Abstract
Buerger's disease is a progressive, nonatherosclerotic, segmental inflammatory vasoocclusive disease of unknown aetiology 1 – 9 , affecting the small and medium sized arteries, veins and nerves and is often bilateral 5 – 7 . The normal structure of the vessel wall is usually preserved, including the internal elastic lamina and media.
Buerger's disease predominantly affects male cigarette smokers 1 – 3 , 8 with 11%–23% of disease distribution in females 6 – 7 .
Buerger's disease remains largely a clinicopathologic entity highlighting the importance of the sonographer's role to obtain a comprehensive clinical history and clinical examination. The combination of clinical assessment and the distinctive appearance of vessels affected by Bueger's disease on colour duplex ultrasound provide a useful tool for correct diagnosis.
Keywords: Buerger's disease, claudication, clinical, digits, ischaemia, smoking, ultrasound assessment
Introduction
Buerger's disease is a progressive, nonatherosclerotic, segmental inflammatory vasoocclusive disease of unknown aetiology 1 – 9 , affecting the small and medium sized arteries, veins and nerves and is often bilateral 5 , 7 where inflammatory thrombi may affect both the arteries and veins 5 . This disorder has been described as an autoimmune response, however the precise triggering antigen has not been discovered 10 , 11 . The normal structure of the vessel wall is usually preserved, including the internal elastic lamina and media. It is this feature that distinguishes Buerger's disease from arteriosclerosis and from other types of systemic vasculitis 3 , 5 (Figures 1a, 1b).
Figures 1a and b.
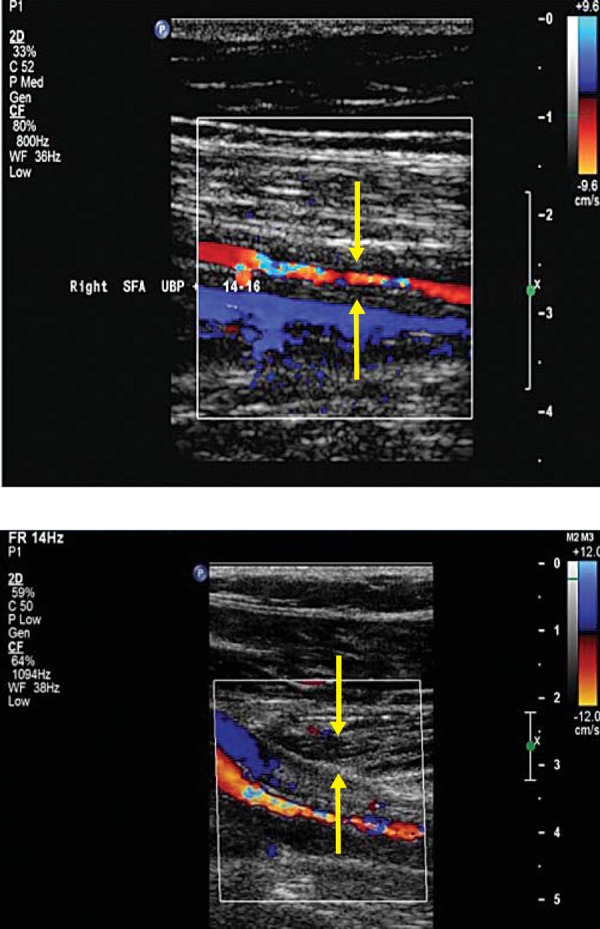
Vasculitis affecting the right mid superficial femoral artery (a) and tibiperoneal trunk (b) of a 52‐year‐old female.
Note: Unlike Buerger's disease, the structure of the vessel wall has been affected with thickening of the vessel wall media (indicated by the arrow).
Buerger's disease predominantly affects male cigarette smokers 1 – 3 , 8 with 11%–23% of disease distribution in females 6 , 7 , in studies of 850 and 112 subjects respectively 2 , 6 , 11 .
The disease progression has a self‐limiting process, with the progression of symptoms influenced by smoking 4 , 10 , and an extremely strong association between heavy use of tobacco with Buerger's disease 3 – 5 . The disease has a high prevalence in people of low socioeconomic class who smoke bidis (homemade cigarettes with raw tobacco found in India) 5 , 12 . More recently, cannabis use has been attributed to the development of a form of vasculitis with very similar features to Buerger's disease 8 , 9 .
The majority of publications view current or past smoking to be a prerequisite for the diagnosis of the condition 1 , 5 – 7 , 11 . A few investigators however believe that Buerger's disease can occur in non‐smokers 2 , 20 , although less than 5% of Buerger's disease patients have been reported as non‐smokers 20 . These cases might be triggered by cold, frostbite, trauma to the extremities or even abuse of sympathomimetic drugs 17 – 20 .
Buerger's disease is a potential cause of lower extremity claudication in young patients, usually with the onset of symptoms occuring before the age of 40 or 45 11 – 15 . Olin, et al. have reported that 7% of 112 patients were older than 60 years old, when first diagnosed 7 . The disease affects both arteries and veins, with typical disease distribution in the upper and lower limbs and, rarely, of the viscera 5 .
Patients may present with symptoms of calf or foot claudication and/or may present with ischaemic extremities 5 . Patients may experience foot claudication within the musculature of the forefoot. This pain may often be mistaken for an orthopaedic problem 5 . As the disease progresses, ischaemic pain at rest and ischemic ulcerations on the toes, feet or fingers may develop 1 .
Shionoya, et al. have published clinical diagnostic criteria which are generally well accepted 4 , 5 , 10 , although not universally 4 , 10 since Buerger's disease remains largely a clinicopathologic entity and there has been a lack of unanimous diagnostic criteria 4 . The distal nature of the disease pattern in Buerger's disease and the involvement of the upper limbs are two major arguments for differentiating Buerger's disease from atherosclerotic arteriopathies 20 .
Case Study
Figures 2a, b and c demonstrate the clinical features of a 42‐year‐old man with known Buerger's disease who had had previous partial right hand digit amputation. He had reduced his smoking but had not ceased completely. He presented to the laboratory with a painful, ischaemic second toe, calf claudication and impotence. He had right resting ankle brachial index of 0.42 and left ankle brachial index of 0.47. Colour duplex ultrasound (CDU) demonstrated patent iliac, femoral and popliteal arteries bilaterally. He had bilateral occlusion of the posterior tibial, peroneal and anterior tibial arteries from approximately the mid calf. Figures 3a and 3b.
Figures 2a, b and c.

42‐year‐old male with Buerger's disease. Note the digital ulceration and ischaemia of the fingers and toes.
Figure 3a.
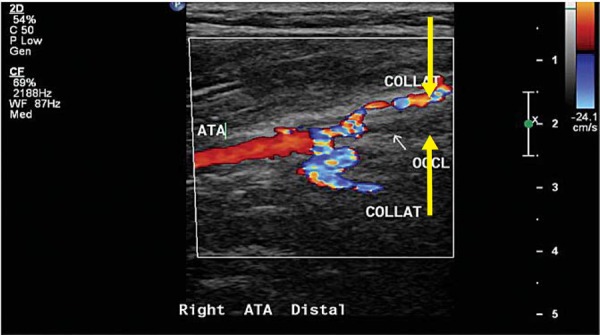
CDU image of the anterior tibial artery in the distal calf just before it occludes with thrombus and a serpiginous course of adjacent collaterals (“corkscrew appearance”). 5 Unlike vasculitis, the occluded vessel walls remain unchanged (indicated by arrows).
Figure 3b.
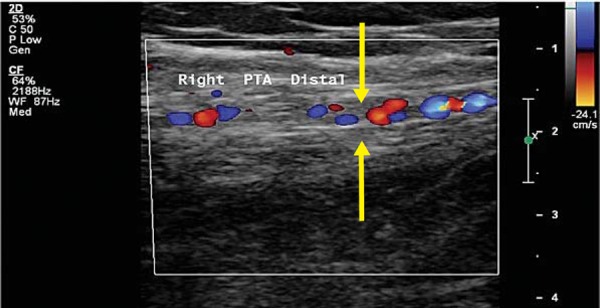
CDU image of an occluded posterior tibial artery with thrombus and serpiginous, collateral flow in and around the vessel. (“corkscrew appearance”). 5 Unlike vasculitis, the occluded vessel walls remain unchanged (indicated by arrows).
Colour duplex ultrasound and clinical assessment of Buerger's disease
Because of the unusual distribution of vascular lesions in Buerger's disease, it is important to combine a clinical assessment of the patient with the CDU findings.
Obtaining a comprehensive clinical history and clinical examination is of paramount importance, since the early stages of this disease may only affect the digits of the hands or feet. Therefore, generally speaking, performing a standard upper or lower extremity arterial duplex alone may not be diagnostic when the disease is in its early stages, because most standard imaging protocols stop at the ankle level in the lower extremity or at the wrists in the upper extremity.
The major CDU abnormalities that may be detected are shown in Table 1. The clinical factors are presented in Table 2, and include the patient's smoking history and careful examination of the upper and lower limbs of the patient.
Table 1.
| Buerger's disease: CDU characteristics |
|---|
| Occlusion of distal calf or pedal arteries |
| Occlusion of forearm, palmar arch or digital arteries |
| Normal appearing arteries proximal to the occlusive lesions |
| Serpiginous or corkscrew collateral development at the level of occlusion |
| Intact vessel wall in the area of thrombotic occlusion, often free of calcification |
Table 2.
| Buerger's disease: clinical diagnotic criteria |
|---|
| Smoking history |
| Onset before the age of 50 years |
| Infrapopliteal artery occlusions |
| Either upper limb involvement or phlebitis migrans |
| Absence of atherosclerotic risk factors other than smoking |
Ankle brachial index measurements are recorded at rest and post‐exercise in accordance to most standard lower extremity CDU imaging protocols. Patients with Buerger's disease will usually have a reduced ankle brachial index with a further reduction following exercise, unless the disease is distal to the level of cuff placement, which is frequently the case. If the disease is distal to the cuff placement, the ankle brachial index may be normal (0.92–1.0) and it will require digital pressure recordings or photoplethysmographic waveform analysis of the toes. A reduction in pressure and/or a dampened or absent waveform may be demonstrated on one or several digits in the presence of digital ischemia related to the disease.
Buerger's disease in the upper extremity is assessed similarly with a wrist to brachial index measurement followed by digital pressure recordings or photoplethysmographic waveform analysis of the fingers and then CDU surveillance of the upper extremity arteries.
A standard upper or lower extremity CDU of the arteries in the affected limb should be performed in all cases. When Buerger's disease is present, CDU may demonstrate thrombotic occlusion of the calf or pedal arteries when assessing the lower limb. In the upper extremity, the radial, ulnar, palmar arch or digital arteries may be occluded. In both instances, the vessels proximal to the diseased segment appear normal. The diseased segment will demonstrate thrombotic occlusion and local collateralisation will often appear serpiginous or corkscrewed 5 in appearance. Other authors have described the angiographic findings as “spiders legs” or “tree roots” 10 .
Conclusion
Buerger's disease is a complex entity and the diagnosis of the condition is dependent upon the fulfillment of clinicopathologic criteria which is generally accepted 4 , 5 , 10 but there has been a lack of unanimous diagnostic criteria 4 . The distal nature of the disease pattern and the involvement of the upper limbs are two major arguments for differentiating Bueger's disease from atherosclerotic arteriopathies 20 .
CDU is a particularly useful imaging tool and can readily identify the distinctively characteristic appearance of vessels affected by Buerger's disease, although the entire clinical picture is of utmost importance.
References
- 1. Mills JL, Porter JM. Buerger's Disease (thromboangiitis obliterans). Ann Vasc Surg 1991; 5 (6): 570–2. [DOI] [PubMed] [Google Scholar]
- 2. Sasaki S, Sakuma M, Kunihara T, Yasuda K. Current trends in thromboangiitis obliterans (Buerger's disease) in women. Am J Surg 1999; 177 (4): 316–20. [DOI] [PubMed] [Google Scholar]
- 3. Lie JT. Visceral Intestinal Buerger's Disease. Int J Cardiol 1998; 66: S249–S256. [DOI] [PubMed] [Google Scholar]
- 4. Shionoya S. Diagnostic criteria of Buerger's disease. Int J Cardiol 1998; 66: S243–S245. [DOI] [PubMed] [Google Scholar]
- 5. Olin JW. Thromboaniitis obliterans (Buerger's disease). N Engl J Med 2000; 343 (12): 864–9. [DOI] [PubMed] [Google Scholar]
- 6. Lie JT. Thromboangiitis obliterans (Buerger's disease) in women. Medicine (Baltimore) 1987; 66: 65–2. [DOI] [PubMed] [Google Scholar]
- 7. Olin JW, Young JR, Graor RA, Ruschhaupt WF, Bartholomew JR. The changing clinical spectrum of thromboangiitis obliterans (Buerger's disease). Circulation 1990; 82 (5): S3–8. [PubMed] [Google Scholar]
- 8. Combemale P, Consort T, Denis‐Thelis L, Estival JL, Dupin M, Kanitakis J. Cannabis arteritis. Br J Dermatol 2005; 151 (1): 166–9. [DOI] [PubMed] [Google Scholar]
- 9. Peyrot I, Gasrsaus AM, Saint‐Cyr I, Quitman O, Sanchez B, Quist D: Cannabis arteritis: a new case report and review of literature. J Eur Acad Dermatol Venereol 2007; 21(3): 388–91. [DOI] [PubMed] [Google Scholar]
- 10. Lazarides MK, Georgiadis GS, Papas TT, Nikolopoulos ES. Diagnostic criteria and treatment of Buerger's disease: a review. Int J Low Extrem Wounds 2006; 5 (2): 89–95. [DOI] [PubMed] [Google Scholar]
- 11. Mills JL. Buerger's disease in the 21st century: clinical features and therapy. Semin Vasc Surg 2003; 16 (3): 179–89. [DOI] [PubMed] [Google Scholar]
- 12. Grove WJ, Stansby GP. Buerger's disease and cigarette smoking in Bangladesh. Ann R Coll Surg Engl 1992; 74: 1115–8. [PMC free article] [PubMed] [Google Scholar]
- 13. Papa MZ, Adar R. A critical look at thromboangiitis obliterans (Buerger's disease). Vasc Surg 1992; 5: 1–18. [Google Scholar]
- 14. Olin JW, Lie JT. Thromboangiitis obliterans (Buerger's disease). In Loscalzo J, Creager MA, Dzau VJ, editors. Vascular Medicine. 2nd ed. Boston: Little, Brown; 1033–49, 996. [Google Scholar]
- 15.Idem. Thromboangiitis obliterans (Buerger's disease) in women. Medicine (Baltimore) 1987; 66: 65–72. [DOI] [PubMed] [Google Scholar]
- 16. Mills JL. Buerger's disease in the modern era. Am J Surg 1987; 154: 123–9. [DOI] [PubMed] [Google Scholar]
- 17. Hagen B, Lohse S. Clinical and radiologic aspects of Buerger's disease. Cardiovasc Intervent Radiol 1984; 7: 283–93. [DOI] [PubMed] [Google Scholar]
- 18. Juergens JL. Thromboangiitis obliterans (Buerger's disease, TAO). In: Juergens JL, Spittel JA, Fairbairn JF, editors. Peripheral vascular diseases. Philadelphia, London, Toronto: WB Saunders; 1980. pp. 469–91. [Google Scholar]
- 19. Hill GL. A rational basis for management of patients with the Buerger syndrome. Br J Surg 1974; 61: 476–81. [DOI] [PubMed] [Google Scholar]
- 20. Puechal X, Fiessinger JN, Thromboangiitis obliterans or Bueger's disease: challenges for the rheumatologist. Rheumatology 2007; 46 (2): 192–9. [DOI] [PubMed] [Google Scholar]


