Abstract
Background
Targeted partner notification (PN), or limiting PN to groups in which efforts are most successful, has been suggested as a potentially cost-effective alternative to providing PN for all syphilis case-patients. The purpose of this study was to identify index case characteristics associated with highest yield partner elicitation and subsequent case finding to determine whether some groups could be reasonably excluded from PN efforts.
Methods
We examined index case characteristics and PN metrics from syphilis case management records of 4 sexually transmitted disease control programs—New York City, Philadelphia, Texas, and Virginia. Partner elicitation was considered successful when a case-patient named 1 or more partners during interview. Case finding was considered successful when a case-patient had 1 or more partners who were tested and had serologic evidence of syphilis exposure. Associations between case characteristics and proportion of pursued case-patients with successful partner elicitation and case finding were evaluated using χ2 tests.
Results
Successful partner elicitation and new case finding was most likely for index case-patients who were younger and diagnosed at public sexually transmitted disease clinics. However, most characteristics of index case-patients were related to success at only a few sites, or varied in the direction of the relationship by site. Other than late latent case-patients, few demographic groups had a yield far below average.
Conclusions
If implemented, targeted PN will require site-specific data. Sites may consider eliminating PN for late latent case-patients. The lack of demographic groups with a below average yield suggests that sites should not exclude other groups from PN.
Partner services, or identifying and treating exposed contacts of persons with a sexually transmitted disease (STD), are routinely applied in syphilis control programs. If not identified and treated, syphilis can cause long-term complications, increase a person’s risk for HIV transmission and acquisition, and have devastating effects if transmitted from a pregnant woman to her unborn child.1 Most syphilis control programs rely on a mechanism known as provider referral, in which trained disease intervention specialists (DIS) interview persons with reactive syphilis tests (index case-patients) to elicit and notify contacts. The effectiveness of provider referral for syphilis case finding and treatment has been well documented.2–5 However, effective provider-referral programs require a substantial allocation of funds and labor.6–9
Between 2008 and 2009, most STD programs in the United States experienced funding cuts that forced drastic service reductions.10 These reductions came at a time of increased syphilis rates in many areas, underscoring the need for evidence-based, cost-effective partner services programs. Targeted partner notification (PN), or limiting PN to groups where efforts are most likely to be successful or have the most public health impact, has been suggested as a potentially cost-effective alternative to providing PN for all syphilis case-patients. Decisions regarding resource allocation require knowledge of which groups would yield the most in terms of partner elicitation and case finding. The purpose of this study was to identify index case characteristics associated with increased partner elicitation and case finding to determine whether targeting syphilis PN is desirable.
MATERIALS AND METHODS
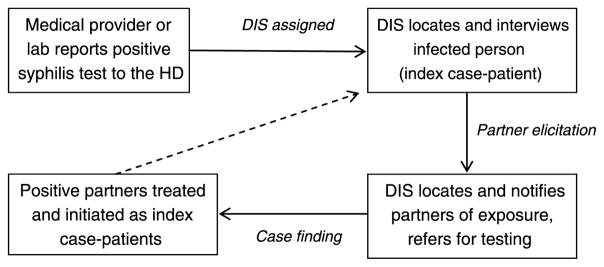
State laws mandate reporting of syphilis cases by providers and laboratories to the local health department upon diagnosis (Fig. 1). Health departments routinely conduct investigations of syphilis cases of specific stages to assure treatment for patients and partners. Transmission is less common during late stages of syphilis, so some health departments may not investigate late latent cases. If staging is unavailable, health departments rely on laboratory reports and patient characteristics to determine whether to conduct a case investigation. A case investigation includes determining disease stage in addition to assuring treatment and conducting PN. Disease intervention specialists attempt to locate and interview assigned index case-patients; interviews are not completed if case-patients cannot be located, refuse to be interviewed, or are deceased. Interviewed case-patients are asked to name sexual partners since the time at which they likely acquired their infection so that the source and subsequent contacts can be tested and treated for exposure or infection. The DIS assigns a disposition code to all elicited contacts to indicate the outcome of PN (e.g., “infected, brought to treatment” or “previously treated”).11
Figure 1.
Flow of syphilis partner services. DIS, indicates Disease Intervention Specialist; HD, health department.
New York City (NYC), Philadelphia, Texas, and Virginia provided de-identified electronic data from their syphilis PN case management systems. These sites were chosen as a convenience sample of syphilis control programs willing to share de-identified electronic data for analysis. Philadelphia, Texas, and Virginia provided data from January 1 to December 31, 2010, whereas NYC provided data from January 1, 2009, to June 30, 2010. Because NYC’s STD surveillance data were migrated to a new system at the end of 2010, data were used for only the first half of 2010 to ensure adequate time for closure of investigations. Each site provided 2 files—one with all case-patients that included demographics and diagnosis and one with all contacts of case-patients that included demographics and the PN outcome.
We define “pursued” case-patients as those assigned to DIS for investigation. Partner elicitation was considered successful when an index case-patient named 1 or more sex partners during an interview. Case finding was considered successful when at least 1 of the case-patient’s partners was successfully traced, tested positive, and treated after the DIS interview (disposition of “infected, brought to treatment,” hereafter referred to as “brought to treatment”). Most (94%) case-patients who named a partner subsequently brought to treatment had only 1 partner brought to treatment, so we considered a dichotomous outcome to be sufficient (i.e., 0 partners named vs. ≥1 partner named). The partner-to-index ratio for each site was calculated by dividing the number of sex partners pursued by the number of case-patients interviewed. Primary, secondary, and early latent diagnoses of syphilis were considered early syphilis.
Associations between index case characteristics and proportion of pursued case-patients with partners successfully elicited and cases subsequently found were evaluated using χ2 tests, with P values less than 0.05 considered statistically significant. All analyses were conducted in SAS 9.3 (Cary, NC).
Data Validation
It is possible that sites and/or DIS may assign PN dispositions differently, making it difficult to compare those brought to treatment across sites. To ensure consistency in the use of dispositions between jurisdictions, we reviewed data at 2 participating study sites: NYC and Philadelphia. We evaluated instances in which a partner was assigned a brought to treatment disposition and examined records from that partner’s corresponding index case. Our expectation was that the partner should be categorized as brought to treatment in the original index case’s chart if the partner was (1) reactive for syphilis and (2) treated after DIS interview of the index case.11 If a partner names back the original index case, the original index case should be classified as previously treated rather than brought to treatment in the partner’s record.11 Disposition errors were corrected in the analysis to see how they affected results.
RESULTS
Site Summary Data
New York City had 5479 syphilis case-patients reported for 18 months (Table 1). Approximately 70% were pursued by a DIS; of the 1661 case-patients not pursued, 98% (n = 1628) had late latent syphilis. Of 3818 pursued, 77% (n = 2946) completed DIS interview and 32% (n = 1218) named 1 or more partners; 17% (n = 732) of those pursued were diagnosed at an STD clinic. Interviewed case-patients named 2046 partners total, for a partner-to-index ratio of 0.7. Approximately 4% of those pursued had 1 or more partners brought to treatment.
TABLE 1.
Syphilis Partner Services Summary Statistics for 4 Sites
| Site | Period | Index Case-persons Reported, n | Index Case-Persons Pursued,* n (%) | Index Case-Persons Interviewed, n (%)† | Partner-to-Index Ratio‡ | Index Case-Persons That Named ≥1 Partner, n (%)† | Index Case-Persons With ≥1 Partner Brought to Treatment, n (%)† |
|---|---|---|---|---|---|---|---|
| NYC | January 2009–June 2010 | 5479 | 3818 (69.7) | 2946 (77.2) | 0.7 | 1218 (31.9) | 154 (4.0) |
| Philadelphia | January 2010–Dec 2010 | 660 | 660 (100.0) | 547 (82.9) | 0.7 | 238 (36.1) | 45 (6.8) |
| Texas | January 2010–Dec 2010 | 6300 | 6178 (98.1) | 5807 (93.4) | 2.2 | 4599 (74.4) | 817 (13.2) |
| Virginia | January 2010–Dec 2010 | 768 | 571 (74.3) | 517 (90.5) | 1.5 | 352 (61.7) | 61 (10.7) |
Assigned to a DIS; includes any stage of syphilis.
Denominator for percentages is number pursued.
Includes multiple partners per case.
Philadelphia had 660 syphilis case-patients reported in 2010. All were assigned to a DIS, and 83% (n = 547) were interviewed. Of those pursued, 46% (n = 301) were diagnosed at an STD clinic. Like NYC, approximately one-third of interviewed cases (36%) named 1 or more partners (n = 238). The 547 case-patients interviewed named 389 partners, for a partner-to-index ratio of 0.7. Approximately 7% had 1 or more partners brought to treatment.
Texas had 6300 syphilis case-patients reported in 2010 and pursued most (98%). Of those not pursued, 73% were late latent syphilis. Of those pursued, 26% (n = 1608) were diagnosed at an STD clinic. A larger proportion of case-patients were interviewed (93%) compared with NYC (77%) and Philadelphia (83%), and 74% of Texas case-patients named 1 or more partners to DIS, more than double that of either of the 2 city programs. The 5807 interviewed reported 12,775 partners for a partner-to-index ratio of 2.2. Of those pursued, 13% had 1 or more partners brought to treatment.
Virginia had 768 syphilis case-patients reported in 2010. Approximately 75% (n = 571) were pursued; 99% not pursued were late latent or infections of unknown duration. Of case-patients pursued, 91% were interviewed and 62% named 1 or more partners, also considerably higher than the NYC and Philadelphia programs. Almost half (49%) of those pursued were diagnosed at an STD clinic. The 517 interviewed case-patients named 776 partners for a partner-to-index ratio of 1.5. Of those pursued, 11% had 1 or more partners brought to treatment.
Bivariate Analyses
Percent With Named Partner
Female sex, younger age (<35 years), and diagnosis at a public STD clinic were consistently associated with effective partner elicitation across sites (Table 2). The association with sex was strongest in NYC, where the percent of female case-patients that named 1 or more partners was almost double the percent of males (53% vs. 30%), although the number of female cases was relatively small (n = 338). The percent of case-patients that named 1 or more partners decreased with increasing age. Even in the oldest age group (≥age 45 years); however, almost a quarter of case-patients named a partner. Those diagnosed as having syphilis at an STD clinic were more likely to name a partner than those diagnosed elsewhere. Those diagnosed by a private doctor were least likely to name a partner.
TABLE 2.
Characteristics of Index Case-Persons With ≥1 Partner Brought to Treatment Disposition
| Index Case Characteristic | NYC (n = 3818)
|
Philadelphia (n = 660)
|
Texas (n = 6178)
|
Virginia (n = 571)
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % With Named Partner | % With Partner Brought to Treat | n | % With Named Partner | % With Partner Brought to Treat | n | % With Named Partner | % With Partner Brought to Treat | n | % With Named Partner | % With Partner Brought to Treat | |
| Overall | 3818 | 31.9 | 4.0 | 660 | 36.1 | 6.8 | 6178 | 74.4 | 13.2 | 571 | 61.7 | 10.7 |
| Sex | ||||||||||||
| Male | 3480 | 29.8 | 3.6 | 530 | 34.3 | 6.8 | 4117 | 70.2 | 11.6 | 485 | 59.0 | 10.3 |
| Female | 338 | 53.3 | 8.3 | 130 | 43.1 | 6.9 | 2060 | 82.9 | 16.4 | 85 | 77.7 | 12.9 |
| Age, y | ||||||||||||
| <25 | 595 | 50.4 | 8.6 | 170 | 50.0 | 12.9 | 2022 | 85.2 | 18.0 | 164 | 76.2 | 14.6 |
| 25–34 | 1000 | 39.4 | 5.9 | 185 | 38.9 | 7.6 | 1861 | 78.6 | 14.5 | 168 | 65.5 | 11.3 |
| 35–44 | 1293 | 24.0 | 2.2 | 145 | 32.4 | 2.8 | 1201 | 66.1 | 9.6 | 105 | 49.5 | 7.6 |
| ≥45 | 930 | 22.9 | 1.6 | 160 | 21.3 | 3.1 | 1093 | 56.6 | 6.3 | 134 | 48.5 | 7.5 |
| Black race | ||||||||||||
| No | 2190 | 30.1 | 3.8 | 109 | 42.2 | 6.4 | 3126 | 71.7 | 13.2 | 229 | 55.0 | 12.2 |
| Yes | 1566 | 35.1 | 4.5 | 491 | 34.8 | 7.1 | 3022 | 77.5 | 13.3 | 341 | 66.3 | 9.7 |
| Hispanic ethnicity | ||||||||||||
| No | 2577 | 31.1 | 3.8 | 592 | 35.6 | 6.8 | 4187 | 74.6 | 12.5 | 523 | 61.8 | 10.5 |
| Yes | 1166 | 34.9 | 4.6 | 68 | 39.7 | 7.4 | 1959 | 74.6 | 14.9 | 47 | 61.7 | 12.8 |
| Sex/Sexual behavior | ||||||||||||
| Female | 338 | 53.3 | 8.3 | 130 | 43.1 | 6.9 | 2060 | 82.9 | 16.4 | 85 | 77.7 | 12.9 |
| MSW only* | 349 | 47.3 | 3.2 | 132 | 33.3 | 5.3 | 1616 | 78.0 | 13.1 | 97 | 63.9 | 10.3 |
| MSM* | 2249 | 37.5 | 5.0 | 294 | 45.2 | 9.9 | 2126 | 75.5 | 12.5 | 361 | 62.1 | 11.1 |
| Provider type | ||||||||||||
| STD clinic | 732 | 55.1 | 9.7 | 301 | 49.8 | 9.6 | 1608 | 88.7 | 15.3 | 282 | 76.6 | 14.5 |
| Private doctor | 1985 | 25.3 | 2.4 | 29 | 17.2 | 3.5 | 1303 | 65.9 | 11.5 | 161 | 43.5 | 5.0 |
| Other† | 1101 | 28.3 | 3.2 | 330 | 25.2 | 4.6 | 3267 | 70.8 | 12.9 | 128 | 51.6 | 9.4 |
| Time-to-assign date, d | ||||||||||||
| ≤7 | 981 | 41.3 | 6.2 | 318 | 37.7 | 8.2 | 2000 | 86.3 | 16.4 | 217 | 68.2 | 13.8 |
| 7–14 | 1904 | 28.2 | 3.2 | 162 | 32.1 | 3.7 | 1955 | 72.5 | 14.4 | 114 | 64.9 | 8.8 |
| 15–30 | 672 | 26.2 | 3.0 | 91 | 33.0 | 5.5 | 1589 | 65.5 | 9.9 | 81 | 53.1 | 6.2 |
| >30 | 202 | 32.2 | 3.5 | 43 | 34.9 | 7.0 | 586 | 64.7 | 7.3 | 42 | 45.2 | 9.5 |
| Previous | ||||||||||||
| STD history | ||||||||||||
| No/Unknown | 1597 | 36.1 | 5.4 | 3678 | 76.4 | 14.3 | ||||||
| Yes | 2221 | 28.9 | 3.1 | 2500 | 71.6 | 11.7 | ||||||
| HIV status | ||||||||||||
| Negative/Unknown | 1958 | 36.9 | 5.3 | 457 | 35.5 | 6.6 | 4770 | 78.2 | 14.7 | 362 | 64.4 | 11.1 |
| Positive | 1860 | 26.6 | 2.7 | 203 | 37.4 | 7.4 | 1408 | 61.9 | 8.2 | 209 | 56.9 | 10.1 |
| Syphilis stage at diagnosis | ||||||||||||
| Primary | 327 | 36.7 | 6.1 | 45 | 42.2 | 11.1 | 310 | 90.3 | 24.2 | 57 | 54.4 | 8.8 |
| Secondary | 1173 | 33.8 | 4.8 | 192 | 39.6 | 12.0 | 919 | 91.3 | 20.6 | 201 | 69.7 | 13.9 |
| Early latent | 1721 | 31.2 | 4.1 | 220 | 44.1 | 6.8 | 1823 | 90.1 | 24.5 | 261 | 60.5 | 10.3 |
| Late latent/unknown duration | 597 | 27.3 | 1.3 | 202 | 22.8 | 1.0 | 3126 | 58.8 | 3.4 | 52 | 44.2 | 1.9 |
| Race and age | ||||||||||||
| Nonblack, ≤35 y | 852 | 43.7 | 7.0 | 43 | 48.8 | 7.0 | 1827 | 79.9 | 16.8 | 114 | 67.5 | 15.8 |
| Nonblack, >35 y | 1338 | 21.5 | 1.7 | 66 | 37.9 | 6.1 | 1298 | 60.1 | 8.2 | 115 | 42.6 | 8.7 |
| Black, ≤35 y | 760 | 26.8 | 2.6 | 206 | 23.8 | 2.4 | 2174 | 83.3 | 15.4 | 227 | 71.8 | 11.9 |
| Black, >35 y | 806 | 42.9 | 6.2 | 285 | 42.8 | 10.5 | 848 | 62.7 | 7.9 | 114 | 55.3 | 5.3 |
Bolding indicates statistical significance at P < 0.05.
Categories may not sum to totals due to missing data.
Missing data make this category difficult to interpret.
”Other” category includes HIV counseling/testing sites, drug treatment facilities, family planning clinics, emergency departments, and correctional facilities.
MSW indicates men who have sex with women.
Race and sex/sexual behavior were associated with naming a partner, but the direction of the association differed by site. Black case-patients were more likely than other races/ethnicities to name 1 or more partners in NYC, Texas, and Virginia, whereas the opposite was true in Philadelphia. Men who have sex with men (MSM) were less likely than women and men who have sex with women only (MSW) to name a partner in NYC, Texas, and Virginia, although the difference between MSM and MSW was small in Virginia (62% vs. 64%). In Philadelphia, MSM were more likely than MSW (45% vs. 33%) and as likely as women (45% vs. 43%) to name a partner.
Hispanics were slightly more likely to name a partner compared with non-Hispanics in NYC (35% vs. 31%) and Philadelphia (40% vs. 36%). There was no difference in naming a partner by Hispanic ethnicity in Texas or Virginia. Shorter time-to-assign date was associated with naming a partner in NYC, Texas, and Virginia. However, this was only true in NYC if the index case was assigned to a DIS within 7 days. Time-to-assign date was not associated with naming a partner in Philadelphia. HIV-negative case-patients were more likely to name a partner in NYC (37% vs. 27% of HIV-positive patients) and Texas (78% vs. 62%), but there was no difference by HIV status in Philadelphia or Virginia. Case-patients diagnosed as having an early stage of syphilis were more likely to name a partner in NYC, but not at other sites. At each site, those with late syphilis or syphilis of unknown duration were least likely to name a partner; however, even in Philadelphia, which had the lowest percent in that category, 22.8% named a partner.
The association between age and naming a partner varied by race in NYC and Philadelphia. As described, case-patients of younger age were more likely to name a partner than older case-patients. However, when this association was stratified by race in the cities, the opposite association was found among blacks compared with other races. Older black case-patients were more likely to name a partner compared with younger black case-patients. In Texas and Virginia, younger case-patients were more likely to name a partner regardless of race.
Percent With a Partner Brought to Treatment
Younger age and provider type were associated with having a partner brought to treatment at all 4 sites. In NYC and Philadelphia, case-patients younger than 25 years were about 4 times more likely than those 35 and older to have a partner brought to treatment. As with naming a partner, case-patients diagnosed in an STD clinic were most likely to have a partner brought to treatment, whereas those diagnosed in a private clinic were least likely.
The association between sex/sexual behavior and having a partner brought to treatment differed by site. In both NYC and Texas, women were most likely to have a partner brought to treatment; however, in NYC, MSM were more likely than MSW to have a partner brought to treatment (5% vs. 3%), whereas in Texas, there was no difference between the 2 groups of men (13% in both). In Philadelphia, MSM were most likely to have a partner brought to treatment (10%). There was no difference by sex/sexual behavior in Virginia. Shorter time-to-assign date was associated with having a partner brought to treatment in NYC and Texas.
HIV-negative case-patients were more likely to have a partner brought to treatment in NYC and Texas, but not in Philadelphia or Virginia. The percentage with a partner brought to treatment was higher for those with early syphilis in NYC, Philadelphia, and Texas. Those with a diagnosis of late latent syphilis or syphilis of unknown duration were least likely to have a partner brought to treatment at all sites. Only 1% to 3% of index case-patients in this category yielded a partner brought to treatment.
Race was not associated with having a partner brought to treatment at any site. However, the association between age and having a partner brought to treatment varied by race in NYC and Philadelphia. Older black case-patients (>age 35 years) were more likely to have a partner brought to treatment compared with younger index case-patients (≤age 35 years), whereas the opposite was true for nonblack case-patients.
Data Validation
Often there was not enough information in the case management system to determine if dispositions were assigned correctly. For case-patients with enough information to make a determination, most partners were correctly assigned as brought to treatment. In some instances, partnerships in which both individuals were reactive for syphilis were marked as partners brought to treatment in each other’s index case charts, although one of the partners should have been dispositioned as previously treated. This error happened 17 times (10% of brought to treatment dispositions) in NYC and 13 times (22%) in Philadelphia. These errors did not affect the results of the analysis when corrected in the data, although did decrease the percent brought to treatment.
There were also 3 instances (5%) in Philadelphia in which partners came into a clinic together for testing, were presumptively treated, and were both dispositioned as brought to treatments when their tests came back reactive. Sites disagreed on whether one or neither partner should be dispositioned as brought to treatment because both were technically treated before DIS intervention. Because a reference standard addressing this scenario could not be found, these dispositions were not changed in the data.
DISCUSSION
Targeted PN has been suggested as a potentially resource-saving alternative to providing PN for all syphilis case-patients. To determine whether some groups could be reasonably excluded from PN efforts, we sought to identify index case characteristics associated with highest yield partner elicitation and subsequent case finding. Successful partner elicitation and case finding were most likely when index case-patients were younger than 35 years and diagnosed at an STD clinic. However, most characteristics were related to success at only a few sites and not others, or had contradictory associations among sites. Also, although most characteristics associated with successful partner elicitation were also associated with successful case finding, some (such as sex and race) were not, indicating that both outcomes should be examined.
Another important finding was that few groups had a proportion of case-patients with a named partner or with a partner brought to treatment that was so far below average that sites should consider curtailing PN among that demographic. The lowest proportion of case-patients that named a partner among all categories was 23%, indicating that almost a quarter in each group named a partner. The proportion of case-patients with a partner brought to treatment was as low as 2% among older age groups in NYC, but only 4% overall had a partner brought to treatment. Case-patients with late latent syphilis or syphilis of unknown duration were consistently unlikely to have a partner brought to treatment, so it may be useful to limit PN to earlier stages. However, syphilis stage is often uncertain until a partner investigation is completed, so it is unclear if decisions on pursuing case-patients should be made from initial staging. In addition, several sites already limit the number of case-patients with late syphilis for which they conduct PN because transmission is unlikely.
Our finding that case-patients diagnosed at STD clinics were most likely to name a partner and have a partner brought to treatment was likely due to having DIS present at STD clinics. Studies have shown that when DIS are available to conduct interviews right after STD diagnosis at clinics with high diagnosis rates (MSM clinics, HIV care clinics, etc), there is an increase in the average number of locatable partners and partners brought to treatment.12,13 Our finding that successful partner elicitation and case finding was not substantially lower among MSM compared with women or MSW was also consistent with previous studies demonstrating that MSM are receptive to PN.14,15
Our study also highlights heterogeneity in successful partner elicitation and case finding across programs. According to these data, Texas and Virginia’s partner services programs seem to do substantially better than those in NYC and Philadelphia. This could be due to differences in assigning dispositions or differences in DIS training by site. Certain DIS are also better at establishing a rapport with case-patients than others. The sex and sexual behavior of DIS may also influence PN metrics; these data were not available for our analysis. Alternatively, it could be that people and providers are more receptive to PN in certain areas. Although NYC and Philadelphia are large urban cities, Texas and Virginia are states with both rural and urban areas. Contacts in rural areas may be more likely to be known versus anonymous and more easily located when compared with contacts in urban areas. Validation of local site data and studies of differences in program success are needed to understand whether these differences are due to modifiable factors that could improve effectiveness.
There are several limitations to this analysis. First, sites and/or DIS may assign dispositions differently, making site comparisons difficult. Differences in disposition codes did not affect results by subgroup in the 2 cities. However, we were unable to visit Texas and Virginia to do similar analyses. In addition, other than the disposition definitions, there is no reference describing standards for assigning dispositions in certain scenarios such as when partners test together. This leads to sites differentially assigning dispositions. Another limitation is that Texas and Virginia data are compiled from statewide PN activities. Geographic regions within states likely vary significantly with respect to demographics, so it may be useful to stratify this analysis by region to determine if targeting would be useful in a particular region. Another limitation is that we do not have a measure of DIS effort; these results may reflect informal DIS work practices (i.e., a priori allocating less effort into PN of certain groups based on past experience). We also do not have measures of cost or time associated with partner services and cannot do a cost-effectiveness analysis to determine if targeting would be cost saving.
Targeting has been suggested as a means to manage a reduced DIS workforce and could be implemented by excluding PN to groups with low yields. Alternatively, targeting could be implemented by spending less time on these case-patients, by restricting time spent locating partners or on conducting reinterviews. However, targeted PN has several limitations. First, targeting fails to take into account the value of PN beyond case finding. This includes fulfilling the duty to warn, counseling of case-patients, establishing community partnerships, and obtaining a better idea of disease transmission patterns in a region.2,16,17 In addition, not all partners brought to treatment are the same. Some are more important than others in preventing onward community transmission, such as high-frequency transmitters and pregnant women, but this is not captured by PN metrics. Finally, targeting guidelines can only be developed using data on located partners and will not address transmission among unnamed partners that cannot be located. Syphilis control programs with a high burden of index case-patients with many unnamed partners will require alternative interventions to decrease syphilis transmission.
In this analysis of 4 syphilis PN programs, characteristics associated with successful partner elicitation and case finding varied by site. Because few groups had substantially lower percentages of partner elicitation and case finding that would indicate that sites should exclude those groups from partner services, it is unclear if targeting would improve PN success. If targeting is considered, it would need to be implemented using site-specific data to determine what groups would yield the most success. In addition, this analysis shows that sites assign disposition codes differently. To make reliable site comparisons, a standardized reference that sites can refer to for guidance in assigning PN metrics is needed.
Acknowledgments
The authors thank Robin Hennessy Makki, MPH (New York City); Karen M. Arrowood, MPH (Texas); and Kristen Kreisel, PhD (Virginia), for their help in obtaining site data.
Funding support: None.
Footnotes
Potential conflicts of interest: None.
References
- 1.Centers for Disease Control and Prevention (CDC) [Accessed October 25, 2013];Syphilis—CDC Fact Sheet. Available at: http://www.cdc.gov/std/syphilis/STDFact-Syphilis.htm.
- 2.Brewer DD. Case-finding effectiveness of partner notification and cluster investigation for sexually transmitted diseases/HIV. Sex Transm Dis. 2005;32:78–83. doi: 10.1097/01.olq.0000153574.38764.0e. [DOI] [PubMed] [Google Scholar]
- 3.Hogben M, Paffel J, Broussard D, et al. Syphilis partner notification with men who have sex with men: A review and commentary. Sex Transm Dis. 2005;32(10 suppl):S43–S47. doi: 10.1097/01.olq.0000180565.54023.bf. [DOI] [PubMed] [Google Scholar]
- 4.Kohl KS, Farley TA, Ewell J, et al. Usefulness of partner notification for syphilis control. Sex Transm Dis. 1999;26:201–207. doi: 10.1097/00007435-199904000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Peterman TA, Toomey KE, Dicker LW, et al. Partner notification for syphilis: A randomized, controlled trial of three approaches. Sex Transm Dis. 1997;24:511–518. doi: 10.1097/00007435-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease, C, Prevention. Recommendations for partner services programs for HIV infection, syphilis, gonorrhea, and chlamydial infection. MMWR Recomm Rep. 2008;57:1–83. quiz CE1-4. [PubMed] [Google Scholar]
- 7.Macke BA, Hennessy MH, McFarlane M. Predictors of time spent on partner notification in four US sites. Sex Transm Infect. 2000;76:371–374. doi: 10.1136/sti.76.5.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oxman GL, Doyle L. A comparison of the case-finding effectiveness and average costs of screening and partner notification. Sex Transm Dis. 1996;23:51–57. doi: 10.1097/00007435-199601000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Reynolds SL, Kapadia AS, Leonard L, et al. Examining the direct costs and effectiveness of syphilis detection by selective screening and partner notification. J Public Health Med. 2001;23:339–345. doi: 10.1093/pubmed/23.4.339. [DOI] [PubMed] [Google Scholar]
- 10.(NCSD), N.C.o.S.D. [Accessed July 10, 2013];STD Program Capacity and Preparedness in the US: Results of a National Survey. 2009 Available at: http://www.ncsddc.org/upload/wysiwyg/NCSD%20Fact%20Sheets/Fact%20Sheet%20STD%20Program%20Capacity%20and%20Preparedness%20in%20the%20United%20States%20Results%20of%20a%20National%20Survey%202009.pdf.
- 11.Centers for Disease Control and Prevention (CDC) [Accessed October 25, 2013];Comprehensive Field Record (CFR) Instructions. Available at http://www.cdc.gov/std/Program/forms/CFR-2013/CFR-Instructions-2013.pdf.
- 12.Taylor MM, Mickey T, Winscott M, et al. Improving partner services by embedding disease intervention specialists in HIV-clinics. Sex Transm Dis. 2010;37:767–770. doi: 10.1097/OLQ.0b013e3181e65e8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rudy ET, Aynalem G, Cross J, et al. Community-embedded disease intervention specialist program for syphilis partner notification in a clinic serving men who have sex with men. Sex Transm Dis. 2012;39:701–705. doi: 10.1097/OLQ.0b013e3182593b51. [DOI] [PubMed] [Google Scholar]
- 14.Woodward CL, Roedling S, Edwards SG, et al. Computer-assisted survey of attitudes to HIV and sexually transmissible infection partner notification in HIV-positive men who have sex with men. Sex Health. 2010;7:460–462. doi: 10.1071/SH09146. [DOI] [PubMed] [Google Scholar]
- 15.Mimiaga MJ, Reisner SL, Tetu AM, et al. Partner notification after STD and HIV exposures and infections: knowledge, attitudes, and experiences of Massachusetts men who have sex with men. Public Health Rep. 2009;124:111–119. doi: 10.1177/003335490912400114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Potterat JJ. Contact tracing’s price is not its value. Sex Transm Dis. 1997;24:519–521. doi: 10.1097/00007435-199710000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Clark EG. The epidemiology of syphilis with particular reference to contact investigation. Am J Med. 1948;5:655–669. doi: 10.1016/0002-9343(48)90141-7. [DOI] [PubMed] [Google Scholar]