Abstract
Purpose
Incisional hernia (IH) is a common complication after colectomy, with impacts on both healthcare utilization and quality of life. The true incidence of IH after minimally invasive colectomy is not well described. The purpose of this study was to examine the IH incidence after minimally invasive right colectomies (RC), and to compare the IH rate after laparoscopic (L-RC) and robotic (R-RC) colectomies.
Methods
This is a retrospective review of patients undergoing minimally invasive RC at a single institution from 2009–2014. Only patients undergoing RC for colonic neoplasia were included. Patients with previous colectomy or intraperitoneal chemotherapy were excluded. Three L-RC patients were included for each R-RC patient. The primary outcome was incisional hernia (IH) rate based on clinical examination or computed tomography (CT). Univariate and multivariate time-to-event analyses were used to assess predictors of IH.
Results
276 patients where included, of which 69 had undergone R-RHC and 207 L-RHC. Patient and tumor characteristics were similar between the groups, except for higher tumor stage in L-RC patients. Both the median time to diagnosis (9.2 months) and the overall IH rate were similar between the groups (17.4% for R-RHC and 22.2% for L-RHC), as were all other postoperative complications. In multivariable analyses, the only significant predictor of IH was former or current tobacco use (HR 3.0, p=0.03).
Conclusions
This study suggests that the incidence of IH is high after minimally invasive colectomy, and that this rate is equivalent after R-RC and L-RC. Reducing the IH rate is an important opportunity for improving quality of life and reducing health care utilization after minimally invasive colectomy.
Keywords: Incisional Hernia, Robotic Colectomy, Laparoscopic Colectomy
Introduction
Minimally invasive techniques are increasingly utilized in colorectal surgery. Multiple randomized trials have shown equivalent oncologic outcomes for laparoscopy compared to open surgery for colorectal cancer, with improved postoperative pain and earlier return of bowel function.[1–4] Wound complications and resulting incisional hernias (IH) remain common problems that significantly impact both quality of life and healthcare utilization. The overall direct costs associated with IH repair range from 3,479-$16,404.[5, 6] In patients with recurrences the total cost may be nearly 5-fold higher. [5] Reducing incisional hernia rate will improve the quality of life of patients treated with laparoscopic surgery and reduce health care costs.
The DaVinci robotic platform has been claimed to facilitate minimally invasive colorectal surgery. Several retrospective studies have indicated that robotically assisted colectomy is a safe option in the treatment of colorectal cancer; at least one prospective study is expected to confirm this finding in rectal cancer.[7, 8] However, data comparing incisional hernia rate and other wound complications in patients treated with laparoscopic or robotic colectomy is limited.
The primary objective of this study, therefore, was to describe the rates of incisional hernia and postoperative complications after minimally invasive colectomy. Our secondary objective was to assess whether the introduction of robotic colectomy has affected the incidence of postoperative surgical site infections and IH. For this study, we chose to investigate the IH rate after minimally invasive right colectomies since the extraction site incision is likely to be vertically oriented and in the midline, and therefore are more prone to the development of incisional hernias.[9]
Methods
All patients who had undergone minimally invasive right colectomy (RC) from January 1, 2009 to March 1, 2014 were identified in the institutional database by CPT codes. Patients were included if they had undergone surgery for a benign or malignant tumor of colonic origin. Exclusion criteria were recurrent disease, intraperitoneal chemotherapy during or within 30 days of the index surgery, pathology consistent with primary lymphoma or tuberculosis, and patients who were lost to follow-up. Additional operative procedures during the index surgery were permitted, and long as they did not involve another intestinal anastomosis. This study was approved by the Institutional Review Board of Memorial Sloan Kettering Cancer Center.
All patients who had undergone robotically assisted extended or standard right colectomy (R-RC) were included in the study. For each patient who had undergone R-RC, 3 consecutive patients who had undergone laparoscopic right colectomy (L-RC) were selected. A retrospective review of the prospectively maintained electronic medical record (EMR) was carried out to collect clinical and demographic data. These data included age, gender, insurance carrier, previous abdominal surgeries, including caesarean section, previous abdominal wall hernias, smoking status, BMI and medical comorbidities, from which the Charlson Comorbidity Index (CCI) score could be calculated[10]. Operative details were collected including operative time, surgeon name, intracorporeal anastomosis technique, use of a stapler for the anastomosis, extraction site location, extraction site length (cm), conversion to open and concurrent procedures. Tumor characteristics of interest included AJCC stage and pathology (adenocarcinoma versus other).
Extensive review of the EMR was carried out by 2 of the researchers, with all complications graded according to the Clavien Dindo (CD) classification, and surgical site infections (SSI) classified according to the CDC-NSQIP criteria. Complications were recorded for 30 days after surgery, and readmission and emergency surgery for 90 days after the index operation. Outcomes of interest included length of stay (LOS), overall complications, highest CD complication grade, SSI, highest SSI grade, anastomotic leak, intraabdominal abscess, and ileus or small bowel obstruction (SBO); for the purposes of this study, a subject was considered to have had an ileus or SBO if based on documentation by a fellow or attending note, findings on imaging or by documentation of nasogastric tube insertion. Incisional hernias were identified both by surgical attendings’ notes during postoperative visits, and by evidence of discontinuity in the anterior abdominal wall fascia on postoperative CT scans. For all hernias seen only on imaging, and not noted by a clinician, two members of the research team reviewed the imaging.
Univariate analyses using t-test, chi-square and non-parametric alternatives were used to compare demographic, clinical and surgical characteristics between R-RC and L-RC cohorts. Postoperative complications and length of stay were similarly analyzed. The primary outcome of this study, the IH rate, was analyzed first using a log-rank test, and then univariate and multivariate Cox proportional hazards models stratified by surgeon. All observations were censored after 500 days in both groups; this was done to control for the differences in follow-up between R-RC and L-RC, given that relatively few R-RCs were done in the beginning of the study period. Covariates were chosen from those that were sufficiently different between L-RC and R-RC, and from a priori knowledge of relevant variables. Additional models using propensity scores and inverse probability weights were attempted given the large number of potential covariates. ultimately, the inference was not affected by these additional approaches. The final model was assessed for non-proportionality and statistical significance was set as p <0.05
Results
A total of 69 patients who underwent R-RC met the inclusion criteria. Accordingly, 207 L-RC patients were included, for an overall 3:1 ratio of patients. Table 1 demonstrates the preoperative clinical and demographic characteristics of these patients. Subjects were similar with respect to age, sex, CCI, BMI class, history of abdominal hernias, and smoking status. Patients undergoing L-RC had more advanced-staged disease and a significantly greater proportion of them had undergone previous abdominal surgeries.
Table 1.
Demographic and Clinical Characteristics
| Laparoscopic (n=207) |
Robotic (n=69) |
p | ||
|---|---|---|---|---|
| Age** years, median (IQR) | 64(22) | 66(20) | 0.23 | |
| Female n (%) | 122 (59) | 36 (52) | 0.33 | |
| Charlson Score n (%) | 0.23 | |||
| 0–2 | 80(39) | 19(28) | ||
| 3–5 | 96(46) | 39(57) | ||
| ≥ 6 | 31(15) | 11(16) | ||
| BMI n (%) | 0.83 | |||
| <25 | 74(36) | 22(32) | ||
| 25–29.9 | 69(33) | 23(33) | ||
| 30–34.9 | 44(21) | 17(25) | ||
| 35–39.9 | 10(5) | 5(7) | ||
| ≥ 40 | 10(5) | 2(3) | ||
| Previous Surgery n (%) | 99 (48) | 6 (9) | <0.01 | |
| Abdominal Hernia n (%) | 15 (7) | 7 (10) | 0.44 | |
| Tobacco Use n (%) | 0.32 | |||
| Never | 128 (62) | 38 (55) | ||
| Previous or Current | 79 (38) | 22 (45) | ||
| Surgeon Characteristics n (%) | <0.01 | |||
| Lap and Robotic | 180 (87) | 43 (62) | ||
| Only Lap or Robotic | 27 (13) | 26 (38) | ||
| Tumor Stage median (IQR) | 2(2) | 2(2) | 0.02 | |
| Payer | ||||
| Private Insurance/Out of Pocket | 95(46) | 31(45) | 0.89 | |
| Medicare/Medicaid | 112(54) | 38(55) | ||
Fisher’s Exact Test
Wilcoxon Rank Sum Test
Table 2 demonstrates the operative techniques of the cohorts. Subjects in the R-RC group were more likely to undergo intracorporeal anastomoses (16%), with no intracorporeal anastomoses performed in the L-RC group. Incision length was similar between the groups, with a median length of 5 cm. The majority of patients had a vertical midline incision as the extraction site, of which 16 were infraumbilical. There was a significant difference in the number of off-midline extraction incisions between the groups, with nearly 10% of R-RC cases having transverse or Pfannenstiel extraction sites, versus only 1% of L-RC cases.
Table 2.
Operative Details
| Laparoscopic (n=207) |
Robotic (n=69) |
p | ||
|---|---|---|---|---|
| Extraction Site* n (%) | <0.01 | |||
| Vertical, Midline | 205(99) | 62 (90) | ||
| Pfannenstiel | 0 | 6(9) | ||
| Off-midline, Transverse | 2(1) | 1(2) | ||
| Stapled Anastomosis* n (%) | 2(1) | 0(0) | >0.99 | |
| Incision Length** cm, median (IQR) | 5(2) | 5(2) | >0.99 | |
| Intracorporeal* n (%) | 0 | 11 (16) | <0.01 | |
Fisher’s Exact Test
Wilcoxon Rank Sum Test
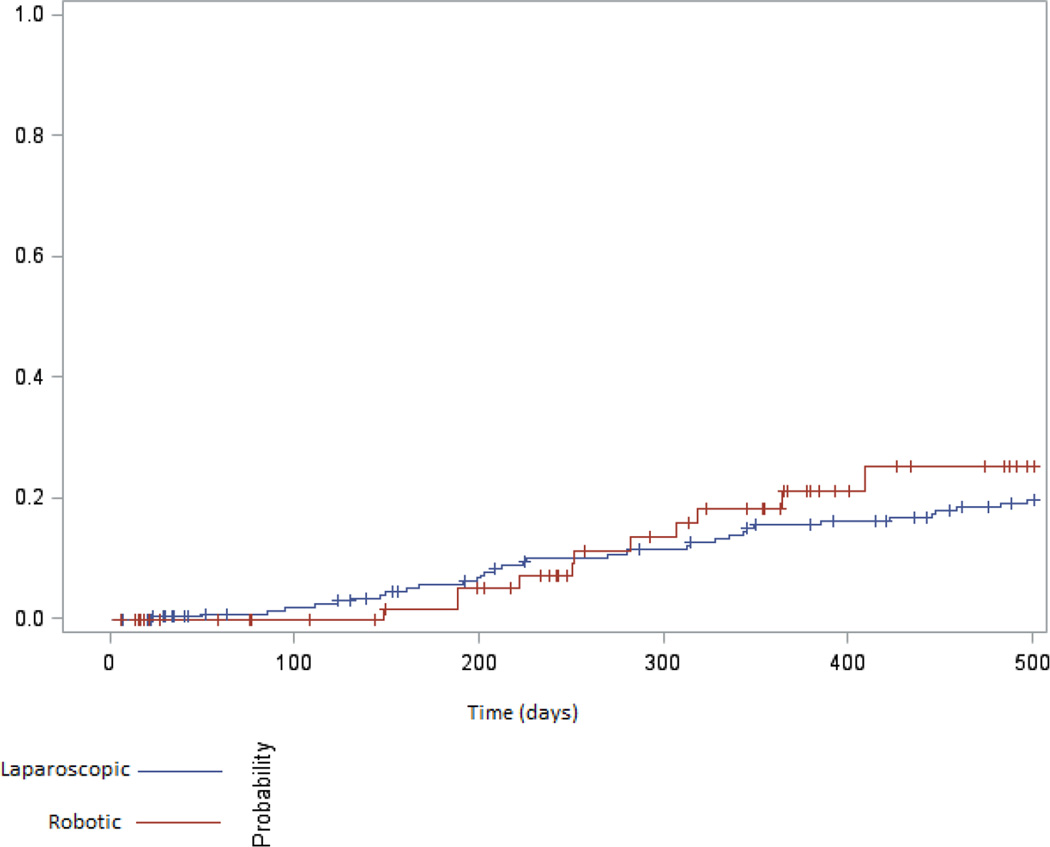
The 30-day postoperative outcomes are presented in Table 3. The operative time was longer in the R-RC group by a median of 32 minutes, but the rates of conversion to open were similar. The overall complication rate was similar between the two groups, with up to 34% of patients having at least one complication. The median CD grade of complications was 2 in both groups; however, there were no grade 4 complications in the R-RC group, versus 2 in the L-RC group. The two cohorts were similar in terms of all other outcomes including specific complications, readmissions and LOS. Long-term complications were also similar between the groups (Table 4). Follow-up time, however, was significantly different between the groups as R-RC was only recently adopted in our institution. The IH rate was17.4% (12/69) in the R-RC group compared to 22.2% (46/207) after L-RC (Table 4). The median time to IH diagnosis after surgery was 9.2 months, which was similar between the groups (Figure 1). Repair of IH was documented for 50% of R-RC patients and only 26% on L-RC patients.
Table 3.
Thirty-day Postoperative Outcomes: Univariate Analyses
| Laparoscopic (n=207) |
Robotic (n=69) |
p | |
|---|---|---|---|
| Mortality n (%) | 0 | 0 | -- |
| Op Time** m, median (IQR) | 128(57) | 160(51) | <0.01 |
| Conversion to Open n (%) | 4 (2) | 2(3) | 0.47 |
| Any Complication n (%) | 71 (34) | 22 (32) | 0.71 |
| Highest CD Grade* n (%) | 2(1) | 2(1) | 0.10 |
| SSI n (%) | 26 (13) | 10 (15) | 0.68 |
| Highest SSI* n (%) | 1(0) | 1(1) | >0.99 |
| Anastomotic Leak* n (%) | 1 (1) | 0 | >0.99 |
| Abscess* n (%) | 2 (1) | 2 (3) | 0.26 |
| Ileus or SBO* n (%) | 10 (5) | 4 (6) | 0.48 |
| Add. Operations* n (%) | 3 (2) | 1 (2) | 0.69 |
| LOS ** days, median (IQR) | 5(2) | 5(2) | 0.84 |
| Readmission in 30 days* n (%) | 12 (6) | 5 (7) | 0.43 |
Fisher’s Exact Test
Wilcoxon Rank Sum Test
Table 4.
Long-term Postoperative Outcomes: Univariate Analyses
| Laparoscopic (n=207) |
Robotic (n=69) |
p | |
|---|---|---|---|
| Readmission in 90 days* n (%) | 19 (9) | 5 (7) | 0.62 |
| Multiple Readmissions* n (%) | 1 (1) | 1 (2) | 0.44 |
| Follow-Up days, median (IQR) | 910(621) | 364(269) | <0.01 |
| Incisional Hernia n (%) | 46 (22) | 12(17) | 0.39 |
| Days to IH Diagnosis** median(IQR) | 313(268) | 266(136) | 0.68 |
| Hernia Repair* n (%) | 12(26) | 6(50) | 0.11 |
Fisher’s Exact Test
Wilcoxon Rank Sum Test
Figure 1.
Time to event analysis: IH after Robotic and Laparoscopic RC
Table 5 shows the univariate and multivariate Cox proportional hazards models predicting IH rate. On univariate analysis, SSI was a significant predictor of IH, and current or former tobacco use had a trend towards significance. On multivariable modeling tobacco use was the sole statistically significant variable predicting IH. Additional models using propensity scores and inverse probability weights did not affect our results, and therefore are not reported.
Table 5.
Univariate and Multivariate Cox Proportional Hazards Models Predicting Incisional Hernia
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| HR* | 95% CI | p | HR | 95% CI | p | |
| Robotic | 1.4 | 0.6–3.1 | 0.40 | 1.3 | 0.5–3.2 | 0. |
| Age | 1.0 | 1.0–1.1 | 0.61 | 1.0 | 1.0–1.02 | 0.82 |
| Female Sex | 1.6 | 0.9–2.9 | 0.14 | 1.6 | 0.8–3.0 | 0.15 |
| Tumor Stage | 0.9 | 0.7–1.2 | 0.50 | 0.8 | 0.6–1.1 | 0.24 |
| Intracorporeal | 0.9 | 0.1–0.7 | 0.93 | 0.4 | 0.0–4.5 | 0.46 |
| Midline Extraction Site | 2.1 | 1.1–4.3 | 0.03 | 0.4 | 0.1–2.0 | 0.25 |
| SSI | 2.1 | 1.1–4.3 | 0.03 | 2.0 | 1.0–4.0 | 0.06 |
| Previous Abdominal Hernia | 1.3 | 0.5–3.2 | 0.62 | 1.2 | 0.4–3.3 | 0.72 |
| Previous Abdominal Surgery | 1.6 | 0.9–2.8 | 0.14 | 1.7 | 0.9–3.4 | 0.11 |
| Tobacco Use | 1.8 | 1.0–3.1 | 0.05 | 2.0 | 1.0–3.5 | 0.04 |
Hazards ratio
Discussion
In this study, we report a high rate of IH after minimally invasive right colectomy. After controlling for multiple clinical and operative factors, nearly 20% of patients developed IH within 1 year of minimally invasive RC. In addition, our results indicate that there is no difference in IH rate between robotic and laparoscopic approaches. Finally, this study shows that other postoperative outcomes after R-RC and L-RC are similar.
The natural history and true incidence of IH after minimally invasive colectomy have not been well described. In a 2008 Cochrane review, only 2 trials reported IH rates after laparoscopic colectomy, and with significantly different results (4.7 and 23%).[11–14] Data regarding the IH rate after robotic colectomy are even sparser. In a recent meta-analysis of 6 R-RC versus L-RC trials, only 3 studies reported the IH rate; in a total of 70 R-RC patients, the IH rate was 1%.[15] In all 3 studies, the IH rate was not the primary outcome, and the method of diagnosing IH was not described.
The IH rate after R-RC in our study is much higher than has been previously reported. This is not surprising since previous studies have had relatively short lengths of follow-up after R-RC. In addition, they likely reported only clinically symptomatic IH or those that required repair. This has been shown to underestimate the true incidence of IH by up to 23%.[15, 16] We know that a proportion of these radiologically-diagnosed IH will eventually become symptomatic if given a long enough follow-up period, which is why chose to include these in our study.
Our results also show that the SSI and IH rates are equivalent after R-RC and L-RC. To some degree this is to be expected since the majority of cases in both groups were performed with extracorporeal anastomoses using vertical, midline extraction incisions. This approach is associated with increased rates of IH compared to off-midline extractions sites, such as a Pfannenstiel incision.[9, 14, 17, 18] In our study, only 10% of R-RC and only 1 L-RC case were performed with alternative incisions and there were no IH in Pfannenstiel incisions. In addition, all Pfannenstiel incisions and the majority of other non-midline incisions were performed in the 11 patients undergoing intracorporeal anastomoses. These findings suggest that a potential advantage of R-RC is that it facilitates the creation of an intracorporeal anastomosis, which in turn permits optimal placement of the extraction site incision.
An unexpected finding was that elective repair was documented for 50% of R-RC patients and only 26% of L-RC patients. The reasons for this discrepancy are unclear. The follow-up period in the L-RC group was longer than in the R-RC group, making underreporting due to loss of follow-up unlikely. It is possible that more L-RC patients had later staged disease, and may have had to forego or delay repair due to adjuvant chemotherapy. In addition, we found that the operative time for R-RC was significantly longer, likely reflecting our institution’s learning curve with this new technology.
The strengths of this study include its size, and the fact that it was performed at a single institution where the majority of the patients are followed for a significant length of time. In addition, as our patients routinely undergo CT scans for cancer surveillance, identifying IH by clinical and CT criteria is feasible. The limitations of this study lie in its retrospective design, and the differences in follow-up time between the two groups. Though the average time to IH diagnosis ranges from 3 weeks to 2.8 years, at least one study has reported IH diagnoses up to 5 years after surgery.[19]
In conclusion, the rate of IH is high after minimally invasive RC, and appears to be similar after R-RC and L-RC performed when midline, vertical incision are used for the anastomosis and specimen extraction. All other postoperative outcomes were also similar between the groups. Incisional hernia is an important complication after colectomy for cancer and exploring methods for reducing the IH rate represents an important opportunity for improving QoL and reducing health care utilization in colorectal surgery.
Footnotes
Disclosures
MW declares no conflict of interest.
MK declares no conflict of interest.
PB declares no conflict of interest.
JG declares no conflict of interest.
GN declares no conflict of interest.
LT declares no conflict of interest.
JGA declares no conflict of interest.
MW declares no conflict of interest.
PP declares no conflict of interest.
References
- 1.Jayne DG, et al. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007;25(21):3061–3068. doi: 10.1200/JCO.2006.09.7758. [DOI] [PubMed] [Google Scholar]
- 2.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Green BL, et al. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg. 2013;100(1):75–82. doi: 10.1002/bjs.8945. [DOI] [PubMed] [Google Scholar]
- 4.Schwenk W, et al. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005;(3):CD003145. doi: 10.1002/14651858.CD003145.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aquina CT, et al. Surgeon volume plays a significant role in outcomes and cost following open incisional hernia repair. J Gastrointest Surg. 2015;19(1):100–110. doi: 10.1007/s11605-014-2627-9. discussion 110. [DOI] [PubMed] [Google Scholar]
- 6.Poulose BK, et al. Epidemiology and cost of ventral hernia repair: making the case for hernia research. Hernia. 2012;16(2):179–183. doi: 10.1007/s10029-011-0879-9. [DOI] [PubMed] [Google Scholar]
- 7.Hellan M, et al. Robotic Rectal Cancer Resection: A Retrospective Multicenter Analysis. Ann Surg Oncol. 2014 doi: 10.1245/s10434-014-4278-1. [DOI] [PubMed] [Google Scholar]
- 8.Collinson FJ, et al. An international, multicentre, prospective, randomised, controlled, unblinded, parallel-group trial of robotic-assisted versus standard laparoscopic surgery for the curative treatment of rectal cancer. Int J Colorectal Dis. 2012;27(2):233–241. doi: 10.1007/s00384-011-1313-6. [DOI] [PubMed] [Google Scholar]
- 9.Samia H, et al. Extraction site location and incisional hernias after laparoscopic colorectal surgery: should we be avoiding the midline? Am J Surg. 2013;205(3):264–267. doi: 10.1016/j.amjsurg.2013.01.006. discussion 268. [DOI] [PubMed] [Google Scholar]
- 10.Charlson M, et al. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 11.Kuhry E, et al. Long-term outcome of laparoscopic surgery for colorectal cancer: a cochrane systematic review of randomised controlled trials. Cancer Treat Rev. 2008;34(6):498–504. doi: 10.1016/j.ctrv.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 12.Winslow ER, et al. Wound complications of laparoscopic vs open colectomy. Surg Endosc. 2002;16(10):1420–1425. doi: 10.1007/s00464-002-8837-3. [DOI] [PubMed] [Google Scholar]
- 13.Braga M, et al. Laparoscopic vs. open colectomy in cancer patients: long-term complications, quality of life, and survival. Dis Colon Rectum. 2005;48(12):2217–2223. doi: 10.1007/s10350-005-0185-7. [DOI] [PubMed] [Google Scholar]
- 14.Navaratnam AV, et al. Incisional hernia rate after laparoscopic colorectal resection is reduced with standardisation of specimen extraction. Ann R Coll Surg Engl. 2015;97(1):17–21. doi: 10.1308/003588414X14055925058274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Petrucciani N, et al. Robotic right colectomy: A worthwhile procedure? Results of a metaanalysis of trials comparing robotic versus laparoscopic right colectomy. J Minim Access Surg. 2015;11(1):22–28. doi: 10.4103/0972-9941.147678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baucom RB, et al. Prospective evaluation of surgeon physical examination for detection of incisional hernias. J Am Coll Surg. 2014;218(3):363–366. doi: 10.1016/j.jamcollsurg.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 17.Lee L, et al. High incidence of symptomatic incisional hernia after midline extraction in laparoscopic colon resection. Surg Endosc. 2012;26(11):3180–3185. doi: 10.1007/s00464-012-2311-7. [DOI] [PubMed] [Google Scholar]
- 18.DeSouza A, et al. Incisional hernia, midline versus low transverse incision: what is the ideal incision for specimen extraction and hand-assisted laparoscopy? Surg Endosc. 2011;25(4):1031–1036. doi: 10.1007/s00464-010-1309-2. [DOI] [PubMed] [Google Scholar]
- 19.Mudge M, Hughes LE. Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg. 1985;72(1):70–71. doi: 10.1002/bjs.1800720127. [DOI] [PubMed] [Google Scholar]