Abstract
Objectives
The current study tested hypotheses derived from Joiner’s (2005) interpersonal theory of suicide, which proposes that deliberate self-harm (DSH) becomes increasingly more reinforcing with repetition.
Methods
One hundred six participants with a history of DSH completed questionnaires about their emotions and experience of physical pain during their most recent DSH episode.
Results
Consistent with prediction, people with more numerous past DSH episodes felt more soothed, more relieved, and calmer following their most recent episode of DSH. Contrary to prediction, greater numbers of past DSH episodes were associated with more intense physical pain during the most recent episode.
Conclusion
The findings suggest that the emotion regulation functions of DSH may become more reinforcing with repetition.
Keywords: deliberate self-harm, opponent process theory, self-injury, suicidal behavior
Introduction
Deliberate self-harm (DSH) refers to a spectrum of behavior that includes suicide attempts (self-injurious behavior with the intent to die and a nonfatal outcome) and nonsuicidal self-injury (NSSI; intentional self-harm behavior, such as cutting or burning oneself, without any intent to die as a result). For decades, repetitive NSSI has been characterized as a puzzling phenomenon and challenging clinical issue in the psychiatric literature (Graff & Mallin, 1967; Brown, Comtois, & Linehan, 2002; Muehlenkamp, 2005; Pattison & Kahan, 1983). Recent conceptualizations of NSSI utilize a functional (e.g., behavioral reinforcement schedule) approach to describe the seemingly addictive qualities of repetitive NSSI among some individuals (Chapman, Gratz, & Brown, 2006; Nock & Prinstein, 2004). For example, Chapman et al. (2006) proposed the Experiential Avoidance Model (EAM), which posits that NSSI among non-psychotic, cognitively normal adults is maintained through a negative reinforcement feedback loop, whereby NSSI functions as a maladaptive coping strategy for avoidance of aversive emotional experiences. Chapman et al.’s (2006) model fits well with findings that individuals who engage in NSSI report doing so for calming effects (Kemperman, Russ, & Shearin, 1997), and findings that adolescents and young adults tend to report engaging in NSSI for the regulation of emotional or physiological experiences (Nock & Prinstein, 2004; Nock, Prinstein, & Sterba, 2009). Psychophysiological evidence bolsters the self-report findings, in that people who habitually engage in NSSI experience physiological signs of tension reduction during self-mutilation imagery tasks (Brain, Haines, & Williams, 1998; Haines et al., 1995).
Muehlenkamp et al. (2009) examined the influence of NSSI on affect in a naturalistic setting with a sample of 131 women with bulimia nervosa. Participants were asked to record behaviors (including DSH) and emotion ratings via a palmtop computer for a two-week period. Participants reported an increase in negative affect leading up to an NSSI episode, but there was not a significant decrease in negative affect following the episode. In contrast, participants reported a decrease in levels of positive affect leading up to the NSSI incident, and a significant increase in positive affect following the incident. This finding is inconsistent with the EAM model prediction that NSSI is negatively reinforced, and suggests that NSSI is more likely to become habitual through positive reinforcement (i.e., increased positive affect following NSSI). However, this interpretation is tentative given the relatively few NSSI incidents (n=19) that occurred during the study period.
In another study, Welch et al. (2008) examined negative affect and DSH among individuals with borderline personality disorder through the use of imagery scripts. Based upon information obtained through interviews, individualized scripts were created for a past NSSI incident and a suicide attempt for each participant. Negative affect was assessed at multiple time points while the participants listened to audio recordings of the incident imagery scripts. Consistent with EAM, the results suggested that individuals experience a decrease in negative affect following (but not during) an NSSI episode. In contrast, participants tended to report more negative affect following an imagined suicide attempt than during the imagined episode. A limitation of the Welch et al. (2008) study is the exclusion of an assessment of positive affect. In light of Muehlenkamp et al.’s (2009) findings, the assessment of both negative (e.g., distress) and positive emotions (e.g., soothed) may be necessary to capture the full effects of DSH on emotional responses.
The interpersonal theory of suicidal behavior (Joiner, 2005; Van Orden, Witte, Cukrowicz, Braithwaite, Selby, & Joiner, 2010) adds to the EAM framework, in that it predicts that DSH (including NSSI and suicide attempts) becomes more reinforcing with number of incidents due to mechanisms outlined in Solomon’s (1980) opponent process theory. Specifically, opponent process theory states that, with repetition, the opposite effects of a provocative stimulus (i.e., the opponent process), are strengthened, which behaviorally manifests as habituation. With regards to suicidal behavior, the interpersonal theory proposes that not only do opponent processes become strengthened by repeated exposure, but also that the primary processes (e.g., fear) weaken with repeated exposure. Thus, the theory posits that suicidal individuals may “build up” a tolerance for the negative aspects of suicide (e.g., physical pain, fear) through repeated exposure to painful stimuli, such as NSSI and suicide attempts, which evoke opponent processes and habituation. That is, as exposure to painful experiences increase, an individual’s experience of negative aspects (the “a” process in opponent process theory) weakens, while their positive experiences (the “b” process in opponent process theory), such as relief, strengthen.
Consistent with the interpersonal theory of suicide, there are data suggesting that repeated NSSI is correlated with higher pain tolerance. Women who are diagnosed with borderline personality disorder (BPD) and who engage in NSSI have higher pain threshold and tolerance levels on laboratory tasks (e.g., the cold pressor task) than BPD patients who do not self-injure (Kemperman et al., 1997), depressed inpatients (Russ et al., 1999), and healthy controls (Bohus et al., 2000). In addition, two studies have demonstrated greater pain tolerance in suicidal individuals than non-suicidal psychiatric patients, community controls (Orbach et al., 1997), and accident victims (Orbach et al., 1996).
One study that specifically speaks to whether DSH becomes more reinforcing with recurrence was conducted by Brain, Haines, and Williams (2002), who found that individuals who had engaged in more frequent NSSI (five or more lifetime incidents) reported feeling more relaxed (as opposed to anxious), more unafraid (as opposed to afraid), more happy (as opposed to sad), and more relieved (as opposed to uptight) after imagining self-mutilating than a group with less frequent NSSI (less than five lifetime incidents). Interestingly, no group differences emerged in the psychophysiological data during the self-mutilation imagery task in this sample. A limitation of the study was the arbitrary dichotomization of participants into groups (five or greater NSSI episodes versus less than five NSSI episodes), rather than treating the frequency of NSSI as a continuous variable. This may have restricted power as there were twice as many participants in the 5 or greater incidents group (n=29) than in the five or fewer incidents group (n=14). Furthermore, the study did not include suicide attempts as a variable even though, the interpersonal theory would predict that suicide attempt history would also influence the experience of NSSI.
The current study sought to build upon previous literature by evaluating the hypotheses, proposed by the interpersonal theory of suicide, that with each incidence of DSH (including suicide attempts and NSSI), the experience of negative feelings (e.g., fear) would decrease, while the experience of positive feelings (e.g., soothed) would increase. It was also predicted that the more DSH episodes individuals reported, the more soothed (as opposed to upset) and the more relieved (as opposed to distressed) they would feel following their most recent DSH episode (i.e., subsequent to repeated exposure and thereby activation of habituation and opponent processes). Finally, it was predicted that the individuals who reported the most episodes of DSH would experience the least amount of physical pain during their most recent episode, because of habituation to the painful aspects of DSH via mechanisms proposed by the opponent process theory and the interpersonal theory of suicide.
Methods
Participants were drawn from two sources between July 2003 and January 2006. Thirty-nine of the participants represented all adults applying to the Florida State University (FSU) Psychology Clinic for therapeutic services from July 2003 to January 2006 who endorsed a history of DSH on a questionnaire that was administered with their application materials. All patients were informed of the research and training nature of the clinic and signed a form consenting to their inclusion in clinic research. The patient sample was comprised of 39 patients: 29 females (74.4%) and 10 males (25.6%). The average age of the adult patient sample was 23.87 (SD = 7.14) with ages ranging from 18 to 43. The ethnic composition was 82.1% (n = 32) White, 2.6% (n = 1) Black, 10.3% (n = 4) Hispanic, 2.6% (n = 1) Asian/Pacific Islander, and 2.6% (n = 1) who chose not to identify his/her race.
The FSU Psychology Clinic serves patients with psychiatric disorders typical of a community outpatient mental health clinic and employs minimal exclusionary criteria, excluding from treatment only those who are at imminent risk to harm themselves or others and require hospitalization. Diagnostic information was gathered by graduate student therapists (under the close supervision of doctoral level clinical psychologists) during the intake process. These chart diagnoses, including Axis II diagnoses, were established using clinical interviewing procedures similar to the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders (SCID; First, Spitzer, Gibbon, & Williams, 1997) in their review of presenting symptoms and systematic differential diagnosis. A prior study using patients from this sample has demonstrated adequate inter-rater reliability of the diagnoses in this clinic (Witte et al., 2009).
Of the patients in the sample who attended the intake session and received a diagnosis (with overlapping ns due to co-morbidity), 26 (66.7%) were diagnosed with at least one mood disorder, 12 (30.7%) with at least one substance use disorder, 9 (23.1%) with at least one personality disorder (8 of which had borderline personality disorder), 7 (17.9%) with anxiety disorders, 3 (7.7%) with eating disorders, 2 (5.1%) with psychotic disorders, and 5 (12.8%) with another disorder not captured in the general diagnostic categories previously named.
An additional 67 participants (88.1% female; mean age = 19.22, SD = 3.01) were drawn from other studies being conducted in a mood disorders laboratory between July 2003 and January 2006. All participants who endorsed having engaged in DSH provided informed consent and were included in the analyses. Diagnostic data are not available for the undergraduate participants. Furthermore, ethnicity/race data were not collected for 36 (31.9%) of the participants due to a data collection error. Of those participants for whom ethnicity/race was available, 38.0% (n = 11) were White, 31.0% (n = 9) were Black, and 31.0% (n = 9) were Hispanic.
The combined database consisted of a total of 106 participants. Because of the relative rarity of DSH, clinical and nonclinical samples were combined for the current study, a method that has been used in previous research on the topic (Brain et al., 2002). Descriptive statistics for the entire sample are provided in Table 1. The clinical participants were compared to the laboratory participants on the following variables: age of first DSH incident, number of NSSI episodes, number of suicide attempts, and current age. The clinical participants tended be older during their first episode of DSH (M =18.03, SD = 9.62 versus M = 14.11, SD = 3.26), and this difference was statistically significant (F [1, 80] = 7.40, p < .01).
Table 1.
Descriptive Statistics for the Entire Sample
| M | SD | N | % | |
|---|---|---|---|---|
| Age | 21.00 | 5.46 | -- | -- |
| Gender | ||||
| Male | -- | -- | 11 | 17.0% |
| Female | -- | -- | 88 | 83.0% |
| Race | ||||
| White | -- | -- | 43 | 40.6% |
| Black | -- | -- | 10 | 9.4% |
| Asian | -- | -- | 1 | 0.9% |
| Hispanic | -- | -- | 13 | 12.3% |
| Missing | -- | -- | 39 | 36.8% |
| No. of lifetime suicide attempts | 1.12 | 2.12 | -- | -- |
| 0 suicide attempts | -- | -- | 49 | 46.2% |
| 1 suicide attempts | -- | -- | 33 | 31.0% |
| 2 or more suicide attempts | -- | -- | 17 | 16.0% |
| Unknown | -- | -- | 7 | 6.6% |
| No. of NSSI episodes (range 1–100) | 9.97 | 10.56 | -- | -- |
| Age at first DSH episode | 15.51 | 6.56 | -- | -- |
| Age at most recent DSH episode | 17.98 | 5.51 | -- | -- |
| Years since most recent DSH episode | 3.89 | 5.83 | ||
| No. of methods used for DSH | 1.73 | 1.11 | -- | -- |
| No. using method for DSH | ||||
| Cutting | -- | -- | 72 | 67.9% |
| Burning | -- | -- | 22 | 20.8% |
| Headbanging | -- | -- | 14 | 13.2% |
| Drug overdose | -- | -- | 40 | 37.7% |
| Other | -- | -- | 18 | 17.0% |
--
Note. No. = number. NSSI = non-suicidal self-injury. DSH = deliberate self-harm.
A questionnaire about DSH was developed by the first and last authors for the purposes of the current study. A new measure was created because, at the time data collection started, there were no measures that specifically assessed constructs that were crucial to the tests of our hypotheses (see the appendix for the full measure). The first item assesses whether or not the individual has ever intentionally hurt him- or herself. All participants in the current study endorsed this item positively, as this was the means by which they were selected for participation. The participants were also asked about the age at which they first engaged in DSH, which methods were utilized (e.g., cutting, burning, drug overdose, etc.), the most recent date of DSH, the number of episodes of NSSI, and the number of lifetime suicide attempts. In the next section of the questionnaire, participants completed a 20-item scale (i.e., 1 = very slightly or not at all; 2 = a little; 3 = moderately; 4 = quite a bit; 5 = extremely) assessing the degree to which the participant experienced various feelings and emotions in the minutes following his or her most recent self-injury (e.g., interested, hostile, calm, afraid, etc.). This section of the questionnaire was modeled after the Positive And Negative Affect Scale (Watson, Clark, & Tellegen, 1988), but included the addition of some items that the authors rationally derived from previous research as relevant for DSH (calm, fascinated, exhilarated, angry). The positive and negative affect scales demonstrated adequate internal reliability (positive affect items, α = .88; negative affect items, α = .87).
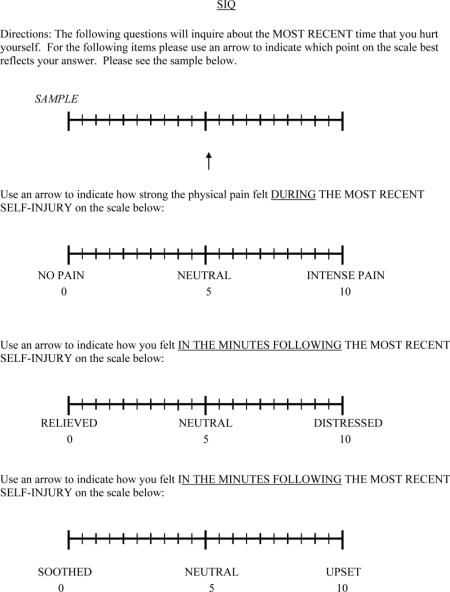
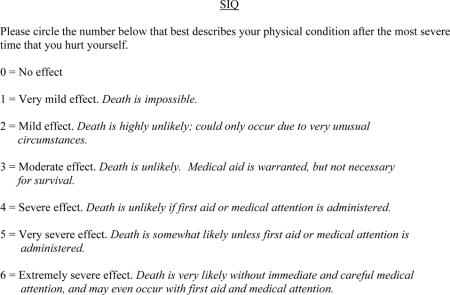
Next, participants were presented with three ten-point scales that assess aspects of their most recent instance of DSH. Anchors for the ten-point scale were derived directly from Joiner’s (2005) theory predictions about the experiences that change as a result of repeated DSH. Participants were asked how much physical pain they had experienced during their most recent DSH episode (1 = no pain…10 = intense pain), how distressed they were in the minutes following the most recent DSH episode (1 = relieved…10 distressed), and how upset they were following the most recent DSH episode (1 = soothed…10 = upset). Finally, participants were asked to characterize their physical condition following their most severe DSH episode by selecting one of the following choices: 0 = no effect; 1 = very mild effect, death is impossible; 2 = mild effect, death is highly unlikely but could occur under very usual circumstances; 3 = moderate effect, death is unlikely, medical aid is warranted but not necessary for survival; 4 = severe effect, death is unlikely if first aid or medical attention is administered; 5 = very severe effect, death is somewhat likely unless first aid or medical attention is administered; 6 = extremely severe effect, death is very likely without immediate and careful medical attention and may even occur with first aid and medical attention (adapted from a section in the Lifetime – Suicide Attempt Self-Injury Scale; Linehan & Comtois, 1996).
Results
DSH history (defined as the summed cumulative number of NSSI episodes and lifetime suicide attempts) was utilized as the independent variable in tests of the hypotheses. Correlations between key variables are displayed in Table 2. Participants tended to report feeling more positive emotions (M = 30.67, SD = 10.27) following their most recent DSH episode compared to negative emotions (M = 17.73, SD = 8.15). As depicted in the table, and contrary to prediction, composite scores for positive and negative affect were not significantly related to the number of DSH episodes. However, the examination of individual scale items revealed a significant negative correlation between the number of DSH episodes and the ratings of how afraid (r = −.22, p <.05) and distressed (r = −.22, p <.05) participants felt following the most recent episode. In addition, there was a significant positive relationship between the number of DSH episodes and ratings of how calm (r = .50, p < .001), and attentive (r = .25, p < .05) participants felt following their most recent DSH incident. This pattern suggests that, consistent with opponent process theory predictions, individuals with more DSH episodes felt less afraid and distressed, and more calm and attentive following their most recent episode.
Table 2.
Intercorrelations Between All Measures
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | -- | |||||||||
| 2. Age | .14 | -- | ||||||||
| 3. NSSI | .07 | −.08 | -- | |||||||
| 4. Attempts | .18 | .27** | .11 | -- | ||||||
| 5. Composite | .12 | −.07 | .99** | .22* | -- | |||||
| 6. Relieved | −.07 | −.09* | −.21* | −.19 | −.24* | -- | ||||
| 7. Soothed | −.02 | −.15* | −.24** | −.09 | −.28** | .65** | -- | |||
| 8. Pain | −.05 | −.15 | .24* | .13 | .23* | −.16 | −.29** | -- | ||
| 9. Positive Emotions | .16 | −.02 | .18 | .26* | .21 | −.21* | −.28* | .04 | -- | |
| 10. Negative Emotions | −.18 | −.05 | −.18 | .04 | −.16 | .30* | .23* | .11 | −.18 | -- |
--
Note. NSSI = nonsuicidal self-injury; Attempts = suicide attempts; Composite = nonsuicidal self-injury and suicide attempts.
= p < .05,
= p <.01.
Regression analyses were used to test the main hypotheses of the study. Because age was significantly correlated with the soothed versus upset and the relieved versus distressed items (see Table 2), age was used as a covariate for the regression analyses. The statistics that are reported reflect findings that include age as a covariate. The first regression revealed that, in support of our hypothesis, number of DSH episodes significantly predicted how soothed versus upset participants felt following the most recent DSH episode (β = −.04, t(88)= −2.52, p=.01, f2= .08), such that the more DSH experience an individual had amassed, the more soothed s/he felt following the most recent DSH episode. Similarly, individuals who reported more incidents of DSH tended to report feeling more relieved (as opposed to distressed) following their most recent DSH episode than individuals who reported fewer incidents of DSH (β = −.04, t(87)= −2.32, p=.02, f2= .06). Also consistent with prediction, a third regression revealed that greater numbers of past DSH episodes were associated with feeling less afraid following the most recent DSH episode (β = −.02, t(87)= −2.20, p=.03, f2= .05). In contrast, a fourth regression revealed that individuals who reported greater numbers of DSH episodes tended to report experiencing more intense physical pain during their most recent DSH episode (β =.03, t(87)= 2.25, p=.027, f2= .06)1.
Discussion
The current study sought to build upon previous literature by examining the effect of repetition on the experience of positive emotions (particularly feeling calm and soothed), negative emotions (especially fear and distress), and physical pain surrounding DSH. Consistent with predictions from the interpersonal theory of suicidal behavior, past histories of repeated lifetime DSH episodes were associated with feeling less afraid, more relieved, and more soothed following the most recent DSH episode. However, contrary to prediction, greater number of lifetime DSH episodes was associated with more intense physical pain during the most recent DSH episode.
The finding that those who have engaged in more DSH episodes experience more physical pain during their most recent DSH episode is inconsistent with our predictions. Nock et al. (2006) found similar results in their clinical adolescent sample; that is, reports of more physical pain were also associated with a greater number of NSSI episodes. In light of our findings and those of Nock et al. (2006), the current conceptualization of DSH within the context of the interpersonal theory warrants revisiting. Opponent process theory concerns changes in affective states with repeated exposure; thus, it is possible that opponent processes and habituation do not apply to the sensory experience of physical pain. If this is the case, we would expect physical pain to remain constant over repeated exposure. However, our results indicate increased pain with repeated exposures. One possible explanation for the findings is that with the reinforcing experience of relief and soothing feelings, individuals may desire a greater intensity of these positive emotions over time, thus it may be necessary to increase the amount of self-inflicted physical pain to achieve even greater emotional relief. This increase in severity of DSH incidents may lead to the inevitable experience of more physical pain over time. Findings that may be in line with this include ours and Nock et al.’s findings that those who engage in NSSI more frequently tend to use a larger variety of methods to inflict self-harm. Perhaps the use of a more diverse array of methods is a reflection of the individual seeking out more extreme methods of DSH over time. Another potential explanation is that the feelings of relief that individuals reported following their most recent DSH are a result of retrospective bias. Those around the person who engaged in DSH may have responded in a caring manner that provided social positive reinforcement for the behavior, which may lead to the decreased negative feelings. This hypothesis could also explain why those who engaged in more frequent DSH also reported more pain. For example, if the social reinforcement of DSH is rewarding enough, the individual may inflict more severe pain in order to continue receiving that positive reinforcement from their environment. It is also possible that the method used in the most recent DSH episode influenced the participants’ pain rating, and that this affected our findings. Finally, Joiner’s interpersonal theory clusters suicide attempts and NSSI together as DSH that can enact opponent processes. Thus, we did not ask participants to differentiate between the two types of DSH when reporting about their most recent DSH episode. There has been recent suggestion that suicide attempts and NSSI should not be clustered together (e.g., Claes et al., 2010), and it is possible that including NSSI with suicide attempts may have influenced our pain findings. Unfortunately, the data from this study were not suited to fully test these hypotheses, but this may be a future direction for research on the role of pain in DSH.
Although this study provides information about the potentially reinforcing properties of DSH, there are some other limitations worth noting. The data were collected cross-sectionally, which limits causal inference regarding repeated DSH and feelings of relief. The EAM (Chapman et al., 2006) and Joiner’s (2005) theory, respectively, are best tested with longitudinal data where variables such as DSH, pain experience, and feelings of relief are assessed at multiple time points. Future longitudinal research is needed to rule out alternative explanations of our findings. For example, it is possible that the individuals who experience the greatest levels of positive and negative reinforcement from DSH are the ones who engage in the behavior more frequently, rather than DSH becoming more reinforcing with repetition. Further, the experiences of individuals who self-injure may be heterogenous and explained by several different functions, such as help-seeking, not just opponent processes and habituation (see Nock, 2009 for a discussion of other possible functions of DSH). A second limitation is that the study relied on retrospective subjective reports of pain and relief. Pain is a difficult experience to measure in that one person might rate certain stimuli as “very painful,” while another person would rate the same stimuli as “mildly painful.” Future research utilizing multiple methods of assessment, including the use of psychophysiological measures, ecological momentary assessment data (Nock et al., 2009), and objective pain tolerance may lead to a more comprehensive understanding of the processes involved with DSH.
With regards to strengths, the current study may contribute to a novel conceptualization of DSH that extends previous models (e.g., EAM; Chapman et al., 2006) and makes new predictions about changes in response to DSH with repetition. Further, given that our results suggest that the affective and physical pain experiences of DSH may operate via different processes and mechanisms, examination of other cognitive and sensory processes could be useful. One candidate process is dissociation, which has been found to be associated with increased frequency of DSH (Foote, Smolin, Neft, & Lipschitz, 2008) and could be associated with altered pain perception. The inclusion of the number of episodes in an explanatory model of DSH may offer new insight into the mechanism through which DSH becomes reinforcing and habit-forming for individuals who exhibit difficulties in regulating intense negative emotions. Finally, the use of a sample that includes both clinical and nonclinical participants may serve to increase the generalizability of our findings through the examination of the variables of interest across a continuum of pathology.
In conclusion, we present data that supports the prediction by the interpersonal theory of suicidal behavior that DSH becomes more reinforcing with repetition (Joiner, 2005). Clinically, our findings suggest the importance of teaching effective emotion regulatory skills to individuals who engage in DSH, such as the skills that are included in Dialectical Behavior Therapy (Linehan, 1993). Because DSH may fulfill an important function for some individuals by providing a sense of relief and soothing feelings, it is important for clinicians to convey to their clients that they understand why they engage in the behavior, but that other, less maladaptive options could serve the same function. Scientifically, these findings suggest that there may be a potentially important role for opponent process theory in maladaptive emotion regulatory behaviors that warrants further investigation.
Appendix


Footnotes
Identical analyses were conducted with values fenced in to within two standard deviations of their respective means. The observed pattern of results was replicated for all four hypotheses, suggesting that outliers were not responsible for the observed pattern of results.
References
- Bohus M, Limberger M, Ebner, et al. Pain perception during self-reported distress andcalmness in patients with borderline personality disorder and self-mutilating behavior. Psychiatry Research. 2000;95(3):251–260. doi: 10.1016/s0165-1781(00)00179-7. [DOI] [PubMed] [Google Scholar]
- Brain KL, Haines J, Williams CL. The psychophysiology of self-mutilation:Evidence of tension reduction. Archives of Suicide Research. 1998;4:227–242. [Google Scholar]
- Brain KL, Haines J, Williams CL. The psychophysiology of repetitive self mutilation. Archives of Suicide Research. 2002;6:199–210. [Google Scholar]
- Brown MZ, Comtois KA, Linehan MM. Reasons for suicide attempts and nonsuicidal self-injury in women with borderline personality disorder. Journal of Abnormal Psychology. 2002;111:198–202. doi: 10.1037//0021-843x.111.1.198. [DOI] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, Brown MZ. Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behaviour Research and Therapy. 2006;44:371–394. doi: 10.1016/j.brat.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Claes L, Muehlenkamp J, Vandereycken W, Hamelinck L, Martens H, Claes S. Comparison of non-suicidal self-injurious behavior and suicide attempts in patients admitted to a psychiatric crisis unit. Personality and Individual Differences. 2010;48:83–87. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-Patient Edition (SCID-I/NP) Biometrics Research Department, New York State Psychiatric Institute; New York: 1997. [Google Scholar]
- Foote B, Smolin Y, Neft DI, Lipschitz D. Dissociative disorders and suicidality in psychiatric outpatients. Journal of Nervous and Mental Disease. 2008;196:29–36. doi: 10.1097/NMD.0b013e31815fa4e7. [DOI] [PubMed] [Google Scholar]
- Graff H, Mallin R. The syndrome of the wrist cutter. American Journal of Psychiatry. 1967;124:36–42. doi: 10.1176/ajp.124.1.36. [DOI] [PubMed] [Google Scholar]
- Haines J, Williams CL, Brain KL, et al. The psychophysiology of self-mutilation. Journal of Abnormal Psychology. 1995;104:471–489. doi: 10.1037//0021-843x.104.3.471. [DOI] [PubMed] [Google Scholar]
- Joiner T. Why People Die By Suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Kemperman I, Russ MJ, Shearin E. Self-injurious behavior and mood regulation in borderline patients. Journal of Personality Disorders. 1997;11(2):146–157. doi: 10.1521/pedi.1997.11.2.146. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York: Guilford; 1993. [Google Scholar]
- Linehan MM, Comtois K. Lifetime Parasuicide History. University of Washington; Seattle, WA: 1996. Unpublished work. [Google Scholar]
- Muehlenkamp JJ, Engel SC, Wadeson A, et al. Emotional state preceding and following acts of non-suicidal self-injury in bulimia nervosa patients. Behavior Research and Therapy. 2009;47:83–87. doi: 10.1016/j.brat.2008.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muehlenkamp JJ. Self-injurious behavior as a separate clinical syndrome. American Journal of Orthopsychiatry. 2005;75:324–333. doi: 10.1037/0002-9432.75.2.324. [DOI] [PubMed] [Google Scholar]
- Nock MK. Why Do People Hurt Themselves?: New Insights Into the Nature and Functions of Self-Injury. Current Directions in Psychological Science. 2009;18:78–83. doi: 10.1111/j.1467-8721.2009.01613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock M, Joiner T, Gordon K, et al. Non-suicidal self-injury among adolescents: Diagnostic correlates and relation to suicide attempts. Psychiatry Research. 2006;144:65–72. doi: 10.1016/j.psychres.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ. A functional approach to the assessment of self-mutilation. Journal of Consulting and Clinical Psychology. 2004;72:885–890. doi: 10.1037/0022-006X.72.5.885. [DOI] [PubMed] [Google Scholar]
- Nock MK, Prinstein MP, Sterba SK. Revealing the form and function of self-injurious thoughts and behaviors: A real-time ecological assessment study among adolescents and young adults. Journal of Abnormal Psychology. 2009;118:816–827. doi: 10.1037/a0016948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orbach I, Mikulincer M, King R, Cohen D, Stein D. Thresholds and tolerance of physical pain in suicidal and nonsuicidal adolescents. Journal of Consulting and Clinical Psychology. 1997;65(4):646–652. doi: 10.1037//0022-006x.65.4.646. [DOI] [PubMed] [Google Scholar]
- Orbach I, Stein D, Palgi Y, et al. Perception of physical pain in accident and suicide attempt patients: self-preservation vs. self-destruction. J Psychiatry Research. 1996;30(4):307–320. doi: 10.1016/0022-3956(96)00008-8. [DOI] [PubMed] [Google Scholar]
- Pattison EM, Kahan J. The deliberate self-harm syndrome. American Journal of Psychiatry. 1983;140:867–872. doi: 10.1176/ajp.140.7.867. [DOI] [PubMed] [Google Scholar]
- Russ MJ, Campbell SS, Kakuma T, et al. EEG theta activity and pain insensitivity in self-injurious borderline patients. Psychiatry Research. 1999;89:201–214. doi: 10.1016/s0165-1781(99)00113-4. [DOI] [PubMed] [Google Scholar]
- Selby EA, Anestis MD, Joiner TE. Understanding the relationship between emotional and behavioral dysregulation: Emotional Cascades. Behaviour Research and Therapy. 2008;46:593–611. doi: 10.1016/j.brat.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Solomon RL. The opponent-process theory of acquired motivation: The costs of pleasure and the benefits of pain. American Psychologist. 1980;35:691–712. doi: 10.1037//0003-066x.35.8.691. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The Interpersonal Theory of Suicide. Psychological Review. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Welch SS, Linehan MM, Sylvers P, et al. Emotional responses to self-injury imagery among adults with borderline personality disorder. Journal of Consulting and Clinical Psychology. 2008;76:45–51. doi: 10.1037/0022-006X.76.1.45. [DOI] [PubMed] [Google Scholar]
- Witte TK, Timmons KA, Fink E, et al. Do major depressive disorder and dysthymic disorder confer differential risk for suicide? Journal of Affective Disorders. 2009;115:69–78. doi: 10.1016/j.jad.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]


