000.61.267. [DOI] [PubMed] [Google Scholar]
- Borders TF, Booth BM. Rural, suburban, and urban variations in alcohol consumption in the United States: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Rural Health. 2007;23:314–321. doi: 10.1111/j.1748-0361.2007.00109.x. [DOI] [PubMed] [Google Scholar]
- Brems C, Johnson ME, Warner TD, Roberts LW. Barriers to healthcare as reported by rural and urban interprofessional providers. Journal of Interprofessional Care. 2006;20:105–118. doi: 10.1080/13561820600622208. [DOI] [PubMed] [Google Scholar]
- Brems C, Johnson ME, Warner TD, Roberts LW. Exploring differences in caseloads of rural and urban healthcare providers in Alaska and New Mexico. Public Health. 2007;121:3–17. doi: 10.1016/j.puhe.2006.07.031. [DOI] [PubMed] [Google Scholar]
- Brown JM, Miller WR. Impact of motivational interviewing on participation and outcome in residential alcoholism treatment. Psychology of Addictive Behaviors. 1993;7:211–218. doi: 10.1037/0893-164X.7.4.211. [DOI] [Google Scholar]
- Brumback T, Cao D, King A. Effects of alcohol on psychomotor performance and perceived impairment in heavy binge social drinkers. Drug and Alcohol Dependence. 2007;91:10–17. doi: 10.1016/j.drugalcdep.2007.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Nich C, Martino S, Frankforter TL, Farentinos C, … Woody GE. Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: A multisite effectiveness study. Drug and Alcohol Dependence. 2006;81:301–312. doi: 10.1016/j.drugalcdep.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Farentinos C, Ball SA, Crits-Christoph P, Libby B, Morgenstern J, … Woody GE. MET meets the real world: Design issues and clinical strategies in the Clinical Trials Network. Journal of Substance Abuse Treatment. 2002;23:73–80. doi: 10.1016/S0740-5472(02)00255-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conklin TJ, Lincoln T, Tuthill RW. Self-reported health and prior health behaviors of newly admitted correctional inmates. American Journal of Public Health. 2000;90:1939–1941. doi: 10.2105/AJPH.90.12.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conley TB. Construct validity of the MAST and AUDIT with multiple offender drunk drivers. Journal of Substance Abuse Treatment. 2001;20:287–295. doi: 10.1016/S0740-5472(01)00159-3. [DOI] [PubMed] [Google Scholar]
- Connor JP, Jack A, Feeney GF, Young RM. Validity of the obsessive compulsive drinking scale in a heavy drinking population. Alcoholism: Clinical and Experimental Research. 2008;32:1067–1073. doi: 10.1111/j.1530-0277.2008.00668.x. [DOI] [PubMed] [Google Scholar]
- De Silva P, Jayawardana P, Pathmeswaran A. Concurrent validity of the Alcohol Use Disorders Identification Test (AUDIT) Alcohol and Alcoholism. 2008;43:49–50. doi: 10.1093/alcalc/agm061. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Bellino LE, Neavins TM. Motivation for change and alcoholism treatment. Alcohol Research & Health. 1999;23:86–92. [PMC free article] [PubMed] [Google Scholar]
- Donovan DM, Kadden RM, DiClemente CC, Carroll KM. Client satisfaction with three therapies in the treatment of alcohol dependence: Results from Project MATCH. The American Journal on Addictions. 2002;11:291–307. doi: 10.1080/10550490290088090. [DOI] [PubMed] [Google Scholar]
- Donovan DM, Kivlahan DR, Doyle SR, Longabaugh R, Greenfield SF. Concurrent validity of the Alcohol Use Disorders Identification Test (AUDIT) and AUDIT zones in defining levels of severity among out-patients with alcohol dependence in COMBINE study. Addiction. 2006;101:1696–1704. doi: 10.1111/j.1360-0443.2006.01606.x. [DOI] [PubMed] [Google Scholar]
- Dorsey ER, Deuel LM, Voss TS, Finnigan K, George BP, Eason S, … Biglan KM. Increasing access to specialty care: A pilot, randomized controlled trial of telemedicine for Parkinson’s disease. Movement Disorders. 2010;25:1652–1659. doi: 10.1002/mds.23145. [DOI] [PubMed] [Google Scholar]
- D’Souza R. Improving treatment adherence and longitudinal outcomes in patients with a serious mental illness by using telemedicine. Journal of Telemedicine and Telecare. 2002;8:113–115. doi: 10.1258/135763302320302280. [DOI] [PubMed] [Google Scholar]
- Durazzo TC, Rothlind JC, Cardenas VA, Studholme C, Weiner MW, Meyerhoff DJ. Chronic cigarette smoking and heavy drinking in human immunodeficiency virus: Consequences for neurocognition and brain morphology. Alcohol. 2007;41:489–501. doi: 10.1016/j.alcohol.2007.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farabee D, Prendergast M, Cartier J. Alcohol, the “un-drug. Psychiatric Services. 2002;53:1375–1376. doi: 10.1176/appi.ps.53.11.1375. [DOI] [PubMed] [Google Scholar]
- Fazel S, Bains P, Doll H. Substance abuse and dependence in prisoners: A systematic review. Addiction. 2006;101:181–191. doi: 10.1111/j.1360-0443.2006.01316.x. [DOI] [PubMed] [Google Scholar]
- Fleming M, Manwell LB. Brief intervention in primary care settings: A primary treatment method for at-risk, problem, and dependent drinkers. Alcohol Research & Health. 1999;23:128–137. [PMC free article] [PubMed] [Google Scholar]
- Fletcher BW, Chandler RK. Principles of drug abuse treatment for criminal justice populations — A research-based guide. 2006 Retrieved from http://www.nida.nih.gov/podat_cj/
- Fortney J, Booth BM. Access to substance abuse services in rural areas. Recent Developments in Alcoholism. 2001;15:177–197. doi: 10.1007/978-0-306-47193-3_10. [DOI] [PubMed] [Google Scholar]
- Fortney J, Mukherjee S, Curran G, Fortney S, Han X, Booth BM. Factors associated with perceived stigma for alcohol use and treatment among at-risk drinkers. The Journal of Behavioral Health Services & Research. 2004;31:418–429. doi: 10.1007/BF02287693. [DOI] [PubMed] [Google Scholar]
- Fortney JC, Booth BM, Blow FC, Bunn JY. The effects of travel barriers and age on the utilization of alcoholism treatment aftercare. The American Journal of Drug and Alcohol Abuse. 1995;21:391–406. doi: 10.3109/00952999509002705. [DOI] [PubMed] [Google Scholar]
- Fuller RK, Hiller-Sturmhofel S. Alcoholism treatment in the United States: An overview. Alcohol Research & Health. 1999;23:69–77. [PMC free article] [PubMed] [Google Scholar]
- Gordon AJ, Maisto SA, McNeil M, Kraemer KL, Conigliaro RL, Kelley ME, Conigliaro J. Three questions can detect hazardous drinkers. The Journal of Family Practice. 2001;50:313–320. [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM–IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Greenfeld LA. Alcohol and crime: An analysis of national data on the prevalence of alcohol involvement in crime. Washington, DC: U.S. Bureau of Justice Statistics; 1998. NCJ Publication No. 168632. [Google Scholar]
- Guze SB, Cantwell DP. Alcoholism, parole observations and criminal recidivism: A study of 116 parolees. The American Journal of Psychiatry. 1965;122:436–439. doi: 10.1176/ajp.122.4.436. [DOI] [PubMed] [Google Scholar]
- Hartley D, Britain C, Sulzbacher S. Behavioral health: Setting the rural health research agenda. The Journal of Rural Health. 2002;18:242–255. doi: 10.1111/j.1748-0361.2002.tb00934.x. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Burnam A, McEvoy LT. Alcohol abuse and dependence: The diagnosis of alcoholism. In: Robins LN, Regier DA, editors. Psychiatric disorders in America: The Epidemiologic Catchment Area Study. New York, NY: The Free Press; 1991. pp. 81–95. [Google Scholar]
- Hester RK, Squires DD. Web-based norms for the Drinker Inventory of Consequences from the Drinker’s Checkup. Journal of Substance Abuse Treatment. 2008;35:322–327. doi: 10.1016/j.jsat.2007.10.005. [DOI] [PubMed] [Google Scholar]
- Jackson JE, Doescher MP, Hart LG. Problem drinking: Rural and urban trends in America, 1995/1997 to 2003. Preventive Medicine: An International Journal Devoted to Practice and Theory. 2006;43:122–124. doi: 10.1016/j.ypmed.2006.02.006. [DOI] [PubMed] [Google Scholar]
- Jones GY, Hoffman NG. Alcohol dependence: International policy implications for prison populations. Substance Abuse Treatment, Prevention, and Policy. 2006;1:33. doi: 10.1186/1747-597X-1-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manfredi L, Shupe J, Batki SL. Rural jail telepsychiatry: A pilot feasibility study. Telemedicine and e-Health. 2005;11:574–577. doi: 10.1089/tmj.2005.11.574. [DOI] [PubMed] [Google Scholar]
- Martin SE, Bryant K, Fitzgerald N. Self-reported alcohol use and abuse by arrestees in the 1998 arrestee drug abuse monitoring program. Alcohol Research & Health. 2001;25:72–79. [PMC free article] [PubMed] [Google Scholar]
- McAuliffe WE, LaBrie R, Woodworth R, Zhang C, Dunn RP. State substance abuse treatment gaps. The American Journal on Addictions. 2003;12:101–121. [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters F, Smith I, Grissom G, … Argeriou M. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-S. [DOI] [PubMed] [Google Scholar]
- Miller WR. Motivational enhancement therapy with drug abusers. Albuquerque, NM: University of Albuquerque Department of Psychology and Center on Alcoholism, Substance Abuse, and Addictions; 1995. Retrieved from http://www.motivationalinterview.org/Documents/METDrugAbuse.PDF. [Google Scholar]
- Miller TR, Cohen MA, Wiersema B. Victim costs and consequences: A new look. Washington, DC: National Institute of Justice, U.S. Department of Justice; 1996. NCJ 155282. Retrieved from https://www.ncjrs.gov/pdffiles/victcost.pdf. [Google Scholar]
- Miller WR, Benefield G, Tonigan JS. Enhancing motivation for change in problem drinking: A controlled comparison of two therapist styles. Journal of Consulting and Clinical Psychology. 1993;61:455–461. doi: 10.1037/0022-006X.61.3.455. [DOI] [PubMed] [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational enhancement therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. Rockville, MD: National Institute of Alcohol Abuse and Alcoholism; 1992. Project MATCH Monograph Series, Vol. 2, DHHS 92–1894. [Google Scholar]
- Moore AA, Beck JC, Babor TF, Hays RD, Reuben DB. Beyond alcoholism: Identifying older, at-risk drinkers in primary care. Journal of Studies on Alcohol. 2002;63:316–324. doi: 10.15288/jsa.2002.63.316. [DOI] [PubMed] [Google Scholar]
- Mumola C. Substance abuse treatment, state and federal prisoners, 1997 (Special Report NCJ 172871) Washington, DC: U.S. Department of Justice; 1999. [Google Scholar]
- Myers TC, Swan-Kremeier L, Wonderlich S, Lancaster K, Mitchell JE. The use of alternative delivery systems and new technologies in the treatment of patients with eating disorders. International Journal of Eating Disorders. 2004;36:123–143. doi: 10.1002/eat.20032. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. National Institute on Alcohol Abuse and Alcoholism: Five year strategic plan FY09–14. Alcohol across the lifespan. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2008. Retrieved from http://pubs.niaaa.nih.gov/publications. [Google Scholar]
- Nelson EL, Barnard M, Cain S. Treating childhood depression over videoconferencing. Telemedicine Journal and E-Health. 2003;9:49–55. doi: 10.1089/153056203763317648. [DOI] [PubMed] [Google Scholar]
- Nochajski TH, Stasiewicz PR. Assessing stages of change in DUI offenders: A comparison of two measures. Journal of Addictions Nursing. 2005;16:57–67. doi: 10.1080/10884600590919127. [DOI] [Google Scholar]
- Oser CB, Leukefeld CG, Tindall MS, Havens JR, Webster JM, Smiley-McDonald HM, Cosentino AL. Male and female rural probationers: HIV risk behaviors and knowledge. AIDS Care. 2006;18:339–344. doi: 10.1080/02652040500200491. [DOI] [PubMed] [Google Scholar]
- Prat G, Adan A, Pérez-Pàmies M, Sànches-Turet M. Neurocognitive effects of alcohol hangover. Addictive Behaviors. 2008;33:15–23. doi: 10.1016/j.addbeh.2007.05.002. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test: An update of research findings. Alcoholism: Clinical Experimental Research. 2007;31:185–199. doi: 10.1111/j.1530-0277.2006.00295.x. [DOI] [PubMed] [Google Scholar]
- Saitz R, Palfai TP, Cheng DM, Horton NJ, Freedner N, Dukes K, … Samet JH. Brief intervention for medical inpatients with unhealthy alcohol use: A randomized, controlled trial. Annals of Internal Medicine. 2007;146:167–176. doi: 10.7326/0003-4819-146-3-200702060-00005. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Lee NK. Hazardous alcohol use: Its delineation as a subthreshold disorder, and approaches to its diagnosis and management. Comprehensive Psychiatry. 2000;41:95–103. doi: 10.1016/S0010-440X(00)80015-2. [DOI] [PubMed] [Google Scholar]
- Sellman JD, Sullivan PF, Dore GM, Adamson SJ, MacEwan I. A randomized controlled trial of motivational enhancement therapy (MET) for mild to moderate alcohol dependence. Journal of Studies on Alcohol. 2001;62:389–396. doi: 10.15288/jsa.2001.62.389. [DOI] [PubMed] [Google Scholar]
- Shore JH, Brooks E, Savin DM, Manson SM, Libby AM. An economic evaluation of telehealth data collection with rural populations. Psychiatric Services. 2007;58:830–835. doi: 10.1176/appi.ps.58.6.830. [DOI] [PubMed] [Google Scholar]
- Shore JH, Manson SM. A developmental model for rural telepsychiatry. Psychiatric Services. 2005;56:976–980. doi: 10.1176/appi.ps.56.8.976. [DOI] [PubMed] [Google Scholar]
- Sinha R, Easton C, Renee-Aubin L, Carroll KM. Engaging young probation-referred marijuana-abusing individuals in treatment: A pilot trial. The American Journal on Addiction. 2003;12:314–323. [PubMed] [Google Scholar]
- Thevos AK, Thomas SE, Randall CL. Social support in alcohol dependence and social phobia: Treatment comparisons. Research on Social Work Practice. 2001;11:458–472. doi: 10.1177/104973150101100403. [DOI] [Google Scholar]
- Tschirch P, Walker G, Calvacca L. Nursing in tele-mental health. Journal of Psychosocial Nursing and Mental Health Services. 2006;44:20–27. doi: 10.3928/02793695-20060501-05. [DOI] [PubMed] [Google Scholar]
- Van Gundy K. Reports on Rural America: Vol. 1, No. 2. Substance abuse in rural and small town America. Durham, NH: The Carsey Institute; 2006. Retrieved from http://www.carseyinstitute.unh.edu/publications/Report_SubstanceAbuse.pdf. [Google Scholar]
- Visher C, LaVigne N, Travis J. Returning home: Understanding the challenges of prisoner reentry. Maryland pilot study: Findings from Baltimore. Washington, DC: Justice Policy Center, The Urban Institute; 2004. JPC Publication CPR04 0122. Retrieved from http://www.urban.org/publications/410974.html. [Google Scholar]
- Walker DD, Roffman RA, Picciano JF, Stephens RS. The check-up: In-person, computerized, and telephone adaptations of motivational enhancement treatment to elicit voluntary participation by the contemplator. Substance Abuse Treatment, Prevention, and Policy. 2007;2:2. doi: 10.1186/1747-597X-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters S. Behavioral change counseling index (BECCI) - Criminal Justice Version. 2002 Retrieved November 2, 2011, Retreived from http://motivationalinterview.net/library/becci-cj.pdf.
- Webster JM, Dickson MF, Duvall JL, Clark DB. Rural and urban differences in Kentucky DUI offenders. Journal of Addiction Medicine. 2010;4:186–190. doi: 10.1097/ADM.0b013e3181c6cb24. [DOI] [PubMed] [Google Scholar]
- Webster JM, Oser CB, Mateyoke-Scrivner A, Cline VD, Havens JR, Leukefeld CG. Drug use and criminal activity among rural probationers with DUI histories. International Journal of Offender Therapy and Comparative Criminology. 2009;53:717–730. doi: 10.1177/0306624X08323615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Matzger H, Kaskutas LA. How important is treatment? One-year outcomes of treated and untreated alcohol-dependent individuals. Addiction. 2003;98:901–911. doi: 10.1046/j.1360-0443.2003.00438.x. [DOI] [PubMed] [Google Scholar]
- Widom CS, White HR, Czaja SJ, Marmorstein NR. Long-term effects of child abuse and neglect on alcohol use and excessive drinking in middle adulthood. Journal of Studies on Alcohol and Drugs. 2007;68:317–326. doi: 10.15288/jsad.2007.68.317. [DOI] [PubMed] [Google Scholar]
- Zaylor C. Clinical outcomes in telepsychiatry. Journal of Telemedicine and Telecare. 1999;5(Suppl 1):S59–S60. doi: 10.1258/1357633991932577. [DOI] [PubMed] [Google Scholar]
- Zhang Z. Drug and alcohol use and related matters among arrestees. Washington, DC: Office of Justice Programs, National Institute of Justice; 2003. NIJ Publication No. 2001C-003. Retrieved from https://www.ncjrs.gov/nij/adam/ADAM2003.pdf. [Google Scholar]


