Abstract
Digital imaging combined with picture archiving and communication system (PACS) access allows detailed image retrieval and magnification. Calcium pyrophosphate dihydrate (CPPD) crystals preferentially deposit in fibrocartilages, the cartilage of the acromioclavicular (AC) joint being one such structure. We sought to determine if examination of the AC joints on magnified PACS imaging of chest films would be useful in identifying chondrocalcinosis (CC). Retrospective radiographic readings and chart reviews involving 1,920 patients aged 50 or more who had routine outpatient chest radiographs over a 4-month period were performed. Knee radiographs were available for comparison in 489 patients. Medical records were reviewed to abstract demographics, chest film reports, and diagnoses. AC joint CC was identified in 1.1 % (21/1,920) of consecutive chest films. Patients with AC joint CC were 75 years of age versus 65.4 in those without CC (p<0.0002). Four hundred eighty-nine patients had knee films. Six of these patients had AC joint CC, and of these, five also had knee CC (83 %). Of the 483 without AC joint CC, 62 (12 %) had knee CC (p=0.002). Patients with AC joint CC were more likely to have a recorded history of CPPD crystal deposition disease than those without AC joint CC (14 versus 1 %, p=0.0017). The prevalence of AC joint CC increases with age and is associated with knee CC. A finding of AC joint CC should heighten suspicion of pseudogout or secondary osteoarthritis in appropriate clinical settings and, in a young patient, should alert the clinician to the possibility of an associated metabolic condition.
Keywords: Acromioclavicular joint, Calciumpyrophosphate dihydrate (CPPD) crystal deposition disease, Chondrocalcinosis
Introduction
Calcium pyrophosphate dihydrate (CPPD) crystal deposition disease is a relatively common arthritic disorder of the elderly, and the prevalence of the disease is 5 % in the general population. Prevalence increases with age [1]. The term chondrocalcinosis refers to the radiographic evidence of linear or punctate calcifications in cartilage. CPPD crystal deposition preferentially involves fibrocartilages such as the menisci of the knee, triangular fibrocartilage of the wrist, acetabular labrum, and symphysis pubis [2]. The acromioclavicular (AC) joint contains fibrocartilage. There is limited literature describing chondrocalcinosis (CC) of the AC joint. AC joint involvement with CC has been described as linear calcifications within the articular discs or punctuate calcifications [3]. In addition, CPPD crystal deposition disease may present on radiographs as a mass adjacent to the joint representing an AC joint cyst, pseudotumor, solitary tophus or calcified/cystic mass immediately adjacent to and cephalad above the joint space [4–6]. Digital imaging combined with picture archiving and communication system (PACS) allows effective image retrieval and optimal interpretation using image manipulation. While AC joint CC is easily visible on routine chest radiographs, no data are available concerning prevalence or association with CPPD deposits in other joints. The purpose of this study was to determine if careful examination of the AC joints using optimized PACS imaging of routine chest films would be useful in identifying CC.
Materials and methods
Approval was obtained from the institutional review board.
Data collection
Medical record review identified 1,920 consecutive outpatients aged 50 or older who had received routine posterior-anterior chest radiographs during a 4-month period between January to April 2011. Knee radiographs were available for comparison in 489 patients.
Radiograph assessment
All radiographs were performed using direct digital radiographic systems or computed radiographic systems with focal spot size of 0.6 mm. Detector resolution for computed radiographic systems was 5 pixels/mm, and resolution for digital radiographic systems was either 2.5 or 3.5 line pairs/mm. All radiographs were performed with a kVp between 117 and 125, and all were controlled with automatic exposure. Examinations were reviewed using the McKesson HRS-A PACS system and workstations, with nominal 3-megapixel monitors (6-megapixel dual-split monitors). Image manipulation including window and level adjustment and magnification was applied as needed to optimize image interpretation. Retrospective radiographic readings and chart reviews involving all 1,920 patients were performed. All chest radiographs were evaluated by one of five subspecialty-trained musculoskeletal radiologists. Radiographs were evaluated to determine if one or both AC joints were visible. If one or both joints were adequately demonstrated, CC was reported as present or absent. If knee radiographs were available, CC was reported as present or absent. Medical records were reviewed to abstract demographics, chest film reports, and clinical diagnoses.
Statistical analysis
The association between age and prevalence of CC was determined by using the Wilcoxon rank sum test. Fisher’s exact test was applied to explore the relationship between the presence of AC CC and knee CC, and the association of AC joint CC with a documented history of a diagnosis of pseudogout, calcium pyrophosphate disease, or CC in the medical records. All statistical analyses were performed using the GraphPad Prism software.
Results
There were 1,056 females and 864 males, with mean age of 66 years (range, 50–96). AC joint CC was identified in 21 subjects, with a prevalence of 1.1 % (21/1,920) of chest films (Fig. 1). The age distribution of the patients was as follows: 0.29 % (2/675) patients aged 50–59, 0.82 % (5/609) aged 60–69, 1.34 % (5/373) aged 70–79 and 3.42 % (9/263) aged 80 or older (Fig, 2). Patients with AC joint CC were 75 (±11.6 SD) years of age versus 65,4 (±10.5 SD) in those without CC. A strong association was found between age and prevalence of AC joint CC (p=0.0002, Wilcoxon rank sum test). There was no significant gender difference in the prevalence of AC joint CC (p=0.35) (Fig. 3). Four hundred eighty-nine patients had knee films. Six of these patients had AC joint CC, and of these, five also had knee CC (83 %). Of the 483 without AC joint CC, 62 (12 %) had knee CC (p=0.002, Fisher’s exact). Of the patients with AC joint CC, only 14 % had a diagnosis of CPPD recorded on the chart, and none had AC joint calcification noted on the official radiology report. Patients with AC joint CC were more likely to have a recorded history of CPPD crystal disease than those without AC joint CC (14 versus 1 %, p=0.0017, Fisher’s exact test).
Fig. 1.
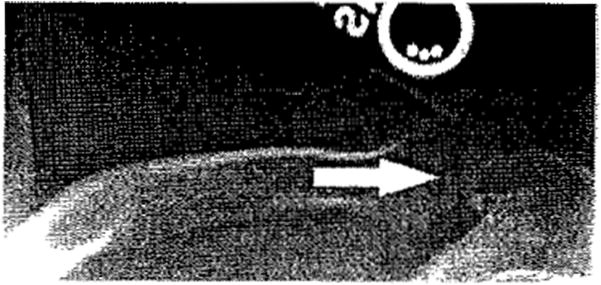
84-year-old female with left AC joint chondrocalcinosis on routine chest radiograph and history of CPPD crystal deposition in the chart
Fig. 2.
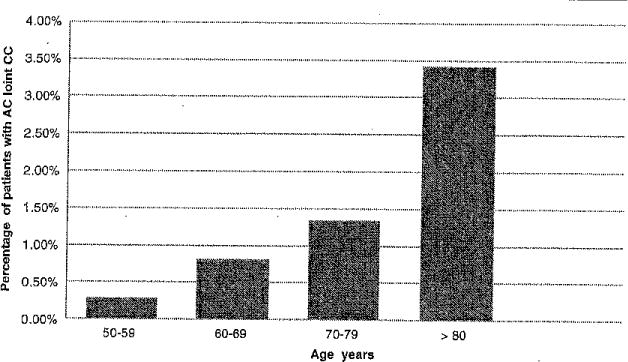
The prevalence of patients with acromioclavicular joint chondrocalcinosis by age group
Fig. 3.
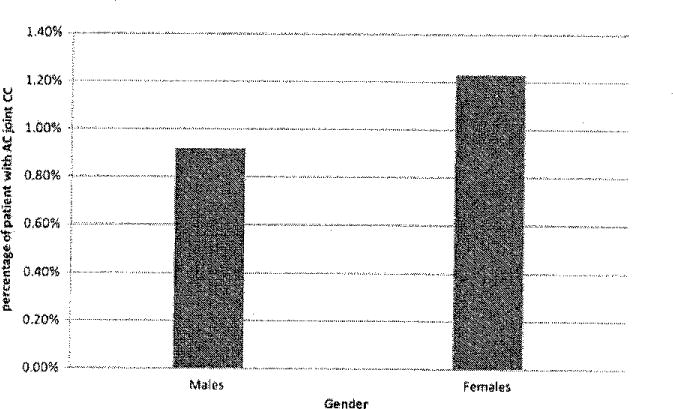
The prevalence of patients with acromioclavicular joint chondrocalcinosis by gender
Discussion
The deposition of CPPD crystals occurs within the hyaline cartilage and especially within fibrocartilages. The AC articulation is a diarthrodial joint formed by the distal clavicle and acromion. It contains a fibrocartilaginous infra-articular disc [7]. To our knowledge, this is the first study investigating the prevalence of AC joint CC and its association with CC/CPPD. By using digital imaging and PACS software magnification, AC joint CC is discernible on routine chest films. We found a 1.1 % prevalence of AC joint CC in routine chest x-rays obtained in the outpatient setting. When present, AC joint CC often indicates associated knee CC. This study confirms a previous report that CC is an age-related condition, with equal prevalence in men and women [8]. The prevalence of AC joint CC is less frequent than knee CC, because AC joint osteoarthritis is a common finding on chest radiographs in elderly patients. We believe that CPPD crystal deposition disease is associated with osteoarthritis, cartilage loss during the degenerative process, and CC may not be always present on imaging studies. AC joint CC is most often overlooked by radiologists interpreting routine chest images. Rheumatologists (and radiologists) should consider assessing available chest films for AC joint CC. A finding of AC joint CC could heighten suspicion of pseudogout or secondary osteoarthritis in appropriate clinical settings. AC joint CC in a young patient, although we did not include patients younger of 50 years old, should alert the clinician to the possibility of an associated metabolic condition such as hemochromatosis, hypomagnesemia, hypophosphatasia, hyperparathyroidism, and possibly hypothyroidism [9]. For these reasons, scrutinizing routine chest films to assess for CC in the AC joints is worthwhile. Such scrutiny is without additional financial cost and requires very little time for the interpreting reader.
Acknowledgments
The authors would like to acknowledge Dan Eastwood and Alexis Visotcky for their assistance with the statistical analysis. We are all grateful to the support received by grant 8UL1TR000055 from the Clinical and Translational Science Award (CTSA) programme of the National Center for Advancing Translational Sciences.
Footnotes
Disclosures None.
Contributor Information
Konstantinos Parperis, Email: kparperis@mcw.edu, Division of Rheumatology, Medical College of Wisconsin, 9200 West Wisconsin Avenue, Milwaukee, WI 53226, USA.
Guillermo Carrera, Department of Radiology, Medical College of Wisconsin, Milwaukee, WI, USA.
Keith Baynes, Department of Radiology, Medical College of Wisconsin, Milwaukee, WI, USA.
Alan Mautz, Department of Radiology, Medical College of Wisconsin, Milwaukee, WI, USA.
Melissa DuBois, Department of Radiology, Medical College of Wisconsin, Milwaukee, WI, USA.
Ross Cerniglia, Department of Radiology, Medical College of Wisconsin, Milwaukee, WI, USA.
Lawrence M. Ryan, Division of Rheumatology, Medical College of Wisconsin, 9200 West Wisconsin Avenue, Milwaukee, WI 53226, USA
References
- 1.McCarty DJ. Crystals and arthritis. Dis Mon. 1994;40:255–299. doi: 10.1016/0011-5029(94)90021-3. [DOI] [PubMed] [Google Scholar]
- 2.Resnick D, Niwayama G, Goergen TG, Utsinger PD, Shapiro RF, Haselwood DH, Wiesner KB. Clinical, radiographic and pathologic abnormalities in calcium pyrophosphate cehydrate deposition disease (CPPD): pseudogout. Radiology. 1977;122(l):l–15. doi: 10.1148/122.1.1. [DOI] [PubMed] [Google Scholar]
- 3.Huang GS, Bachmann D, Taylor JA, Marcelis S, Haghighi P, Resnick D. Calcium pyrophosphate dehydrate crystal deposition disease and pseudogout of the acromioclavicular joint: radiographic and pathologic features. J Rheumatol. 1993;20(12):2077–2082. [PubMed] [Google Scholar]
- 4.Tshering Vogel DW, Steinbach LS, Hertel R, Bcmhard J, Stauffer B, Anderson SE. Acromioclavicular joint cyst: nine cases of a pseudotumor of the shoulder. Skeletal Radiol. 2005;34(5):260–265. doi: 10.1007/s00256-004-0883-6. [DOI] [PubMed] [Google Scholar]
- 5.Marcove RC, Wolfe SW, Healey JH, Huvos AG, Boskey A, Fleisher M. Massive solitary tophus containing calcium pyrophosphate dihydrate crystals at the acromioclavicular joint. Clin Orthop Relat Res. 1998;27:305–309. [PubMed] [Google Scholar]
- 6.Cooper AM, Hayward C, Williams BD. Calcium pyrophosphate deposition disease—involvement of the acromioclavicular joint with pseudocyst formation. Br J Rheumatol. 1993;32(3):248–250. doi: 10.1093/rheumatology/32.3.248. [DOI] [PubMed] [Google Scholar]
- 7.Renfree KJ, Wright TW. Anatomy and biomechanics of the acromioclavicular and sternoclavicular joints. Clin Spoils Med. 2003;22(2):219–238. doi: 10.1016/s0278-5919(02)00104-7. [DOI] [PubMed] [Google Scholar]
- 8.Neame RL, Carr AJ, Muir K, Doherty M. UK community prevalence of knee chondrocalcinosis: evidence that correlation with osteoarthritis is through a shared association with osteophyte. Ann Rheum Dis. 2003;62(6):513–518. doi: 10.1136/ard.62.6.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenthal AK, Ryan LM. Calcium pyrophosphate crystal deposition disease, pseudogout, and articular chondrocalcinosis. In: Koopman WJ, editor. Arthritis and allied conditions: a textbook of rheumatology. 14th. Lippincott Williams and Wilkins; Philadelphia: 2001. pp. 2348–2371. [Google Scholar]


