Abstract
Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome is a rare urogenital anomaly. Patients typically present at puberty, shortly after menarche with increasing pelvic pain, dysmenorrhea and pelvic mass. There may be a known history of unilateral renal agenesis. Diagnosis can usually be established by ultrasound or magnetic resonance imaging. Resection of the vaginal septum is the treatment of choice. Early diagnosis and treatment can relieve symptoms, prevent complications and preserve fertility. We present two cases of OHVIRA syndrome diagnosed by ultrasound to promote recognition of this rare but important condition.
Keywords: Herlyn‐Werner‐Wunderlich syndrome, obstructed hemivagina, OHVIRA syndrome, renal anomaly, ultrasound, uterine didelphys
Introduction
The combination of obstructed hemivagina and uterine didelphys was first reported in 1922. 1 The triad of uterine didelphys with obstructed hemivagina and ipsilateral renal agenesis has been referred to as Herlyn‐Werner‐Wunderlich syndrome with the first paper in English to use this term published in 2006. 2 The acronym OHVIRA (obstructed hemivagina and ipsilateral renal anomaly) syndrome was proposed in 2007 to allow inclusion of other uterine and renal anomalies. 3 The incidence of uterine didelphys related to this syndrome is approximately 1/2,000 to 1/28,000, and it is accompanied by unilateral renal agenesis in 43% of cases. 4 It has been estimated that there would be only four to five cases of uterine didelphys and obstructed hemivagina per year in Australia. 5 Early diagnosis and surgical intervention in OHVIRA syndrome is important to relieve symptoms, prevent complications and preserve future fertility. 6 We present two cases of OHVIRA syndrome seen and managed at our institution to promote recognition of this rare urogenital anomaly.
Cases
1) A 13‐year‐old girl presented to the Emergency Department with worsening lower abdominal pain. This was her third such presentation in nine months. She was known to have an absent right kidney. She had menarche at the age of 11 years with menses lasting 5 to 6 days and irregular 30 to 60 day cycle length. She had worsening dysmenorrhoea requiring treatment. At her first presentation she was admitted with suspected appendicitis. The appendix was found to be normal at surgery and on histopathology. At her second presentation she was treated for a suspected urinary tract infection. Pelvic ultrasound performed in the Medical Imaging Department at her third presentation showed uterine didelphys, right hematometrocolpos (Figure 1) and probable right haematosalpinx (Figure 2). The left hemiuterus appeared normal (Figure 3). The right kidney was absent (Figure 4). Laparoscopy and hysteroscopy revealed normal ovaries and left tube, normal left hemiuterus, enlarged right hemiuterus, right haematosalpinx and a thick longitudinal vaginal septum with right‐sided haematocolpos. The vaginal septum was excised with drainage of 400 milliliters of old blood.
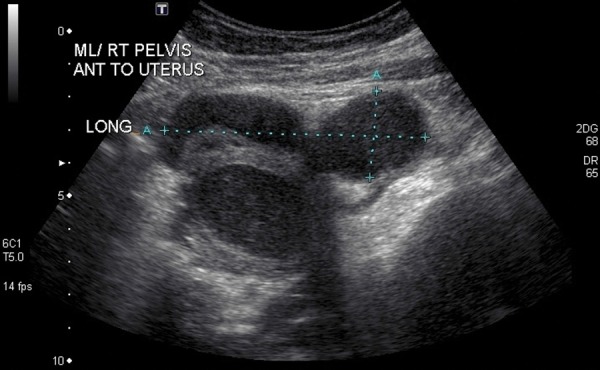
Figure 1.

Sagittal scan showing right hemiuterus with distended cavity and vagina containing echogenic material.
Figure 2.
Sagittal scan showing a tubulocystic collection containing echogenic material arising from the cornu of the right hemiuterus.
Figure 3.

Sagittal scan showing normal left hemiuterus.
Figure 4.

Sagittal scan showing absence of the kidney in the right renal fossa.
The postoperative course was uncomplicated.
2) A 13‐year‐old girl was referred to our hospital for definitive surgical management. She was known to have a congenitally absent left kidney. She had menarche at the age of 12 years. Her menses were gradually getting irregular with worsening dysmenorrhoea despite progestin therapy. Pelvic ultrasound organised by her general practitioner demonstrated uterine didelphys, haematometra of the left uterine cavity, haematocolpos and absent left kidney. Examination under anaesthesia by her private gynecologist showed obstructed non‐communicating hemivagina. Repeat pelvic ultrasound in the Medical Imaging Department confirmed the above findings (Figures 5–8). Examination under anesthesia and hysteroscopy revealed uterine didelphys with left transverse obstructing vaginal septum and haematocolpos. The vaginal septum was excised with drainage of 450 ml of old blood. The postoperative course was uncomplicated.
Figure 5.
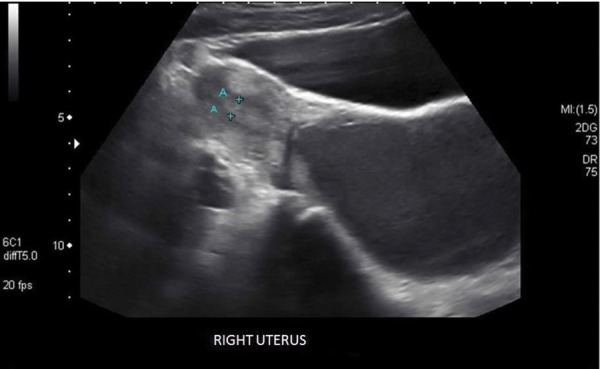
Sagittal scan showing normal right hemiuterus.
Figure 8.

Sagittal scan showing absence of the kidney in the left renal I fossa.
Discussion
The pathogenesis of OHVIRA syndrome is related to anomalous development of both the paramesonephric (Mullerian) and mesonephric (Wolffian) ducts. 7 The Wolffian ducts induce normal Mullerian duct fusion and give origin to the kidneys. Abnormal Wolffian duct development leads to unilateral renal agenesis and imperforate hemivagina associated with OHVIRA syndrome. 8 The Mullerian duct on the side where the Wolffian duct is absent is displaced laterally and cannot fuse with the contralateral Mullerian duct, resulting in uterine didelphys. The contralateral Mullerian duct gives rise to a vagina, whereas the displaced Mullerian duct cannot come into contact with the urogenital sinus and centrally forms a blind sac, leading to an imperforate or obstructed hemivagina. There may be an associated longitudinal or transverse vaginal septum and this was seen in the two cases presented. Renal agenesis is the most common associated renal anomaly and is always seen on the same side as the obstructed hemivagina.
Figure 6.
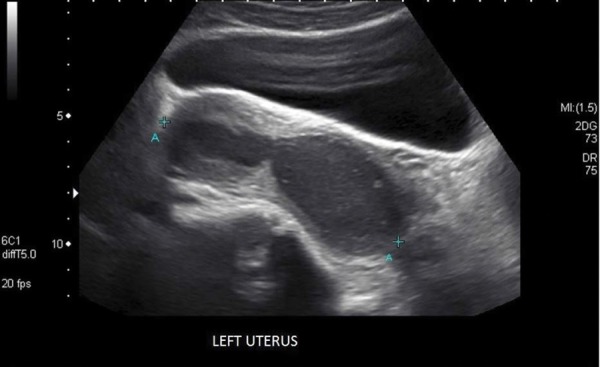
Sagittal scan showing left hemiuterus with distended cavity containing echogenic material.
Figure 7.

Sagittal scan showing distended vagina containing echogenic material.
OHVIRA syndrome is usually discovered at puberty, shortly after menarche because of increasing pelvic pain, dysmenorrhoea and pelvic mass secondary to haematometrocolpos from retained blood in the obstructed hemivagina. 4 It may remain unrecognised initially as regular menstrual flow from the patent unobstructed hemivagina gives the appearance of normal menses, and dysmenorrhoea, if present, is a common complaint in this age group. 7 Symptom relief of dysmenorrhoea with non‐steroidal anti‐inflammatory and oral contraceptive medication may also lead to a delay in diagnosis. 9 The clinical presentation may be variable and non‐specific features such as acute abdominal, 4 , 10 pelvic 9 , 11 or vaginal 12 pain, dysuria, 13 urinary retention, 7 vaginal discharge 14 , 15 and infertility 16 have been reported. The two cases presented were both known to have an absent kidney and this should prompt investigation for Mullerian duct anomalies and vice versa. Associated complications include acute infectious collections and long‐term sequelae such as endometriosis, pelvic adhesions, and infertility. 9 Initial misdiagnosis of OHVIRA syndrome and a significant delay from the time of onset of symptoms to diagnosis have been reported with patients undergoing unnecessary and potentially harmful invasive investigations before appropriate surgery was performed. 5 , 17 – 19
Ultrasonography and magnetic resonance imaging (MRI) are used to diagnose OHVIRA syndrome. Ultrasound is quick, cheap, noninvasive and readily available. 7 , 20 It will generally identify uterine didelphys, haematometrocolpos and unilateral absence of a kidney. The vaginal septum however is difficult to visualise on ultrasound. 7 , 20 MRI is said to be the imaging modality of choice to correctly diagnose OHVIRA syndrome. 9 , 10 , 16 , 18 , 21 It is more sensitive in assessing uterine contour, shape of the uterine cavity, thickness and location of the vaginal septum, type of collection in the obstructed hemivagina and coexisting urinary tract malformations. 9 The two cases presented were diagnosed on ultrasound without the benefit of MRI.
Laparoscopy has been advocated as the gold standard for evaluation of OHVIRA syndrome. 2 , 17 Others suggest that laparoscopy, rather than being performed routinely, be reserved for those cases when the diagnosis is not clear after imaging, when MRI is not available or when there is suspected concurrent intraperitoneal pathology such as endometriosis, adhesions and pelvic infection. 3 , 9 , 15 Laparoscopy was performed in one of the two cases presented because of a probable haematosalpinx seen on ultrasound.
The treatment of choice for OHVIRA syndrome is resection of the vaginal septum in order to reestablish the continuity of the obstructed hemivagina. 6 , 9 , 10 , 17 , 20 This may be performed as a single‐stage or two‐stage procedure. The single stage procedure involves excising the vaginal septum completely and marsupialising the vaginal cuff. The two‐stage procedure involves reducing the haematocolpos first and then excising the remaining septum tissue after a period of wound healing and vaginal remodeling. The latter procedure is considered if there is infection and/or anatomical distortion preventing satisfactory assessment of the vagina for repair. 3 The two cases reported were successfully managed with single stage excision of the vaginal septum.
Conclusion
OHVIRA syndrome should be considered in patients presenting with dysmenorrhoea and a history of renal agenesis. Ultrasound remains a reliable and accurate imaging tool in the diagnosis of this syndrome. Early diagnosis and surgical intervention is important to relieve symptoms, prevent complications and preserve future fertility.
References
- 1. Purslow CE. A case of unilateral haematocolpos, haematometra and haematosalpinx. J Obstet Gynaecol Br Emp 1922; 29: 643. [Google Scholar]
- 2. Gholoum S, Puligandla PS, Hui T, Su W, Quiros E, Laberge JM. Management and Outcome of patients with combined vaginal septum, bifid uterus, and ipsilateral renal agenesis (Herlyn‐Werner‐Wunderlich syndrome). J Pediatr Surg 2006; 4: 987–92. [DOI] [PubMed] [Google Scholar]
- 3. Smith N, Laufer M. Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: management and follow‐up. Fertil Steril 2007; 87: 918–22. [DOI] [PubMed] [Google Scholar]
- 4. Del Vescovo R, Battisti S, Di Paola V, Piccolo CL, Cazzato RL, Sansoni I, Grasso RF, Zobel BB. Herlyn‐Werner‐Wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosis. BMC Med Imaging 2012; 12: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kimble RM, Khoo SK, Baartz D, Kimble RM. The obstructed hemivagina, ipsilateral renal anomaly, uterus didelphys triad. Aust N Z J Obstet Gynaecol 2009; 49: 554–57. [DOI] [PubMed] [Google Scholar]
- 6. Tong J, Zhu L, Lang J. Clinical characteristics of 70 patients with Herlyn‐Werner‐Wunderlich syndrome. Int J Gynaecol Obstet 2013; 121: 173–75. [DOI] [PubMed] [Google Scholar]
- 7. Mandava A, Prabhakar RR, Smitha S. OHVIRA syndrome (obstructed hemivagina and ipsilateral renal anomaly) with uterus didelphys, an unusual presentation. J Pediatr Adolesc Gynecol 2012; 25: e23–25. [DOI] [PubMed] [Google Scholar]
- 8. Orazi C, Lucchetti MC, Schingo PMS, Marchetti P, Ferro F. Herlyn‐Werner‐Wunderlich syndrome: uterus didelphys, blind hemivagina and ipsilateral renal agenesis. Sonographic and MR findings in 11 cases. Pediatr Radiol 2007; 37 (7): 657–65. [DOI] [PubMed] [Google Scholar]
- 9. Sen KK, Balasubramaniam D, Kanagaraj V. Magnetic resonance imaging in obstructive Müllerian anomalies. J Hum Reprod Sci 2013; 6: 162–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gungor Ugurlucan F, Bastu E, Gulsen G, Kurek Eken M, Akhan SE. OHVIRA syndrome presenting with acute abdomen: a case report and review of the literature. Clin Imaging 2014; 38: 357–59. [DOI] [PubMed] [Google Scholar]
- 11. Aveiro AC, Miranda V, Cabral AJ, Nunes S, Paulo F, Freitas C. Herlyn‐Werner‐Wunderlich syndrome: a rare cause of pelvic pain in adolescent girls. BMJ Case Reports 2011; doi: 10.1136/bcr.04.2011.4147. [DOI] [PMC free article] [PubMed]
- 12. Beer WM, Carstairs SD. Herlyn Werner Wunderlich syndrome: an unusual presentation of acute vaginal pain. J Emerg Med 2013; 45: 541–43. [DOI] [PubMed] [Google Scholar]
- 13. Berger‐Chen S, Ritch JM, Kim JH, Evanko J, Hensle TW. An unusual presentation of uterine didelphys and obstructed hemivagina. J Pediatr Adolesc Gynecol 2012; 25: e129–31. [DOI] [PubMed] [Google Scholar]
- 14. Frei KA, Bonel HM, Häberlin FC. Uterus didelphys, obstructed hemivagina and ipsilateral renal agenesis with excessive chronic vaginal discharge. Acta Obstet Gynecol Scand 1999; 78: 460–61. [PubMed] [Google Scholar]
- 15. Lin TB, Hsieh MF, Han SC, Chin WL, Hsueh YL. Obstructed hemivagina and ipsilateral renal anomaly with uterus didelphys and vaginal discharge. Taiwan J Obstet Gynecol 2013; 52: 593–96. [DOI] [PubMed] [Google Scholar]
- 16. Ahmad Z, Goyal A, Das CJ, Deka D, Sharma R. Herlyn‐Werner‐Wunderlich syndrome presenting with infertility: Role of MRI in diagnosis. Indian J Radiol Imaging 2013; 23: 243–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zurawin RK, Dietrich JE, Heard MJ, Edwards CL. Didelphic uterus and obstructed hemivagina with renal agenesis. Case report and review of the literature. J Pediatr Adolesc Gynecol 2004; 17: 137–41. [DOI] [PubMed] [Google Scholar]
- 18. Christianson MS, Yates MM, Woo I, Khafagy A, Garcia JE. L.A. Kolp Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA): diagnostic features and management of a frequently misdiagnosed syndrome. Fertil Steril 2012; 98: S222. [Google Scholar]
- 19. Cardamone S, Creighton C. Obstructed Hemivagina in the Adolescent: A Diagnostic Challenge. J Pediatr Adolesc Gynecol 2014; 27: e62. [Google Scholar]
- 20. Jindal G, Kachhawa S, Meena GL, Dhakar G. Uterus didelphys with unilateral obstructed hemivagina with hematometrocolpos and hematosalpinx with ipsilateral renal agenesis. J Hum Reprod Sci 2009; 2: 87–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nguyen T, Lawrence L, Ratts V, Odem R, Siegel C, Merritt D. Diagnosis and management of didelphic uterus, obstructed hemivagina and ipsilateral renal agenesis (Herlyn‐Werner‐Wunderlich syndrome): the Washington University experience. Fertil Steril 2007; 88: S54. [Google Scholar]


