Abstract
Purpose
We evaluate solutions for an applanating surface modification to the Goldmann tonometer prism, which substantially negates the errors due to patient variability in biomechanics.
Methods
A modified Goldmann or correcting applanation tonometry surface (CATS) prism is presented which was optimized to minimize the intraocular pressure (IOP) error due to corneal thickness, stiffness, curvature, and tear film. Mathematical modeling with finite element analysis (FEA) and manometric IOP referenced cadaver eyes were used to optimize and validate the design.
Results
Mathematical modeling of the optimized CATS prism indicates an approximate 50% reduction in each of the corneal biomechanical and tear film errors. Manometric IOP referenced pressure in cadaveric eyes demonstrates substantial equivalence to GAT in nominal eyes with the CATS prism as predicted by modeling theory.
Conclusion
A CATS modified Goldmann prism is theoretically able to significantly improve the accuracy of IOP measurement without changing Goldmann measurement technique or interpretation. Clinical validation is needed but the analysis indicates a reduction in CCT error alone to less than ±2 mm Hg using the CATS prism in 100% of a standard population compared to only 54% less than ±2 mm Hg error with the present Goldmann prism.
Translational Relevance
This article presents an easily adopted novel approach and critical design parameters to improve the accuracy of a Goldmann applanating tonometer.
Keywords: glaucoma, intraocular pressure, corneal biomechanics, tonometry
Introduction
Glaucoma is the disease most commonly associated with intraocular pressure (IOP). However, IOP is arguably the second-most critical metric next to visual acuity for assessing the ocular health of an individual. Therefore, accurate, repeatable, and interpatient comparable measurements of IOP often are helpful and occasionally critical for the treatment of all ocular disease processes as well as for routine screening exams by any eye care professional. Intraocular pressure measurement not only is critical to the accurate diagnosis of ocular disease, but also is a necessary guide to effective treatment strategies. The IOP is assessed routinely on the majority of patient visits to eye care professionals, including ophthalmologists and optometrists, which total approximately 50,000 in the United States and approximately 450,000 worldwide.1,2 Glaucoma alone is a chronic and potentially debilitating disease requiring lifelong treatment. This disease currently affects 2.2 million Americans, with 3.3 million more expected by the year 2020. Glaucoma is now the leading cause of blindness in the aging Hispanic and African American populations, and nearly three times as common in African Americans as in White Americans. Worldwide, there were 60.5 million people with various types of glaucoma in 2010; this figure is expected to increase to 79.6 million by 2020.3 Patients still go blind and suffer significant debilitating vision loss from glaucoma due to misdiagnosis and mismanagement.4
For almost 60 years, Goldmann applanation tonometry (GAT) remains the standard for measurement of IOP.5,6 Numerous significant errors in the GAT IOP measurements (mm Hg) have been described previously. Those errors are due to patient variability in corneal thickness (±7 mm Hg), corneal rigidity (±8 mm Hg), corneal curvature (±2 mm Hg), and corneal tear film (±5 mm Hg).7–9 The combined errors of patient variable parameters are potentially sight threatening to a large population of patients, such as those with glaucoma or undiagnosed ocular hypertension from other causes, yet currently this is the best method we have clinically. Despite the inherent shortcomings identified in the GAT, nothing has improved upon its accuracy, cost-effectiveness, and ease of use. This problem was brought into the spotlight by the findings of the Ocular Hypertension Treatment Study (OHTS), which noted that pressure readings tend to be overestimated in thick, and underestimated in thinner, corneas. These errors lead to a misdiagnosis of glaucoma.10 Since the OHTS findings, the standard of practice has changed to include a measurement of central corneal thickness (CCT) with a nomogram to correct the pressure for the CCT. Additionally, the effects of laser-assisted in situ keratomileusis (LASIK) surgery render accurate IOP measurement by the GAT problematic.11 The CCT correction has been partially effective but unreliable due to the other potential corneal biomechanical and tear film errors. Attempts were made to measure and quantify the various error components to correct the GAT measurement and yield a standard IOP reading comparable between patients.12 However, the process in practice is error prone and cumbersome, leading to very limited clinical adoption with the exception of CCT. Other direct measurements of IOP that potentially reduce error have been developed, such as the dynamic contour tonometer (DCT) which provides for a constant appositional force of 1 g on a concave surface, which contains a central miniaturized piezoresistive pressure sensor. This device is very similar to a tonopen tonometer but adds the constant 1 g of force which partially negates biomechanical errors by allowing the corneal deformation force to be partly resisted by the portion of the contact surface that does not measure IOP. The DCT similar to the error correcting noncontact ocular response analyzer (ORA) is not widely used and has had minimal clinical acceptance for routine IOP measurement.
Central corneal thickness or corneal thickness in general is a geometric quantity affecting the rigidity of the cornea.8 The cornea is assumed by the Imbert-Fick principle to be an infinitely thin membrane that by definition has no shear rigidity, only strength in tension.5,8 The “rigidity” of the cornea also is affected by the corneal curvature. A steeply curved cornea must be “bent” more to applanate against the tonometer prism overestimating the IOP. Conversely a flat cornea, such as in someone who has had LASIK, underestimates the IOP. Also, the intrinsic material property of the cornea (the modulus of elasticity – both Young's and shear) greatly affect the “rigidity” of the cornea.13–15 All of these rigidity-affecting components together increase the force on the tonometer prism, which is attributed to IOP but, in fact, have no direct relation to IOP, hence the error. Finally, attraction created by the surface tension in the tear film (which also is extremely variable in patients) was theorized to negate much of the “rigidity” error.16,17 However, no clinical quantification of this highly variable attractive capillary force has been demonstrated in its effect on IOP.
The CATS tonometer prism is a modification of the GAT prism. The CATS prism optimizes the corneal applanating surface of the flat surface GAT prism. The function of the CATS prism, including force to pressure conversion supplied by the GAT armature, remains unchanged. The optimized CATS prism is designed to measure the same pressure as GAT prism under “nominal” conditions. The “nominal” conditions include a standard average corneal thickness, curvature, rigidity, and tear film. However, approximately 50% of the patient population do not have a “nominal” cornea.7,9,10,12 In these patients, the variability in each of these parameters induces significant individual and combined error in GAT IOP measurement, as mentioned previously.7–9 Even the errors due to corneal thickness alone, which is but a fraction of the total error, are sight threatening.10 For this reason, CCT correction was adopted as a standard of practice.10 Although several other separate measurements and error corrections were proposed, they have been too cumbersome to be adopted clinically.12 The CATS tonometer prism, illustrated in Figures 1 and 2, can significantly reduce all of the identified measurement errors using the exact same measurement apparatus (with a modified prism), practitioner protocol, and measurement technique without calculations, increased time, and at minimal cost.
Figure 1.
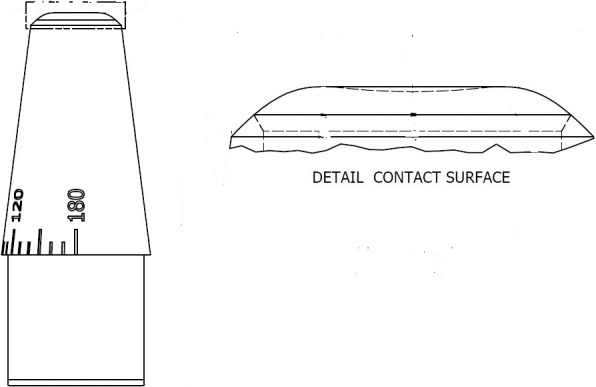
Sagittal cross-section of the CATS tonometer prism applanating surface.
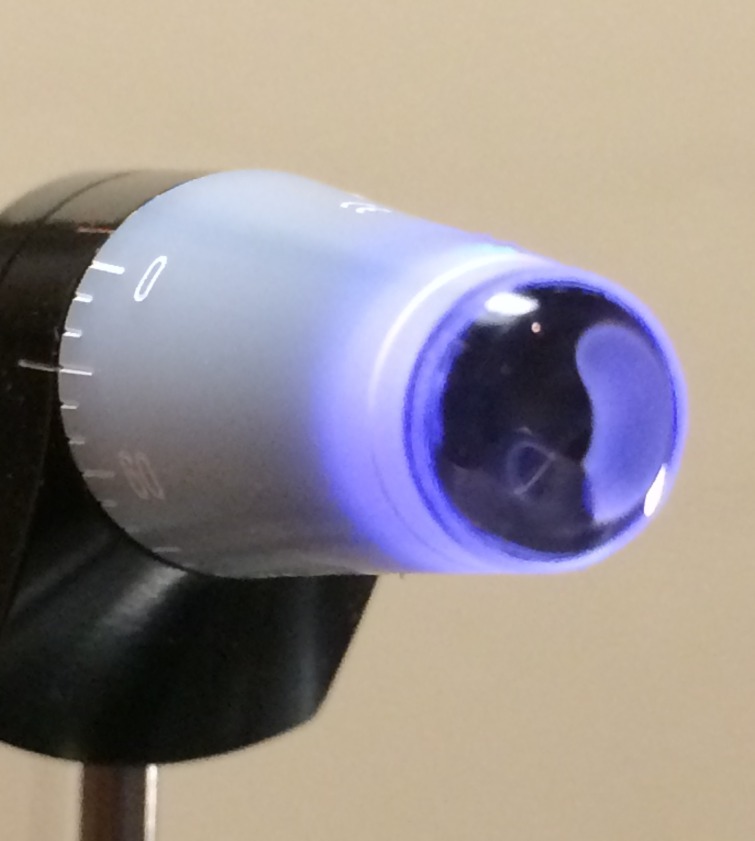
Figure 2.
Photograph of the concave–convex CATS tonometer prism applanating surface on the prototype illustrating the optically polished and contoured surface.
Methods
Two methods were used to assess the GAT: the finite element modeling (FEM), and cadaveric human eye benchtop testing. These methods are described in detail below.
Finite Element Modeling
A GAT estimates IOP by applanation of the cornea to a specified area. Based on the Imbert-Fick principle,5 the force to pressure conversion assumes that the IOP is uniquely responsible for the force required to applanate the cornea force.18,19 In reality, the structure of the eye contributes significantly to the applanation force.7–10 Moreover, its contribution will vary based on the specimen. It is known that the measured IOP is affected by material properties and geometry of the eye.7,8,12–14
Through computer modeling simulations, information is gained about tonometry that is not possible from theoretical and experimental consideration. To properly guide these simulations, appropriate assumptions about the physical behavior of cornea tissue were made. The tissue of the cornea is an assembly of cells with complex anatomies and structural properties. In simulation, tissue as a continuum was analyzed, with inhomogeneous material properties. For the purposes of this study, the models were assumed to have three variable material properties: (1) cornea substrate elastic modulus, (2) collagen elastic modulus, and (3) relative collagen thickness. These materials were assigned to particular physical entities in a virtual assembly, and optimized to match real-world behavior.
A basic theory of GAT is the Imbert-Fick principle, as shown in Equation 1. This simple equation states that the reaction force of the eye, F, is a linear function of the IOP, P. The reaction force also depends on the force to deform the cornea tissue, T, and the cross-sectional contact area of the tonometer surface, A. In this study, the normal IOP, P0, was 16.0 mm Hg.
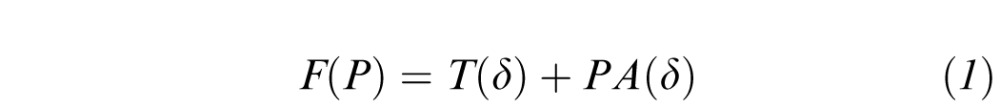 |
The contact area is a function of the displacement depth, δ. In this study, the modeled cornea had a spherical radius of 7.800 mm, and the tonometer had a cylindrical radius of 1.53 mm. This resulted in the maximum displacement of 0.147 mm, and the maximum contact area was 7.354 mm2. The calculation of the contact area, A, as a function of the spherical radius of the cornea, R, and the vertical displacement, δ, is shown in Equation 2.
 |
In GAT, the measured IOP, PGAT, is a linear function of the reaction force. It also depends on a calibration reaction force F(P), which is compared to the normal cornea F550(P0), where the 550 refers to the nominal 550 μm CCT, and P0 is the nominal IOP. This is shown in Equation 3.
 |
The virtual models were designed in Autodesk Inventor LT 2015 and simulated in Autodesk Simulation Mechanical 2015 (Autodesk, San Rafael, CA). Several simulations were executed to determine the sensitivities of the CATS tonometer to various cornea properties. These included: (1) IOP, (2) Young's modulus, (3) CCT, and (4) and central cornea curvature (CC). Each of these were simulated so as to be comparable to results from other studies in this field.14,21–25
Geometric and constitutive models were selected based on the results of previous studies.14,21,25 The material properties were determined via analyses of finite element simulations. The effects of the various geometric aspects of the cornea were measured and studied in previous studies. Since the published corneal material properties vary widely, the specific properties were chosen to approximate known reactions to GAT diagnostics. The force required for applanation of a normal cornea under normal conditions was set near 1.6 g. The cornea was allowed to contribute only 30% of this applanation force under nominal conditions, with the rest coming from the IOP. The finite element mesh density was set so that the perimeter of the applanation area would be precise to within 30 μm, but with a measurement tolerance of no finer than 0.1 g. A nominal cornea has a CCT of 550 μm, central radius of curvature of 7.8 mm, P value of 0.82, and width of 11.0 mm. The P value is a metric of eccentricity of an ellipsoid. A sphere has a P value of 1. A prolate ellipsoid, such as the human cornea, has a P value less than 1.
The sensitivities to the various properties were analyzed parametrically. Those of material and physical properties were simulated with a normal geometry. Those of geometric properties required unique virtual models. The virtual applanation of the normal cornea with the CATS prism is shown in Figure 3.
Figure 3.
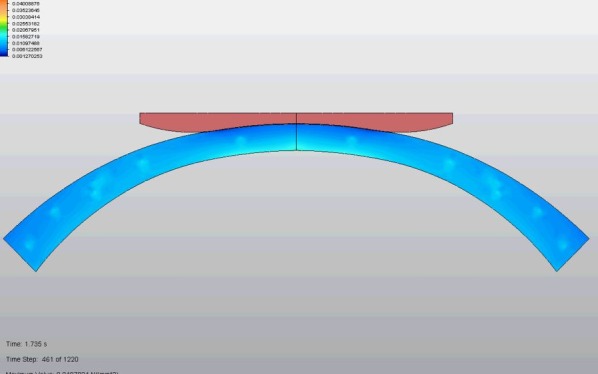
Concave-convex prism surface cross-section of the CATS prism surface in contact with the cornea.
The key to the optimization process was minimization of intracorneal stress during applanating deformation, which occurs at the perimeter of the contact area. Minimization of the maximum stress also reduces the corneal contribution to the measured IOP. Comparison of the GAT and optimized CATS prism designs indicates reduced transition-zone stress concentration. Alternatively, this also is minimization of the second derivative or the rate of change of curvature of the cornea.
The IOP error dependence on tear film is quantitatively minimized, but is not included in the FEA model. Tear film modeling was completed using publications on capillary pressure calculation of a fluid bridge between two curved solids.16,17 The attractive force created by the fluid bridge and associated surface tension of the tear film between the tonometer prism and cornea is reduced in the mathematical model by increasing the contact angle between the cornea and contacting prism in the region of the tear film meniscus with the CATS Tonometer prism. (Fig. 1)
Ultimately, the results of the mathematical modeling theoretically optimized the applanation surface of the tonometer prism. The optimized surface then is incorporated in the GAT design. Several prototypes were constructed and their proper design and function were verified. The CATS prisms then were placed into existing Goldmann tonometer armatures for clinical evaluation.
Human Cadaveric Eye Testing
Bench testing was performed with the CATS Tonometer prism prototypes representative of the device to be marketed. The bench testing consisted of human cadaveric eyes to test for accuracy and repeatability. Specifically, we were examining IOP measurement bias and variability comparing the CATS and GAT prism measurements relative to the manometric and pressure gauge measured IOP as a true value. The objective of this testing was to demonstrate substantial equivalence on a nominal cornea between the series of measurements made by the GAT prism and the CATS prism at each pressure.
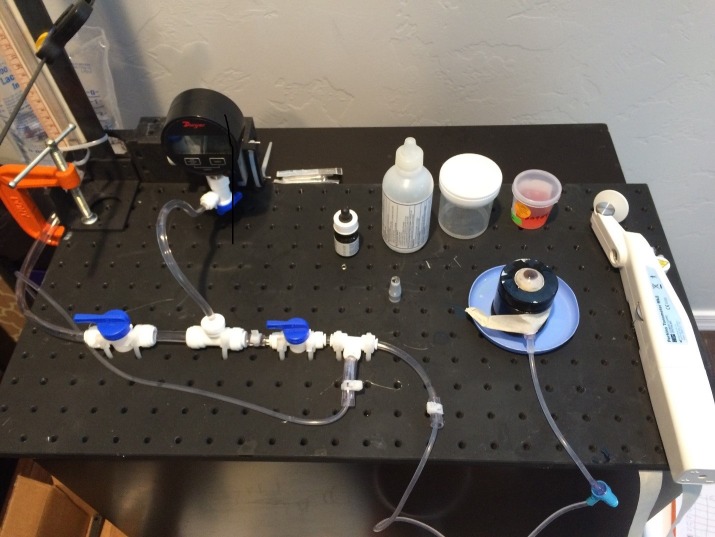
Three enucleated human globes were stabilized in a specially designed chamber for pressurizing a whole globe (Fig. 4) with the cornea exposed.
Figure 4.

Ocular globe stabilizing apparatus for measuring IOP.
Standard biological precautions were followed when handling eye tissue. The pressure was initially set to a true 16 mm Hg via intracameral transducer and the corneal thickness measured via ocular coherence tonometer (OCT). Intraocular pressure measurements were taken using a Perkins-type GAT with the GAT and CATS prisms. Previous studies demonstrated that the Perkins tonometer is clinically equivalent to the slit-lamp mounted GAT.26 Three eyes were individually measured five times with each prism at each of the following nine intracameral pressures (0, 5, 10, 15, 20, 25, 30, 40, 50 mm Hg). Each measurement was rotated counterclockwise 90° from a standard reference axis to account for any astigmatic errors. For example, three cadaver eyes were tested four times (alternately rotating 90°) at a 5 mm Hg intracameral pressure using the GAT and the CATS prisms. A randomization occurred to determine which tonometer prism was used first.
The San Diego Eye Bank (San Diego, CA) provided three freshly enucleated human cadaver globes that were suitable for corneal transplantation. Eyes were stored at 4°C in Optisol chambers until use.27 The cadaver eyes were used on the day of arrival and within hours postmortem. The eyes, ages of the cadavers, and cause of death were recorded. Eyes with a history or evidence of previous anterior segment intraocular surgery (except cataract) or corneal abnormalities were excluded.
Central corneal thickness was measured with a spectral domain ocular coherence tomographer HD-OCT pachymeter (HD-OCT-5000; Zeiss, Jena, Germany). All eyes remained epithelized and hydrated with standard isotonic ocular surgical balanced salt solution (BSS) (Alcon, Ft. Worth, TX). Balanced Salt Solution was used to hydrate the corneal epithelium between measurements before the application of fluorescein solution. A 22-gauge needle with Y-adaptor (Saf-T-Intima, Vialon; Becton, Dickinson and Company, Franklin Lakes, NJ) was inserted into the anterior chamber via a separate scleral approach. Extreme care was taken with all penetrations of the eye to avoid touching the endothelium, iris, or lens. The entire globe was mounted in the eye stabilization device shown in Figure 4 embedded in moisturized gauze facing upward to be measured by the Perkins tonometer (Haag Streit USA, Inc., Mason, OH) fitted with the GAT and CATS prisms. The use of the Perkins tonometer facilitated the globe's upward placement, which minimized measurement errors due to the weight and subsequent distortion of the enucleated globe in the ocular stabilization device. This use of the Perkins in enucleated globes increased the accuracy of all measurements. The needle IV tube was connected to a manometric transducer (Dwyer Instruments, Michigan City, IN), an isotonic sodium chloride solution infusion bottle, and an open-air reference tube (Fig. 5).
Figure 5.
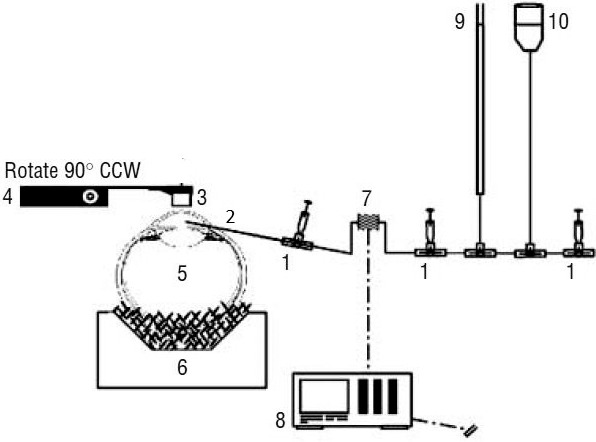
Experimental set up for cadaver eye IOP comparison. 1, stop-cock. 2, intracameral needle. 3, tonometer prism (Goldmann or CATS). 4, Perkins tonometer armature. 5, whole human globe. 6, ocular stabilizing apparatus. 7, pressure transducer. 8, pressure transducer signal pressure read-out in mm Hg. 9, manometer tube pressure measurement. 10, intracameral fluid reservoir.
Multiple stopcocks also were attached to bleed all bubbles from the system, allowing either open or closed stopcock techniques. The transducer and anterior chamber were maintained at the same height. The isotonic sodium chloride solution infusion bottle was attached to a manually driven intravenous pole for bottle height adjustment. After each series of measurements on an eye, the bottle height was lowered to the initial 4.8 cm. The series was only accepted if the initial and closing manometric pressures are within ±1 mm Hg. Figure 6 is the photograph of the schematic in Figure 5.
Figure 6.
Experimental set up for cadaver eye IOP comparison.
Results
Finite element modeling simulations analyzed the effects of corneal properties on the IOP measurement, and made it possible to design of a set of prism contact surfaces to improve measurement fidelity. The design optimization process used the verified FEM to flatten the isobaric curves of the simulated IOP with respect to the error-producing GAT parameters. The objective was to create a prism surface that is independent of corneal thickness, rigidity, corneal curvature, and tear film. The optimal solution, shown in Figure 7 below, is a polynomial approximated central concavity with a peripheral annular convexity that minimizes the effect of the error causing parameters.
Figure 7.
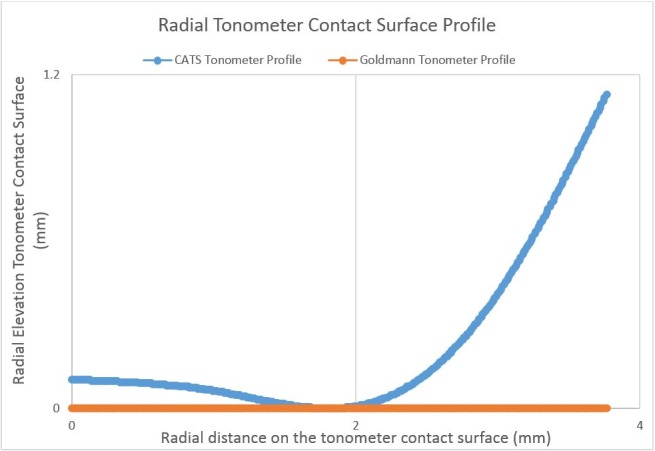
Optimized radial profile of the CATS tonometer prism surface designed to minimize the corneal mechanical and tear film hydrostatic contributions to measured IOP in applanation tonometry.
The polynomial in Figure 7 above was determined to be the ideal design after extensive FEM optimization. This profile yielded a CCT sensitivity of 5.0 mm Hg/mm, which is an improvement of 88.2%, compared to the GAT flat prism surface (see Fig. 8). The contact surface reduces sensitivity to cornea thickness by structurally supporting the central section of tissue, which causes the stress to be more evenly distributed, represented in Figure 9. Von Mises stress is represented for this contour in Figures 8 and 9 as follows: the top bar is the exterior surface, the bottom bar is the interior surface, and the center shape is the sagittal cross-section. The highest stress is produced along the perimeter of the contact surface.
Figure 8.
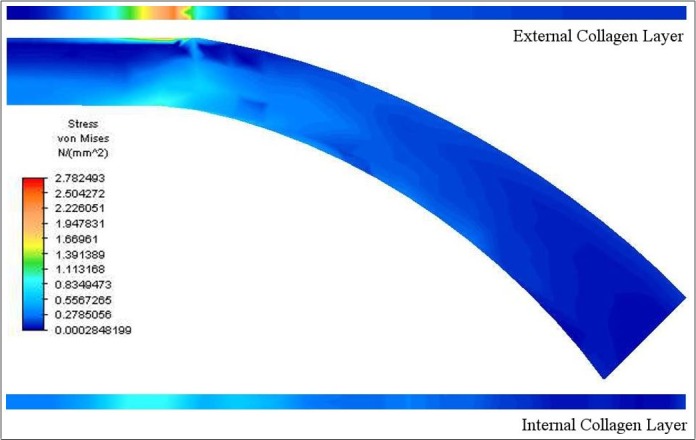
Von Mises stress in cornea applanated to a flat contact surface.
Figure 9.
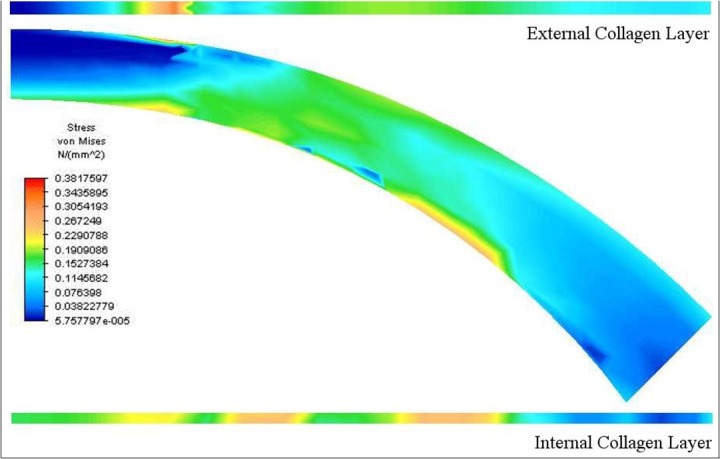
Von Mises stress in applanation with CATS polynomial concave–convex contact surface.
This sensitivity can be further reduced by closely matching the curvature of the prism to that of the cornea. However, one must be careful to avoid perfectly matching the cornea anterior surface, as this would cause the applanation area to be met with zero applied force, thereby providing no useable measurement.
The contact surface of the prism was optimized with FEA. In this process, the surface was modified to minimize the contribution of CCT to the applanation force. The sensitivities of the measured IOP to CCT for the standard GAT and CATS prisms are shown in Figure 10. The shallower slope and lower variance indicate an improvement of measurement accuracy. Finite element analysis indicates that the CATS tonometer has a maximum IOP measurement error of ±2 mm Hg due to variations in subject CCT compared to ± 5 mm Hg with the standard GAT prism.
Figure 10.
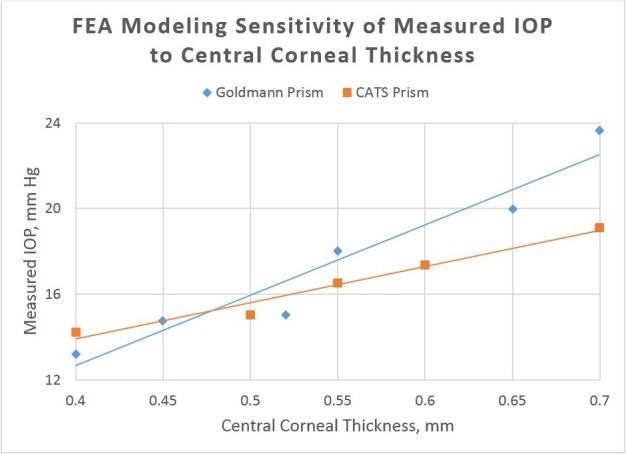
Finite element analysis modeling CCT error sensitivity with constant Young's modulus, constant corneal curvature, and constant IOP (note reduced slope indicating decreased error sensitivity with the CATS prism).
The CATS tonometer also is optimized to reduce sensitivity to an individual's average corneal modulus of elasticity. Young's modulus or corneal rigidity can vary up to an order of magnitude in individuals and previous studies have demonstrated that it is age-dependent.7 The simulated sensitivity of each prisms' IOP measurement to modulus of elasticity is shown in Figure 11. Again, the shallower slope indicates that the CATS prism is less sensitive to this source of error. Finite element analysis of the CATS prism indicates a maximum IOP measurement error of ±2 mm Hg maximum error due to variations of corneal Young's modulus compared to ±8 mm Hg error with the standard GAT prism.
Figure 11.
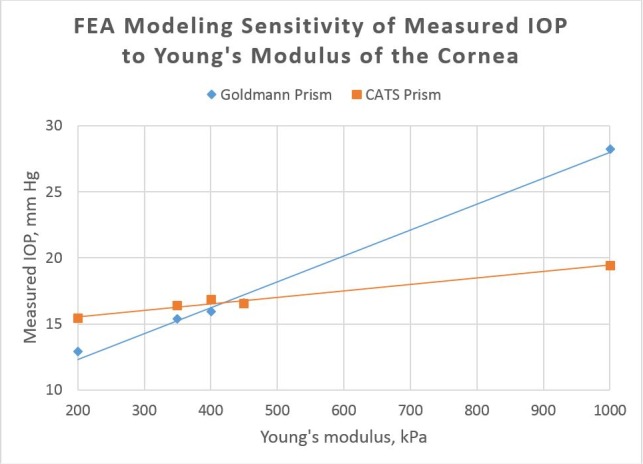
Finite element analysis modeling corneal rigidity (Young's modulus) error sensitivity with constant corneal thickness, curvature, and IOP (note reduced slope indicating decreased error sensitivity with the CATS prism).
The sensitivity to Young's modulus is codependent with CCT; the slope of the sensitivity is proportional to the CCT. Therefore, it follows that corneal rigidity (resistance to deformation) is dependent upon the modulus of elasticity and CCT. Corneal rigidity typically is not corrected for clinically, but could cause more significant error than CCT in the measurement of IOP. This also was demonstrated by Kotecha et al. in 2006.8 The design also was analyzed for a reduction in corneal curvature error dependence. The design effectively reduced the corneal curvature error from ±2.5 mm Hg with the GAT prism to ±1.5 mm Hg with the CATS prism.
The CATS prism theoretically reduces the sensitivity of IOP measurement to the tear film. The effect of the tear film was not included in the finite element analysis. Tear film modeling was completed using publications on capillary pressure calculation of a fluid bridge between two curved solids.16,17 The CATS prism effectively minimized the contribution from capillary tear film adhesion by decreasing the radius of curvature of the CATS surface where the tear film bridged between the two solids prism surface and cornea. The calculated attractive force created by the fluid bridge and associated surface tension of the tear film between the tonometer prism and cornea is reduced approximately 45% for the CATS prism compared to that of the standard GAT. This is achieved by increasing the contact angle between the cornea and contact surface, as illustrated in Figure 12. The range of values shown for the GAT and CATS prisms is due to variations in cornea geometry. This reduction in average attractive force is equivalent to a reduction of IOP measurement error of approximately 1.5 mm Hg.
Figure 12.
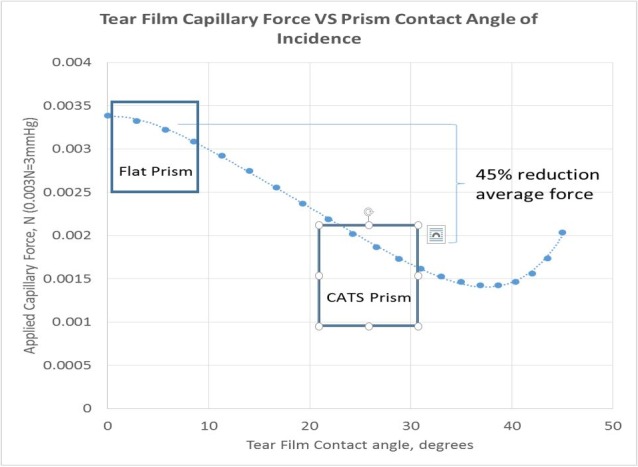
Corneal tear film adhesion force error. Note 45% reduction in tear film error in CATS tonometer prism (0.003 N = 0.3 g force = 3 mm Hg on GAT, approximately).
Human Cadaveric Eye Testing
The three enucleated globes were measured to have a CCT of 641, 786, and 840 μm in eye1, eye2, and eye3, respectively. The intracameral IOP measurements were recorded for each of the cadaveric globes shown in Figures 13A to C. While the GAT prism, CATS prism, and Tonopen measurements were substantially equivalent, the CATS did trend toward improved accuracy (in this limited sample size) when compared to true manometric intracameral pressure. The improved accuracy tended to be in thicker corneas. The increased sensitivity of the CATS tonometer prism also appears in the cadaveric eyes to improve accuracy at low IOP (<10 mm Hg). The purpose of cadaveric manometric referenced testing was to demonstrate general equivalence and repeatability. The altered CCT seen in even fresh human cadaveric eyes also indicates possible alterations in other biomechanical properties, such as Young's modulus. To show, significantly improved IOP measurement capabilities with reduced error requires actual clinical conditions on live human eyes.
Figure 13.
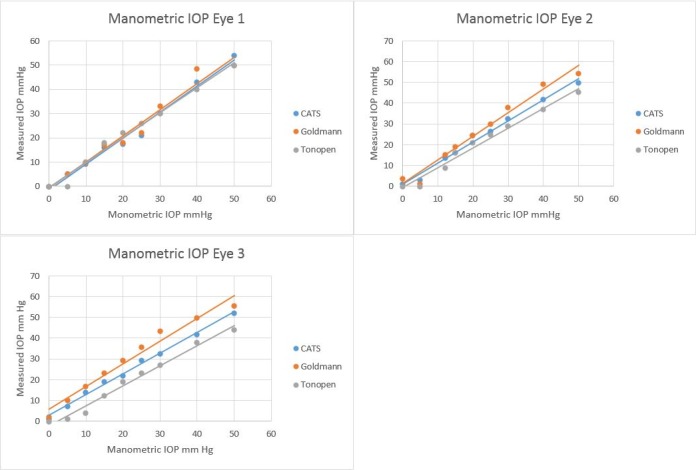
Measurement of IOP in (3) cadaveric human globes (A), (B), and (C), using the GAT prism, CATS prism, and Tonopen versus manometric intracameral IOP.
Discussion
Today virtually all clinicians have the in-office capability to measure IOP with a GAT, as a majority of practitioners consider it the most accurate measurement modality and it is used as the reference tonometer by the Food and Drug Administration (FDA). Furthermore, it is a required protocol if there is any question in the IOP measurements made by other devices. However, GAT errors are well known to the clinician community. As a result, most clinicians also use an expensive pachymeter to measure CCT separately for partial correction of corneal thickness error although this correction is incomplete given the totality of other errors.
The CATS prism optimizes the shape of the flat GAT prism surface, without any change in measurement technique or examination time, and significantly addresses all known mechanical errors in GAT IOP measurements; corneal thickness, corneal curvature, corneal rigidity, and corneal tear film. It is reasonable to predict an additional reduction in scleral expansion error (listed as approximately 2% in the GAT prism) in IOP measurement due to decreased volume displacement of the cornea and aqueous fluid with the CATS prism.
The function of the prism, including force to pressure conversion supplied by the GAT armature, remains unchanged. The optimized CATS prism is designed to measure the same pressure as the flat surface GAT prism under “nominal” conditions. The “nominal” conditions include a standard average corneal thickness, a standard average corneal curvature, a standard average corneal rigidity, and a standard average corneal tear film. However, for approximately 50% of the population, patient cornea variability in each of these parameters has a significant individual and combined error in GAT IOP measurement, as mentioned previously.7–9 Even the errors due to corneal thickness alone, which is but a fraction of the total error, were shown to be potentially sight threatening.10 For this reason, CCT correction has been adopted as a standard of practice.10 Although several other separate measurements and error corrections were proposed, they have been too cumbersome to be adopted clinically.12
The published data indicates that the combined error in IOP measurement can total ±15 to 19 mm Hg for patients at the extremes of corneal thickness, rigidity, curvature, and tear film.7 The most common recognized error is that due to CCT at a published ±7 mm Hg, which is but a small portion of the total possible error. The effect of an error corrected IOP on clinical decisions can be profound. For example, if we only consider corneal thickness GAT error at ±7 mm Hg over a standard distribution of varying thicknesses: The average CCT is approximately 556 ± 40 μm standard deviation.10 Using this distribution, the percentage of people who's IOP error is greater than ±2 mm Hg translates to 46% of all patients with significant IOP error from CCT alone. Using the CATS tonometer, the number of patients in which the IOP error is greater than ± 2 mm Hg drops to 0%. The CATS tonometer prism may negate the need for pachymetry measurement and CCT correction.
The CATS tonometer prism is designed to significantly reduce all of the identified measurement errors by 50% using the exact same measurement apparatus (with a modified prism) and the same technique without any calculations or increased time and at a minimal cost. The expense incurred by the clinician is limited to only the replacement of the prism. The prism is designed to operate in any existing GAT or Perkins tonometer system.
Clinical studies have noted a −3.5 mm Hg bias in the GAT prism when compared to true intracameral manometric pressures and we also found this bias in our FEM analysis.28 The mathematical modeling predicted this bias and the cadaver eye study and preliminary clinical evaluation also indicated this bias. Therefore, to make it equivocal to the GAT prism for an average eye with nominal error characteristics, the decision was made also to include this bias in the CATS prism. This bias equalization in the design means that a nominal eye with average corneal thickness, average corneal rigidity, and average corneal curvature will measure the same IOP with the GAT and CATS prisms. However, The CATS measurements will differ significantly from GAT as the error parameters vary from average, which is significant in likely greater than 50% of the population.7–10,12
The GAT and CATS prisms require a centered cornea on the prism face to accurately measure IOP. The GAT prism will measure applanated mires imaged through the prism anywhere on the flat prism face, but decentration is listed in the GAT instructions for use as necessary for accurate measurement. Conversely, the CATS tonometer, due to its concave–convex, surface will not allow the mires to intersect unless the prism is centered on the cornea. Under the cadaver eye conditions, the prism was easily centered for IOP readings. Within the relatively narrow range that the CATS mires do intersect, the effect on pressure measurement appears negligible. This insensitivity to small amounts of decentration is supported by the minimal variability in repeat measurements equivalent to that seen with the GAT prism. It remains to be seen in clinical studies the effect under saccadic and nystagmus conditions.
A CATS prism clinical study is proposed to demonstrate the relative improvement in IOP measurement between the GAT and CATS prisms when correlated to the known error parameters. The study involves examining the difference in CATS and GAT measurements in correlation to the individual error parameter (i.e., CCT). An additional clinical study has been proposed to determine the absolute IOP measurement improvement with the CATS prism using an intracameral cannulated pressure transducer placed in the anterior chamber during cataract surgery.
Current clinical practice does not correct for errors due to corneal rigidity, curvature, and tear film. However, the CATS tonometer demonstrates the capacity to correct for these errors. This is a significant improvement in the number of patients who otherwise would be at risk due to inaccurate IOP measurement and subsequent undertreatment or overtreatment. Increasing the fidelity of IOP measurement greatly improves patient care and safety and significantly reduces healthcare cost. The CATS prism can provide a single error-corrected measurement with no additional measurement, calculation, or interpretation error.
Acknowledgments
Supported in part by NIH SBIR Grant R43 EY026821-01 and Arizona Eye Consultants, Tucson, AZ with extensive facilities use. All testing according to the Declaration of Helsinki document on human research ethics.
Disclosure: S. McCafferty, Intuor Technologies (I, E); G. Lim, Intuor Technologies (E); W. Duncan, Intuor Technologies (E); E. Enikov, None; J. Schwiegerling, Intuor Technologies (I)
References
- 1.May, 2014. Bureau of Labor Statistics, United States, - Occupational statistics. 29-1041 Optometrists.
- 2. Holden B,, Resnikoff S. The role of optometry in vision 2020. Community Eye Health. 2002; 15: 33–36. [PMC free article] [PubMed] [Google Scholar]
- 3. Quigley H,, Broman T. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006; 90: 262–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Susanna R, Jr,, De Moraes CG,, Cioffi GA,, Ritch R. Why do people (still) go blind from glaucoma? Trans Vis Sci Tech. 2015; 4: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Goldmann H,, Schmidt T. Uber Applanationstonometrie. Ophthalmologica. 1957; 134: 221. [DOI] [PubMed] [Google Scholar]
- 6. Holden B. The role of optometry in vision 2020. Community Eye Health. 2005; 10: 3–8. [PMC free article] [PubMed] [Google Scholar]
- 7. Liu J,, Roberts CJ. Influence of cornea biomechanical properties on intraocular pressure measurement: quantitative analysis. J Cataract Refract Surg. 2005; 31: 146–155. [DOI] [PubMed] [Google Scholar]
- 8. Kotecha A,, Elsheikh A,, Roberts C,, Haogang Z,, Garway-Heath D. Corneal thickness- and age related biomechanical properties of the cornea measured with the ocular response analyzer. Invest Ophthalmol Vis Sci. 2006; 47: 5337–5347. [DOI] [PubMed] [Google Scholar]
- 9. Whitacre M,, Stein R. Sources of error with use of Goldmann-type tonometers. Surv Ophthalmol. 2002; 38: 1–30. [DOI] [PubMed] [Google Scholar]
- 10. Kass M,, Heuer D,, Higginbotham E,, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002; 120: 701–713. [DOI] [PubMed] [Google Scholar]
- 11. McCafferty SJ,, Schwiegerling JT,, Enikov ET. Corneal surface asphericity, roughness, and transverse contraction after uniform scanning excimer laser ablation. Invest Ophthalmol Vis Sci. 2012; 53: 1296–1305. [DOI] [PubMed] [Google Scholar]
- 12. Elsheikh A,, Alhasso D,, Gunvant P,, Garway-Heath D. Multiparameter correction equation for Goldmann applanation tonometry. Optom Vis Sci. 2011; 88: E102–E112. [DOI] [PubMed] [Google Scholar]
- 13. Neuburger M,, Maier P,, Böhringer D,, Reinhard T,, Jordan J. The impact of corneal edema on intraocular pressure measurements using goldmann applanation tonometry Tono-Pen XL, iCare, and ORA: an in vitro model. J Glaucoma. 2013; 22: 584–590. [DOI] [PubMed] [Google Scholar]
- 14. Orssengo G,, Pye D. Determination of the true intraocular pressure and modulus of elasticity of the human cornea in vivo. Bull Math Biol. 1999; 61: 551–572. [DOI] [PubMed] [Google Scholar]
- 15. McCafferty SJ,, Schwiegerling JT,, Enikov ET. Thermal load from a CO2 laser radiant energy source induces changes in corneal surface asphericity roughness. Invest Ophthalmol Vis Sci. 2012; 53: 4279–4288. [DOI] [PubMed] [Google Scholar]
- 16. Tselishchev Y,, Val'tsifer V. Influence of the type of contact between particles joined by a liquid bridge on the capillary cohesive forces. Colloid J. 2003; 65: 385–389. [Google Scholar]
- 17. Orr F,, Scriven L,, Rivas A. Pendular rings between solids: meniscus properties and capillary force. J Fluid Mech. 1975; 67: 723–742. [Google Scholar]
- 18. Tesser P. Applanation area in Goldmann applanation tonometry. Arch Ophthalmol. 2006; 124: 1664. [DOI] [PubMed] [Google Scholar]
- 19. Moses R. The Goldmann applanation tonometer. Am J Ophthalmol. 1958; 46: 865–869. [DOI] [PubMed] [Google Scholar]
- 20. Pandolfi A,, Holzapfel GA. Three-dimensional modeling and computational analysis of the human cornea considering distributed collagen fibril orientations. J Biomed Eng. 2008; 130: 1–12. [DOI] [PubMed] [Google Scholar]
- 21. Elsheikh A,, Ross S,, Alhasso D,, Rama P. Numerical study of the effect of cornea layered structure on ocular biomechanics. Curr Eye Res. 2009; 34: 26–35. [DOI] [PubMed] [Google Scholar]
- 22. Kling S,, Marcos S. Finite element modeling of intrastomal ring segment implantation into a hyperelastic cornea. Invest Ophthalmol Vis Sci. 2013; 54: 881–889. [DOI] [PubMed] [Google Scholar]
- 23. Elsheikh A,, Wang D,, Kotecha A,, Brown M,, Garway-Heath D. Evaluation of Goldmann applanation tonometry using a nonlinear finite element ocular model. Ann Biomed Eng. 2006; 34: 1628–1640. [DOI] [PubMed] [Google Scholar]
- 24. Sr'odka W. Biomechanical model of the human eyeball and its applications. Optica Applicata. 2009; 39: 401–415. [Google Scholar]
- 25. Luce D. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg. 2005; 31: 156–162. [DOI] [PubMed] [Google Scholar]
- 26. Schneider E,, Grehn F. Intraocular pressure measurement: comparison of dynamic contour tonometry and Goldmann applanation tonometry. J Glaucoma. 2006; 15: 2–6. [DOI] [PubMed] [Google Scholar]
- 27. Kniestedt C,, Nee M,, Stamper RL. Dynamic contour tonometry: a comparative study on human cadaver eyes. Arch Ophthalmol. 2004; 122: 1287–1293. [DOI] [PubMed] [Google Scholar]
- 28. A-Yong Y,, Su-Fang D,, Yun EZ,, et al. Correlation between corneal biomechanical properties, applanation tonometry and direct intracameral tonometry. Br J Ophthalmol. 2012; 96: 640–644. [DOI] [PubMed] [Google Scholar]