Abstract
Objectives
Neck and shoulder pain are common but underreported by older people, raising important questions of frequency, medical comorbidities, gender and racial disparities and functional impact associated with neck and shoulder symptoms in elders, which we examined in this analysis.
Methods
We performed a cross-sectional analysis in the community-based Johnston County Osteoarthritis Project, a cohort that is representative of the U.S. population, utilizing data from 1672 participants with a mean age of 68 years; 69% were white and 68% were women. Trained staff obtained data on participant-reported: symptoms, comorbidities, depression, and functional status; and performance-based functional assessments. Regression models of neck and shoulder symptoms and functional measures were adjusted for age, sex, race, and body mass index, and additionally for other joint symptoms and comorbidities.
Results
Symptoms of neck (8%), shoulder (13%) or both (13%) were reported by participants. Neck symptoms were most frequently reported by White women; shoulder symptoms were evenly distributed among race and gender subgroups. Neck and shoulder symptoms were associated with cancer, diabetes mellitus, depression, and lung, cardiovascular, and other musculoskeletal problems, as well as pain, aching or stiffness at other sites, and independently with self-reported and performance –based functional measures.
Conclusions
These findings suggest that primary health care providers should inquire about neck and shoulder symptoms and address potential underlying causes to improve functional status and decrease disability in older people.
Keywords: Neck and shoulder symptoms, musculoskeletal pain, functional status, disability
INTRODUCTION
Half of U.S. adults (approximately 127 million people) reported a musculoskeletal medical condition in the 2012 National Health Interview Survey (NHIS).(1) Data from the Agency for Healthcare Research and Quality Medical Expenditures Panel survey indicate a 117% increase in annual aggregate total cost related to musculoskeletal disease over 15 years, to nearly $800 billion in 2011 dollars.(1) As a result, there has been a research focus on knee, hip, and lower back pain; however, neck and shoulder pain have been left relatively unexamined despite their relatively high prevalence in the general population based on systematic reviews (Point prevalence for neck pain 6–22%, for shoulder 7–27%; Lifetime prevalence for neck pain 14–71%, for shoulder 7–67%).(2, 3) Leijon et al., showed that the overall prevalence of nonspecific neck-shoulder-arm pain increased in the general population from 1990 to 2006, suggesting that this may soon become one of the most common origins of musculoskeletal complaints.(4) This finding is concerning because neck and shoulder pain can have a significant impact on quality of life in the adult population.(5–9) Myofascial pain and fibromyalgia, which commonly affect the upper extremity (10) and may contribute to neck and shoulder symptoms, are also very prevalent in the population, affecting around 2% of adults in the U.S. or about 4 million people, based on 2012 NHIS data.(11)
Older individuals are particularly affected, with an estimated 80% of the population having some form of musculoskeletal complaint by the age of 65 years; and neck and shoulder pain account for a greater proportion of this each year.(4, 12) This may be even more concerning to the female population in which neck and shoulder pain is shown to be most prevalent.(9, 13) In addition, there may be variations in the prevalence of shoulder and neck pain depending on race/ethnicity. Three distinct surveys, spanning various age groups, found that neck pain is more prevalent in the white population (9, 13, 14), although shoulder pain has received less study. Thus, a better understanding of which populations are most affected by neck and shoulder pain is needed.
An improved understanding of the determinants and comorbidities that are associated with neck and shoulder pain would help providers consider, diagnose, and treat these symptoms. However, there have been few studies looking at this, and only a single study has used a cohort within the United States.(3, 6, 8, 9, 15) In Finland, neck and shoulder pain were shown to be associated with mental disorders, low back pain, and osteoarthritis of knee, hip and hand in the Finns 30 years or older.(8, 15) In the United States, Vogt et al reported similar findings in an older population [70 to 79 year-old men and women], in addition to showing associations between neck and shoulder pain and poorer self-rated health, depressive symptoms, and a medical history of heart attack, angina, and arthritis.(9) There are a variety of potential etiologies for neck and shoulder symptoms, including traumatic or arthritic disorders, neurologic and vascular conditions, and myofascial pain syndromes which may be primary or overlay one or more other sources of pain.(10)
This retrospective cross-sectional analysis of neck and shoulder symptoms uses data from the Johnson County Osteoarthritis Project [JoCo OA], which includes white and African American [AA] men and women with an average age of 68 years living in a single county in North Carolina. The purpose of this study was to answer important questions regarding the frequency and functional impact of such symptoms in these demographic groups, and to identify potentially novel associations with specific comorbidities to inform identification for potential intervention in clinical practice and rehabilitation.
METHODS
Participants
Data were collected from a community-based cohort of non-institutionalized white and AA men and women aged 45 years and older with and without osteoarthritis enrolled in the JoCo OA, a sample that has been previously described in detail.(16) For the current analysis, we used cross-sectional data from the second follow-up time point of the JoCo OA, collected from 2006–2010 [n= 1697]. All participants signed informed consent and participated in two home interviews administered by trained staff and one clinic visit, where radiographs were taken and trained study personnel administered a physical examination and functional measures. The JoCo OA has been continuously approved by the Institutional Review Boards of the University of North Carolina at Chapel Hill and the Centers for Disease Control and Prevention.
Symptoms
Neck and shoulder symptoms were separately assessed based on answers to the questions, “On MOST days do you have pain, aching, or stiffness of your neck/left or right shoulders?”. Those participants answering in the affirmative were then asked to rate their symptoms as mild, moderate, or severe for each site. Similar symptoms questions were also asked for the feet, knees, hips, and hands, and for the mid- and low back; axial symptoms were considered present with an affirmative response, and symptoms at a specific appendicular site if present in either right or left sides.
Additional Clinical Covariates
Body mass index [BMI] was calculated in kg/m2 from height [cm] and weight [kg] measured during the physical examination, while age, gender, and race were self-reported. Self-reported medical conditions included bronchitis, emphysema, lung trouble, stroke, heart trouble, circulation problems, fibrositis, gout, tendonitis, cancer, and diabetes mellitus (DM), adapted from the National Health Interview Survey.(17) Lung problems [bronchitis, emphysema, lung trouble], cardiovascular problems [stroke, heart trouble, circulation problems] and musculoskeletal problems [fibrositis, gout, tendonitis] were consolidated into dichotomous variables for data analysis. Depressive symptoms were evaluated using the validated Center for Epidemiologic Study Depression Scale [CES-D].(18) The CES-D consists of 20 questions, with each question scored on a scale from 0–3, with a possible range of 0–60; higher scores indicate an increased number of depressive symptoms. The average score for the general population has been reported as 9.1±8.6.(19) This study utilized the commonly used score of 16 or greater as a cutoff for depressive symptoms.(20)
Outcomes: Disabilities and Functional Status
The Disability of Arm, Shoulder and Hand [DASH] questionnaire was used to assess patient perceived disability of the upper extremity over the prior week.(21) This consists of 30 questions: 21 on physical function, 5 on symptoms, and one each related to social role function, work, sleep, and confidence. DASH is scored on a scale of 0 to 100, with higher scores correlating with greater perceived disability. The average score in the general population has been reported as 10.1 ± 14.7.(22)
The Stanford Health Assessment Questionnaire Disability Index [HAQ] was used for self-reported functional status assessment. This questionnaire consists of 20 items addressing activities of daily living categorized across eight domains [dressing, arising, eating, walking, reaching, gripping, chores and hygiene] in order to assess disability over the past week.(23) Each activity was scored on a scale from 0 to 3 [0 – with no difficulty, 1 – with little difficulty, 2 – with much difficulty, and 3 - unable to perform]. The maximum scores from each domain were then averaged together to produce the final HAQ score [0–3], with higher scores corresponding to a greater degree of disability.
Grip and pinch strength were measured in kilograms for both hands using the Jamar Hydraulic Hand Dynamometer and the Jamar Hydraulic Pinch Gauge, respectively [Bolingbrook, IL]. Three trials were conducted for pinch and grip strength measurements, and an average of the three trials was used for analysis.
Functional reach was measured using a meter stick mounted to a wall.(24) Participants were asked to stand with their dominant side beside the wall and extend their dominant arm along the meter stick. Normal arm length was measured to the third metacarpal. Participants were then asked to reach forward to their maximum capacity without taking a step and the farthest point of reach was measured to the third metacarpal. Each participant was given two practice trials and the subsequent 3rd trial was recorded. Functional reach was calculated from the difference between normal arm length and maximum reach in centimeters. In healthy volunteers, functional reach measurements lessen with age, with a mean of 38–43 cm among 20–40 year olds, decreasing to 25–33 cm in 70–87 year old participants.(24)
A “back scratch” measure was assessed as another measure of shoulder range of motion and function.(25) Participants were asked to reach over the right shoulder with the right hand, and reach with the left hand up the middle of the back, in an attempt to touch the fingers together, and then repeat on the other side. The distance between the extended middle fingers was measured in centimeters. This test was categorized into quintiles based on the distribution of the measurements: Q1) overlapping fingers [best], Q2) 0–20cm, Q3) 20–40cm, Q4) greater than 40cm, or Q5) unable to do [worst].
Statistical Methods
Separate analyses were carried out for neck and shoulder symptoms. Participants were categorized into three groups by self-reported symptom status: no symptoms, mild symptoms, or moderate to severe symptoms on most days. The moderate and severe groups were combined for analysis due to small numbers in the severe group (n=42 for neck and n=46 for shoulder symptoms, or ~3% of participants).
Descriptive statistics were calculated for the whole sample and by race and gender. Measures of central location and dispersion were computed for continuous data. Frequency distributions were determined for categorical variables. Cochran–Mantel–Haenszel statistics for categorical variables and linear regression testing of trend for continuous variables were used to compare all demographic and clinical characteristics [age, BMI, gender, race, medical conditions, and CES-D Scale] among the three symptoms groups for neck and shoulder separately.
In order to determine the impact of each self-reported medical condition on neck and shoulder symptom presence and severity, a logistic regression model was fit where each medical condition was treated as an independent variable and the neck or shoulder symptom severity as the dependent variable, controlling for age, BMI, gender, and race. Models were then also adjusted for all other comorbidities and CES-D to determine the independent impact of each condition. Adjusted odds ratios were produced for comparing the effect of each medical condition on the likelihood of having mild neck and shoulder symptoms versus no symptoms, and the likelihood of having moderate or severe neck and shoulder symptoms versus no symptoms.
To examine associations between the neck and shoulder symptoms groups (independent variables) and the presence of joint symptoms at other sites, such as foot, knee, hip, hand, mid-back, and lower back (yes/no, dependent variables), separate logistic regression models for neck and shoulder symptoms were used to determine the unadjusted odds ratios and adjusted odds ratios for symptoms at other sites, controlling for age, BMI, gender, and race. Models were then additionally adjusted for all comorbidities and for CES-D.
For continuous outcomes of functional impact [DASH, HAQ, pinch strength, grip strength, and functional reach scores], the statistical significance of differences between the symptoms groups was assessed using general linear regression models, with neck or shoulder symptoms as independent variables and each outcome of functional impact as the dependent variable. Multiple linear regression was used for each of the continuous outcomes to adjust for potential confounders such as age, BMI, gender, and race, and additionally for symptoms at other joint sites. The “back scratch” measure was analyzed categorically in 5 levels, and a polytomous logistic regression model with proportional odds [where the proportional odds assumption was met] and generalized logit model [where the proportional odds assumption was violated] was fit.
Interactions among the covariates and variables of interest included in the model were tested jointly in each model. In models with significant interactions [P-values <0.1], appropriate sub-groups were examined, and point estimates and 95% confidence intervals were calculated separately for each sub-group. All statistical computations were performed using SAS Version 9.3 software [SAS Institute, Cary, NC].
RESULTS
Of the 1697 participants with available clinic data at the second follow-up time point, 1638 had complete data for neck and 1672 for shoulder symptoms analyses [2 were excluded for missing/implausible BMI, 57 for missing neck symptoms and 23 for missing shoulder symptoms data, Figure].
Figure.
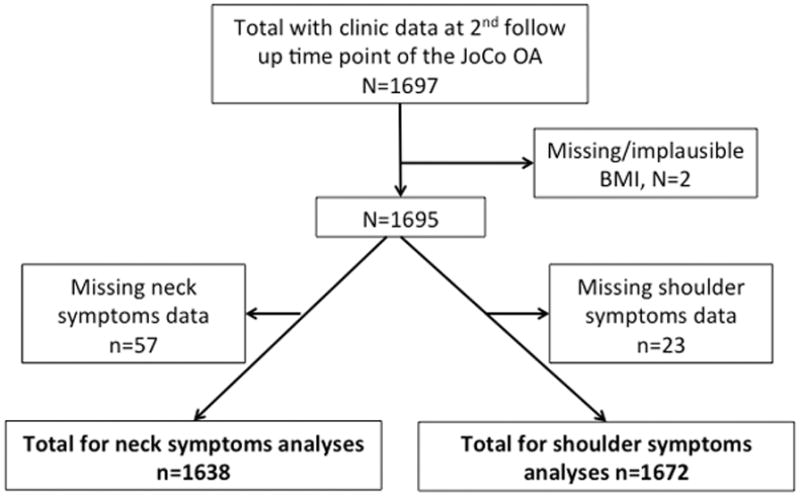
Description of the included study sample
The participants were 32.5 % men, 31.3 % African American, with an average age of 68.0 ± 9.1 years, and average BMI of 31.5 ± 7.2 kg/m2 [Table 1].
Table 1.
Sample characteristics
| Sample Characteristics | Overall (n=1672) | Any neck symptoms* (n=341) | Any shoulder symptoms* (n=419) |
|---|---|---|---|
| Age, mean (SD) years | 68.0(9.1) | 67.7(8.9) | 68.2(9.0) |
| BMI, mean (SD) kg/m2 | 31.5(7.2) | 32.5(7.4) | 32.5(7.7) |
| Male n (%) | 543(32.5) | 86(25.2) | 128(30.6) |
| African American n (%) | 523(31.3) | 85(24.9) | 130(31.0) |
| Lung problems† n (%) | 323(19.7) | 112(34.0) | 123(30.1) |
| Cardiovascular problems† n (%) | 652(39.8) | 159(48.3) | 201(49.1) |
| Cancer n (%) | 297(18.1) | 76(23.1) | 87(21.3) |
| Other MSK problems† n (%) | 585(35.7) | 177(53.8) | 212(51.8) |
| Diabetes n (%) | 393(24.0) | 91(27.7) | 133(32.5) |
| Depression† n (%) | 188(11.5) | 71(20.9) | 94(22.8) |
| Symptoms at other sites‡ n (%) | 1134(71.6) | 318(93.3) | 388(93.7) |
| DASH, mean (SD) | 13.8(17.1) | 27.2(19.8) | 12.7(19.5) |
| HAQ, mean (SD) | 1.2(1.0) | 1.8(1.0) | 1.8(1.0) |
| Grip strength, mean (SD) kg | 26.9(11.5) | 24.2(11.1) | 24.9(11.5) |
| Pinch strength, mean (SD) kg | 7.4(7.4) | 6.7(6.9) | 7.0(7.8) |
| Functional reach, mean (SD) cm | 29.4(9.3) | 27.8(9.2) | 26.3(10.0) |
| “Back scratch” worst 2§ (%) | 390(23.3) | 112(32.8) | 166(39.6) |
Presence of symptoms of any severity (mild, moderate, or severe)
Lung Problems (bronchiti s, emphysema, and lung trouble); Cardiovascular Problems (stroke, heart attack, heart trouble, circulation problems); Other MSK Problems (fibrositis, gout, tendonitis); Depression (CES-D ≥ 16)
Pain, aching or stiffness reported in foot, knee, hip, hand, mid-back, and/or lower back
“Back scratch” worst 2 categories: >40cm between fingers or unable to perform the test.
BMI=body mass index; MSK=musculoskeletal; DASH=Disability of the Arm, Shoulder, and Hand; HAQ=Health Assessment Questionnaire; n for neck symptoms=1638; n for shoulder symptoms=1672.
Those with neck symptoms, in particular, were less likely to be male or African American compared with the overall sample. Individuals reporting neck or shoulder symptoms were more likely to have lung, cardiovascular, and other musculoskeletal comorbidities as well as diabetes, depression, and symptoms at other joint sites [Table 1]. There were no significant interactions in any model.
Prevalence of Neck and shoulder Symptoms
Shoulder symptoms without neck symptoms were reported by 12.8% of participants, while 8.2% reported neck symptoms without shoulder symptoms, and 12.6% reported symptoms in both sites. Of those reporting neck symptoms (n=341), these were mild in 154 (45%), moderate in 145 (43%) and severe in 42 (12%). Of those with shoulder symptoms (n=419), these were mild in 189 (45%), moderate in 184 (44%), and severe in 46 (11%). Due to small numbers in the severe category, moderate and severe symptoms were combined for analysis. The prevalence of neck and shoulder symptoms by race and gender is shown in table 2.
Table 2.
Percentages (95% confidence intervals) of neck, shoulder, and the combination of neck and shoulder symptoms in the sample
| Neck Symptoms | Any Symptoms* (n=341) | p value† | Moderate/Severe Symptoms (n=187) | p value† |
|---|---|---|---|---|
| AA men (n=140) | 17.1 (11.0, 23.3) | <.001 | 8.6 (3.9, 13.2) | .001 |
| AA women (n=370) | 16.5 (12.7, 20.3) | 9.2 (6.3, 12.1) | ||
| White men (n=396) | 15.7 (12.1, 19.2) | 8.1 (5.4, 10.8) | ||
| White women (n=732) | 26.5 (23.3, 29.7) | 14.9 (12.4, 17.5) | ||
| Total (n=1638) | 20.8 (18.9, 22.8) | 11.4 (9.9, 12.9) |
| Shoulder Symptoms | Any Symptoms* (n=419) | p value† | Moderate/Severe Symptoms (n=230) | p value† |
|---|---|---|---|---|
| AA men (n=143) | 24.5 (17.4, 31.5) | .749 | 13.3 (7.7, 18.9) | .374 |
| AA women (n=380) | 25.0 (21.7, 29.3) | 14.2 (10.7, 17.7) | ||
| White men (n=400) | 23.3 (19.1, 27.4) | 11.3 (8.2, 14.4) | ||
| White women (n=749) | 26.2 (23.0, 29.3) | 15.0 (12.4, 17.5) | ||
| Total (n=1672) | 25.1 (23.0, 27.1) | 13.8 (12.1, 15.4) |
| Both Neck and Shoulder | Any Symptoms* (n=206) | p value† | Moderate/Severe Symptoms (n=105) | p value† |
|---|---|---|---|---|
| AA men (n=143) | 9.8 (4.9, 14.7) | .001 | 2.8 (0.1, 5.5) | .004 |
| AA women (n=380) | 10.3 (7.2, 13.3) | 5.5 (3.2, 7.8) | ||
| White men (n=400) | 8.5 (5.8, 11.2) | 4.0 (2.1, 5.9) | ||
| White women (n=749) | 15.9 (13.3, 18.5) | 8.5 (6.5, 10.6) | ||
| Total (n=1672) | 12.3 (10.7, 13.9) | 6.3 (5.1, 7.4) |
Any symptoms=presence of symptoms of any severity (mild, moderate, or severe)
p-value is for the overall comparison of the distribution of neck and shoulder pain among the subgroups.
n for neck symptoms=1638; n for shoulder symptoms=1672
Neck symptoms of any severity were most prevalent among white women [26.5%], with significant differences by race and gender [P≤0.001]. Shoulder symptoms were also most prevalent in white women [26.2%]; however, a more even distribution was seen by race and gender without significant differences [P>0.05]. The presence of both neck and shoulder symptoms was reported by 9–16% of the sample, again most frequently among white women [P=0.001]. Moderate to severe symptoms in both the neck and shoulder were reported by 3–4% of men and 6–9% of women [Table 2].
Medical comorbidities of participants by neck or shoulder symptoms
Increasing severity of neck and shoulder symptoms was associated with the presence of lung or musculoskeletal problems, cancer, and depressive symptoms [Table 3].
Table 3.
Medical comorbidities by neck and shoulder symptoms
| NECK | SHOULDER | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| None (n=1297) | Mild (n=154) | Mod/Severe (n=187) | None (n=1253) | Mild (n=189) | Mod/Severe (n=230) | |
| Lung Problems (%) | 16.1 | 28.8 | 38.3 | 16.3 | 21.3 | 37.2 |
| OR* | referent | 2.0 (1.3, 2.9) | 3.0 (2.1, 4.1) | referent | 1.3 (0.9, 2.0) | 2.9 (2.1, 3.9) |
| OR† | referent | 1.6 (1.1, 2.4) | 2.4 (1.7, 3.4) | referent | 1.1 (0.7, 1.6) | 2.1 (1.5, 3.0) |
| Cardiovascular Problems (%) | 37.7 | 52.1 | 45.4 | 36.6 | 42.1 | 54.9 |
| OR* | referent | 1.8 (1.3, 2.7) | 1.5 (1.1, 2.0) | referent | 1.2 (0.9, 1.7) | 2.2 (1.6, 3.0) |
| OR† | referent | 1.6 (1.1, 2.3) | 1.2 (0.8, 1.7) | referent | 1.0 (0.7, 1.4) | 1.8 (1.3, 2.5) |
| Cancer (%) | 16.8 | 21.2 | 24.6 | 17.1 | 19.7 | 22.6 |
| OR* | referent | 1.3 (0.8, 2.0) | 1.6 (1.1, 2.3) | referent | 1.1 (0.8, 1.7) | 1.4 (1.0, 2.0) |
| OR† | referent | 1.3 (0.8, 1.9) | 1.5 (1.0, 2.2) | referent | 1.2 (0.8, 1.7) | 1.3 (0.9, 1.9) |
| Musculoskeletal Problems (%) | 31.1 | 52.1 | 55.2 | 30.3 | 46.5 | 56.2 |
| OR* | referent | 2.4 (1.7, 3.4) | 2.7 (1.9, 3.7) | referent | 1.2 (0.9, 1.7) | 2.2 (1.6, 3.0) |
| OR† | referent | 2.1 (1.5, 3.0) | 2.4 (1.7, 3.3) | referent | 1.8 (1.3, 2.5) | 2.5 (1.8, 3.3) |
| Diabetes Mellitus (%) | 23.0 | 31.5 | 24.6 | 21.1 | 34.4 | 31.0 |
| OR* | referent | 1.6 (1.1, 2.3) | 1.0 (0.7, 1.5) | referent | 1.9 (1.3, 2.7) | 1.6 (1.1, 2.2) |
| OR† | referent | 1.3 (0.9, 1.9) | 0.8 (0.6, 1.3) | referent | 1.7 (1.2, 2.5) | 1.2 (0.9, 1.8) |
|
| ||||||
| Depression (CESD ≥16, %) | 9.1 | 12.4 | 28.0 | 7.7 | 20.3 | 24.9 |
| OR* | referent | 1.4 (0.9, 2.4) | 3.9 (2.6, 5.7) | referent | 3.2 (2.1, 4.9) | 4.0 (2.7, 5.8) |
| OR† | referent | 1.1 (0.6, 1.9) | 3.3 (2.2, 4.9) | referent | 2.8 (1.8, 4.3) | 3.3 (2.2, 4.9) |
Odds ratios adjusted for age, BMI, gender, race, where the medical condition is the independent variable and neck/shoulder symptoms are the dependent (outcome) variable
Odds ratios adjusted for age, BMI, gender, race, all other medical comorbidities, and CES-D.
For lung (bronchitis, emphysema, and lung trouble), cardiovascular (stroke, heart attack, heart trouble, circulation problems), and other musculoskeletal (fibrositis, gout, tendonitis) comorbidities, n=1640; diabetes, n=1639; CESD, n=1636; n for neck symptoms=1638; n for shoulder symptoms=1672
Lung problems were associated with 2–3 times higher odds of mild or moderate to severe neck symptoms, and twice the odds of moderate to severe shoulder symptoms, independent of other comorbidities. Cardiovascular problems were independently associated with 60% higher odds of mild neck symptoms, and nearly twice the odds of moderate to severe shoulder symptoms. Cancer increased the odds of moderate to severe neck symptoms by 50%, but was not independently associated with shoulder symptoms. The presence of other musculoskeletal problems (fibrositis, gout, tendonitis) resulted in twice the odds of neck or shoulder symptoms independent of other comorbidities. The association between DM and neck pain was not statistically significant after full adjustment; there was a 70% increase in the odds of mild but not moderate to severe shoulder symptoms. Depression resulted in 3–4 times the odds of moderate to severe neck or shoulder symptoms, independent of other covariates [Table 3].
Symptoms at Other Sites
All severity levels [mild or moderate to severe] of neck and shoulder symptoms were associated with musculoskeletal symptoms [pain, aching, or stiffness] at other joint sites [Table 4].
Table 4.
Adjusted Odds Ratios* (95% Confidence Interval) for associations between neck (top) or shoulder (bottom) symptoms and symptoms at other joint sites
| Symptoms at other sites | n(%) | Mild neck symptoms OR (95% CI)† |
Moderate/severe neck symptoms OR (95% CI)† |
|---|---|---|---|
| Shoulder | 415 (25.3) | 5.1 (3.6. 7.3) | 12.1 (8.5,17.2) |
| Foot | 357 (24.2) | 2.1 (1.4. 3.0) | 3.8 (2.7, 5.3) |
| Knee | 645 (39.4) | 2.3 (1.6. 3.3) | 3.4 (2.4, 4.7) |
| Hip | 483 (29.5) | 3.4 (2.4. 4.8) | 6.1 (4.4, 8.5) |
| Hand | 600 (36.6) | 3.6 (2.5. 5.1) | 6.0 (4.3, 8.5) |
| Mid-back | 190 (12.9) | 3.5 (2.3. 5.4) | 6.6 (4.5, 9.6) |
| Low-back | 603 (40.9) | 5.4 (3.7. 7.9) | 6.6 (4.6, 9.4) |
|
| |||
| n (%) |
Mild shoulder symptoms OR (95% CI) |
Moderate/severe shoulder symptoms OR (95% CI) |
|
| Neck | 341 (20.8) | 5.8 (4.1. 8.2) | 10.4 (7.6,14.4) |
| Foot | 357 (24.2) | 2.7 (1.9. 3.9) | 3.8 (2.8, 5.2) |
| Knee | 656 (39.2) | 2.8 (2.1. 3.9) | 3.5 (2.5, 4.7) |
| Hip | 496 (29.7) | 3.5 (2.5. 4.8) | 5.0 (3.7, 6.7) |
| Hand | 608 (36.4) | 3.6 (2.6. 5.0) | 5.2 (3.8, 7.0) |
| Mid-back | 190 (12.9) | 5.2 (3.4. 8.0) | 6.9 (4.8,10.1) |
| Low-back | 603 (40.9) | 3.3 (2.3. 4.5) | 5.1 (3.7, 7.1) |
Odds ratios adjusted for age, BMI, gender, race, where neck/shoulder symptoms are the independent variables and other body sites symptoms are the dependent (outcome) variables; all associations are statistically significant
The reference group is those without symptoms
For shoulder, knee, hip, and hand n=1672; for foot, mid and low back, n=1473; for neck n=1638
Specifically, participants with moderate or severe neck symptoms had more than twelve times the odds of reporting shoulder symptoms, three to four times the odds of reporting foot or knee symptoms, and six times the odds of reporting hip, hand, mid-back or lower back symptoms. Participants with moderate or severe shoulder symptoms had ten times the odds of reporting neck symptoms, three to four times the odds of reporting foot or knee symptoms, five times the odds of reporting hip, hand or lower back symptoms, and seven times the odds of reporting mid-back symptoms.
Disability and Functional Measures
Increasing severity of neck and shoulder symptoms was independently associated with increased perception of disability as measured by the DASH and HAQ [Table 5].
Table 5.
Measured outcome scores by symptomatic group
| Outcome score | No neck symptoms (n=1297) | Mild neck symptoms (n=154) | Moderate/severe neck symptoms (n=187) | No shoulder symptoms (n=1253) | Mild shoulder symptoms (n=189) | Moderate/severe shoulder symptoms (n=230) |
|---|---|---|---|---|---|---|
| DASH | 10.9 (14.9) | 22.4 (17.6)*† | 31.0 (20.7)* † | 9.2 (13.3) | 21.3 (16.5)* † | 35.2 (19.7)* † |
| HAQ | 1.0 (1.0) | 1.7 (1.0)* † | 2.0 (0.9)* † | 0.9 (1.0) | 1.6 (1.0)* † | 2.1 (0.9)* † |
| Grip (kg) | 27.5 (11.3) | 24.6 (10.6) | 23.8 (11.6) | 27.5 (11.5) | 25.5 (10.3) | 24.4 (12.5) |
| Pinch (kg) | 7.6 (7.6) | 6.7 (6.1)* | 6.6 (7.6)* | 7.5 (7.3) | 7.1 (7.9)* | 6.9 (7.7)* |
| Functional reach (cm) | 29.8 (9.4) | 28.7 (9.4) | 27.1 (8.9)* | 30.3 (8.9) | 26.9 (10.2)* | 25.9 (9.8)* † |
P-value<0.05 compared to no symptoms for this outcome, adjusting for age, BMI, gender, and race (neck/shoulder symptoms were the independent variables while functional scores were the dependent (outcome) variables)
P-value<0.05 compared to no symptoms for this outcome, adjusting for age, BMI, gender, race and symptoms at other sites (foot, knee, hip, hand, mid-back, low-back)
For DASH n=1241; HAQ n=1671; pinch and grip n=1461; functional reach n=1505; n for neck symptoms=1638; n for shoulder symptoms=1672
Additionally, all levels of neck and shoulder symptoms were associated with decreased grip strength, although this was no longer seen after adjusting for symptoms at other sites. All levels of shoulder symptoms and moderate or severe neck symptoms were associated with decreased functional reach. No statistically significant associations were seen between neck or shoulder symptoms and pinch strength [table 5].
Compared to people with no shoulder symptoms, those with shoulder symptoms had more difficulty in performing the “back scratch” test. For example, the odds of falling into a worse category on this measure increased 2.5 to 14 times for people with moderate to severe shoulder symptoms compared with those with no shoulder symptoms (compared to the referent Q1, for Q2: OR 2.5 [95% CI 0.7–8.3]; Q3: OR 3.2 [95% CI 1.0–10.6]; Q4: OR 8.0 [95% CI 2.3–28.2]; Q5 (unable): OR 14.3 [95% CI 4.2–48.6]).
DISCUSSION
Our study found that neck and shoulder symptoms are common in the JoCo OA, a cohort that is reflective of the general U.S. population, particularly among white women. In addition, we identified significant associations between neck and shoulder symptoms and several medical conditions including DM, cardiovascular and lung problems, depressive symptoms, cancer, and musculoskeletal problems. Finally, neck and shoulder symptoms were associated with musculoskeletal symptoms at other sites, increased disability, and decreased functional ability. Therefore, neck and shoulder symptoms are likely to have a clinically significant impact on medical and rehabilitative care of a variety of conditions in older adults.
Neck and Shoulder Symptoms and Diabetes
Several studies have examined the association between diabetes mellitus (DM) and musculoskeletal complaints.(8, 15, 26–31) The majority of these studies have supported an association between DM and musculoskeletal pain, but the strength of this relationship is controversial. Some argue that musculoskeletal pain and DM have a spurious association that can be explained by obesity, a confounding variable that is an established risk factor for DM type II. Others argue that this is a true causal association that results from the accumulation of advanced glycosylation end products [AGEs] in joints,(27, 30) a direct pathologic consequence of DM. Neck and shoulder pain are of particular interest in this debate because they are non-weight bearing regions and thus less susceptible to symptoms caused by increased bearing of weight. To date, several studies have examined this specific association,(8, 15, 26, 28–30) but a consensus has not yet been reached. Cole et al found that greater than 25% of participants from a general Australian population with DM had shoulder pain or stiffness, which were more prevalent in the patient population with DM than in the patient population without DM; however, this was no longer true when the data was adjusted for obesity. On the other hand, the association between shoulder pain and obesity, regardless of DM status, remained statistically significant.(26) In contrast, Molsted et al reported that there was not a highly significant relationship between higher BMI and more severe shoulder or neck pain in an elderly Danish population suggesting that DM may have direct pathologic consequences, regardless of BMI.(28) Furthermore, Makela et al only found a weak association between obesity and neck pain, suggesting that there is an indirect association with an unidentified casual factor such as DM.(15) We found higher proportions of individuals self-reporting DM in the groups with neck or shoulder symptoms than in those without. This association remained significant for mild neck symptoms and all levels of shoulder symptoms after adjustment for age, BMI, gender, and race. However, when adjusted for all other medical comorbidities (lung or cardiovascular problems, cancer, musculoskeletal problems) and depression, only mild shoulder symptoms had a significant association with diabetes mellitus. Therefore, DM was associated with neck and shoulder symptoms independent of BMI, although with extensive adjustment for comorbidities this relationship was no longer seen, suggesting that there is only a modest association between DM and neck and shoulder symptoms.
Neck and Shoulder Symptoms and Cardiovascular and Pulmonary Disease
Patients with cardiovascular disease [CVD] are more likely than those without to have comorbid musculoskeletal complaints, particularly arthritis,(32) that may limit their cardiac rehabilitation.(33) Several studies have examined the association between CVD and musculoskeletal conditions; however, most have focused on general musculoskeletal pain, lower back pain, or knee pain.(31, 33, 34) Few have focused on the shoulder (9, 30) and only one, to our knowledge, has investigated the association between neck symptoms and CVD.(9) Our data demonstrate a statistically significant association between cardiovascular problems (stroke, heart attack, heart trouble, circulation problems) and mild neck symptoms and moderate to severe shoulder symptoms after adjustment for age, BMI, gender, race, other medical comorbidities, and depression. Similarly, the relationship between lung disease and musculoskeletal complaints has been studied to a limited degree, in spite of the fact that this relationship may increase the burden of disease and the risk for limited activity.(31) The majority of studies performed focused on chronic obstructive pulmonary disease (COPD) and generalized musculoskeletal comorbidities; and although these studies lend strong support for a statistically significant relationship between COPD and musculoskeletal conditions,(35–37) the literature is lacking data on the association between pulmonary disorders and specific neck and shoulder symptoms. We found a statistically significant independent association between lung problems [bronchitis, emphysema, lung trouble] and all levels of neck symptoms, as well as moderate to severe shoulder symptoms. These results suggest that there are clinically relevant associations between heart and lung disease and shoulder and neck symptoms that may limit recommended physical activity and general rehabilitation of affected patients.
Neck and Shoulder Symptoms and Depressive Symptoms
Musculoskeletal complaints and depressive symptoms both contribute to disability and a decreased quality of life; and, unfortunately, both are becoming highly prevalent in older populations worldwide.(38, 39) Several studies have demonstrated that there is a direct relationship between shoulder and neck pain and depressive symptoms.(4, 9, 40–42) Furthermore, Leijon et al showed that, over a 12-year period [1990 to 2002], there was an increase in the prevalence of neck-shoulder-arm pain and concurrent psychological distress in both males and females.(4) Although cross-sectional, our study supports these findings and, additionally, found that the odds of increasing severity of neck and shoulder symptoms increased substantially with scoring greater than 16 on the CESD.
Neck and Shoulder Symptoms, Other Musculoskeletal Disorders, and Cancer
Musculoskeletal disorders (fibromyalgia, myofascial pain, tendonitis, and gout) and cancer are known to be associated with local and generalized musculoskeletal symptoms. The symptoms, particularly pain, associated with these conditions are important because they can decrease quality of life and, in the case of cancer, may even affect a patient’s will to survive.(43, 44) Our study demonstrates that there is a positive correlation between cancer and moderate to severe neck symptoms. In addition, we found that musculoskeletal disorders were positively correlated with all levels of neck symptoms and moderate or severe shoulder symptoms. These associations remained significant after adjustments were made for age, BMI, gender, race, all medical comorbidities, and depression. Thus, both cancer and musculoskeletal disorders have a significant association with musculoskeletal symptoms in the neck and shoulder.
Neck and Shoulder Symptoms and Musculoskeletal Symptoms at Other Sites
This study demonstrates that both neck and shoulder symptoms are strongly associated with symptoms at other sites. In particular, the presence of moderate or severe neck symptoms is associated with twelve times the odds of reporting shoulder symptoms, and the presence of moderate or severe shoulder symptoms is associated with ten times the odds of reporting neck symptoms. This suggests that patients either have difficulty distinguishing between neck and shoulder symptoms, or the pathology is closely linked.(10) Regardless, these results support previous findings that there is a significant association between neck and shoulder symptoms and other musculoskeletal symptoms, (6, 8, 9, 15) as well as our prior work demonstrating that symptoms, rather than structural disease, are of greatest importance in relation to functional limitation.(45) A study of 440 patients seeking primary care for neck and shoulder pain found that about 25% had additional episodes of care for pain in other body sites, suggestive of a myofascial pain disorder.(46) The upper body is a common site for myofascial pain, and treatment directed at this (such as education, addressing sleep and biomechanical issues, stretching, and aerobic exercise) may be beneficial for such patients.(10)
Neck and Shoulder Symptoms and Functional Measures
Finally, as severity of neck and shoulder pain increases, there is a significant increase in self-reported disability scores [DASH and HAQ] and a significant decrease in performance-based functional ability [as measured by grip strength, functional reach, and “back scratch”]. Even after adjustment for these potential confounders including symptoms at other body sites, we found that neck and shoulder symptoms are independently related to an increase in DASH and HAQ scores, in agreement with prior studies.(6–9, 15) Thus, although symptoms at other sites may partially contribute to disability, neck and shoulder symptoms also have a significant independent role in both self-reported and performance-based functional limitation.
The limitations of this analysis include the age of the cohort which may limit generalizability to younger individuals. A small number of cases reported “severe” symptoms, necessitating combination with the moderate symptoms group. The cross-sectional nature of this work does not allow us to make any temporal or causal inferences regarding the observed associations. Finally, the medical conditions were self-reported, although self-reported medical conditions are highly related to medical record review.(47, 48) In contrast, the strengths of this study include the large sample size, the biracial cohort of both men and women, the community-based nature of this cohort, which is representative of the U.S. population, and perhaps most importantly, consideration of single and joint affection of the neck and shoulder, inclusion of multiple comorbid conditions and joint symptoms in other sites, and assessment of functional impact by self-reported as well as performance-based measures.
In conclusion, neck and shoulder symptoms are highly prevalent and significantly associated with medical comorbidities such as diabetes mellitus, CVD, and lung diseases, and are independently associated with increased disability. Primary health care providers should be aware of these associations in order to better assess and treat such patients, potentially improving functional status and decreasing disablity in older people.
Acknowledgments
Funding for this work was provided in part by NIA 5-T35-AG038047-04 - UNC-CH Summer Research in Aging for Medical Students (ARW, PI:JBW); CDC/ASPH S043 and S3486 (JMJ), NIH/NIAMS MCRC P60 AR49465 (JMJ); NIH/NIAMS K23 AR061406 (AEN).
We would like to thank the participants and staff of the Johnston County Osteoarthritis Project, without whom this work would not be possible.
Footnotes
Sponsor’s role. The sponsors of this work played no role in design, methods, recruitment, data collection, analysis, or manuscript preparation.
Conflict of Interest. The authors have no conflicts to report in relation to this work.
References
- 1.United States Bone and Joint Initiative. The Burden of Musculoskeletal Disease in the United States. 2014 [cited 9/30/2015]; 3rd: Available from: http://www.boneandjointburden.org/2014-report/ib0/prevalence-select-medical-conditions.
- 2.Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J. 2006;15:834–48. doi: 10.1007/s00586-004-0864-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luime JJ, Koes BW, Hendriksen IJ, Burdorf A, Verhagen AP, Miedema HS, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol. 2004;33:73–81. doi: 10.1080/03009740310004667. [DOI] [PubMed] [Google Scholar]
- 4.Leijon O, Wahlstrom J, Mulder M. Prevalence of self-reported neck-shoulder-arm pain and concurrent low back pain or psychological distress: time-trends in a general population, 1990–2006. Spine (Phila Pa 1976) 2009;34:1863–8. doi: 10.1097/BRS.0b013e3181ab3397. [DOI] [PubMed] [Google Scholar]
- 5.Badley EM, Tennant A. Changing profile of joint disorders with age: findings from a postal survey of the population of Calderdale, West Yorkshire, United Kingdom. Ann Rheum Dis. 1992;51:366–71. doi: 10.1136/ard.51.3.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cote P, Cassidy JD, Carroll L. The Saskatchewan Health and Back Pain Survey. The prevalence of neck pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976) 1998;23:1689–98. doi: 10.1097/00007632-199808010-00015. [DOI] [PubMed] [Google Scholar]
- 7.Hartvigsen J, Christensen K, Frederiksen H. Back and neck pain exhibit many common features in old age: a population-based study of 4,486 Danish twins 70–102 years of age. Spine (Phila Pa 1976) 2004;29:576–80. doi: 10.1097/01.brs.0000099394.18994.2f. [DOI] [PubMed] [Google Scholar]
- 8.Makela M, Heliovaara M, Sainio P, Knekt P, Impivaara O, Aromaa A. Shoulder joint impairment among Finns aged 30 years or over: prevalence, risk factors and co-morbidity. Rheumatology (Oxford) 1999;38:656–62. doi: 10.1093/rheumatology/38.7.656. [DOI] [PubMed] [Google Scholar]
- 9.Vogt MT, Simonsick EM, Harris TB, Nevitt MC, Kang JD, Rubin SM, et al. Neck and shoulder pain in 70- to 79-year-old men and women: findings from the Health, Aging and Body Composition Study. Spine J. 2003;3:435–41. doi: 10.1016/s1529-9430(03)00150-5. [DOI] [PubMed] [Google Scholar]
- 10.Simons DG, Travell JG, Simons LS. Myofascial Pain and Dysfunction: The Trigger Point Manual. 2. Baltimore, MD: Williams & Wilkins; 1999. [Google Scholar]
- 11.Walitt B, Nahin RL, Katz RS, Bergman MJ, Wolfe F. The Prevalence and Characteristics of Fibromyalgia in the 2012 National Health Interview Survey. PLoS One. 2015;10:e0138024. doi: 10.1371/journal.pone.0138024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gorevic PD. Osteoarthritis. A review of musculoskeletal aging and treatment issues in geriatric patients. Geriatrics. 2004;59:28–32. quiz 5. [PubMed] [Google Scholar]
- 13.Plesh O, Adams SH, Gansky SA. Racial/Ethnic and gender prevalences in reported common pains in a national sample. J Orofac Pain. 2011;25:25–31. [PMC free article] [PubMed] [Google Scholar]
- 14.Carey TS, Freburger JK, Holmes GM, Jackman A, Knauer S, Wallace A, et al. Race, care seeking, and utilization for chronic back and neck pain: population perspectives. J Pain. 2010;11:343–50. doi: 10.1016/j.jpain.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Makela M, Heliovaara M, Sievers K, Impivaara O, Knekt P, Aromaa A. Prevalence, determinants, and consequences of chronic neck pain in Finland. Am J Epidemiol. 1991;134:1356–67. doi: 10.1093/oxfordjournals.aje.a116038. [DOI] [PubMed] [Google Scholar]
- 16.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;34:172–80. [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. NHIS survey description document. 2002 [cited 9/11/13]; Available from: http://www.cdc.gov/nchs.
- 18.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 19.Boyd JH, Weissman MM, Thompson WD, Myers JK. Screening for depression in a community sample. Understanding the discrepancies between depression symptom and diagnostic scales. Arch Gen Psychiatry. 1982;39:1195–200. doi: 10.1001/archpsyc.1982.04290100059010. [DOI] [PubMed] [Google Scholar]
- 20.Smarr KL, Keefer AL. Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9) Arthritis Care Res (Hoboken) 2011;63(Suppl 11):S454–66. doi: 10.1002/acr.20556. [DOI] [PubMed] [Google Scholar]
- 21.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–8. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 22.Hunsaker FG, Cioffi DA, Amadio PC, Wright JG, Caughlin B. The American academy of orthopaedic surgeons outcomes instruments: normative values from the general population. J Bone Joint Surg Am. 2002;84-A:208–15. doi: 10.2106/00004623-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980;23:137–45. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- 24.Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45:M192–7. doi: 10.1093/geronj/45.6.m192. [DOI] [PubMed] [Google Scholar]
- 25.Jones CJR, RE Measuring functional fitness of older adults. The Journal on Active Aging. 2002;1:24–30. [Google Scholar]
- 26.Cole A, Gill TK, Shanahan EM, Phillips P, Taylor AW, Hill CL. Is diabetes associated with shoulder pain or stiffness? Results from a population based study. J Rheumatol. 2009;36:371–7. doi: 10.3899/jrheum.080349. [DOI] [PubMed] [Google Scholar]
- 27.Lebiedz-Odrobina D, Kay J. Rheumatic manifestations of diabetes mellitus. Rheum Dis Clin North Am. 2010;36:681–99. doi: 10.1016/j.rdc.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 28.Molsted S, Tribler J, Snorgaard O. Musculoskeletal pain in patients with type 2 diabetes. Diabetes Res Clin Pract. 2012;96:135–40. doi: 10.1016/j.diabres.2011.12.022. [DOI] [PubMed] [Google Scholar]
- 29.Moren-Hybbinette I, Moritz U, Schersten B. The painful diabetic shoulder. Acta Med Scand. 1986;219:507–14. doi: 10.1111/j.0954-6820.1986.tb03347.x. [DOI] [PubMed] [Google Scholar]
- 30.Rauoof MA, Lone NA, Bhat BA, Habib S. Etiological factors and clinical profile of adhesive capsulitis in patients seen at the rheumatology clinic of a tertiary care hospital in India. Saudi Med J. 2004;25:359–62. [PubMed] [Google Scholar]
- 31.Slater M, Perruccio AV, Badley EM. Musculoskeletal comorbidities in cardiovascular disease, diabetes and respiratory disease: the impact on activity limitations; a representative population-based study. BMC Public Health. 2011;11:77. doi: 10.1186/1471-2458-11-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. Arthritis as a potential barrier to physical activity among adults with heart disease--United States, 2005 and 2007. MMWR Morb Mortal Wkly Rep. 2009;58:165–9. [PubMed] [Google Scholar]
- 33.Marzolini S, Candelaria H, Oh P. Prevalence and impact of musculoskeletal comorbidities in cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2010;30:391–400. doi: 10.1097/HCR.0b013e3181e174ac. [DOI] [PubMed] [Google Scholar]
- 34.Marzolini S, Oh PI, Alter D, Stewart DE, Grace SL. Musculoskeletal comorbidities in cardiac patients: prevalence, predictors, and health services utilization. Arch Phys Med Rehabil. 2012;93:856–62. doi: 10.1016/j.apmr.2011.11.034. [DOI] [PubMed] [Google Scholar]
- 35.Skeletal muscle dysfunction in chronic obstructive pulmonary disease. A statement of the American Thoracic Society and European Respiratory Society. Am J Respir Crit Care Med. 1999;159:S1–40. doi: 10.1164/ajrccm.159.supplement_1.99titlepage. [DOI] [PubMed] [Google Scholar]
- 36.Kim HC, Mofarrahi M, Hussain SN. Skeletal muscle dysfunction in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2008;3:637–58. doi: 10.2147/copd.s4480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sethi S. Musculoskeletal effects of chronic obstructive pulmonary disease: prevalent, linked, but ignored. Am J Respir Crit Care Med. 2004;170:1267–8. doi: 10.1164/rccm.2410001. [DOI] [PubMed] [Google Scholar]
- 38.Brattberg G, Parker MG, Thorslund M. A longitudinal study of pain: reported pain from middle age to old age. Clin J Pain. 1997;13:144–9. doi: 10.1097/00002508-199706000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Licht-Strunk E, van der Kooij KG, van Schaik DJ, van Marwijk HW, van Hout HP, de Haan M, et al. Prevalence of depression in older patients consulting their general practitioner in The Netherlands. Int J Geriatr Psychiatry. 2005;20:1013–9. doi: 10.1002/gps.1391. [DOI] [PubMed] [Google Scholar]
- 40.Chen X, Cheng HG, Huang Y, Liu Z, Luo X. Depression symptoms and chronic pain in the community population in Beijing, China. Psychiatry Res. 2012 doi: 10.1016/j.psychres.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 41.Cho CH, Jung SW, Park JY, Song KS, Yu KI. Is shoulder pain for three months or longer correlated with depression, anxiety, and sleep disturbance? J Shoulder Elbow Surg. 2012 doi: 10.1016/j.jse.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 42.Roh YH, Lee BK, Noh JH, Oh JH, Gong HS, Baek GH. Effect of depressive symptoms on perceived disability in patients with chronic shoulder pain. Arch Orthop Trauma Surg. 2012;132:1251–7. doi: 10.1007/s00402-012-1545-0. [DOI] [PubMed] [Google Scholar]
- 43.Daut RL, Cleeland CS. The prevalence and severity of pain in cancer. Cancer. 1982;50:1913–8. doi: 10.1002/1097-0142(19821101)50:9<1913::aid-cncr2820500944>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 44.Roux CH, Guillemin F, Boini S, Longuetaud F, Arnault N, Hercberg S, et al. Impact of musculoskeletal disorders on quality of life: an inception cohort study. Ann Rheum Dis. 2005;64:606–11. doi: 10.1136/ard.2004.020784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nelson AE, Elstad E, DeVellis RF, Schwartz TA, Golightly YM, Renner JB, et al. Composite measures of multi-joint symptoms, but not of radiographic osteoarthritis, are associated with functional outcomes: the Johnston County Osteoarthritis Project. Disabil Rehabil. 2014;36:300–6. doi: 10.3109/09638288.2013.790490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rekola KE, Levoska S, Takala J, Keinanen-Kiukaanniemi S. Patients with neck and shoulder complaints and multisite musculoskeletal symptoms--a prospective study. J Rheumatol. 1997;24:2424–8. [PubMed] [Google Scholar]
- 47.Haapanen N, Miilunpalo S, Pasanen M, Oja P, Vuori I. Agreement between questionnaire data and medical records of chronic diseases in middle-aged and elderly Finnish men and women. Am J Epidemiol. 1997;145:762–9. doi: 10.1093/aje/145.8.762. [DOI] [PubMed] [Google Scholar]
- 48.Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57:1096–103. doi: 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]


