Abstract
Background: Lung ultrasound is frequently used to identify pulmonary oedema, using the ‘B line’ artefact. A small study in 2011 suggested that novice sonologists had a potential diagnostic accuracy of 85%, when performing the test without reference to other patient information.
Aim: We aimed to test the overall diagnostic accuracy of novice clinician sonologists incorporating the 2011 protocol into routine assessment of the patient.
Method: A prospective convenience sample of breathless older patients presenting to ED received an 8‐view lung scan early in management. Initial ED diagnoses, utilising all information including ultrasound result, were compared against the opinion of a medical expert auditing the patient records after discharge from hospital.
Results: The cohort of five novices scanned 63 cases, from which eleven were excluded.
Novices using ultrasound differentiated between pulmonary oedema and other causes of breathlessness with a sensitivity of 71% (95%CI 44 to 87), Specificity of 91% (76 to 98), a diagnostic accuracy of 85% (72 to 92), a positive LR of 8.2 (2.7 to 25) and a negative LR of 0.32 (0.15 to 0.68).
Discussion: The diagnostic accuracy of emergency department clinicians incorporating novice lung ultrasound into the investigation of breathlessness is consistent with the diagnostic accuracy of scanning performed in parallel to patient care, and is likely to be an improvement on current estimates of conventional ED diagnostic strategies. Clinicians should not be afraid that their learning curve would disadvantage the patient.
Keywords: diagnostic accuracy, heart failure, lung ultrasound, novice
Introduction
Despite a growing body of evidence supporting the use of lung ultrasound in the investigation of breathlessness, uptake by the health professional has been slow.
Evidence has accumulated over 17 years, showing that lung ultrasound B‐lines indicate pulmonary oedema.1–11 There is now a growing body of research showing lung ultrasound (LUS) to be pivotal in the diagnostic workup of the aged breathless patient in Emergency Medicine.12–15 We wondered if the slow translation of this evidence into practice was due to the fear of causing harm during the learning curve of the novice practitioner.
The first studies to examine lung ultrasound protocols tested expert sonologists against chest xray and CT scans.4–7 In the next generation of trials, unblinded expert sonologists investigated the effects of inserting LUS into management protocols.13,16,18 They reported on changes to decision‐making, treatment outcomes, and costs of care. Novice interpretation13,19,20 and novice acquisition21–23 have been studied, but as yet none have specifically added novice scanning to the diagnostic workup.
In 2011 we commenced investigation of LUS to identify pulmonary oedema among breathless older patients presenting to the ED.24 We recorded the sonologists bedside impressions, saved the scans and had them reviewed by a blinded expert sonologist. Although bedside and blinded reviewer differed in some interpretations, the diagnostic accuracy for both was comparable. We surmised that novice sonologists supplemented their interpretation with visual cues they were unable to capture for the blinded review. Chiem, et al. have subsequently published comparable findings, using a shorter training schedule.23
Following on from these results, we decided to test whether the routine insertion of LUS scanning into the care of the breathless patient had any adverse effect on diagnostic accuracy – we wanted to reassure novice clinicians that their learning curve in LUS assessment did not affect patient safety. Whereas the 2011 project estimated the accuracy of novice lung ultrasound as a test, and this study aimed to demonstrate safety and reproducibility when inserted into routine assessment.
Method
Participants
As with the LUS2011 study, this 2013 study was conducted in the Ipswich Hospital Emergency Department. It serves a community of approximated 250 000 people from the western edge of Greater Brisbane and nearby rural areas. There are over 50 000 adult and paediatric presentations annually.
A new cohort of novices received near‐identical training in the same protocol, and added it into their care of breathless older patients. Protocol nomenclature was changed for the second group, but cut‐offs between diagnostic groups remained the same. LUS‐assisted ED diagnoses were compared to post discharge chart audit diagnoses to calculate diagnostic accuracy when lung ultrasound was incorporated into initial patient care.
The study recruited from the group of patients who present with a sensitive but non‐specific indicator of heart failure (breathlessness) and who almost invariably undergo rigorous but imprecise investigation to rule out pulmonary oedema.
The study used prospective convenience sampling, recruiting patients of at least 60 years of age who presented to an urban ED and reporting any degree of breathlessness at triage, important enough to be noted in the triage complaint field on the emergency department information system (EDIS). If the treating doctor had completed the LUS training package, the patient was considered for the trial. No formally credentialed or experienced sonologists participated. All treating doctors were registrar level clinicians (PGY3–5).
Patients were excluded if they required active resuscitation or reported any degree of trauma as part of the presenting complaint. Recruitment ceased with the commencement of multicentre LUS trial.
A formal screening log was not attempted because patient sampling was constrained by the limited numbers of trained doctors. This limitation meant many potential patients were not recruited.
Waiver of consent was obtained from the Queensland Civil and Administrative Tribunal. Public Health Act approval was obtained from the Director General. The West Moreton Ethics Board approved the amendments to the original protocol.
Data collection
The treating doctor performed the LUS scan as early as practicable in the patient's management, usually before the chest x‐ray was obtained. Scans were saved to a computer hard drive and the LUS result noted immediately in a trial book. As the patient was discharged from the ED the treating doctor's final diagnosis was entered into a trial book, taking all ED test results and the LUS into account. Missing diagnosis data were retrieved by chart recall and review by the treating doctor. The formal radiologist chest xray report was also extracted. For safety and quality monitoring, saved novice scans were later reviewed by an expert sonologist.
After hospital discharge, the auditor reviewed the patient's ED notes, clinical investigations, and all subsequent clinical notes made by inpatient clinical staff to give an opinion on the cause of breathlessness at presentation. The auditor was blinded to the LUS results but not the diagnostic impression of the treating ED doctor.
Test method
The treating doctors were taught a standard 8 view LUS protocol10,21,24,25 performed on a GE Logic‐e (China) with the 2–5 MHz curved probe.
A ‘wet’ scan contained 12 or more B lines, with at least 3 B lines per view in two views per side. Fewer than 12 B lines indicated a ‘dry’ scan. To allow the sonologist to indicate uncertainty, ‘dry’ scans that came close to the 12 B line cut‐off were called ‘subclinical’, but still tallied within the ‘dry’ category. ‘Wet’ scans that contained other pathology such as consolidation, could be sub‐labelled ‘dual pathology’ but were still counted within the ‘wet’ category. Examples are illustrated in Figure 1.
Figure 1.
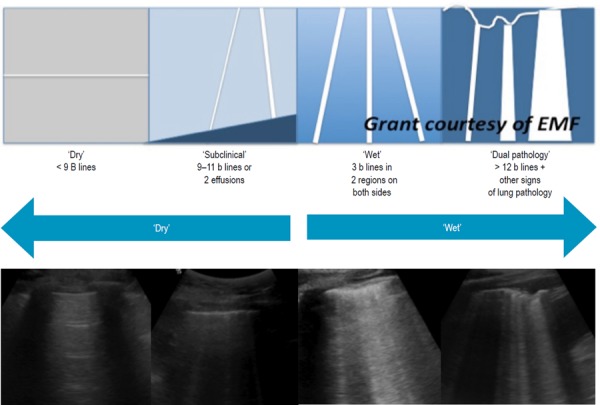
Classification of LUS results by diagram and example. Sub categories of ‘subclinical’ and ‘dual pathology’ took the place of the free field bedside comments used in the 2011 study. In this way, both studies allowed the sonologist to indicate possible treated or resolving oedema (subclinical) or false positive (dual pathology).
Training
The treating doctors performing LUS were given the same training package presented to the 2011 cohort of novices. Five registrar level staff had attended a basic introduction to ultrasound (five day course) in the preceding year, followed by a four hour LUS training workshop. Each then performed ten proctored lung ultrasound scans before being allowed to recruit for the trial (Figure 2).
Figure 2.

Training Package for Lung ultrasound.
A scan of adequate quality required eight appropriately labelled views, with distinct pleura, and a rib shadow in the upper views or diaphragm/liver/spleen glimpsed in the lowest view (Figure 3). Good quality scans had the focus high and the depth between 10 and 15 cm, although this was not mandatory for a diagnosis.
Figure 3.
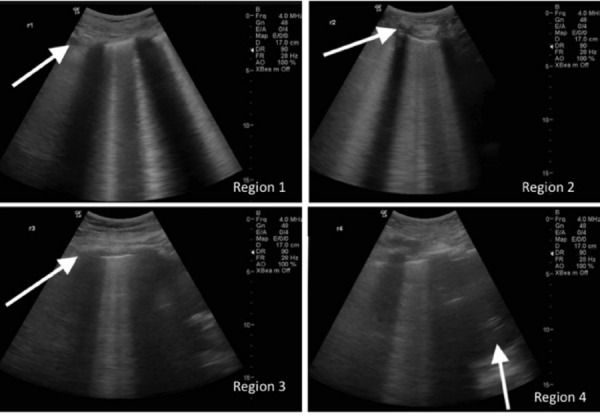
A good quality scan set contained appropriate labels, a high focus and a low depth. A set order was required to mitigate poor labelling (R1 to 4 then L1 to 4) and when dubious this was crosschecked against subtle differences in the views, as indicated by block arrows. Region 1 usually contains either clavicle or subclavian vessel in the top left corner, region 2 has more rounded or cartilaginous rib, region 3 has fewer or less distinct rib shadows due to oblique rib position in axilla, and region 4 requires a moiety of either diaphragm, liver or spleen, to demonstrate that the sonologist has scanned the lowermost portion of lung posterolaterally. This scan set is strongly positive.
Training resources, sample cases and important literature links are available on an educational Facebook page at https://www.facebook.com/BrisbaneLungUltrasound?ref=hl.


