Abstract
This paper describes the use of clinician‐performed ultrasound to detect sternal fractures in trauma patients. It is a pictorial essay that describes the ultrasound technique, the normal anatomy and ultrasound findings, variants, potential pitfalls and the appearance of fractures when they occur in both children and adults.
Keywords: sternum, sternal fracture, ultrasound, ultrasonography
Introduction
Focused Assessment with Sonography for Trauma (FAST) has an established role in the emergency evaluation of trauma patients to allow the rapid detection of hemoperitoneum and pericardial effusions 1 . More recently, bedside ultrasonography has become accepted for the detection of pneumothorax and hemothorax in trauma patients (‘extended’ FAST or EFAST) 2 . The use of clinician‐performed ultrasound to detect fractures in various settings has also been described.
Sternal fractures are not an uncommon injury in patients involved in motor vehicle accidents, where the seatbelt or steering wheel may impact the sternum. Small studies published to date suggest that ultrasound is at least as good (if not better) than the more traditional lateral sternal radiograph to diagnose sternal fractures.
The increasing availability of bedside ultrasound in the emergency department for FAST and EFAST examination, and the ease of rapid and accurate sternal assessment make ultrasound an attractive option to confirm or exclude sternal fractures in trauma patients.
This paper describes the use of clinician‐performed ultrasound to detect sternal fractures in these patients. It describes the ultrasound technique, the normal ultrasound findings, variants, potential pitfalls and the appearance when fractures occur.
Methods
The Medline (1980 to February 2010) database was searched using MeSH and keywords: “ultrasound” or “ultrasonography” or “management” and “sternum” or “sternal” and “fracture”. The references of relevant papers were manually searched and standard emergency medicine and surgical textbooks were reviewed using MD Consult (www.mdconsult.com) to identify further relevant articles. Some papers were not published in the English language and only the abstracts were reviewed.
Sternal fractures
Sternal fractures most commonly result from motor vehicle crashes, particularly in those wearing seatbelts 3 – 5 . Falls and direct violence account for a minority of cases 3 – 5 . Mechanisms of sternal fracture include direct trauma, indirect trauma (e.g. cervical compression, sometimes associated with thoracic crush fractures), or the action of opposing muscle groups 5 – 6 .
An isolated sternal fracture is generally a benign injury; associated cardiac and aortic injuries are rare 3 , 4 , 7 , 8 . In isolated sternal fractures a normal electrocardiograph (ECG) and chest radiograph is thought to rule out significant complications 8 . Treatment of sternal fractures is generally conservative if there are no coexistent injuries, and reduction is rarely required 5 , 9 . Pain requiring analgesia persists for a mean of 11 weeks 5 , 9 . The clinically well patient with a normal ECG and the absence of underlying cardiorespiratory disease does not require hospital admission 3 , 7 , 10 , 11 .
In contrast, serious complications may occur in the patient with multiple coexisting traumatic injuries and further imaging (e.g. CT chest) should be considered 4 , 5 . Such complications include pulmonary contusion, myocardial contusion and laceration, pericardial effusion, flail chest and bone marrow embolisation 4 , 5 . Recinos, et al. found associated rib fractures in nearly half of patients with a sternal fracture, as well as significant complications such as cardiac contusion (8%) and aortic injury (4%) 4 .
Sternal fractures are traditionally visualised on a lateral chest radiograph. Ideally the penetrance used should be greater than a standard lateral chest radiograph to better appreciate sternal fractures 5 . Lateral chest radiographs are often difficult to obtain in a trauma patient, particularly if there are multiple injuries.
Current evidence consisting of small prospective and retrospective studies suggest that sonographic examination of sternal fractures is at least as sensitive as conventional radiography, and may be up to twice as sensitive 12 – 15 . It also appears to outperform bone scans when the ultrasound is performed by experts 14 .
It has been shown that generally isolated sternal fractures have little clinical relevance, however occasionally, long term effects such as non‐union, painful pseudoarthroses and overlap deformities occur. These may require delayed surgical repair 16 . Two articles claim that ultrasound may not provide an accurate indication of the grade of a sternal fracture 12 , 13 . This is not surprising as ultrasound is only able to evaluate the outer cortex of the sternum. In our experience however there is little doubt that visual assessment of the fracture can ascertain the degree of displacement and angulation of the outer cortex and, if these are significant, the fracture is likely to involve both cortices. In addition if there is independent movement of the sternum of either side of the fracture site through the respiratory cycle, it is reasonable to assume the fracture involves both cortices.
Ultrasound assessment of sternal fractures is rapid, the median time for assessment was 46 seconds (range 32–112 seconds) in an audit of 20 scans in our department.
Anatomy
The anatomy and development of the sternum should be considered when assessing potential sternal injuries 5 , 17 . The sternum has three parts, the manubrium, the body of the sternum and the xiphoid process (Figures 1 and 2).
Figure 1.
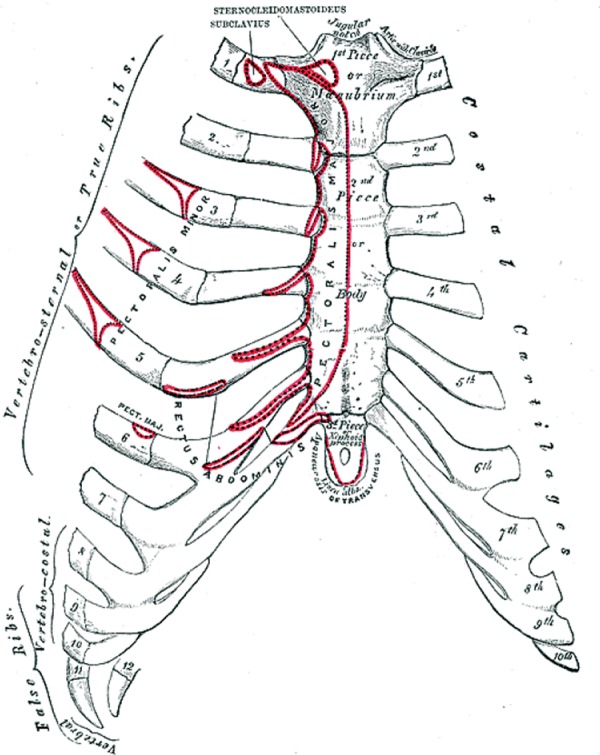
The anterior surface of the sternum and costal cartilages 18 .
Figure 2.
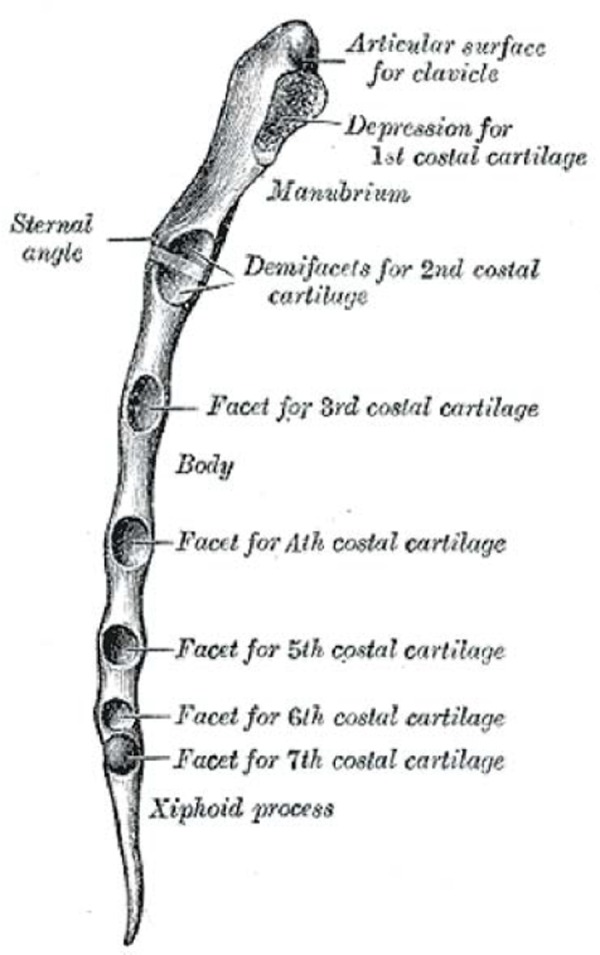
Lateral view of the sternum 18 .
The manubrium is uppermost, its concave upper margin forming the jugular notch. It forms the anterior wall of the superior mediastinum, and has upper angles that form the sternoclavicular joints. It is connected to the body of the sternum by a secondary cartilaginous joint (the sternal angle, or angle of Louis) at the level of the second costal cartilages.
The body of the sternum has lateral articular facets for the lower part of the second costal cartilages and the third to seventh costal cartilages. The sternum has numerous muscular and ligamentous attachments and is closely related to important structures. It overlies the mediastinum including the heart and great vessels, as well as the trachea and the medial aspects of the lungs.
The sternum is formed as two cartilaginous plates that fuse in the midline during fetal development 5 , 17 . There are a variable number of primary ossification centres in the manubrium and in each of the four parts (sternebrae) of the body of the sternum (Figure 3). The double ossification centres merge, but fusion of the sternebrae may be delayed until adulthood. Similarly, the xiphisternum may not ossify until adulthood and its symphysis with the sternal body may not ossify until middle age.
Figure 3.
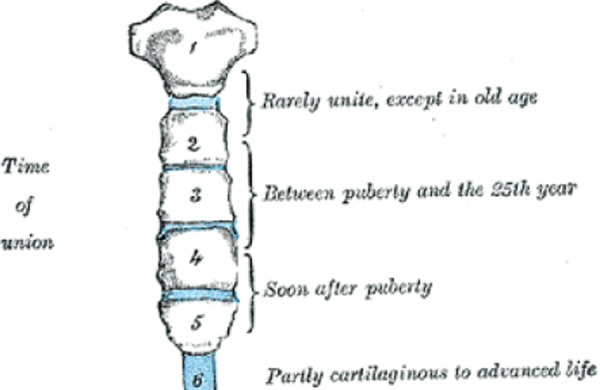
Development of the sternum; the sternebrae 18 .
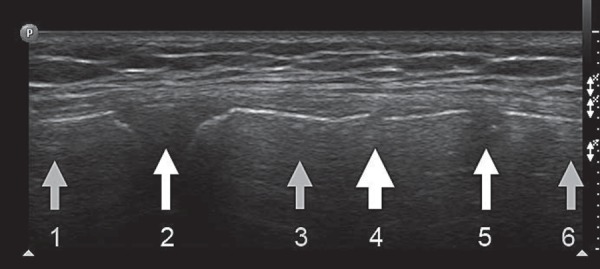
Even after complete ossification it is not uncommon for subtle transverse ridges to remain across the sternum at the level of the third, fourth and occasionally fifth costal cartilage articular facets (Figure 4).
Figure 4.
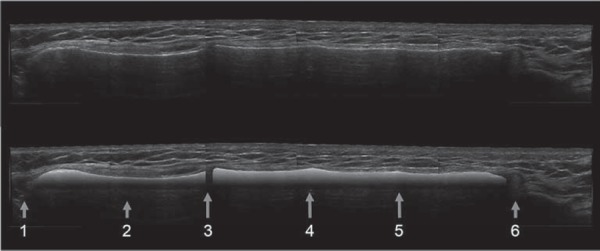
Ultrasound of normal adult sternum (longitudinal composite view). The anterior cortex has been highlighted in the lower image. (1) Jugular notch; (2) manubrium; (3) sternomanubrial junction (4) ridge at level of 3rd costal cartilage (5) ridge at level of 4th costal cartilage (6) xiphisternum.
Sternal anomalies include failure of midline fusion, when a sternal fissure or foramen may result (Figure 7).
Figure 7.
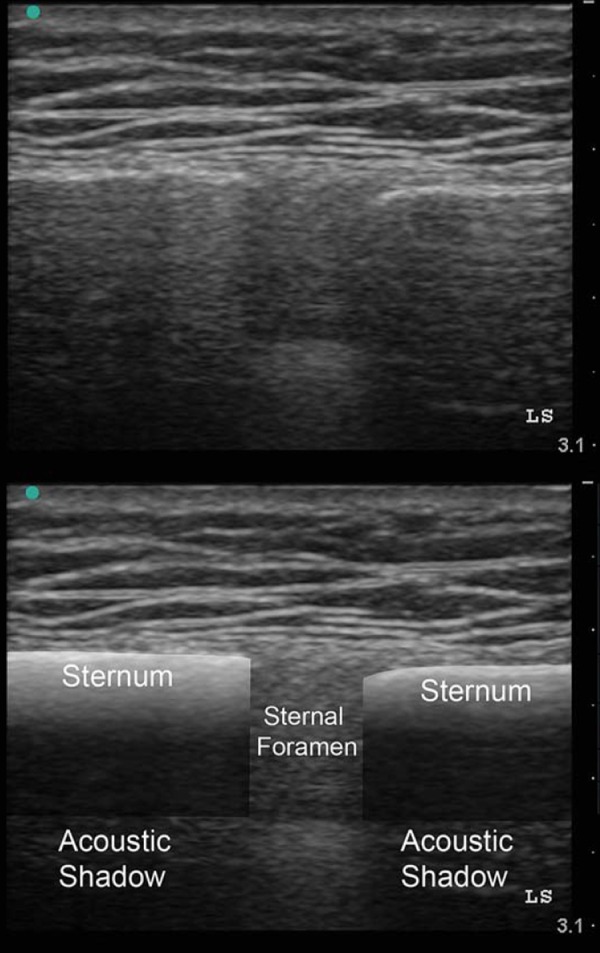
Sternal foramen.
The sternum terminates inferiorly as the xiphoid process, which attaches to the linea alba at the level of the 10th or 11th thoracic vertebra.
Ultrasound technique and appearance
Ultrasound evaluation of the sternum may be performed when there is clinical suspicion of a sternal fracture based on mechanism of injury and clinical findings (e.g. local pain and tenderness, deformity, contusion and/or crepitus).
The anterior cortex of the manubrium and sternum will be parallel with the skin. It will be relatively superficial, echogenic, and demonstrate posterior acoustic shadowing. This means it is not possible to make a direct evaluation of the posterior cortex. Ultrasound will be transmitted through cartilaginous structures such as the sternomanubrial angle and any cartilaginous plates between ossification centres in children. It will also be transmitted through any rarer congenital defects in the sternum such as sternal foramen. At these sites moving mediastinal structures (such as the heart) may be visualised.
Our recommendations for ultrasound evaluation of the sternum are:
Use a linear array high‐frequency ultrasound transducer with the patient in the supine position.
Use a musculoskeletal or small parts preset with a high frequency, superficial focal zone and shallow depth setting.
Align the probe longitudinally over the sternum after application of ultrasound transmission gel.
Adjust gain settings to ensure that the highly echogenic cortex is a clearly visible linear structure.
Move the probe caudally from the jugular notch to the xiphisternum to ensure the entire surface of the sternum is assessed (Figures 4 and 8).
Figure 8.
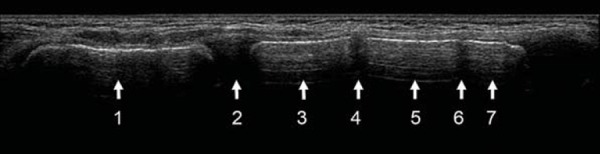
Normal paediatric sternum.
This is a longitudinal panoramic ultrasound view of the sternum of a 6 year‐old. (1) Manubrium; (2) sternomanubrial junction; (3) 1st sternebra; (4) intersternebral cartilaginous junction; (5) 2nd sternebra, (6) intersternebral cartilaginous junction; (7) 3rd sternebra.
Figures 9a–g.
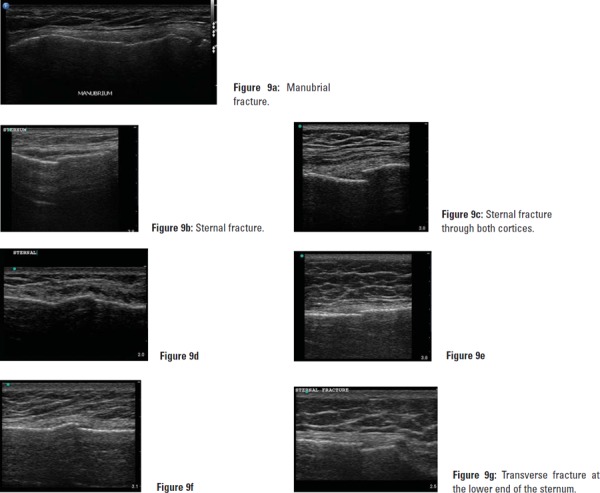
Manubrial and sternal fractures in adults.
A step in the cortex at the site of maximal tenderness, running transversely across the sternum is likely to be a fracture. If the fracture traverses both cortices the proximal and distal portions may move independently through the respiratory cycle.
Figure 9.
Paediatric sternal fracture. Here a step is seen in the anterior cortex of the first sternebrae. This 9 year‐old child had been in a car accident, was wearing a seatbelt and complained of pain and tenderness at exactly the site of the cortical step. (1) Manubrium; (2) sternomanubrial junction; (3) 1st sternebra; (4) fracture; (5) cartilaginous junction; (6) 2nd sternebra.
One may repeat the investigation with the probe orientated for transverse views however this is not essential (Figures 5 and 6).
Figure 5.
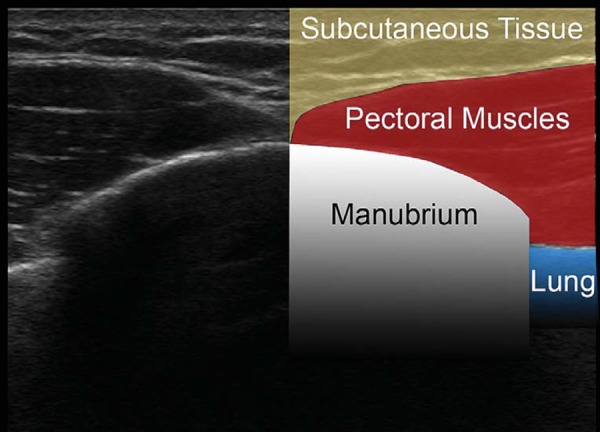
Transverse ultrasound image of the manubrium.
Figure 6.
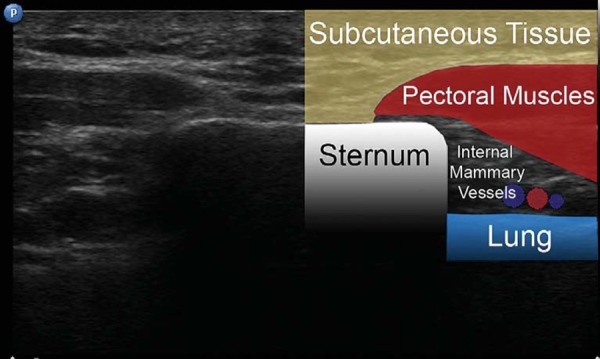
Transverse ultrasound image of the sternum.
A sternal foramen is a round or ovoid congenital defect in the body of the sternum, resulting from incomplete fusion of the ossification centres. Estimated prevalence is 4.5% 19 .
Ultrasound appearance of fractures
Sternal fractures almost always run transversely or obliquely across the sternum and are detected with the ultrasound probe in the longitudinal axis. A sternal fracture is diagnosed if a discontinuity or step in the linear sternal cortex is demonstrated. If there is a clear step, or if the two parts of the sternum on either side of the fracture move independently with respiration as is often the case, a grade 3 or 4 sternal fracture (involving both cortices) has occurred.
Tips and pitfalls
Correlate the ultrasound findings with your clinical impression. A fracture will be at the site of maximal tenderness.
Assessment should not be painful – minimal pressure is needed if generous amounts of ultrasound gel is used.
Inadequate views may result from extensive surgical emphysema.
Avoid misinterpreting the sternomanubrial angle or the xiphisternal junction as fractures – correlate clinically.
Do not mistake sites of incomplete fusion for fractures. These sites occur at the insertion of the costal cartilages in children and young adults (Figure 3). The ultrasound appearance may be one of a cartilaginous junction such as at the sternomanubrial angle (Figure 8).
After fusion has occurred many people have up to three transverse ridges running across the sternum at the levels of the third, fourth and fifth costal cartilage articular facets. Move the probe laterally to determine whether the costal cartilage arises at the level of the ridge. Careful ultrasound examination will demonstrate there is a ridge running across the sternum at these levels rather than a sharp step or break in the cortex (Figure 4).
Incomplete fusion of the inferior end of the sternum may result in a perforated or bifid xiphisternum and sternal fissures or foramina may persist from the incomplete fusion of ossification centres (Figure 7).
Conclusion
Ultrasound evaluation of sternal fractures is a rapid and clinically useful bedside investigation that may be easily performed by emergency physicians assessing trauma patients using the approach described. It is important to understand the development and the variations in normal anatomy of the sternum to avoid either missing or incorrectly diagnosing sternal fractures.
Acknowledgements
Both authors contributed significantly to the creation of this paper. Chris Nickson performed the literature review, assisted with gaining images for the study, and did the initial write up.
James Rippey conceived the idea, gained the images, adjusted them for publication, proof read, amended the paper and then submitted it for publication. James Rippey is on the editorial board of the Australasian Journal of Ultrasound in Medicine.
References
- 1. Rose JS. Ultrasound in abdominal trauma. Emerg Med Clin North Am 2004; 22(3): 581–99, vii. [DOI] [PubMed] [Google Scholar]
- 2. McGahan JP, Richards J, Fogata ML. Emergency ultrasound in trauma patients. Radiol Clin North Am 2004; 42 (2): 417–25. [DOI] [PubMed] [Google Scholar]
- 3. Brookes JG, Dunn RJ, Rogers IR. Sternal fractures: a retrospective analysis of 272 cases. J Trauma 1993; 35 (1): 46–54. [DOI] [PubMed] [Google Scholar]
- 4. Recinos G, Inaba K, Dubose J, Barmparas G, Teixeira PG, Talving P, et al. Epidemiology of sternal fractures. Am Surg 2009; 75 (5): 401–4. [PubMed] [Google Scholar]
- 5. Mazzocca AD, Garretson R, Romeo AA. Section I: Sternum and Rib Fractures in Adults and Children. In: DeLee JC, Drez D, Miller MD, editors. DeLee and Drez's Orthopaedic Sports Medicine. 2nd ed. Philadelphia: Elsevier Science; 2003. [Google Scholar]
- 6. Fowler AW. Flexion‐compression injury of the sternum. J Bone Joint Surg Br 1957; 39: 487–97. [DOI] [PubMed] [Google Scholar]
- 7. Bar I, Friedman T, Rudis E, Shargal Y, Friedman M, Elami A. Isolated sternal fracture – a benign condition? Isr Med Assoc J 2003; 5 (2): 105–6. [PubMed] [Google Scholar]
- 8. Wright SW. Myth of the dangerous sternal fracture. Ann Emerg Med 1993; 22 (10): 1589–92. [DOI] [PubMed] [Google Scholar]
- 9. de Oliveira M, Hassan TB, Sebewufu R, Finlay D, Quinton DN. Long‐term morbidity in patients suffering a sternal fracture following discharge from the A and E department. Injury 1998; 29 (8): 609‐12. [DOI] [PubMed] [Google Scholar]
- 10. Jones A. Towards evidence based emergency medicine: best BETS from the Manchester Royal Infirmary. Admission of isolated sternal fracture for observation. J Accid Emerg Med 1998; 15 (4): 227–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sadaba JR, Oswal D, Munsch CM. Management of isolated sternal fractures: determining the risk of blunt cardiac injury. Ann R Coll Surg Engl 2000; 82 (3): 162–6. [PMC free article] [PubMed] [Google Scholar]
- 12. Engin G, Yekeler E, Guloglu R, Acunas B, Acunas G. US versus conventional radiography in the diagnosis of sternal fractures. Acta Radiol 2000; 41 (3): 296–9. [DOI] [PubMed] [Google Scholar]
- 13. Hendrich C, Finkewitz U, Berner W. Diagnostic value of ultrasonography and conventional radiography for the assessment of sternal fractures. Injury 1995; 26 (9): 601–4. [DOI] [PubMed] [Google Scholar]
- 14. Jin W, Yang DM, Kim HC, Ryu KN. Diagnostic values of sonography for assessment of sternal fractures compared with conventional radiography and bone scans. J Ultrasound Med 2006; 25 (10): 1263–8; quiz 9–70. [DOI] [PubMed] [Google Scholar]
- 15. Mahlfeld A, Franke J, Mahlfeld K. Ultrasound diagnosis of sternum fractures. Zentralbl Chir 2001; 126 (1): 62–4. [DOI] [PubMed] [Google Scholar]
- 16. Johnson I, Branfoot T. Sternal fracture – a modern review. Arch Emerg Med 1993; 10 (1): 24–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sinnatamby CS. Last's Anatomy: Regional and Applied. 10th ed. Edinburgh: Churchill Livingstone; 1999. [Google Scholar]
- 18. Gray, H . Anatomy of the Human Body. Philadelphia: Lea & Febiger; 1918. [Google Scholar]
- 19. Yekeler E, Tunaci M, Tunaci A, Dursun M, Acunas G. Frequency of sternal variations and anomalies evaluated by MDCT. Am J Roentgenol 2006; 186: 956–60. [DOI] [PubMed] [Google Scholar]


