Abstract
Background and aims
People with mental illnesses and substance abuse disorders are important targets for smoking cessation interventions. Mental health professionals (MHPs) are ideally placed to deliver interventions, but their attitudes may prevent this. This systematic review therefore aimed to identify and estimate quantitatively MHPs attitudes towards smoking and main barriers for providing smoking cessation support and to explore these attitudes in‐depth through qualitative synthesis.
Methods
The online databases AMED, EMBASE, Medline, PsychINFO, HMIC and CINAHL were searched in March 2015 using terms relating to three concepts: ‘attitudes’, ‘mental health professionals’ and ‘smoking cessation’. Quantitative or qualitative studies of any type were included. Proportions of MHPs' attitudes towards smoking and smoking cessation were pooled across studies using random effects meta‐analysis. Qualitative findings were evaluated using thematic synthesis.
Results
Thirty‐eight studies including 16 369 participants were eligible for inclusion. Pooled proportions revealed that 42.2% [95% confidence interval (CI) = 35.7–48.8] of MHPs reported perceived barriers to smoking cessation interventions, 40.5% (95% CI = 30.4–51.0) negative attitudes towards smoking cessation and 45.0% (95% CI = 31.9–58.4) permissive attitudes towards smoking. The most commonly held beliefs were that patients are not interested in quitting (51.4%, 95% CI = 33.4–69.2) and that quitting smoking is too much for patients to take on (38%, 95% CI = 16.4–62.6). Qualitative findings were consistent with quantitative results, revealing a culture of smoking as ‘the norm’ and a perception of cigarettes as a useful tool for patients and staff.
Conclusions
A significant proportion of mental health professionals hold attitudes and misconceptions that may undermine the delivery of smoking cessation interventions; many report a lack of time, training and confidence as main barriers to addressing smoking in their patients.
Keywords: Attitudes, health care professionals, mental health, meta‐analysis, psychiatric patients, systematic review, tobacco treatment
Introduction
The prevalence of smoking among people with mental illnesses and substance use disorders is much higher than in the general population. Smoking rates stand at above 70% for those with severe mental illnesses such as schizophrenia and bipolar disorder 1, 2, 3, are similarly high among individuals with substance use disorders 4, 5 and are also above average for those with common mental disorders, including depression and anxiety 1. People with mental illness or substance use disorders are more likely to be heavier and more dependent smokers 6, 7, and their life expectancy is reduced by up to 20 years 8, 9, mainly because of smoking 7. It is therefore vital that smokers from this population receive effective smoking cessation interventions.
Mental health professionals (MHPs), broadly defined as those who received specialist training to offer services designed to improve an individual's mental health (such as clinical psychologists, psychiatrists, clinical social workers and psychiatric nurses), have a crucial role in reducing tobacco smoking among people with mental illness, as they are best placed to encourage and support smokers to quit 10. Indeed, UK clinical guidelines on smoking cessation in secondary care advise that all health and social care practitioners in in‐patient and community‐based mental health services identify smokers and offer advice and assistance to quit 11. However, smokers with mental illness are less likely to be offered advice and support to quit than those without 12, 13.
One possible barrier to the delivery of smoking cessation intervention is MHPs' attitudes towards and beliefs about smoking and/or smoking cessation among individuals with mental illnesses and substance abuse disorders. For instance, previous research has identified that some hold concerns that patients' mental health or abstinence will suffer 14, 15, 16, 17 and that smokers are unable 18 or unmotivated to quit 19. This is in contrast to evidence that smoking cessation, if not actually benefitting mental health, does not impact mental health negatively in people with or without psychiatric disorders 20, even in life‐long, long‐term smokers 21, and that smokers with mental illnesses are just as likely to want to quit as smokers without 22. MHPs have also been reported to hold permissive attitudes towards smoking, such as the belief that smoking with patients can help build a therapeutic relationship 15, 23, 24 and that allowing patients to smoke ensures a smoother running of wards in in‐patient settings 19.
To implement smoking cessation interventions effectively for people with mental illness and substance abuse disorders, it is necessary to understand the relevant attitudes and beliefs of MHPs who engage with these individuals. Such an understanding would lead to greater insight into the potential barriers to delivering smoking cessation support which, in turn, can then inform strategies to reduce tobacco use. However, to our knowledge, there has been no recent systematic investigation of MHPs' attitudes to smoking cessation to identify possible barriers, if any.
The current systematic review and meta‐analysis aims to synthesize the qualitative and quantitative literature on MHPs' attitudes towards smoking and smoking cessation among people with mental illnesses and/or substance abuse disorders. Specifically, it sought to (a) identify and estimate quantitatively MHPs' attitudes towards smoking and main barriers for providing smoking cessation support such as negative attitudes towards smoking cessation and permissive attitudes towards smoking, and (b) to explore these attitudes towards smoking, smoking cessation and support in‐depth through qualitative synthesis.
Methods
The current review followed Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines 25.
Search strategy
The literature was searched for studies reporting on MHPs' beliefs and attitudes relating to smoking among people with mental illnesses and substance use disorders. An initial search strategy was developed in the databases Medline and Embase, and through the identification of key terms used commonly in the literature.
The main keywords used in the search strategy were structured around three key concepts: ‘attitudes’, ‘mental health professionals’ and ‘smoking’, and customized to each database. The final search was conducted on 17 March 2015 in the following databases: AMED (OVID platform), CINAHL (EBSCO platform), classic + Embase, Embase, HMIC Health Management Information Consortium, Medline and PsycINFO (OVID platform) (see Supporting information, Table S1 for full search strategy and number of records identified). To find further eligible papers, forward and backward citation searches of included studies were also conducted.
Eligibility screening
Studies were eligible for inclusion if they met the following criteria:
The sample was health‐care professionals working in mental health, drug or alcohol treatment (referred to as MHPs throughout).
The study measured attitudes/beliefs related to patients' smoking or the delivery of smoking cessation support/advice to patients.
It was a primary quantitative or qualitative study published in a peer‐reviewed journal (only baseline data from longitudinal or experimental studies were eligible for inclusion to provide unbiased, background estimates).
Studies were excluded if they were not in the English language, focused only on attitudes towards smoke‐free policies, were based on child and adolescent services (the focus of this review was adult services), if the sample was composed only of health professionals in training or if they were published prior to 2003. This date limit was chosen as this was the year in which the World Health Organization Framework Convention of Tobacco Control (WHO FCTC) was published. The WHO FCTC states that parties to the convention should adopt or implement legislation that promotes training on tobacco control for health workers, community workers and social workers 26. As the FCTC was widely ratified and embraced, with 168 signatories, we judged that the date of its publication would serve as an appropriate marker for a shift in MHPs' attitudes towards tobacco and its treatment and capture the most accurate indication of current attitudes.
An inclusion/exclusion criteria checklist was used to screen located articles for inclusion. To establish the reliability of the checklist, two independent reviewers (K.S. and I.T.) screened a random subset (34%) of papers, yielding excellent reliability (Cohen's kappa = 0.95). Disagreements were resolved through discussion.
Quality appraisal
Studies were evaluated with the Mixed Methods Appraisal Tool (MMAT), which has good validity and reliability 27, 28, 29. For quantitative studies, the MMAT includes three subsections distinguishing between randomized controlled trials, non‐randomized comparative studies and descriptive studies. For the current review, the ‘descriptive’ subsection was used for the appraisal of all included quantitative studies (including where baseline data had been extracted from pre‐test–post‐test or longitudinal studies), as only baseline data and non‐comparative findings were extracted for the purpose of this review.
Data extraction and synthesis
Data were extracted by one researcher (K.S.) using a standardized data extraction form to provide consistency, reduce bias and increase validity and reliability 30.
Quantitative studies
For quantitative studies, all measures of MHPs' attitudes or beliefs relating to smoking among patients or the delivery of smoking cessation support to patients were extracted. Measures of attitudes towards smoke‐free policies and attitudes reported by patients were not extracted. Extracted measures deemed to be reflective of the same beliefs or attitudes were grouped into categories by K.S. and L.S. These categories were organized further into higher‐level grouping on the basis of the types of attitudes or beliefs they represented. The proportion of participants reporting either negative attitudes towards providing smoking cessation support or permissive attitudes towards patients' smoking was extracted for measures within each category. Proportions were extracted systematically using predefined criteria (see Box 1). If relevant data were not included in published reports, authors were contacted to request data.
| Box 1. Guidelines for the extraction of proportions | |
| Response option | Method |
| Dichotomous (e.g. yes/no) | The proportion of participants choosing either ‘yes’ or ‘no’, depending on which indicated a negative attitude |
| Yes/unsure/no | The proportion of participants choosing either ‘yes’ or ‘no’, depending on which indicated a negative attitude |
| 4‐point scale | The proportion of participants choosing ‘3’ or ‘4’ OR the proportion of participants choosing ‘1’ or ‘2’, depending on which indicated a negative attitude |
| 5‐point scale | The proportion of participants choosing ‘4’ or ‘5’ OR the proportion of participants choosing ‘1’ or ‘2’, depending on which indicated a negative attitude |
| 6‐point scale | The proportion of participants choosing within the range of 4–6 OR the proportion of participants choosing within the range of 1–3, depending on which indicated a negative attitude |
| 7‐point scale | The proportion of participants choosing within the range of 5–7 OR the proportion of participants choosing 1–3, depending on which indicated a negative attitude |
| 10‐point scale | The proportion of participants responding within the range of 1–4 OR the proportion of participants responding within the range of 7–10, depending on which indicated a negative attitude |
| 100‐point scale | The proportion of participants responding within the range of 1–40 OR the proportion of participants responding within the range of 70–100, depending on which indicated a negative attitude |
Where more than one measure from a single study was included in a category, the mean proportion across measures was calculated prior to pooling. Pooling of proportions within each category and within the higher‐level groups was carried out in Stata version 13 using standard methodology 31. Proportions were first transformed using the Freeman–Tukey double arcsine method, pooled with a random effects meta‐analysis with the ‘metan’ command to account for heterogeneity, and then back‐transformed to proportions. Heterogeneity was assessed with the I 2 statistic 32. Only categories for which data were available from two or more studies were included in the data synthesis to allow for confidence in the accuracy of the findings.
Additionally, a meta‐regression was conducted to examine whether study characteristics were predictive of study outcomes using the ‘metareg’ command in Stata. Following convention 33, only outcomes with data from at least 10 studies were analysed. Study‐level covariates included in the analysis, thought to potentially influence outcomes, were year of publication (pre‐2010/2010‐onwards, based on a median split), country (US/non‐US) and service type (mental health services/drug and alcohol services). All study‐level covariates were entered into the same model concurrently, and values were adjusted for multiple comparisons.
Qualitative studies
All text contained in the ‘Results’ or ‘Findings’ section was extracted from published reports and analysed using thematic synthesis. First, textual data were coded line‐by‐line and were then categorized by similarity to generate descriptive themes occurring across included studies 34. Line‐by‐line coding and theme generation was carried out independently by two coders (K.S. and I.T.) and agreed in discussion to establish reliability. As some qualitative studies included interview questions focused on smoke‐free policies, and/or included data gathered from interviews with patients, lines in which findings were related explicitly to smoke‐free policy or attributed to patients were not included in the coding.
Results
Search results
Database searches yielded a total of 327 records after the removal of duplicates. After full‐text screening, 33 papers met inclusion criteria. Forward/backward citation searches yielded an additional eight papers, resulting in a total of 41 papers reporting on 38 studies being included in this review (Fig. 1).
Figure 1.
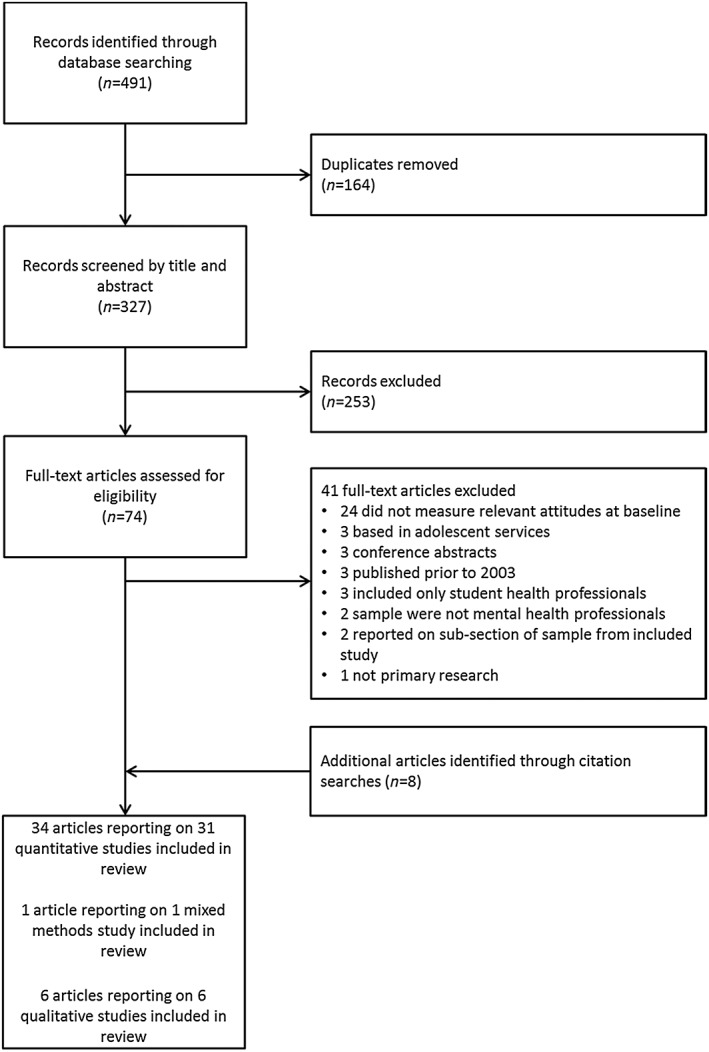
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram
Of the included studies, 31 used a quantitative methodology, six were qualitative and one employed a mixed‐methods approach. The total number of participants across quantitative studies (including the mixed‐methods study) was 16 215. One qualitative study 35 did not report a sample size; across the remainder the total sample size was 154, resulting in a total sample of 16,369 participants across all included studies. The majority of studies recruited MHPs from a range of professional roles (including nurses, psychiatrists and clinical psychologists) were set in a mental health‐care context and conducted in the United States (see Table 1 for details).
Table 1.
Characteristics of included studies.
| First author (Reference ) | Country | Study design | Data collection method | Sample | Recruitment/setting | Sample size | Response rate |
|---|---|---|---|---|---|---|---|
| Akpanudo 49 | USA | Cross‐sectional survey | Mailed self‐report questionnaire | Clinical psychologists | Random sample selected from the National Register of Health Service Providers in Psychology | 352 | 57% |
| Amole 50 | USA | Pre‐test–post‐test | Online self‐report questionnaire | Psychiatric nurses | Convenience sample in Georgia, USA, obtained through the American Nurses Crendentialling Centre | 201 | Not reported |
| Ashton 39 | Australia | Mixed methods | Mailed self‐report questionnaire with closed and open response options | Range of staff | Government and non‐government mental health services in Adelaide, South Australia | 324 | 60% |
| Brown 51 | USA | Pre‐test–post‐test | Mailed self‐report questionnaire | Programme/clinical directors of substance use disorder treatment programmes | Stratified random sample of substance use disorder treatment programmes licensed by the New York State Office of Alcoholism and Substance Abuse Services | 285 | 81.9% |
| Connolly 24 | New Zealand | Cross‐sectional survey | Online self‐report questionnaire | Psychiatric nurses | Invitations for nurses working in in‐patient or community mental health services distributed via the newsletter for a government organization involved with work‐force development across the mental health sector | 104 | 17% |
| Cookson 53 | UK | Cross‐sectional survey | Self‐report questionnaire (administered on site) | Range of staff | Convenience sample from four community drug treatment services associated with the South London and Maudsley NHS Foundation Trust | 145 | 97% |
| Dickens 23; Stubbs 52 | UK | Cross‐sectional survey | Mailed questionnaires | Range of staff | A single large, charitable status, psychiatric hospital in Northampton, UK | 599 | 40.7% |
| Dwyer 54 | Australia | Cross‐sectional survey | Mailed self‐report questionnaire | Psychiatric nurses | Random sample of endorsed mental health nurses selected from the Queensland Nursing Council register | 289 | 28.9% |
| Fuller 55 | USA | Cross‐sectional survey | Self‐report questionnaire (method of administration not reported) | Range of staff | Drug abuse treatment programmes participating in the National Drug Abuse Treatment Clinical Trials Network | 3786 | 71% |
| Gifford 41 | USA | Qualitative | Semi‐structured interviews | Range of staff | 15 residential substance abuse treatment programmes | 25 | N/A |
| Glover 36 | New Zealand | Qualitative | Semi‐structured interviews (face‐to‐face or telephone) | Range of staff | Invited ‘key informants’ including managers and workers in mental health and drug and alcohol services and smoke‐free coordinators and cessation providers within district health boards | 61 | 42% |
| Guo 56 | Taiwan | Cross‐sectional survey | Self‐report questionnaire (method of administration not reported) | Nurses | Two community psychiatric hospitals providing in‐patient and out‐patient care | 199 | 79.6% |
| Guydish 57 | USA | Pre‐test–post‐test | Self‐report questionnaire (administered on site) | Range of staff | All state‐certified addiction treatment programmes in New York State excluding prevention, education, short‐term, hospital‐based, criminal justice and adolescent programmes invited to participate | 235 | 92% |
| Himelhoch 58 | USA | Cross‐sectional survey | Self‐report questionnaire (administered on site) | Primarily psychiatrists and master's level therapists | Nine government‐funded community mental health services in Maryland, USA (only clinicians present on day of recruitment invited) | 95 | 100% |
| Hunt 38 | USA | Cross‐sectional survey | Questionnaire administered via phone, fax, mail or e‐mail | Clinic directors, medical directors, counselling supervisors, head nurses and clinic owners | Representative sample of out‐patients substance abuse treatment facilities selected from the Substance Abuse and Mental Health Services Inventory of Substance Abuse Treatment Services (one person in a leadership position from each clinic) | 405 | Not reported |
| Johnson 59 | Canada | Cross‐sectional survey | Self‐report questionnaire (administered on site) | Range of staff | 8 mental health teams within Vancouver Community Mental Health Services and 14 contracted community agencies | 282 | 32–38% |
| Keizer 60 | Switzerland | Cross‐sectional survey | Self‐report questionnaire (method of administration not reported) | Range of staff | Single public psychiatric hospital in Geneva, Switzerland | 155 | 72.4% |
| Knudsen 61; Knudsen 62 | USA | Longitudinal survey | Self‐report questionnaire administered via phone | Service administrators | Publicly and privately funded substance abuse treatment programmes, and therapeutic communities, identified through prior participation in the National Treatment Centre Study | 897 | 85.2% |
| Knudsen 63; Knudsen 64 | USA | Cross‐sectional survey | Mailed self‐report questionnaire | Counsellors | Publicly and privately funded substance abuse treatment programmes, and therapeutic communities, identified through prior participation in the National Treatment Centre Study | 2127 | 55.5% |
| Lawn 35 | Australia | Qualitative | Participant observation (ethnography) and open‐ended interviews | Range of staff | Two psychiatric hospitals in Queensland and South Australia | Not reported | NA |
| Leffingwell 65 | USA | Cross‐sectional survey | Mailed self‐report questionnaire | Clinical psychologists | Clinical psychologists identified through a public listing of all licensed psychologists in Oklahoma, USA | 167 | 34.7% |
| McCool 66 | USA | Cross‐sectional survey | Self‐report questionnaire administered via phone, fax or mail | Programme leaders (clinic directors, medical directors, supervising counsellors and head nurses) | All out‐patient methadone clinics in the USA (identified from lists of US methadone providers from the Food and Drug Administration and the Center for Substance Abuse Treatment). One programme leader per clinic invited to participate. | 408 | 58.4% |
| McNally 14 | UK | Cross‐sectional survey | Mailed self‐report questionnaire | Range of staff | Three NHS Trusts in London, Staffordshire and Ipswich, UK | 837 | 46% |
| Miller‐Thomas 67 | USA | Cross‐sectional survey | Mailed self‐report questionnaire | Range of staff | 12 substance abuse treatment programmes: range of perinatal, Veteran's Affairs, hospital‐based and community‐based | 376 | 85.3% |
| Morris 40 | USA | Qualitative | Focus groups | Range of staff | Representative sample of urban and rural regions in the public mental health system in Colorado, USA | 19 | NA |
| Praveen 68 | UK | Cross‐sectional survey | Self‐report questionnaire (administered on site) | Range of staff | In‐patient mental health units in Birmingham, Buckinghamshire and central London, UK | 308 | 68.4% |
| Price 19 | USA | Cross‐sectional survey | Mailed self‐report questionnaire | Psychiatrists | Invitations to all community mental health centres with Ohio Department of Mental Health certification | 80 | 53% |
| Ratschen 16 | UK | Cross‐sectional survey | Mailed self‐report questionnaire | Range of staff | All in‐patient mental health units within a single NHS Trust | 459 | 68% |
| Ratschen 43 | UK | Qualitative | Semi‐structured interviews | Range of mental health professionals | Two acute adult mental health wards in a single mental health trust | 16 | NA |
| Richter 42 | USA | Qualitative | Semi‐structured interviews | Range of staff | Eight drug treatment facilities in a metropolitan area of the Midwestern United States | 33 | NA |
| Robson 69 | UK | Cross‐sectional survey | Mailed self‐report questionnaire | Psychiatric nurses | Convenience sample from workforce of a single, large NHS Mental Health Trust | 585 | 52% |
| Sharp 70 | USA | Cross‐sectional survey | Electronic self‐report questionnaire | Psychiatric nurses | Sample of nurses selected from members of the American Psychiatric Nurses' Association | 1365 | 31.6% |
| Sidani 71 | USA | Cross‐sectional survey | Mailed self‐report questionnaire | Counsellors | Nationally representative random sample of clinical mental health counsellors identified through membership with the American Mental Health Counsellors Association | 330 | 53.1% |
| Steiner 72 | USA | Cross‐sectional survey | Mailed self‐report questionnaire | Range of staff | Single mental health centre in Connecticut, USA, providing in‐patient and out‐patient services | 175 | 87% |
| Walsh 17 | Australia | Cross‐sectional survey | Mailed self‐report questionnaire | Range of staff | Alcohol and drug treatment agencies identified from the Australian Directory of Alcohol and Other Drug Services and from directories of treatment agencies in all states and territories of Australia. One unit manager and one other staff member per unit invited to participate | 417 | 51.6% |
| Weinberger 73 | USA | Cross‐sectional survey | Self‐report questionnaire (method of administration not reported) | Range of staff | Single mental health centre in Connecticut, USA | 34 | 53% |
| Williams 37 | USA | Pre‐test–post‐test | Self‐report questionnaire (administered on site) | Range of staff | Attendees at a training course focused on training mental health treatment providers to address tobacco dependence | 71 | NA |
| Wye 74 | Australia | Cross‐sectional survey | Mailed self‐report questionnaire | Nurse managers | All publicly funded psychiatric in‐patient units in New South Wales, Australia. One nurse manager per unit invited to participate | 123 | 94% |
Quality appraisal
All studies included stated clear research questions or objective, and in all but one study (which did not provide the requisite information in the published report 36), data were judged to be sufficient to address the stated research questions or objectives (however, this study provided relevant for the current review and was therefore included here).
Quantitative studies (including the quantitative aspect of the mixed‐methods study)
Twenty‐two quantitative studies were judged to have used an adequate random (stratified or non‐stratified) sampling strategy. The remainder used convenience or unclear sampling. For most studies (n = 30) the sample representativeness could not be determined, either because the inclusion/exclusion criteria were unclear or because reasons for non‐response or differences between responders and non‐responders were unknown. Two studies were judged to have unrepresentative samples: in one study the sample was attendees at a smoking cessation training programme 3, and in the other the authors stated that their sample was not representative 38. The majority of studies (n = 28) used established measures which were clearly reflective of the variable of interest. For the remainder, the source and/or wording of measures was unclear. Fewer than half (n = 15) of the studies had a response rate of ≥ 60%.
Qualitative studies (including the qualitative aspect of the mixed‐methods study)
All qualitative studies used data sources (i.e. participants/recruitment settings) that were relevant to the research question, and used relevant approaches to data collection and analysis. Four of the seven qualitative studies discussed their findings in consideration of the research context, but only one explicitly considered the researchers' influence on their findings.
Synthesis of quantitative findings
Fourteen categories of attitudes were measured in at least five of the studies included and were therefore considered to be reliable and replicable. These categories were organized into three higher‐level groups: ‘perceived barriers to providing support’ (three categories), ‘negative attitudes towards smoking cessation’ (seven categories) and ‘permissive attitudes towards smoking’ (four categories).
The most frequently measured categories were ‘lack of knowledge/training/skills in providing smoking cessation treatment’, ‘quitting smoking might have a negative impact on symptoms/recovery’, ‘smoking cessation is not a priority’, ‘patients are not interested in quitting’ and ‘lack of time to provide smoking cessation treatment’ (see Table 2 for all categories and example measures). For some categories, suitable data could not be extracted from at least two studies, and therefore these categories were not included in the quantitative analysis.
Table 2.
Categories of attitudes/beliefs measured in five or more included studies.
| Category | Example measures | No. of studies measuring category |
|---|---|---|
| Perceived barriers to the provision of smoking cessation support | ||
| Lack of knowledge/training/skills is a barrier to providing treatment | ‘Mental health nurses do not have the appropriate skills to help a smoker with mental illness stop smoking’ | 16b |
| Lack of time is a barrier to providing smoking cessation treatment | ‘I don't have enough time as a healthcare provider to deal with tobacco use’ | 12b |
| Low confidence in ability to address patients' smoking | ‘How confident are you in your ability to counsel smokers who are interested in quitting smoking?’ | 12b |
| Negative attitudes towards smoking cessation | ||
|---|---|---|
| Quitting smoking might have a negative impact on symptoms/recovery | ‘Quitting smoking would make other mental health symptoms worse’ | 15 |
| Smoking cessation treatment is not a priority | ‘Smoking and tobacco use are not important issues in the successful treatment of other substance abuse problems’ | 14 |
| Patients are not interested in quitting | ‘Most patients who smoke aren't interested in giving up smoking’ | 13b |
| Smoking cessation treatment is not part of own role | ‘Do you believe it is part of your role to help clients to become smoke‐free?’ | 11b |
| Providing smoking cessation treatment is not part of the role of drug treatment/mental health services | ‘How involved should mental health services be in helping people with a mental illness to quit smoking or reduce their consumption?’ | 10b |
| Patients who smoke should not be encouraged/given assistance to quit | ‘Do you think that patients who smoke should be encouraged/helped to stop or cut back?’ | 6a, b |
| Smoking cessation intervention is not effective | ‘Pessimism about the effectiveness of stop smoking interventions is a barrier’ | 5b |
| Permissive attitudes towards smoking b | ||
|---|---|---|
| Smoking is an important coping mechanism | ‘Smoking helps clients cope with the stress in their lives’ | 6a, b |
| Smoking with patients helps to establish a therapeutic relationship | ‘Sometimes it is useful for staff to smoke with a patient to build rapport/trust’ | 5b |
| Quitting smoking is too much for patients to take on alongside their other issues | ‘Clients should not be encouraged to give up smoking, as they have enough to cope with’ | 5b |
| Smoking is a personal choice | ‘Clients can decide for themselves about quitting’ | 5a, b |
Not included in meta‐analysis as data could not be extracted from ≥ 2 studies.
Not included in meta‐regression as data could not be extracted from ≥10 studies.
Because there was significant heterogeneity across measures within all categories (all I 2 ≥ 94.7, all Ps < 0.001), data were pooled using a random‐effects meta‐analysis (see Table 3).
Table 3.
Pooled proportions within included categories of beliefs/attitudes.
| Category | Studies included in analysis | Pooled proportion (95% CI) | Range | Pooled frequencies | I2 (%) |
|---|---|---|---|---|---|
| Perceived barriers | 17, 19, 49, 51, 53, 58, 61, 62, 63, 64, 70, 71 | 42.2 (35.7–48.8) | 16.2–61.9% | 2588/5870 | 95.5 |
| Lack of knowledge/training/skills | 17, 19, 49, 63, 64, 70, 71, 73 | 35.8 (24.3–48.2) | 17.1–61.9% | 1902/5382 | 98.6 |
| Lack of time | 17, 19, 51, 58, 61, 62, 63, 64, 71 | 35.1 (24.4–46.7) | 5.1–56.0% | 1442/4129 | 97.8 |
| Low confidence | 17, 19, 49, 53, 70, 71 | 31.0 (20.1–43.1) | 16.2–49.7% | 1016/2530 | 97.1 |
| Negative attitudes | 17, 19, 24, 37, 38, 49, 39, 51, 53, 55, 58, 60, 61, 62, 63, 64, 65, 66, 70, 71, 74 | 40.5 (30.4–51.0) | 13.5–76.6% | 4027/11 184 | 99.1 |
|---|---|---|---|---|---|
| Patients are not interested | 17, 19, 49, 58, 70, 71, 74 | 51.4 (33.4–69.2) | 19.9–76.6% | 1490/2556 | 98.6 |
| Intervention is not effective | 17, 19, 37, 49, 71 | 27.6 (13.8–44.2) | 2.5–55.1% | 444/1217 | 97.1 |
| Not a priority | 19, 38, 49, 39, 53, 60, 61, 62, 63, 64, 70, 74 | 26.5 (19.5–34.2) | 2.5–59.9% | 1938/5876 | 97.2 |
| Negative impact on symptoms/recovery | 17, 19, 37, 38, 49, 51, 58, 61, 62, 63, 64, 71 | 24.4 (14.8–35.4) | 5.0–70.5% | 1110/4799 | 98.4 |
| Not part of own role | 24, 37, 51, 65, 71 | 18.0 (1.8–45.7) | 2.1–72.5% | 182/936 | 98.8 |
| Not part of the role of services | 38, 39, 55, 60, 66, 74 | 17.4 (11.6–24.0) | 8.4–44.7% | 868/4988 | 94.7 |
Perceived barriers
Around four of 10 participants reported perceived barriers to offering smoking cessation intervention, with lack of knowledge or training being the most prevalent perceived barrier, followed by lack of time and low confidence.
Negative attitudes to cessation
A similar proportion reported negative attitudes related to smoking cessation. The most commonly held beliefs were that patients are not interested in quitting smoking and that smoking cessation interventions are not effective. The least prevalent beliefs were that delivering smoking cessation intervention is not part of MHPs' role or that of mental health/drug and alcohol services.
Permissive attitudes to smoking
Nearly half of MHPs held permissive attitudes towards patients' smoking, with more than a third reporting the belief that quitting smoking is too much for patients to take on and that smoking with patients helps to establish a therapeutic relationship or build rapport.
Meta‐regression
Meta‐regression was conducted on only a subsection of outcomes (see Table 2) and revealed no significant associations of study characteristics with proportions for higher‐level groupings. However, in the analysis of individual categories there was a significant association between study country and the proportion of respondents who endorsed the view that quitting smoking might have a negative impact on symptoms and recovery. Controlling for other study‐level covariates, MHPs in studies from the United States were less likely than those from other countries to be worried about the negative impact of smoking cessation on mental health, with an absolute difference in proportions of 30.3% [95% confidence interval (CI) = 3.1–69.6, P < 0.05].
Synthesis of qualitative findings
Seven studies were included in the qualitative synthesis. The thematic synthesis yielded five main/recurring themes: (1) beliefs about patients quitting smoking; (2) barriers to the provision of smoking cessation treatment; (3) attitudes to the provision of smoking cessation treatment; (4) acceptance of patients' smoking; and (5) smoking as a useful tool. Table 4 shows the subthemes identified within each of these alongside illustrative quotes.
Table 4.
Themes and subthemes identified in qualitative synthesis.
| Theme | Subtheme | Study references | Illustrative quotes |
|---|---|---|---|
| Beliefs about patients quitting smoking | Negative perceptions of patients' motivation/ability to quit | 35, 37, 32, 31, 36, 39, 38 | ‘Some directors and staff members 9 and only 1 client cited that clients do not want to quit… ‘But the reality is most of our adult smokers could care less. I mean they're not interested in quitting smoking’ 38 |
| ‘Providers and consumers both voiced negative expectations regarding the ability of persons with mental illnesses to quit smoking, but providers made these comments more frequently’ 36 | |||
| Concerns about the negative consequences of quitting | 37, 32 | ‘Some wondered whether attempting to provide SC treatment in SRTPs could jeopardize patients' sobriety’ 37 | |
| ‘Helping service users to quit smoking was ‘too hard’…, and there was a fear of patients becoming violent’ 32 | |||
| Barriers to the provision of smoking cessation treatment | Lack of opportunity to provide treatment | 35, 37, 32, 36, 39, 38 | ‘Providers cited a lack of clinical resources such as smoking cessation groups and financial resources [both patient and system] to pay for the treatment’ 36 |
| ‘Time restraints mean other issues increase in priorities’ 35 | |||
| Lack of capability to provide treatment | 32, 36, 39, 37 | ‘The participants' skills and knowledge relating to smoking and nicotine dependence treatment seemed lacking’ 39 | |
| ‘One respondent suggested that there was a ‘total lack of knowledge’ about the importance of, or the need for, service users to stop smoking’ 32 | |||
| Health professionals' behaviour | 37, 32, 31, 36, 38 | ‘In the locked settings, clients and staff spent much time in direct contact, often in the smoking area with the majority of clients and staff smoking, with staff acting as social role models for clients at such times’ 31 | |
| ‘Far from encouraging cessation, some staff enabled smoking by “offering cigarettes” with ‘nurses who purchase cigarettes [for the service users], even out of their own money at times’ 32 | |||
| Attitudes to the provision of smoking cessation treatment | It is important | 35, 37, 32, 36, 39, 38 | ‘Providers identified tobacco cessation for persons with mental illnesses as a promising or emerging evidence‐based practice and strongly supported integrating tobacco cessation services in mental health settings as a clinical priority’ 36 |
| It is not a priority | 35, 37, 32, 36, 39, 38 | ‘Another difference reported [between smoking and other drug use] was that smoking was not a focus or a high priority in drug treatment’ 38 | |
| ‘An ‘unwillingness to place nicotine addiction high enough to warrant the same attention as other addictions’ led to a ‘low need to quit’ 32 | |||
| It is not part of own role | 35, 37, 32, 38 | ‘Several participants said that SC counseling was not in their job description and was outside their scope of work’ 37 | |
| ‘The capacity to provide cessation support was perceived to be limited by exclusion of the requirement to possess the skill or deliver support in employee job descriptions’ 32 | |||
| Negative beliefs about providing treatment | 37, 32, 36, 38 | ‘Participants stated concerns that “trying to force patients to quit” might make them leave the programme’ 37 | |
| ‘As one provider put it, “the problem is that there isn't actually evidence that it [cessation strategies] works”’ 36 | |||
| It is dependent upon the patient | 35, 37, 39, 38 | ‘Most participants expressed discomfort with advising uninterested patients to quit, indicating interventions were typically presented to only patients who explicitly asked for help. One participant described the process as, “If they say they don't want to stop smoking, they get told about the dangers and that's it”’ 37 | |
| Acceptance of patients' smoking | Culture of smoking | 37, 32, 31 | ‘A number of staff beliefs and practices supported a “culture of smoking”, with “smoking as the norm”’ 32 |
| It is a patients' right/personal choice | 35, 37, 32 | ‘I believe people should have a choice if they smoke or not’ 39 | |
| Smoking is a ‘core need’ | 31, 36, 39 | ‘Several providers commented that “they [mental health consumers] don't care how much they spend on cigarettes. Their cigarettes are so important to them, it doesn't matter”’ 36 | |
| ‘Clients and staff focused much attention on ensuring the supply of cigarettes as a core need for clients’ 31 | |||
| Smoking as a useful tool | For patients | 32, 31, 36, 39, 38 | ‘Respondents generally viewed smoking as an important coping mechanism for patients—providing a way to deal with stress’ 39 |
| ‘In the locked ward I don't think there's much in the way of one‐to‐one therapeutic activity that happens. It's a kind of, “Let's wait for the medication to work”. There's just nothing to do. The only normal thing to do at the time is to smoke’ 31 | |||
| For staff | 37, 32, 31, 36 | ‘Some respondents believed that smoking enabled positive social experiences, which helped staff develop rapport with service users’ 32 | |
| ‘Moreover, in some settings, such as psychiatric hospitals, consumers earned smoking privileges as a behavioural reward’ 36 |
Beliefs about patients quitting smoking
The most apparent subtheme within this theme was negative perceptions of patients' ability and motivation to quit, which was identified in all studies. This perception appeared to arise from beliefs that patients would not be interested in quitting smoking 39, 40, 41, 42, that patients would be unable to quit smoking successfully 35, 36, 40 and the view that smoking cessation would be too much for patients to cope with alongside their other issues 36, 39, 41, 42, 43. A minority of studies reported concerns about the negative consequences of quitting smoking, such as concerns about a negative impact on psychiatric symptoms/abstinence 36, 41, the potential effects on medication 36 and a fear that smoking cessation may make patients violent 36.
Barriers to the provision of smoking cessation treatment
A perceived lack of opportunity to provide smoking cessation support was evident 36, 39, 40, 41, 42, 43. This generally arose from a perceived lack of treatment resources either on‐site or to refer patients to off‐site 36, 40, 41, 42 and a lack of guidance for implementing smoking cessation treatment alongside treatment for patients' primary disorders 36, 41, 42, 43. In addition, a lack of staff 36, 41, staff time 36, 39, funding 36, 40 and support from management 36, 41 were identified as further barriers to providing smoking cessation treatment.
In a number of studies, staff did not appear to feel that they had the capability to treat nicotine dependence effectively 36, 40, 41, 43. This arose both from a lack of knowledge about nicotine dependence and pharmacological treatments 36, 40, 41, 43 and from a perceived need for specialized training in the provision of smoking cessation support to people with mental illnesses and/or drug and alcohol disorders 40, 41, 43.
The behaviour of MHPs was identified commonly as a barrier to addressing smoking among patients 35, 40, 41, 42. This tended to relate to professionals' smoking status, as staff smoking was viewed as providing a bad example to patients 35, 36, 40, 41, 42 and could potentially undermine motivation to address patients' smoking (e.g. because it would be hypocritical) 41. In addition, professionals' role in facilitating patients' smoking (i.e. by providing lights and/or cigarettes) was a further potential barrier to providing smoking cessation treatment 35, 36.
Attitudes to the provision of smoking cessation treatment
Smoking cessation generally was viewed to be important for patients 36, 39, 40, 41, 42, 43, primarily because of the potential to improve patients' health 39, 41, 42, 43 and reduce their financial burden 39, 42. Two studies reported that staff felt smoking cessation treatment should be integrated into patients' care 39, 43. Despite this positive attitude to the provision of smoking cessation treatment, results from the majority of studies indicated that the provision of smoking cessation treatment was not viewed as a priority in the context of treatment for patients' primary disorders [36,39–43.] For instance, some staff thought that treating tobacco dependence was less important than treating addictions to alcohol or illicit drugs, as cigarettes are not illegal or as harmful to health 36, 42. In some cases, the provision of smoking cessation treatment was seen to be dependent upon the patient; for instance, if they showed an interest in quitting 39, 41, 42, 43 or displayed any negative health effects of smoking 39.
The provision of smoking cessation treatment was often not seen as part of MHPs' role 36, 39, 41, 42, and in many cases staff held negative beliefs about smoking cessation treatment 36, 40, 41, 42. For instance, some reported the belief that smoking cessation treatment is not effective 40, 41, while others had concerns that encouraging smoking cessation might drive patients away 36, 41.
Acceptance of smoking
Overall, a general acceptance of patients' smoking by MHPs could be noted. This seemed to stem from the view that there was a long‐standing ‘culture of smoking’ in in‐patient mental health and drug and alcohol services 35, 36, 41, alongside the belief that it is a patient's right/personal choice to smoke 36, 39, 41. Further, some staff felt that smoking was a ‘core need’ for their patients—something essential that they could not be without 35, 40, 43.
Smoking as a useful tool
Across studies, MHPs viewed cigarettes and smoking as useful tools in managing patients 35, 36, 40, 41, 42, 43. Patients were seen to use smoking as a form of self‐medication (e.g. to cope with abstinence from other addictive drugs or with psychiatric symptoms) or stress‐relief 35, 36, 40, 42, 43, to relieve boredom 35, 40 and facilitate socializing 40. Smoking was also viewed as a useful tool to be used by staff, either through smoking with patients to build rapport 35, 36, 40, 41, by using cigarettes as a behavioural incentive/reward 35, 36, 40 or using cigarettes to keep patients calm and minimize aggression 35.
Discussion
We identified 38 relevant studies investigating MHPs' attitudes towards smoking and smoking cessation among people with mental illnesses and substance abuse disorders, most of which were quantitative rather than qualitative. A significant proportion of MHPs held negative attitudes towards smoking cessation and permissive attitudes towards smoking, and perceived a number of barriers to providing smoking cessation treatment. Meta‐regression analyses revealed no associations between attitudes and year of publication or type of service, but showed that MHPs in US‐based studies were less likely to hold concerns about the negative impact of smoking cessation on symptoms and recovery. The thematic synthesis of qualitative studies was consistent with the quantitative results, and in addition revealed a richer insight into MHPs' views on patients' smoking, particularly in the context of in‐patient services. Cigarettes were viewed as a useful tool for both patients and staff, and the smoking behaviour of staff was identified as a barrier to providing effective smoking cessation support. A general acceptance of patients' smoking was also apparent in the qualitative findings, with a culture of smoking being seen as the ‘norm’ in some services.
This synthesis of the existing literature examining MHPs' attitudes towards smoking and smoking cessation among patients reveals that a significant minority hold attitudes and beliefs that may prevent them from delivering smoking cessation support. The relationship between attitudes/beliefs, intentions and behaviour is well established (e.g. 44, 45), and health professionals are no exception 46. This review highlights the potential for such attitudes to present a barrier to integrate smoking cessation interventions effectively into treatment for mental illnesses and substance use disorders. In addition, this review identified a number of target misconceptions that are inconsistent with the scientific literature. For instance, the belief that patients are not interested in quitting is contradicted by evidence that people with mental illnesses are just as likely to want to quit as those without 22. Similarly, concerns about the negative impact of quitting on patients' symptoms or recovery are not supported by research 20, 21.
It is encouraging that the current review identified that most MHPs felt that it was part of their role to address patients' smoking, even though a minority of approximately one‐fifth felt that it was not part of their role. Further, the qualitative findings indicated that most felt that smoking cessation was important, suggesting that MHPs view the provision of smoking cessation treatment positively. However, despite this generally positive attitude towards providing support, MHPs' reported beliefs about patients' ability and/or motivation to quit, and perceptions of their own ability to successfully deliver interventions and intervention effectiveness which may prevent them from providing support. Most notably, more than half of MHPs in this review reported that patients are not interested in quitting smoking and almost 40% felt that quitting smoking was too much for patients to take on, suggesting that one of the main barriers to the delivery of smoking cessation support may be implicit beliefs about patients, and a tendency to shift responsibility for smoking cessation to patients alone. In agreement with previous work 18, these findings highlight a need for greater prioritization of smoking cessation treatment in mental health and substance abuse care, a need for specialist training in smoking cessation interventions and broader education to challenge misconceptions about smoking cessation in the context of mental health and drug and alcohol treatment. One notable policy change recently instigated in the United Kingdom that may prove effective is the introduction of smoke‐free policies 47; other levers which could be pursued to address existing barriers include mandatory smoking cessation training for MHPs and, in the context of private health‐care systems, governmental subsidies for cost‐effective smoking cessation pharmacotherapy. In fact, National Institute for Health and Care Excellence (NICE) guidance on smoke‐free policy indicates that this policy should only be introduced alongside training and systematic identification of smokers and treatment, as introducing such policies by themselves is unlikely to change attitudes 11. In addition, the inclusion of effective smoking cessation medications on the hospitals' formulary will ensure that smokers with and without mental illness have equal access to pharmacotherapy to treat tobacco addiction.
It is unclear why MHPs in the United States were less likely to be concerned about the negative impact of smoking cessation than those from other countries. This may reflect differences in the training provided to MHPs in different countries. However, clinical practice guidelines on smoking cessation from the United States, Australia and the United Kingdom (the two countries that formed the majority of studies not conducted in the United States) do not provide a clear explanation for this divide. While guideline recommendations in the United Kingdom do not cover the topic of smoking cessation, psychiatric symptoms and addiction recovery explicitly, they clearly encourage smoking cessation in this setting 11, and both US 48 and Australian 3 guidelines state that smoking cessation is unlikely to have any adverse effects. The lack of evidence of any recent changes in attitudes to support cessation is also of concern in light of accumulating evidence of the positive impact of cessation on mental health 20, 21, 22, and may indicate a need to disseminate this information to MHPs more effectively.
The main strength of this review is that is provides an up‐to‐date overview of the most prevalent beliefs and attitudes that may present a barrier to the delivery of smoking cessation intervention in mental health and drug and alcohol services. This review also has some limitations. Data for pooled proportions were not available from all studies, and there was significant heterogeneity among studies. However, quantitative results were largely confirmed by the qualitative synthesis, increasing confidence in these findings. The study selection might be biased due to the focus on English language and full‐text publications; however, every effort was made to make the search strategy as inclusive as possible. None the less, relatively little qualitative work was identified, and further studies should explore potential solutions to overcome common barriers and enable the effective integration of stop smoking service provision into mental health care.
In summary, a significant proportion of MHPs appear to hold negative attitudes towards offering smoking cessation advice and support to patients with mental illness and substance use disorders. These present a potential barrier to the successful implementation of smoking cessation interventions in mental health/substance abuse services, and highlight the continued need for dedicated education and training amongst this group of health professionals.
Declaration of interests
L.S. has received a research grant and honoraria for a talk and travel expenses from a Pfizer, manufacturer of smoking cessation medications.
Supporting information
Table S1. Full search strategy and records identified.
Supporting info item
Acknowledgements
We are grateful to Cancer Research UK and the British Heart Foundation for funding the study (Lynn MacFadyen PhD Studentship in Tobacco Control; C27061/A18679). Many thanks also to Radhika Pal, who assisted in the screening and data extraction stages of the review. All authors are part of the UK Centre for Tobacco and Alcohol Studies, a UK Clinical Research Collaboration Public Health Research: Centre of Excellence. Funding from the Medical Research Council, British Heart Foundation, Cancer Research UK, Economic and Social Research Council and the National Institute for Health Research under the auspices of the UK Clinical Research Collaboration is gratefully acknowledged (MR/K023195/1). The funders played no role in the study design, collection, analysis and interpretation of the data, in the writing of the manuscript and in the decision to submit this manuscript for publication.
Sheals, K. , Tombor, I. , McNeill, A. , and Shahab, L. (2016) A mixed‐method systematic review and meta‐analysis of mental health professionals' attitudes toward smoking and smoking cessation among people with mental illnesses. Addiction, 111: 1536–1553. doi: 10.1111/add.13387.
References
- 1. Lasser K., Boyd J. W., Woolhandler S., Himmelstein D. U., McCormick D., Bor D. H. Smoking and mental illness: a population‐based prevalence study. JAMA 2000; 284: 2606–10. [DOI] [PubMed] [Google Scholar]
- 2. Kelly C., McCreadie R. Cigarette smoking and schizophrenia. Adv Psychiatr Treat 2000; 6: 327–31. [Google Scholar]
- 3. Royal Australian College of General Practitioners Supporting Smoking Cessation: A Guide For Health Professionals. Melbourne: Royal Australian College of General Practitioners; 2011. [Google Scholar]
- 4. Kelly P. J., Baker A. L., Deane F. P., Kay‐Lambkin F. J., Bonevski B., Tregarthen J. Prevalence of smoking and other health risk factors in people attending residential substance abuse treatment. Drug Alcohol Rev 2012; 31: 638–44. [DOI] [PubMed] [Google Scholar]
- 5. Grant B. F., Hasin D. S., Chou S. P., Stinson F. S., Dawson D. A. Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry 2004; 61: 1107–15. [DOI] [PubMed] [Google Scholar]
- 6. Coulthard M., Farrell M., Singleton N., Meltzer H. Tobacco, Alcohol and Drug Use and Mental Health. London: Office for National Statistics; 2002. [Google Scholar]
- 7. Royal College of Physicians, Royal College of Psychiatrists Smoking and Mental Health: A Joint Report by the Royal College of Physicians and the Royal College of Psychiatrists. London: Royal College of Physicians; 2013. [Google Scholar]
- 8. Chang C. K., Hayes R. D., Perera G., Broadbent M. T. M., Fernandes A. C., Lee W. E., et al. Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS One 2011; 6: e19590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chesney E., Goodwin G. M., Fazel S. Risks of all‐cause and suicide mortality in mental disorders: a meta‐review. World Psychiatry 2014; 13: 153–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ziedonis D., Hitsman B., Beckham J., Zvolensky M., Adler L., Audrain‐McGovern J., et al. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine Tob Res 2008; 10: 1691–715. [DOI] [PubMed] [Google Scholar]
- 11. National Institute for Health and Care Excellence Smoking Cessation in Secondary Care: Acute, Maternity and Mental Health Services. London: National Institute for Health and Care Excellence; 2013. [Google Scholar]
- 12. Prochaska J. J., Reyes R. S., Schroeder S. A., Daniels A. S., Doederlein A., Bergeson B. An online survey of tobacco use, intentions to quit, and cessation strategies among people living with bipolar disorder. Bipolar Disord 2011; 13: 466–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Szatkowski L., McNeill A. The delivery of smoking cessation interventions to primary care patients with mental health problems. Addiction 2013; 108: 1487–94. [DOI] [PubMed] [Google Scholar]
- 14. McNally L., Oyefoso A., Annan J., Perryman K., Bloor R., Freedman S., et al. A survey of staff attitudes to smoking‐related policy and intervention in psychiatric and general health care settings. J Public Health 2006; 28: 192–6. [DOI] [PubMed] [Google Scholar]
- 15. Johnson J., Moffatt B., Malchy L. In the shadow of a new smoke free policy: a discourse analysis of health care providers' engagement in tobacco control in community mental health. Int J Ment Health Syst 2010; 4: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ratschen E., Britton J., Doody G., Leonardi‐Bee J., McNeill A. Tobacco dependence, treatment and smoke‐free policies: a survey of mental health professionals' knowledge and attitudes. Gen Hosp Psychiatry 2009; 31: 576–82. [DOI] [PubMed] [Google Scholar]
- 17. Walsh R. A., Bowman J. A., Tzelepis F., Lecathelinais C. Smoking cessation interventions in Australian drug treatment agencies: a national survey of attitudes and practices. Drug Alcohol Rev 2005; 24: 235–44. [DOI] [PubMed] [Google Scholar]
- 18. Leonardi‐Bee J., Jayes L., O'Mara‐Eves A., Stansfeld C., Gibson K., Ratschen E., et al. Barriers and Facilitators for Smoking cessation interventions in Mental Health (Evidence Report for NICE Guidelines [PH48]). London: National Institute for Health and Care Excellence; 2012. [Google Scholar]
- 19. Price J. H., Ambrosetti L. M., Sidani J. E., Price J. A. Psychiatrists' smoking cessation activities with Ohio community mental health center patients. Community Ment Health J 2007; 43: 251–66. [DOI] [PubMed] [Google Scholar]
- 20. Taylor G., McNeill A., Girling A., Farley A., Lindson‐Hawley N., Aveyard P. Change in mental health after smoking cessation: systematic review and meta‐analysis. BMJ 2014; 348: g1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shahab L., Gilchrist G., Hagger‐Johnson G., Shankar A., West E., West R. Reciprocal associations between smoking cessation and depression in older smokers: findings from the English Longitudinal Study of Ageing. Br J Psychiatry 2015; 207: 243–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Siru R., Hulse G. K., Tait R. J. Assessing motivation to quit smoking in people with mental illness: a review. Addiction 2009; 104: 719–33. [DOI] [PubMed] [Google Scholar]
- 23. Dickens G. L., Stubbs J. H., Haw C. M. Smoking and mental health nurses: a survey of clinical staff in a psychiatric hospital. J Psychiatr Ment Health Nurs 2004; 11: 445–51. [DOI] [PubMed] [Google Scholar]
- 24. Connolly M., Floyd S., Forrest R., Marshall B. Mental health nurses' beliefs about smoking by mental health facility inpatients. Int J Ment Health Nurs 2013; 22: 288–93. [DOI] [PubMed] [Google Scholar]
- 25. Moher D., Liberati A., Tetzlaff J., Altman D. G. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta‐Analyses: the PRISMA Statement. BMJ 2009; 339: b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. World Health Organization WHO Framework Convention on Tobacco Control. Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- 27. Pluye P., Gagnon M. P., Griffiths F., Johnson‐Lafleur J. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in mixed studies reviews. Int J Nurs Stud 2009; 46: 529–46. [DOI] [PubMed] [Google Scholar]
- 28. Pace R., Pluye P., Bartlett G., Macaulay A. C., Salsberg J., Jagosh J., et al. Testing the reliability and efficiency of the pilot mixed methods appraisal tool (MMAT) for systematic mixed studies review. Int J Nurs Stud 2012; 49: 47–53. [DOI] [PubMed] [Google Scholar]
- 29. Sirriyeh R., Lawton R., Gardner P., Armitage G. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract 2012; 18: 746–52. [DOI] [PubMed] [Google Scholar]
- 30. Higgins J. P. T., Green S. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5 [updated May 2005]. John Wiley & Sons, Ltd: Chichester, UK; 2005. [Google Scholar]
- 31. Nyaga V. N., Arlyn M., Aerts M. Metaprop: a Stata command to perform meta‐analysis of binomial data. Arch Public Health; 72: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Higgins J. P., Thompson S. G., Deeks J. J., Altman D. G. Measuring inconsistency in meta‐analyses. BMJ 2003; 327: 557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Borenstein M., Hedges L., Higgins J., Rothstein H. Introduction to Meta‐Analysis. Chichester, UK: Wiley; 2009. [Google Scholar]
- 34. Thomas J., Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008; 8: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lawn S. L. Systemic barriers to quitting smoking among institutionalised public mental health service populations: a comparison of two Australian sites. Int J Soc Psychiatry 2004; 50: 204–15. [DOI] [PubMed] [Google Scholar]
- 36. Glover M., Fraser T., Bullen C., Wallace‐Bell M., McRobbie H., Hadwen G. Transition to a smoke‐free culture within mental health and drug and alcohol services: a survey of key stakeholders. Int J Ment Health Nurs 2014; 23: 183–91. [DOI] [PubMed] [Google Scholar]
- 37. Williams J. M., Steinberg M. L., Zimmermann M. H., Gandhi K. K., Lucas G.‐E., Gonsalves D. A., et al. Training psychiatrists and advanced practice nurses to treat tobacco dependence. J Am Psychiatr Nurses Assoc 2009; 15: 50–8. [DOI] [PubMed] [Google Scholar]
- 38. Hunt J. J., Cupertino A., Gajewski B. J., Jiang Y., Ronzani T. M., Richter K. P. Staff commitment to providing tobacco dependence in drug treatment: reliability, validity, and results of a national survey. Psychol Addict Behav 2014; 28: 389–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ashton M., Lawn S., Hosking J. Mental health workers' views on addressing tobacco use. Aust NZ J Psychiatry 2010; 44: 846–51. [DOI] [PubMed] [Google Scholar]
- 40. Morris C. D., Waxmonsky J. A., May M. G., Giese A. A. What do persons with mental illnesses need to quit smoking? Mental health consumer and provider perspectives. Psychiatr Rehabil J 2009; 32: 276–84. [DOI] [PubMed] [Google Scholar]
- 41. Gifford E., Tavakoli S., Wisdom J., Hamlett‐Berry K. Implementation of smoking cessation treatment in VHA substance use disorder residential treatment programs. Psychiatr Serv 2015; 66: 295–302. [DOI] [PubMed] [Google Scholar]
- 42. Richter K. P., Hunt J. J., Cupertino A. P., Garrett S., Friedmann P. D. Understanding the drug treatment community's ambivalence towards tobacco use and treatment. Int J Drug Policy 2012; 23: 220–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ratschen E., Britton J., Doody G., McNeill A. Smoke‐free policy in acute mental health wards: avoiding the pitfalls. Gen Hosp Psychiatry 2009; 31: 131–6. [DOI] [PubMed] [Google Scholar]
- 44. Armitage C. J., Conner M. Efficacy of the theory of planned behaviour: a meta‐analytic review. Br J Soc Psychol 2001; 40: 471–99. [DOI] [PubMed] [Google Scholar]
- 45. Hagger M. S., Chatzisarantis N. L. D., Biddle S. J. H. A meta‐analytic review of the theories of reasoned action and planned behavior in physical activity: predictive validity and the contribution of additional variables. J Sport Exerc Psychol 2002; 24: 3–32. [Google Scholar]
- 46. Godin G., Belanger‐Gravel A., Eccles M., Grimshaw J. Healthcare professionals' intentions and behaviours: a systematic review of studies based on social cognitive theories. Implement Sci 2008; 3: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ratschen E., Britton J., McNeill A. Implementation of smoke‐free policies in mental health in‐patient settings in England. BrJ Psychiatry 2009; 194: 547–51. [DOI] [PubMed] [Google Scholar]
- 48. Fiore M. C., Jaen C. R., Baker T. B., Bailey W. C., Benowitz N. L., Curry S. J., et al. Treating Tobacco Use and Dependence: 2008 Update—Clinical Practice Guidelines. Rockville, MD: US Department of Health and Human Services, Public Health Service; 2008. [Google Scholar]
- 49. Akpanudo S. M., Price J. H., Jordan T., Khuder S., Price J. A. Clinical psychologists and smoking cessation: treatment practices and perceptions. J Community Health 2009; 34: 461–71. [DOI] [PubMed] [Google Scholar]
- 50. Amole J. J., Heath J., Joshua T. V., McLear B. Online tobacco cessation education to optimize standards of practice for psychiatric mental health nurses. Nurs Clin North Am 2012; 47: 71–9. [DOI] [PubMed] [Google Scholar]
- 51. Brown E., Nonnemaker J., Federman E. B., Farrelly M., Kipnis S. Implementation of a tobacco‐free regulation in substance use disorder treatment facilities. J Subst Abuse Treat 2012; 42: 319–27. [DOI] [PubMed] [Google Scholar]
- 52. Stubbs J., Haw C., Garner L. Survey of staff attitudes to smoking in a large psychiatric hospital. Psychol Bull 2004; 28: 204–7. [Google Scholar]
- 53. Cookson C., Strang J., Ratschen E., Sutherland G., Finch E., McNeill A. Smoking and its treatment in addiction services: clients' and staff behaviour and attitudes. BMC Health Serv Res 2014; 14: 304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Dwyer T., Bradshaw J., Happell B. Comparison of mental health nurses' attitudes towards smoking and smoking behavior. Int J Ment Health Nurs 2009; 18: 424–33. [DOI] [PubMed] [Google Scholar]
- 55. Fuller B. E., Guydish J., Tsoh J., Reid M. S., Resnick M., Zammarelli L., et al. Attitudes toward the integration of smoking cessation treatment into drug abuse clinics. J Subst Abuse Treat 2007; 32: 53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Guo S.‐E., Wang A.‐L., Shu B.‐C. Self‐efficacy in providing smoking‐cessation services among psychiatric nurses in central and southern taiwan: an exploratory study. Int J Ment Health Nurs 2015. .no pagination specified [DOI] [PubMed] [Google Scholar]
- 57. Guydish J., Tajima B., Kulaga A., Zavala R., Brown L. S., Bostrom A., et al. The New York policy on smoking in addiction treatment: findings after 1 year. Am J Public Health 2012; 102: e17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Himelhoch S., Riddle J., Goldman H. H. Barriers to implementing evidence‐based smoking cessation practices in nine community mental health sites. Psychiatr Serv 2014; 65: 75–80. [DOI] [PubMed] [Google Scholar]
- 59. Johnson J., Malchy L., Ratner P., Hossain S., Procyshyn R., Bottorff J., et al. Community mental healthcare providers' attitudes and practices related to smoking cessation interventions for people living with severe mental illness. Patient Educ Couns 2009; 77: 289–95. [DOI] [PubMed] [Google Scholar]
- 60. Keizer I. Staff representations and tobacco‐related practices in a psychiatric hospital with an indoor smoking ban. Int J Ment Health Nurs 2014; 23: 171–82. [DOI] [PubMed] [Google Scholar]
- 61. Knudsen H. K., Studts J. L., Boyd S., Roman P. M. Structural and cultural barriers to the adoption of smoking cessation services in addiction treatment organizations. J Addict Dis 2010; 29: 294–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Knudsen H. K., Muilenburg J., Eby L. T. Sustainment of smoking cessation programs in substance use disorder treatment organizations. Nicotine Tob Res 2013; 15: 1060–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Knudsen H. K., Studts J. L. The implementation of tobacco‐related brief interventions in substance abuse treatment: a national study of counselors. J Subst Abuse Treat 2010; 38: 212–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Knudsen H. K., Studts C. R., Studts J. L. The implementation of smoking cessation counseling in substance abuse treatment. J Behav Health Serv Res 2012; 39: 28–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Leffingwell T. R., Babitzke A. C. Tobacco intervention practices of licensed psychologists. J Clin Psychol 2006; 62: 313–23. [DOI] [PubMed] [Google Scholar]
- 66. McCool R. M., Richter K. P., Choi W. S. Benefits of and barriers to providing smoking treatment in methadone clinics: findings from a national study. Am J Addict 2005; 14: 358–66. [DOI] [PubMed] [Google Scholar]
- 67. Miller‐Thomas T., Leoutsakos J. M. S., Terplan M., Brigham E. P., Chisolm M. S. Comparison of cigarette smoking knowledge. Attitudes, and practices among staff in perinatal and other substance abuse treatment settings. J Addict Med 2014; 8: 377–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Praveen K. T., Kudlur S. N. C., Hanabe R. P., Egbewunmi A. T. Staff attitudes to smoking and the smoking ban. Psychol Bull 2009; 33: 84–8. [Google Scholar]
- 69. Robson D., Haddad M., Gray R., Cournay K. Mental health nursing and physical health care: a cross‐sectional study of nurses' attitudes, practice, and perceived training needs for the physical health care of people with severe mental illness. Int J Ment Health Nurs 2013; 22: 409–17. [DOI] [PubMed] [Google Scholar]
- 70. Sharp D. L., Blaakman S. W., Cole R. E., Evinger J. S. Report from a national tobacco dependence survey of psychiatric nurses. J Am Psychiatr Nurses Assoc 2009; 15: 172–81. [DOI] [PubMed] [Google Scholar]
- 71. Sidani J. E., Price J. H., Dake J. A., Jordan T. R., Price J. A. Practices and perceptions of mental health counselors in addressing smoking cessation. J Ment Health Couns 2011; 33: 264–82. [Google Scholar]
- 72. Steiner J. L., Weinberger A. H., O'Malley S. S. A survey of staff attitudes about smoking cessation. Psychiatr Serv 2009; 60: 707–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Weinberger A. H., Reutenauer E. L., Vessicchio J. C., George T. P. Survey of clinician attitudes toward smoking cessation for psychiatric and substance abusing clients. J Addict Dis 2008; 27: 55–63. [DOI] [PubMed] [Google Scholar]
- 74. Wye P., Bowman J., Wiggers J., Baker A., Carr V., Terry M., et al. Providing nicotine dependence treatment to psychiatric inpatients: the views of Australian nurse managers. J Psychiatr Ment Health Nurs 2010; 17: 319–27. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Full search strategy and records identified.
Supporting info item


