Abstract
Purpose: To assess the ultrasound performance on patients presenting to Waikato hospital ultrasound department with a clinical suspicion of appendicitis.
Method: This was a retrospective audit of 309 patients presenting to our department within business hours with clinical suspicion of appendicitis between September 2012 and March 2014. The patients were evaluated by operators of mixed experience. The scan reports, surgical reports, histology and discharge summaries were reviewed.
Results: The overall sensitivity of ultrasound on detecting appendicitis was 50%, the specificity was 98.5%. The positive predictive value and the negative predictive value were 84% and 92.6% respectively. The appendix was visualised in 14% of the true positive cases. When the appendix was visualised, the sensitivity and specificity of ultrasound was 95.2% and 69.2% respectively. Conclusion: The sensitivity of ultrasound to appendicitis was lower than that commonly reported in the literature, but on a par with a recent audit from another tertiary hospital in New Zealand.
Keywords: appendicitis, appendix, ultrasound
Introduction
Appendicitis constitutes one of the most common abdominal emergencies. Diagnostic ultrasound is the imaging modality of choice in patients with suspected appendicitis due to its accessibility, lack of ionising radiation and good diagnostic accuracy reported in the literature. The principal limitation of ultrasound is the variability of its diagnostic performance depending on operator experience, patient population characteristics (paediatric versus adult) and body characteristics of the individual patient. A wide range of sensitivity and specificity of ultrasound for appendicitis has been reported. Whether ultrasound is a reliable tool for diagnosing appendicitis remains controversial. 1 , 2 An unpublished retrospective audit performed at a tertiary metropolitan hospital in New Zealand demonstrated relatively modest sensitivity (56%) in detecting appendicitis. 3 The aim of this audit was to determine the diagnostic performance of ultrasound in the diagnosis of appendicitis in patients presenting with a clinical suspicion of appendicitis to the Department of Ultrasound at Waikato Hospital (Hamilton, New Zealand).
Methods
Patient Selection
We performed a retrospective internal audit to evaluate the performance of ultrasound during a 19‐month period between September 2012 and March 2014. We used the referral booking system to identify patients who presented to the hospital with a clinical suspicion of appendicitis during regular business hours. Patients were included in the audit if appendicitis was the primary clinical diagnosis or if appendicitis was listed as a differential diagnosis. Exclusion criteria included the following: 1) patients from the community (outpatient clinic), 2) patients scanned during on‐call and on weekends, 3) patients from peripheral hospitals affiliated with our centre, 4) where appendicitis was an incidental discovery rather than a differential of the diagnostic work‐up. We identified 309 patients with suspected appendicitis who underwent ultrasound evaluation in our department.
Classifications of patients
The scan report for each patient was reviewed and was categorised into either scan‐positive or scan‐negative group based on the findings. The scan result was defined as positive when the report included phrases such as: “correlate with appendicitis”, “consistent with appendicitis”, “most suggestive of appendicitis”, “most probably appendicitis”, “may represent appendicitis”, “very suspicious for appendicitis”. The scan was defined as negative when no convincing features of appendicitis were reported and the report contained statements such as: “no evidence of appendicitis”, “no indirect signs of appendicitis”, “appendicitis not visualised” “appendicitis cannot be ruled out”.
The surgical report, histology report and discharge letter for each patient were reviewed. The gold standard for the diagnosis of appendicitis was a positive histology report. The true negative group of patients included those who a) proceeded with an exploratory laparoscopy but without appendicectomy, b) underwent appendicectomy and histology report showed negative results for appendicitis, and c) the patient was discharged without appendicectomy. Re‐admission after discharge occurred in a small number of cases, each of them was analysed individually. Based on the continuity of the patients' symptoms and the length of the interval between two admissions (ranging from 18 days up to a year), they were either combined with the first admission and logged as one single incident, or recorded as a new case.
Scan Procedure
Ultrasound examinations were performed by staff sonographers or radiology registrars of mixed clinical expertise using Philips iU22 (Bothel, Washington) or Siemens Acuson Sequoia 512 (Mountainview, California) systems. Graded compression technique in the right iliac fossa (RIF) was used to assess for the presence of appendicitis, in addition to routine abdominal, transvaginal and other regional ultrasound assessments as required. The scan session was limited to 30 minutes. The operators were blinded to future audit.
Results
Among the 309 selected patients, 25 were classified by ultrasound as positive for appendicitis and 284 patients were diagnosed negative. A total number of 94 patients underwent laparoscopy, 42 of which had positive histology results. Only half (21/42) of these true positive cases were identified by the ultrasound scan prior to the laparoscopy, while the other 21 cases had negative ultrasound reports (Figure 1). The sensitivity of ultrasound in detecting appendicitis was therefore 50%, and specificity was 98.5%. The positive predictive value and the negative predictive value were 84% and 92.6% respectively. Of those who were diagnosed with appendicitis on histology reports, the appendix was visualised in 50% of the cases (21/42). When the appendix was visualised, the sensitivity of ultrasound was 95.2% (20/21) and specificity was 69.2% (9/13). There was a high female to male ratio (11:1). The prevalence of appendicitis in our study was very low (14%). The age range of the true positive group was 3 to 55, with a median of 19 years.
Figure 1.
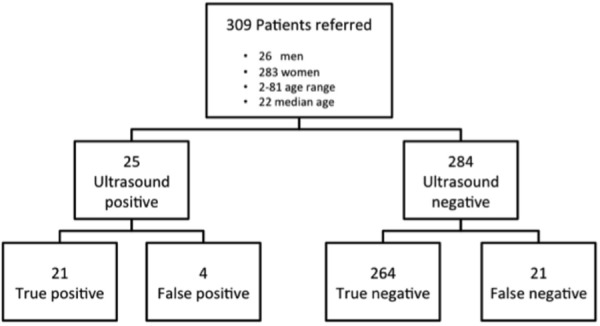
Flow chart of case analysis.
Discussion
The overall sensitivity of ultrasound for the diagnosis of appendicitis in our audit was low compared with the literature. Two published systematic reviews comparing computed tomography (CT) and ultrasound in detecting acute appendicitis demonstrated substantially higher overall sensitivity of 86% and 78%. 4 , 5 Both reviews included prospective studies only. More recent prospective studies also reported similar or even higher sensitivity of ultrasound, ranging from 72.5% to 91%. 6 – 10 On the contrary, some retrospective studies consistently reported much lower sensitivity, ranging from 23.1% to 56.4%. 1 , 11 – 13 One retrospective study showed a sensitivity of 99.1%; however the cases with non‐visualisation of appendix were not included in the study. 2 The tendency for prospective studies to report better performance than retrospective studies may be in part due to the study design. Prospective studies draw more input from senior or expert practitioners; the patient selection may be better and the operators are not blinded. The performance of ultrasound tested prospectively therefore reflects an optimal diagnostic environment. In contrast, retrospective studies investigate the performance of ultrasound in “real life” clinical circumstances where operators with variable expertise may be scanning a suboptimally selected population of patients with multiple comorbidities in an otherwise busy and distracting clinical environment.
When the appendix was visualised in our study, appendicitis was correctly diagnosed on ultrasound in 95.2% of the cases. One can expect that by improving the visualisation of the appendix, the accuracy of ultrasound in diagnosing appendicitis could also be improved. This idea is supported by Taylor (2014) who demonstrated that the more frequently ultrasound was used for detecting appendicitis, the higher the sensitivity of ultrasound and the better the visualisation rate. 8
The prevalence of appendicitis in our study was only 14%, which is well below the published rates. For example, van Randen and colleagues studied a population with a prevalence of 28%. 7 The referral patterns and low prevalence rate in our patients would likely to have a negative impact on the operator performance, operator expertise and overall sensitivity of ultrasound to appendicitis. Furthermore, our referrers were not utilising ultrasound as a targeted test for appendicitis, but more as a screening tool to assess for a broader range of differentials. Perhaps in real life practice this phenomenon is inevitable, owing to the similarity of the presentations of the common right iliac fossa pathologies, and the inconsistency of the symptoms of acute appendicitis. However, the low prevalence rate of appendicitis in patients where appendicitis was listed as a differential on the ultrasound referral none‐the‐less reflects suboptimal pre‐selection of patients.
There were a number of limitations to this study. Our retrospective analysis of the ultrasound reports required us to develop a system of definitions for a positive and negative scan result. When the appendix was not confidently visualised on ultrasound, the results of the scans were often intermediate. The ultrasound reports often contained equivocal wording, which reflected the drawbacks and limitations of the ultrasound scan. For the purpose of statistical analysis, we classified each intermediate report into either positive or negative group by evaluating the context and the wording of the report. Another limitation was the relatively low number of patients with histologically proven appendicitis. We also did not correct for those patients who were classified as ultrasound positive for appendicitis, did not have appendicitis but instead had other appendiceal pathology such as an appendiceal tumour. Finally, although appendicectomy remains the standard treatment for acute appendicitis, 14 appendicitis may also resolve with antibiotics. 15 It is therefore possible that we have categorised some of these patients with appendicitis into the true negative group on the basis of patient being discharged from the hospital.
Conclusion
Our retrospective audit showed less optimistic performance of ultrasound in the diagnosis of appendicitis in a general hospital setting than the literature suggests. Our performance was in close agreement with an audit performed at Auckland Hospital. Compared with carefully planned prospective studies, retrospective studies better reflect the true diagnostic performance of ultrasound practitioners in a day‐to‐day clinical setting and generally report less optimistic performance parameters.
Acknowledgements
We thank Anabel Greville for her assistance in preparing the study, and Cecilia Barnard for helping with data collection.
References
- 1. Ekere C, Mehta C, Royston E, Arrowsmith C, Talbot R. Does ultrasound scanning RIF pain have a role in the investigation of suspected acute appendicitis. Int J Surg 2013; 11 (8): 699. [Google Scholar]
- 2. Park JS, Jeong JH, Lee JI, Lee JH, Park JK, Moon HJ. Accuracies of diagnostic methods for acute appendicitis. Am Surg 2013; 79 (1): 101–06. [PubMed] [Google Scholar]
- 3. Greville A. The accuracy of ultrasound for suspected appendicitis in the emergency setting. Annual Scientific Meeting of the New Zealand Branch of ASUM; Auckland: 2012. [Google Scholar]
- 4. Terasawa T, Blackmore CC, Bent S, Kohlwes RJ. Systematic review: Computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med 2004; 141 (7): 537–46. [DOI] [PubMed] [Google Scholar]
- 5. van Randen A, Bipat S, Zwinderman AH, Ubbink DT, Stoker J, Boermeester MA. Acute appendicitis: Meta‐analysis of diagnostic performance of CT and graded compression US related to prevalence of disease. Radiology 2008; 249 (1): 97–106. [DOI] [PubMed] [Google Scholar]
- 6. Al‐Ajerami Y. Sensitivity and specificity of ultrasound in the diagnosis of acute appendicitis. EMHJ 2012; 18 (1): 66–9. [DOI] [PubMed] [Google Scholar]
- 7. van Randen A, Lameris W, van Es HW, van Heesewijk HP, van Ramshorst B, Ten Hove W, et al. A comparison of the accuracy of ultrasound and computed tomography in common diagnoses causing acute abdominal pain. Eur Radiol 2011; 21 (7): 1535–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Taylor GA. Abdominal ultrasound is specific but insufficiently sensitive in diagnosing appendicitis. J Pediatr 2014; 164 (3): 672–73. [DOI] [PubMed] [Google Scholar]
- 9. Toorenvliet BR, Wiersma F, Bakker RF, Merkus JW, Breslau PJ, Hamming JF. Routine Ultrasound and Limited Computed Tomography for the Diagnosis of Acute Appendicitis. World J Surg 2010; 34 (10): 2278–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hussain S, Rahman A, Abbasi T, Aziz T. Diagnostic accuracy of ultrasonography in acute appendicitis. JAMC. 2014; 26 (1): 12–7. [PubMed] [Google Scholar]
- 11. Mandavia R, Li M, Sheth H. The efficacy of ultrasound scanning as a diagnostic tool in cases of suspected appendicitis. Int J Surg 2013; 11 (8): 719. [Google Scholar]
- 12. Johnson CY. Philip; Fernando, Suresh; Graham, Jonathan. The emperor's new clothes? An evaluation of the accuracy of transabdominal ultrasound in diagnosing acute appendicitis. European Congress of Radiology Vienna 2013.
- 13. Lobban C, D'Souza KA. What is the value of abdominal ultrasound for the detection of appendicitis? BMJ 2013; 100: 83. [Google Scholar]
- 14. Wilms IM, de Hoog DE, de Visser DC, Janzing HM. Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane Database Syst Rev 2011; (11): CD008359. [DOI] [PubMed] [Google Scholar]
- 15. Allescher HD. Appendicitis: Can Immediate Antibiotic Treatment Still Be Withheld? Gastroenterology 2012; 142 (3): 666–69. [DOI] [PubMed] [Google Scholar]


