Abstract
Objective: To compare transabdominal (TA) and transvaginal (TV) ultrasound assessment of cervical length at 16–41 weeks gestation.
Methods: TA and TV ultrasound measurements of cervical length were made on 491 pregnancies of 16–41 weeks gestation. Cervical length was measured from internal to external cervical os. Bland‐Altman plots and Wilcoxon signed rank test were used to evaluate differences between TA and TV measurements.
Results: The validity of the TA method depended on cervical length. Although the TA method underestimated cervical length by 2.0 mm on average (P < 0.001), Bland Altman plots showed an inverse trend with shorter cervixes. In women with a cervix < 25 mm (n = 30) based on TV scan measurement, TA overestimated cervical length by 12 mm (P < 0.001). The sensitivity and specificity of TA as a test to detect cervical length < 25 mm were 10% (95% CI: 2.1–26%) and 94% (95% CI: 92–96%) respectively; the negative LR was 0.96 (95% CI: 0.84–1.08). The maximum area under the ROC curve would be obtained at a TA cut‐off = 32 mm (to detect a cervix < 25 mm), corresponding to a sensitivity of 77% and a specificity of 58%.
Conclusion: TA measurements do not reflect TV assessment accurately, particularly if the cervix is short. At 24–34 weeks, a policy of proceeding to TV scan if TA measurement is < 25 mm will only detect 10% of affected pregnancies and has a poor positive predictive value so is of limited value as a predictive tool for women attending with symptoms and signs of preterm labour > 24 weeks gestation. There is no value in TA assessment of the cervix > 36 weeks.
Keywords: cervical length, preterm labour, risk prediction, ultrasound
Introduction
Spontaneous preterm birth (PTD) is increasingly prevalent and causes significant mortality and morbidity. 1 , 2 There is good data demonstrating an association between PTD and a short cervix, measured by ultrasound. 3 A recent meta‐analysis suggests that the rate of PTD can be reduced by treating women who have a short cervix with progesterone. 4 As both a predictive test and a therapeutic intervention are available, there is considerable interest in routine ultrasound assessment of the cervix. 5
In Australia, the morphology scan is usually performed between 18 and 20 weeks gestation and provides an ideal opportunity for routine cervical assessment. Cervical length is affected by a range of factors that need to be considered for accurate assessment. These include demographic differences, such as gestational age, maternal age, parity and ethnicity, the quality of antenatal care, nutrition, smoking and alcohol intake. 6 The cervix lengthens with increasing bladder volume (Figure 1) and as increased transducer pressure is applied. 7 The process of cervical effacement and shortening appears to start at the internal cervical os, leading to funneling that may be revealed by applying fundal pressure. 8 The cervix is dynamic and protocols that standardise measurement recommend making multiple measurements over a five minute period of assessment. 6 Algorithms that describe individualised levels of risk of preterm delivery have been proposed. 9 The accuracy of these algorithms is dependent on the quality of measurement of cervical length and may be affected by the mode of ultrasound assessment. 10 – 13
Figure 1.
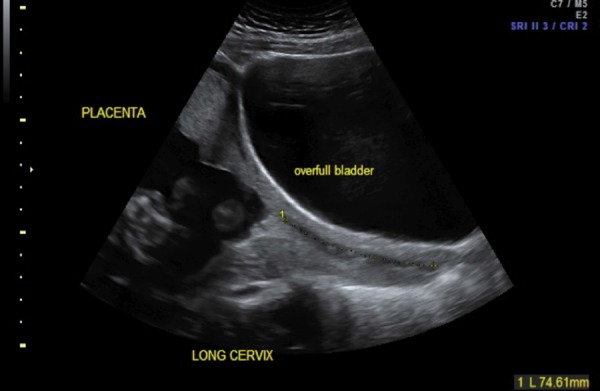
Transabdominal image of the maternal pelvis demonstrating cervical length. The overfull bladder combined with transducer pressure causes elongation of the cervical canal and distorts the cervix with apparent thinning of the anterior wall.
There is no consensus on the best approach to cervical surveillance and specifically as to whether all women should have a transvaginal (TV) scan or whether this can be restricted to women with a short cervix on initial transabdominal (TA) assessment. 14 – 21 Although some protocols advise TV assessment if cervical length is ≤25 mm, many practitioners continue to avoid this mode of scanning which may result in adverse pregnancy outcome. From a resource perspective, most sonographers are reluctant to perform a routine TV scan without better data demonstrating a clinical advantage. In this study, we aim to compare TA and TV measurements of cervical length to assess the efficacy of an initial TA assessment in defining a group of women that should have further TV evaluation. We also assess intra‐observer variation of both TA and TV measurement.
Materials and Methods
A consecutive series of 491 pregnancies were examined in one specialist obstetric imaging unit between 16 and 41 weeks gestation. The indication for ultrasound evaluation included a history of cervical incompetence, routine morphology assessment, follow up of a low‐lying placenta or of a short cervix identified at a previous scan, suspicion of abnormal fetal growth / wellbeing or previous PTD. The practice policy includes TV as well as TA assessment for all these scan indications and examination time was not extended to facilitate this study. Ethics permission was given to audit this data set (X08–0309).
In all cases the cervix was assessed first TA and then TV. In both circumstances, a static image of the cervix was obtained with the long axis of the entire cervix running horizontally across the screen with anterior and posterior walls being equidistant from the cervical canal (Figure 2). Cervical length was measured from the internal to the external cervical os as has been described previously. 6 , 13 If the cervix was significantly curved then the length was measured with trace mode rather than in a straight line. 8 Women were advised to have a full bladder for the TA scan and were then asked to void before the TV assessment.
Figure 2.
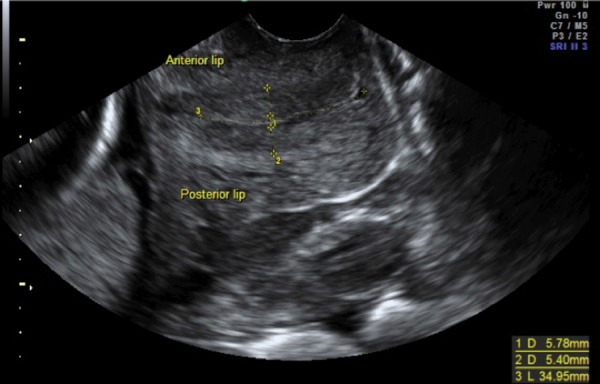
Transvaginal image of the maternal pelvis demonstrating cervical length. The probe is first advanced into the anterior fornix and then slightly withdrawn so that good image quality is maintained while avoiding placing pressure on the cervix. Cervical length is measured from internal to external os. The endocervical canal is also marked and can be differentiated by its echolucency. The anterior and posterior cervical walls are of similar thickness.
Data were assessed to establish the difference between TA and TV measurement of the cervix and to determine whether this difference changed depending on the gestational age at assessment. Intra‐observer variability was calculated for both TA and TV approach using a sub‐set of random pregnancies and with the same image being measured twice. The screening efficacy of using an initial TA assessment, with cervix ≤25mm in length, to define a group for further TV evaluation was calculated.
Statistical analysis
The normality of measurements were assessed using the Shapiro– Wilk test and by visually inspecting the data. Measures of cervical length appeared non‐Gaussian (in accordance with Salomon, et al.) even after logarithmic transformation. 22 Consequently, the distributions of cervical length measurements were compared by the non‐parametric Wilcoxon sign‐rank test. The measurements were further analysed by Bland‐Altman plots. Intra‐observer variation was evaluated by comparing differences between two measures of the same cervix by the Wilcoxon sign‐rank test, with Bland‐Altman plots, and by calculating the intra‐class correlation of correlation. Test characteristics were calculated for the effectiveness of a TA scan in detecting a cervix ≤25mm in length. All statistical analyses were performed with Stata (Version 11, StataCorp, College Station, Texas, USA).
Results
Of the 491 participants: 335, 139 and 17 presented at 16–23, 24–35 and > 36 weeks' respectively. The measurements of cervical length according to gestation are shown in Table 1. Testing for normality found that the data were not normally distributed (Shapiro‐Wilk; P < 0.01). The distributions of the TA and TV measurements, as illustrated by Q‐Q plots (Figure 3a, 3b) are different; the distinct deviation from normality for shorter cervixes measured by a TV approach was not seen in the TA distribution. There were small intra‐observer variations in both the TA (ICC = 0.74) and the TV (ICC = 0.88) measures, with a tendency to more consistent estimates for the TV measures.
Table 1.
Difference in cervical length based on transabdominal and transvaginal measurements. The data are categorised by gestational age.
| Cervical length | Test for normality | Difference between U/S approach | ||||||
|---|---|---|---|---|---|---|---|---|
| Gestation | N | Modality | Mean (sd) | Median (range) | Skewness | P * | meanTA – meanTV | P ** |
| Overall (16 wks‐term) | 491 | TA | 33.0 (6.28) | 32 (13–58) | 0.42 | < 0.001 | −2.0 | < 0.001 |
| TV | 35.0 (7.18) | 35 (0–57) | −0.68 | < 0.001 | ||||
| 16–23 weeks | 335 | TA | 33.6 (6.11) | 33 (13–58) | 0.25 | 0.014 | −2.7 | < 0.001 |
| TV | 36.2 (5.86) | 36 (17–57) | 0.42 | < 0.001 | ||||
| 24–35 weeks | 139 | TA | 32.1 (6.54) | 31 (19–57) | 0.80 | < 0.001 | −1.0 | 0.045 |
| TV | 33.1 (8.50) | 35 (0–47) | −1.04 | < 0.001 | ||||
| > 36 weeks | 17 | TA | 27.9 (4.38) | 28 (22–36) | 0.41 | 0.74 | 2.3 | 0.48 |
| TV | 25.6 (9.27) | 25 (10–43) | 0.07 | 0.94 | ||||
U/S = ultrasound; TA = transabdominal; TV = transvaginal
*Shapiro‐Wilks test;
**Wilcoxon signed‐rank test
Figure 3a.
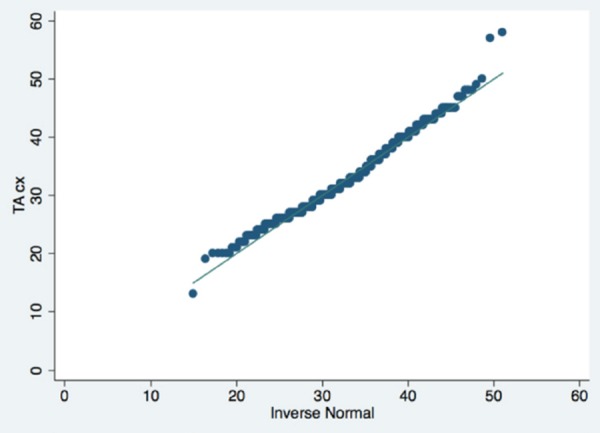
Q‐Q plot, TA measures.
Figure 3b.
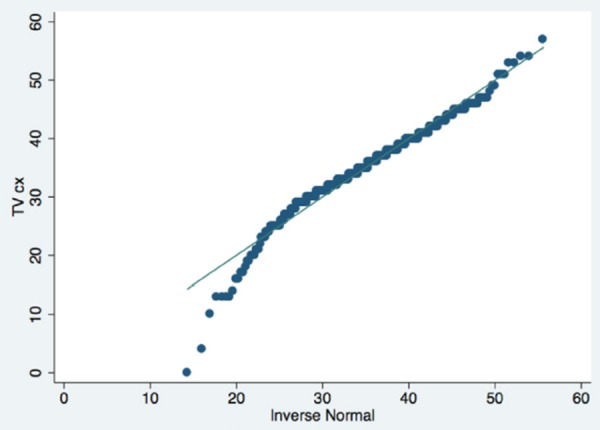
Q‐Q plot, TV measures.
The mean cervical length at 16–23 weeks was 33 mm based on TA assessment and 36 mm based on TV assessment; there was a significant difference of 2.7 mm between these methods of assessment (P < 0.001). TA assessment appeared to overestimate cervical length in cases scanned at 24–35 weeks gestation, but this difference was small (1.0mm; P = 0.045). The cervix was shorter using TV assessment > 36 weeks, although this was not statistically significant (P = 0.48). While cervical length appears to be constant between 16 and 24 weeks, there is evidence of a linear rate of decay beyond 24 weeks gestation, with cervical length decreasing at a rate of 0.74 mm (95% CI: 1.14–0.35) per week (P < 0.001) (Figure 4).
Figure 4.
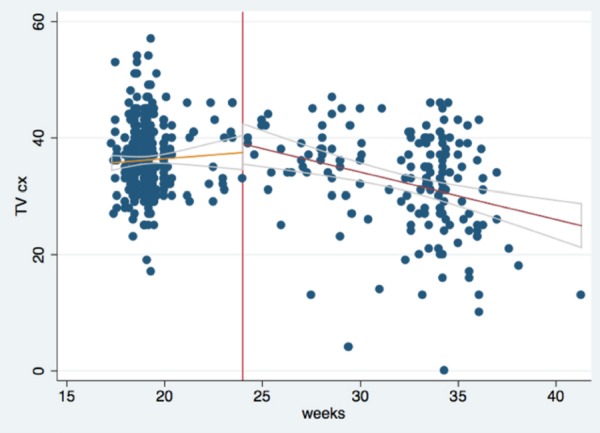
Changes in cervical length in course of pregnancy (transvaginal measurements).
Bland‐Altman plots show large differences (up to 34 mm) in TA and TV measurements within individual cases. Analysis in the gestational sub‐groups show a tendency for the TA approach to over‐measure short cervixes when the assessment is performed > 24 weeks (Figures 5a–5c). For all cases that had a short cervix (≤ 25 mm), TA assessment overestimated mean cervical length by 12.0 mm (mean TA=29.9mm; mean TV=17.8 mm (P < 0.001)) (Figure 6). TA measurements were significantly more likely to overestimate cervical length when TV measurements were ≤ 25mm (Wilcoxon; P < 0.001). In 29 of the 30 cases with a short cervix, TA measurement overestimated length. The sensitivity and specificity of TA assessment in identifying a short cervix (defined as cervical length ≤ 25 mm on TV scan) were 10% and 94% respectively (Table 2). The receiver operator curve for TA identification of a short cervix is shown in Figure 7. There is no threshold of cervical length at which a TA approach provides a satisfactory alternative to TV screening.
Figure 5a to c.
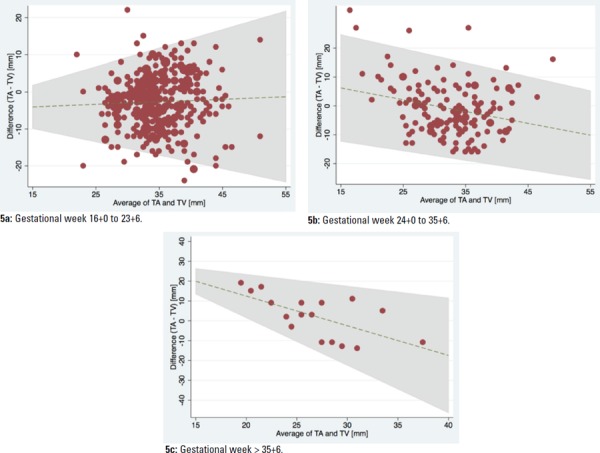
Bland‐Altman plots according to gestation.
Figure 6.
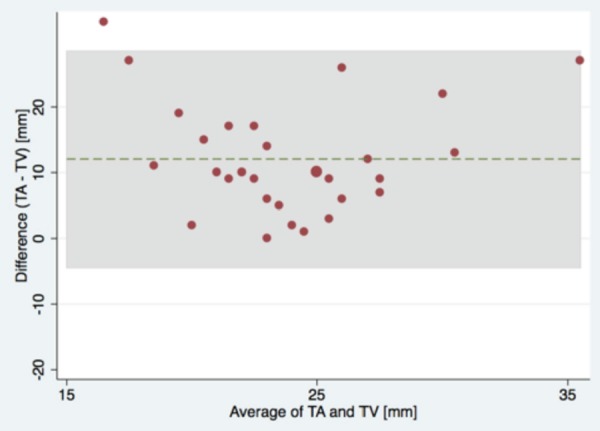
Bland‐Altman plot, cervical length < 25 mm (TV measurement).
Table 2.
Screening efficacy of a transabdominal approach to identifying a short cervix (defined as < 25 mm by transvaginal assessment).
| cervix < 25 mm (TV) | ||||
|---|---|---|---|---|
| No | Yes | |||
| Test < 25 mm (TA) | No | 434 | 27 | 461 |
| Yes | 27 | 3 | 30 | |
| 461 | 30 | 491 | ||
| N % | (95% CI) | |||
| Sensitivity | 3 / 30 | 10.0 (2.1–26.5) | ||
| Specificity | 434 / 461 | 94.1 (91.5–96.0) | ||
Figure 7.
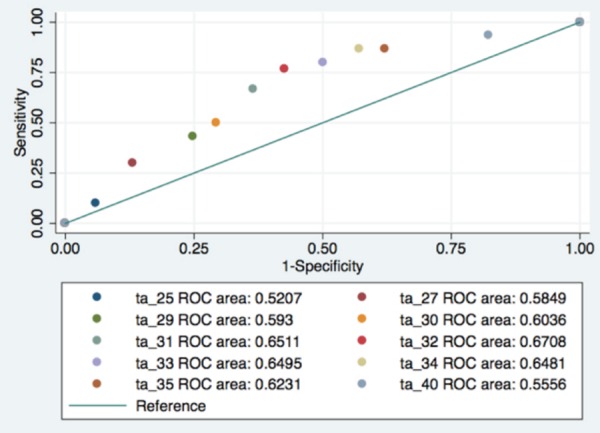
ROC‐curve, cut‐off transvaginal cervical length=25 mm.
Discussion
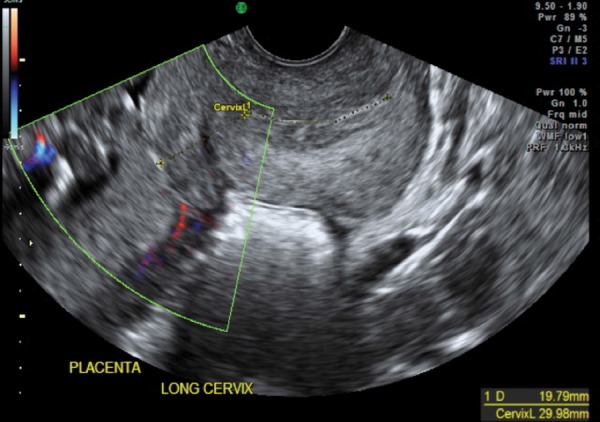
These data show that while there is only a small overall difference in cervical length assessed by either a TA or TV approach, there are large differences in measurement in individual patients and this is clinically significant in circumstances where the cervix is < 25 mm in length (Figure 8a, b). Accepting TV assessment as the gold standard, the TA measurement gave an underestimate of cervical length at the extremes of gestation and an overestimate of cervical length in mid‐pregnancy. This may reflect the different complications faced with TA assessment at these gestations including bladder filling and low uterine contractions (Figure 9). In the later part of the first trimester it is often difficult to distinguish between the lower segment of the uterus and the internal margin of the cervical isthmus while at late gestations, the presenting part produces acoustic shadowing that masks the internal cervical os. The sensitivity of TA ultrasound in defining a cohort of women who have a short (< 25 mm closed length) cervix was poor (10%). Six percent of women were defined as having a short cervix using the TA technique, but the positive predictive value was only 10%. Further receiver‐operator analysis could not define any cervical length where a TA approach provided a reasonable first line alternative to TV sonography.
Figure 8a,b.
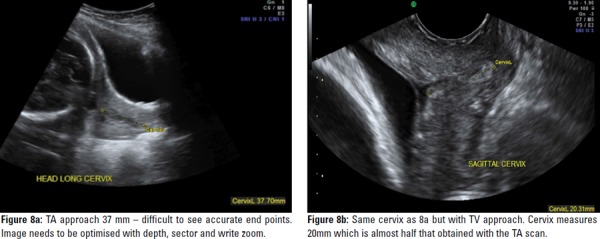
Same cervix measured with TA then TV approach.
Figure 9.
TV image of cervix with a contraction and posterior placenta. A common error is mistaking a lower uterine contraction for placental edge / cervix which can mimic placenta previa.
The mean transvaginal cervical length measured at 16–23 weeks' gestation was 36 mm; comparable to mean measurements of 36 mm and 39 mm reported by Heath, et al. and the SCOPE study group respectively. 6 , 15 Intra‐observer variability was low (3.5%) confirming previous reports that TV measurements are reproducible. 6 The data show that cervical length is not normally distributed; in line with the previous observations of Solomon, et al. 22 While the cervix appears to have stable length < 24 weeks, there is then a gradual reduction in cervical length of approximately 1mm per week gestation thereafter; these cross‐sectional data are consistent with previous longitudinal assessment, showing a decay rate of 0.5 mm / week gestation. 23 There have been some reports that multiple measures of cervical length may be useful in defining an excessive rate of cervical decay from 16 weeks, that is predictive of preterm labour. 24 Our data, that show wide variation in TA and TV measurement made within individual patients would also suggest that multiple measures would only be of value if assessments were made transvaginally, as the degree of measurement variation seen with the TA approach would mask any objective assessment of cervical decay.
The data of this study support a growing body of literature that suggest that TA measurement of cervical length is unreliable at all stages of gestation when compared with the TV approach and is not appropriate when screening for risk of spontaneous preterm delivery. 19 , 20 The original work of Hassan, et al. used a protocol that allowed a TA examination as a routine, but reverted to a TV approach with cervix < 25 mm. The same group have more recently published data that found that this policy would miss a significant proportion of those with a short cervix. 18 This is also supported by Freidman, et al. with a claim that 40% of women that had a TA could avoid a TV assessment but there was a 30% false positive rate and 10% of short cervixes were missed on TA alone. 17 Conflicting datasets included that of the SCOPE study by Stone, et al., and Roh, et al., where the correlation between TA and TV cervical length found the TA to be consistently shorter than the TV approach and so could be used as a screening for the short cervix. 15 , 20 The Roh study had no significant short cervix cohort for comparison and stated the numerous circumstances that a TA measurement was unreliable.
Standardising measuring protocols for both TA & TV could assist with implementing best clinical practice. Iams, et al. analysed over 4,000 TV images of the cervix, performed by 327 sonographers, to see how many conformed to written criteria for imaging and measuring the cervix. 13 Errors occurred when images did not include required landmarks, excessive transducer compression, incorrect image size and calliper placement. Bladder fullness also has the potential to impact on TA cervical length measuring, as was shown in studies by Anderson, To and Chaudhury, and so is unreliable. 10 , 11 , 21 However the Saul group concluded that post void TA cervical length correlated well with the TV measurement and therefore was useful as a screening tool for the short cervix. 16
This was a prospectively collected dataset of women referred to an ultrasound practice that has a focus on obstetric and gynaecological imaging. TV assessment was performed as a matter of routine according to practice protocol. The data therefore reflect the potential pitfalls of TA assessment in routine practice. The data are, however limited as there was some bias towards inclusion of high risk patients, specifically referred for cervical assessment and there are only small numbers of cases assessed > 36 weeks gestation. A commitment to transvaginal sonography does impact on practice management; preparing women for TV assessment adds a minimum of 5 minutes to the total examination time and in the context of a normal sonography schedule this would add 60 minutes to the time taken to scan a list of 12 patients. We did not collect data on the effect of bladder filling nor of maternal body habitas, both factors that have been reported to affect TA visualisation of the cervix. 7 , 10 , 11 , 20 Despite this, we feel that the overall poor performance of TA assessment would negate defining any sub‐population where transabdominal sonography was appropriate for screening.
In conclusion, transvaginal assessment of cervical length should be regarded as the gold standard for assessment of risk of preterm delivery. Measurements made by this approach appear to be more reproducible and robust and therefore allow ready comparison to established normal ranges as well as to datasets that report the rate of cervical decay. The poor sensitivity (10%) of TA assessment in detecting a short cervix means that a policy of using a TA approach first, then reverting to TV assessment for a subgroup with a cervix < 25 mm has a limited use in obstetric practice.
Acknowledgements
Thank you to the team at Northern Women's Imaging – Dr Terry Chang, Dr Glen McNally for input and sonographers Janet Benstead, Asya Klistorner & Anna Marriott‐Brittan for assisting with data collection.
References
- 1. Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet 2008; 371: 75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moore T, Hennessy EM, Myles J, Johnson SJ, Draper ES, Costeloe KL, et al. Neurological and developmental outcome in extremely preterm children born in England in 1995 and 2006: The EPICure studies. BMJ 2012; 345 e7961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Honest H, Bachmann LM, Coomarasamy A, Gupta JK, Kleijnen J, Khan KS. Accuracy of cervical transvaginal sonography in predicting preterm birth: A systematic review. Ultrasound Obstet Gynecol 2003; 22: 305–22. [DOI] [PubMed] [Google Scholar]
- 4. Romero R, Nicolaides K, Conde‐Agudelo A, Tabor A, O'Brien JM, Cetingoz E, et al. Vaginal progesterone in women with an asymptomatic sonographic short cervix in the midtrimester decreases preterm delivery and neonatal morbidity: A systematic review and meta‐analysis of individual patient data. Am J Obstet Gynecol 2012; 206: 124. e1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Campbell S. Universal cervical‐length screening and vaginal progesterone prevents early preterm births, reduces neonatal morbidity and is cost saving: Doing nothing is no longer an option. Ultrasound Obstet Gynecol 2011; 38: 1–9. [DOI] [PubMed] [Google Scholar]
- 6. Heath VC, Southall TR, Souka AP, Novakov A, Nicolaides KH. Cervical length at 23 weeks gestation: Relation to demographic characteristics and previous obstetric history. Ultrasound Obstet Gynecol 1998; 12: 304–11. [DOI] [PubMed] [Google Scholar]
- 7. Mason G. Alterations in bladder volume and the ultrasound appearance of the cervix. Br J Obstet Gynaecol 1990; 97: 457–61. [DOI] [PubMed] [Google Scholar]
- 8. Owen J, Yost N, Berghella V, Thom E, Swain M, Dildy GA 3rd, et al, and the National Institute of Child Health and Human Development . Maternal‐Fetal Medicine Units Network. Mid‐trimester endovaginal sonography in women at high risk for spontaneous preterm birth. JAMA 2001; 286: 1340–48. [DOI] [PubMed] [Google Scholar]
- 9. Celik E, To M, Gajewska K, Smith GC, Nicolaides KH, and the Fetal Medicine Foundation Second Trimester Screening Group . Cervical length and obstetric history predict spontaneous preterm birth: Development and validation of a model to provide individualized risk assessment. Ultrasound Obstet Gynecol 2008; 31 (5): 549–54. [DOI] [PubMed] [Google Scholar]
- 10. Anderson H. Transvaginal and transabdominal ultrasonography of the uterine cervix during pregnancy. J Clin Ultrasound 1991; 19: 77–80. [DOI] [PubMed] [Google Scholar]
- 11. To M, Skentou C, Cicero S, Nicolaides K. Cervical assessment at the routine 23 week scan: Problems with transabdominal sonography. Ultrasound Obstet Gynecol 2000; 15: 292–96. [DOI] [PubMed] [Google Scholar]
- 12. To M, Skentou C, Cicero S, Nicolaides K. Cervical assessment at the routine 23 week scan: Standardizing techniques. Ultrasound Obstet Gynecol 2001; 17: 217–19. [DOI] [PubMed] [Google Scholar]
- 13. Iams J, Grobman W, Lozitska A, Spong CY, Saade G, Mercer BM, et al. Adherence to criteria for transvaginal ultrasound imaging and measurement of cervical length. Am J Obstet Gynecol 2013; 209 (4): 365. e1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hassan SS, Romero R, Berry SM, Dang K, Blackwell SC, Treadwell MC, et al. Patients with an ultrasonographic cervical length < or =15 mm have nearly a 50% risk of early spontaneous preterm delivery. Am J Obstet Gynecol 2000; 182: 1458–67. [DOI] [PubMed] [Google Scholar]
- 15. Stone PR, Chan EH, McCowan LM, Taylor RS, Mitchell JM, and the SCOPE Consortium . Transabdominal scanning of the cervix at the 20–week morphology scan: Comparison with transvaginal cervical measurements in a healthy nulliparous population. Aust N Z J Obstet Gynaecol 2010; 50: 523–27. [DOI] [PubMed] [Google Scholar]
- 16. Saul LL, Kurtzman JT, Hagemann C, Ghamsary M, Wing DA. Is transabdominal sonography of the cervix after voiding a reliable method of cervical length assessment? J Ultrasound Med 2008; 27 (9): 1305–11. [DOI] [PubMed] [Google Scholar]
- 17. Freidman AM, Srinivas SK, Parry S, Elovitz MA, Wang E, Schwartz N. Can transabdominal ultrasound be used as a screening test for short cervical length? Am J Obstet Gynecol 2013; 208 (3): 190–97. [DOI] [PubMed] [Google Scholar]
- 18. Hernandez‐Andrade E, Romero R, Ahn H, Hussein Y, Yeo L, Korzeniewki SJ, et al. Transabdominal evaluation of uterine cervical length during pregnancy fails to identify a substantial number of women with a short cervix. J Matern Fetal Neonatal Med 2012; 25 (9): 1682–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Marren A, Mogra R, Pedersen LH, Walter M, Ogle RF, Hyett JA. Ultrasound assessment of cervical length at 18–21 weeks' gestation in an Australian obstetric population: Comparison of transabdominal and transvaginal approaches. Aust N Z J Obstet Gynaecol 2014; 54 (3): 250–55. (doi:10.1111/ajo.12204). [DOI] [PubMed] [Google Scholar]
- 20. Roh H, Ji Y, Jung C, Jeon G, Chun S, Cho H. Comparison of cervical lengths using transabdominal & transvaginal sonography in mid pregnancy. J Ultrasound Med 2013; 32: 1721–28. [DOI] [PubMed] [Google Scholar]
- 21. Chaudhury K, Ghosh M, Halder A, Senapati S, Chaudhury S. Is transabdominal ultrasound scanning of cervical measurement in mid‐trimester pregnancy a useful alternative to transvaginal ultrasound scan? J Turkish‐German Gynecol Assoc 2013; 14: 225–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Salomon LJ, Diaz‐Garcia C, Bernard JP, Ville Y. Reference range for cervical length throughout pregnancy: Non‐parametric LMS‐based model applied to a large sample. Ultrasound Obstet Gynecol 2009; 33: 459–64. [DOI] [PubMed] [Google Scholar]
- 23. Moroz LA, Simhan HN. Rate of sonographic cervical shortening and the risk of spontaneous preterm birth. Am J Obstet Gynecol 2012; 206 (3): 234. e1–5. (doi:10.1016/j.ajog.2011.11.017). [DOI] [PubMed] [Google Scholar]
- 24. Szychowski J, Owen J, Hankins G, Iams J, Sheffield J, Perez‐Delboy A, et al. Timing of mid‐trimester cervical length shortening in high risk women. Ultrasound Obstet Gynecol 2009; 33: 70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]


