Abstract
OBJECTIVE
We examined surveillance data to describe the epidemiology of tuberculosis (TB) among healthcare workers (HCWs) in the United States during the period 1995–2007.
DESIGN
Cross-sectional descriptive analysis of existing surveillance data.
SETTING AND PARTICIPANTS
TB cases reported to the Centers for Disease Control and Prevention from the 50 states and the District of Columbia from 1995 through 2007.
RESULTS
Of the 200,744 reported TB cases in persons 18 years of age or older, 6,049 (3%) occurred in individuals who were classified as HCWs. HCWs with TB were more likely than other adults with TB to be women (unadjusted odds ratio [95% confidence interval], 4.1 [3.8–4.3]), be foreign born (1.3 [1.3–1.4]), have extrapulmonary TB (1.6 [1.5–1.7]), and complete TB treatment (2.5 [2.3–2.8]).
CONCLUSIONS
Healthcare institutions may benefit from intensifying TB screening of HCWs upon hire, especially persons from countries with a high incidence of TB, and encouraging treatment for latent TB infection among HCWs to prevent progression to TB disease.
Since the early 1990s, outbreaks of tuberculosis (TB) and multidrug-resistant TB in various medical settings have demonstrated patient-to-healthcare worker (HCW) transmission of Mycobacterium tuberculosis,1-4 and other investigations have suggested that HCWs with untreated latent TB infection (LTBI) can later experience progression to TB disease, which can cause workplace exposure to patients and other HCWs.5,6 The extent of occupational risk of TB for HCWs varies according to many factors, including prevalence of TB in the patient population, immunocompetency of the HCW, and effectiveness of infection control measures in the healthcare setting.7
The objective of this analysis was to examine surveillance data and describe the epidemiology of TB among HCWs in the United States during the period 1995–2007. Additional goals were to compare demographic characteristics and treatment outcomes of reported TB cases among HCWs and other adults and to compare US-born and foreign-born HCWs.
METHODS
This study describes new analyses of existing data routinely submitted to the Centers for Disease Control and Prevention through the National Tuberculosis Surveillance System. These data are collected for the purposes of disease surveillance and not human subject research that requires ethical institutional board review. TB cases were reported by the 50 states and the District of Columbia. Data were collected on a standardized form that included demographic, laboratory, clinical, and treatment outcome information.
We calculated the proportion of TB cases reported during 1995–2007 that occurred in persons 18 years of age or older whose occupations were categorized as “healthcare worker.” Data for treatment outcomes were analyzed only through 2005 to provide a 2-year period to complete reporting. To calculate an annual TB incidence rate among HCWs, we used the US Census Bureau Current Population Survey’s estimate for the denominator of HCWs in the United States for 2003–2007.8 Estimated numbers of HCWs in the United States were not available before 2003.
Persons were considered to be foreign born if the reported country of birth was outside the United States or its jurisdictions in the Pacific and Caribbean. Method of TB treatment was recorded as (i) directly observed therapy (DOT), (ii) self-administered therapy, (iii) a combination of self-administered therapy and DOT, or (iv) unknown. DOT, an adherence-enhancing strategy in which a HCW or other trained person watches a patient swallow each dose of medication, is the standard care for all patients with TB disease and is a preferred option for patients treated for LTBI in the United States, when feasible.9-11 Persons were classified as having a previous diagnosis of TB if they had verified TB in the past, had completed TB therapy, or were lost to supervision for more than 12 months and had verified TB again. The proportion of human immunodeficiency virus (HIV)–infected persons was calculated as a percentage of the total number of persons with test results reported (ie, negative, positive, or indeterminate). The number of persons documented as having refused an HIV test was also reported; others were classified as HIV status unknown (ie, HIV test not offered or result not reported).
Unadjusted odds ratios (uORs) were used to compare characteristics of HCWs who had TB with those of other adults who had TB and to compare characteristics of US-born HCWs who had TB with characteristics of foreign-born HCWs who had TB. Data were analyzed with SAS for Windows, version 9.1 (SAS Institute), and Microsoft Excel 2003 (Microsoft).
RESULTS
During the period 1995–2007, of the 200,744 TB cases involving patients 18 years of age or older, 6,049 (3%) were classified as HCWs (mean of 429 HCWs with TB per year). Using the US Census Bureau population estimates for HCWs for 2003–2007 (ie, an annual average of 1.8 million male and 7.0 million female US-born HCWs and 400,000 male and 1.1 million female foreign-born HCWs),8 the estimated overall annual incidence of TB for HCWs was 4.2 cases per 100,000 population (range, 3.8–4.6), similar to the overall national TB case rate of 4.4–5.1 cases per 100,000 population during the same time period.12 However, the estimated annual incidence of TB among foreign-born HCWs was approximately 10 times higher than the incidence among US-born HCWs. Among male HCWs, the TB incidence rate was 2.3 cases per 100,000 US-born persons and 21.4 cases per 100,000 foreign-born persons; among female HCWs, the TB incidence rate was 1.6 cases per 100,000 US-born persons and 16.6 cases per 100,000 foreign-born persons. Nationally, the TB case rate ranged between 20.7 cases and 23.5 cases per 100,000 foreign-born persons during 2003–2007.12
HCWs Who Had TB Compared with Other Adults Who Had TB
Characteristics of persons with TB according to HCW status are summarized in Table 1. Compared with other adults, HCWs were more likely to be women (uOR, 4.1 [95% confidence interval (CI), 3.8–4.3]), be foreign born (uOR, 1.3 [95% CI, 1.3–1.4]), have extrapulmonary TB (uOR, 1.6 [95% CI, 1.5–1.7]), complete TB treatment (uOR, 2.5 [95% CI, 2.3–2.8]), and have a reported HIV test result (uOR, 1.2 [95% CI, 1.1–1.2]). Among cases with reported HIV test results, fewer HCWs (13%) than other adults (20%) were HIV infected.
TABLE 1.
Characteristics of Patients with Tuberculosis (TB), by Healthcare Worker (HCW) Status, among Individuals 18 Years of Age or Older, 1995–2007
| Patients with TB (n = 200,744) |
||
|---|---|---|
| Characteristic | HCWs (n = 6,049) |
Other adults (n = 194,695) |
| Female sex | 4,195 (69) | 69,661 (36) |
| Mean/median age at diagnosis, years | 41/40 | 49/47 |
| Age at diagnosis range, years | 18–91 | 18–112 |
| Age group, years | ||
| 18–35 | 2,322 (38) | 54,798 (28) |
| 36–54 | 2,774 (46) | 68,135 (35) |
| ≥55 | 953 (16) | 71,762 (37) |
| Birth country | ||
| United States | 2,736 (45) | 101,382 (52) |
| Othera | 3,302 (55) | 92,491 (48) |
| Unknown | 11 (<1) | 822 (<1) |
| TST result at time of TB diagnosisb | 4,724 (78) | 138,173 (71) |
| Positive | 4,175/4,724 (88) | 109,513/138,173 (79) |
| Negative | 549/4,724 (12) | 28,660/138,173 (21) |
| Culture positive for Mycobacterium tuberculosis | 4,829 (80) | 162,718 (84) |
| Site of disease | ||
| Pulmonary TB only | 3,803 (63) | 142,471 (73) |
| Extrapulmonary TB only | 1,766 (29) | 36,700 (19) |
| Both pulmonary and extrapulmonary TB | 477 (8) | 15,457 (8) |
| Findings among patients with any pulmonary TB | ||
| Positive acid-fast bacilli sputum smear result | 1,698/4,280 (40) | 75,135/157,928 (48) |
| Positive cavitary chest radiograph findingsc | 1,053/4,280 (25) | 43,313/157,928 (27) |
| Drug resistanced | 4,708 (78) | 157,213 (81) |
| Isoniazid monoresistance | 461/4,708 (10) | 12,094/157,213 (8) |
| Multidrug resistance | 89/4,708 (2) | 1,968/157,213 (1) |
| HIV test result reportede | 3,331 (55) | 99,621 (51) |
| HIV positive | 430/3,331 (13) | 20,392/99,621 (20) |
| Refused HIV test | 479 (8) | 11,394 (6) |
| HIV test not offered, result unknown, or not reported | 2,239 (37) | 83,680 (43) |
| No previous diagnosis of TB | 5,817 (96) | 182,244 (94) |
| Postmortem diagnosis of TB | 52 (<1) | 5,893 (3) |
| Excessive alcohol use | 215 (4) | 30,461 (16) |
| Injection or noninjection drug use | 131 (2) | 17,146 (9) |
| Incarceration at time of diagnosis | 23 (<1) | 7,674 (4) |
| Method of TB treatmentf | ||
| Directly observed therapy | 1,792/5,233 (34) | 79,679/170,478 (47) |
| Self-administered therapy | 2,071/5,233 (40) | 39,907/170,478 (23) |
| Both directly observed and self-administered therapy | 1,237/5,233 (24) | 41,661/170,478 (24) |
| Unknown | 133/5,233 (3) | 9,231/170,478 (5) |
| Treatment outcomef | ||
| Completed therapy | 4,745/5,233 (91) | 135,062/170,478 (79) |
| Did not complete therapy | 488/5,233 (9) | 35,416/170,478 (21) |
| Moved | 98/5,233 (2) | 5,133/170,478 (3) |
| Lost to follow-up | 62/5,233 (1) | 4,225/170,478 (2) |
| Died | 134/5,233 (3) | 15,420/170,478 (9) |
| Uncooperative/refused | 44/5,233 (1) | 1,114/170,478 (1) |
| Other/unknown | 150/5,233 (3) | 9,524/170,478 (6) |
NOTE. Data are no. (%) of persons with TB, unless otherwise indicated. Sum of percentages may not equal 100% due to rounding. HIV, human immunodeficiency virus; TST, tuberculin skin test.
Birth outside of the United States.
Analysis was limited to those with a reported TST result.
Analysis was limited to those with an abnormal chest radiograph finding.
Analysis was limited to those with a positive culture result and an isolate that had drug resistance results reported.
Numbers and percentages for HIV status do not include data for California or Vermont cases. California has not reported HIV data for TB cases since 2004 and, in earlier years, only reported cases as HIV infected or unknown; negative HIV test results were not reported. Vermont has not reported HIV data for TB cases since 2006.
Data were analyzed through 2005 to provide a 2-year period to complete reporting.
Clinical features of TB were similar among HCWs and other adults who had TB. Of those with reported initial drug-susceptibility results, HCWs had slightly higher percentages of isoniazid monoresistant TB (10% compared with 8% of other adults) and multidrug-resistant TB (2% compared with 1%); these differences were not statistically significant. Fewer HCWs (34%) were reported to have received all doses of TB medication by DOT, compared with 47% of other adults with TB (Table 1).
Foreign-Born HCWs Who Had TB Compared with US-Born HCWs Who Had TB
Of the 6,049 HCWs reported to have TB during those 13 years, 3,302 (55%) were foreign born. Of those, 67% were women, and 56% were Asian (Tables 1 and 2) From 1995 through 2007, the proportion of foreign-born HCWs with TB increased from 42% to 71%. Meanwhile, among all TB cases, the proportion of cases among foreign-born persons increased annually from 35% to 58%.12
TABLE 2.
Characteristics of Patients with Tuberculosis (TB) among US-Born and Foreign-Born Healthcare Workers (HCWs) 18 Years of Age or Older, 1995–2007
| HCWs with TB (n = 6,049) |
||
|---|---|---|
| Characteristic | US born (n = 2,736) |
Foreign born (n = 3,302) |
| Female sex | 1,969 (72) | 2,220 (67) |
| Mean/median age at diagnosis, years | 43/43 | 39/37 |
| Age at diagnosis range, years | 18–91 | 18–87 |
| Age group, years | ||
| 18–35 | 815 (30) | 1,504 (46) |
| 36–54 | 1,352 (49) | 1,417 (43) |
| ≥55 | 569 (21) | 381 (12) |
| Race/ethnicity | ||
| Black, non-Hispanic | 1,318 (48) | 815 (25) |
| White, non-Hispanic | 1,060 (39) | 194 (6) |
| Hispanic | 243 (9) | 418 (13) |
| Asian | 58 (2) | 1,836 (56) |
| American Indian/Alaska Native | 29 (1) | 3 (<1) |
| Native Hawaiian/Pacific Islander | 14 (<1) | 5 (<1) |
| Unknown or multiple races | 14 (<1) | 31 (1) |
| TST result at time of TB diagnosisa | 2,216 (81) | 2,501 (76) |
| Positive | 1,855 (84) | 2,315 (93) |
| Negative | 361 (16) | 186 (7) |
| Culture positive for Mycobacterium tuberculosis | 2,126 (78) | 2,692 (82) |
| Site of disease | ||
| Pulmonary TB only | 1,917 (70) | 1,883 (57) |
| Extrapulmonary TB only | 617 (23) | 1,143 (35) |
| Both pulmonary and extrapulmonary TB | 200 (7) | 276 (8) |
| Findings among patients with any pulmonary TB | ||
| Positive acid-fast bacilli sputum smear result | 861/2,117 (41) | 836 (39) |
| Positive cavitary chest radiograph findingsb | 550/2,117 (26) | 503 (23) |
| Drug resistancec | 2,056 (75) | 2,641 (80) |
| Isoniazid monoresistance | 130/2,056 (6) | 331/2,641 (13) |
| Multidrug resistance | 35/2,056 (2) | 54/2,641 (2) |
| HIV test result reportedd | 1,678 (67) | 1,649 (65) |
| HIV positive | 237/1,678 (14) | 193/1,649 (12) |
| Refused HIV test | 208 (8) | 268 (8) |
| HIV test not offered, result unknown, or not reported | 850 (31) | 1,385 (42) |
| No previous diagnosis of TB | 2,646 (97) | 3,162 (96) |
| Postmortem diagnosis of TB | 33 (1) | 18 (<1) |
| Excessive alcohol use | 172 (6) | 42 (1) |
| Injection or noninjection drug use | 106 (4) | 23 (1) |
| Incarceration at time of diagnosis | 19 (1) | 4 (<1) |
| Method of TB treatmente | ||
| Directly observed therapy | 955/2,457 (39) | 835/2,710 (31) |
| Self-administered therapy | 856/2,457 (35) | 1,202/2,710 (44) |
| Both directly observed and self-administered therapy | 595/2,457 (25) | 642/2,710 (24) |
| Unknown | 51/2,457 (2) | 31/2,710 (1) |
| Treatment outcomee | ||
| Completed therapy | 2,229/2,457 (91) | 2,508/2,710 (93) |
| Did not complete therapy | 228/2,457 (9) | 202/2,710 (7) |
| Moved | 27/2,457 (1) | 71/2,710 (3) |
| Lost to follow-up | 26/2,457 (1) | 36/2,710 (1) |
| Died | 86/2,457 (4) | 46/2,710 (2) |
| Uncooperative/refused | 31/2,457 (1) | 13/2,710 (<1) |
| Other/unknown | 58/2,457 (2) | 36/2,710 (1) |
NOTE. Data are no. (%) of persons with TB, unless otherwise indicated. Sum of percentages may not equal 100% due to rounding. HIV, human immunodeficiency virus; TST, tuberculin skin test.
Analysis was limited to those with a reported TST result.
Analysis was limited to those with an abnormal chest radiograph finding.
Analysis was limited to those with a positive culture result and an isolate that had drug resistance results reported.
Numbers and percentages for HIV status do not include data for California or Vermont cases. California has not reported HIV data for TB cases since 2004 and, in earlier years, only reported cases as HIV infected or unknown; negative HIV test results were not reported. Vermont has not reported HIV data for TB cases since 2006.
Data were analyzed through 2005 to provide a 2-year period to complete reporting.
Compared with US-born HCWs who had TB, foreign-born HCWs who had TB were more likely to have isoniazid monoresistant TB (uOR, 2.1 [95% CI, 1.7–2.7]), have extrapulmonary TB (uOR, 1.5 [95% CI, 1.3–1.7]), and complete TB treatment (uOR, 1.3 [95% CI, 1.1–1.6]; Table 2).
The top 3 countries of birth for foreign-born HCWs with TB in the United States were Philippines (32%), India (15%), and Haiti (6%), which represented 53% of all foreign-born HCWs with TB (Figure 1), whereas only 21% of other foreign-born adults with TB were from those 3 countries combined. In contrast, during this time period, the top countries of birth for all foreign-born persons with TB in the United States were Mexico (24%), Philippines (11%), and Vietnam (10%).12 The median number of years that foreign-born HCWs had resided in the United States was 7 (range, 0–64). Approximately 7% of foreign-born HCWs received a diagnosis of TB within 6 months of arrival to the United States; 18% received a diagnosis within the first year after arrival, 25% within 2 years after arrival, and 43% within 5 years after arrival. In stratified analysis comparing foreign-born Asian HCWs with other foreign-born HCWs, extrapulmonary TB was reported for 46% of foreign-born Asian HCWs, compared with 23% of other foreign-born HCWs.
figure 1.
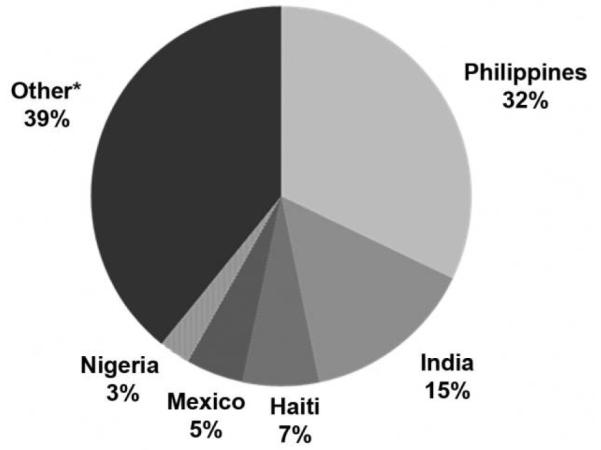
Top 10 countries of birth of foreign-born healthcare workers who had tuberculosis in the United States, 1995–2007 (n = 3,302). *“Other” includes Kenya (2%), Vietnam (2%), China (2%), Ethiopia (2%), Peru (2%), and others.
DISCUSSION
Although the rate of TB among HCWs was similar to the national rate, consequences in the workplace can be severe when HCWs have TB because of the vulnerable populations that they serve. These findings enable additional understanding of TB among HCWs in the United States and highlight the importance of maintaining a high index of suspicion for TB disease, especially among foreign-born workers, and of providing interventions to diagnose and treat LTBI among HCWs.
Despite the 2005 estimate that only 15% of HCWs in the United States were foreign born,13 the estimated annual incidence of TB was approximately 10 times higher among foreign-born HCWs during 2003–2007 than among US-born HCWs, and more than half of all TB cases among HCWs during 1995–2007 occurred among foreign-born persons, which reflects the growing number of TB cases among foreign-born persons in the United States.12,14
Overall, during this time period, 11%–12% of foreign-born persons with TB were from Philippines. That percentage is in contrast to the 32% of foreign-born Filipino HCWs in this analysis, although consistent with the high proportion of foreign-born HCWs in the United States from Philippines.15,16 In 2000, almost 40% of internationally trained nurses in the United States were Filipino.16 In 2005, Philippines reported a TB incidence rate of 291 cases per 100,000 persons.17
Findings of our stratified analysis were also consistent with several studies that suggested that, compared with the general population, foreign-born persons, including HCWs, and specifically South Asian HCWs, were more likely to have extra-pulmonary TB than pulmonary TB.18-21
The findings in this report are subject to a number of limitations. Seven percent of the 1995–2007 TB cases had missing data for occupation, and data were incomplete for other variables; HIV test results and treatment outcomes were missing for 37% and 8% of all HCWs, respectively (Table 1). However, completeness of reported TB data improved throughout the study period. For example, in 1995, 45% of all reported TB cases were missing information on HIV status; in 2007, 23% had missing HIV data. Also, for the years included in this analysis, the National TB Surveillance System did not collect the specific occupation, duration of employment in healthcare, or type of healthcare facility, nor did it collect previous diagnosis or treatment of LTBI.
In 2009, the National TB Surveillance System was modified to include LTBI history and, for foreign-born individuals, immigration status. This additional information could provide a better understanding of which interventions may improve diagnosis and treatment of LTBI among foreign-born HCWs before or soon after entry into the United States. In general, only individuals entering the United States as immigrants or refugees are subject to a TB screening before entry.22 Of the foreign-born HCWs in this analysis, 25% received a diagnosis of TB within 2 years after arrival to the United States, which suggests that infection was acquired before entry rather than within the United States, which is a finding consistent with other studies.23,24
According to the reported data, HCWs were less likely than other adults with TB to have received all doses of treatment by DOT. DOT has multiple benefits, including maximizing the likelihood of treatment completion, preventing development of drug-resistant disease, and providing an opportunity to identify possible adverse effects of the medication. Providing DOT for HCWs at their work site has been an effective option for ensuring HCWs complete treatment for TB disease and, when possible, for LTBI.5,10 Identifying and treating LTBI is critical to preventing TB disease in this occupational group, but HCWs appear to be less likely to accept treatment for LTBI.25-27
Healthcare institutions, especially those associated with a high risk for TB exposure,10 may benefit from an intensified approach to TB education and screening of HCWs upon hire, particularly foreign-born workers, and from encouraging completion of treatment for LTBI, if indicated. Such strategies have been associated with cost savings.28 National guidelines recommend that HCWs who may be exposed to TB at the workplace be screened for TB disease symptoms and receive a tuberculin skin test or an interferon γ release assay blood test for TB infection annually.10 Strengthening TB prevention and control in healthcare settings will protect HCWs from TB, which will in turn protect patients and the community and further our progress toward the goal of TB elimination in the United States.
ACKNOWLEDGMENTS
We thank the healthcare providers and all state and local health departments throughout the United States whose staff collected and reported the data that made these analyses possible. We thank Ryan Wallace from the Centers for Disease Control and Prevention for assistance with data analysis and Tom Navin, MD, also from the Centers for Disease Control and Prevention, for valuable insight into the manuscript.
Financial support. The Centers for Disease Control and Prevention.
Footnotes
Potential conflicts of interest. All authors report no conflicts of interest relevant to this article. All authors submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and the conflicts that the editors consider relevant to this article are disclosed here.
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Dooley SW, Jarvis WR, Martone WJ, Snider DE., Jr Multidrug-resistant tuberculosis. Ann Intern Med. 1992;117:257–259. doi: 10.7326/0003-4819-117-3-257. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Nosocomial transmission of multidrug-resistant tuberculosis to health-care workers and HIV-infected patients in an urban hospital—Florida. MMWR Morb Mortal Wkly Rep. 1990;39:718–722. [PubMed] [Google Scholar]
- 3.Pearson ML, Jereb JA, Frieden TR, et al. Nosocomial transmission of multidrug-resistant Mycobacterium tuberculosis: a risk to patients and health care workers. Ann Intern Med. 1992;117(3):191–196. doi: 10.7326/0003-4819-117-3-191. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Nosocomial transmission of multidrug-resistant tuberculosis among HIV-infected persons: Florida and New York, 1988–1991. MMWR Morb Mortal Wkly Rep. 1991;40:585–591. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention Mycobacterium tuberculosis transmission in a newborn nursery and maternity ward: New York City, 2003. MMWR Morb Mortal Wkly Rep. 2005;54(50):1280–1283. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Tuberculosis transmission in a renal dialysis center: Nevada, 2003. MMWR Morb Mortal Wkly Rep. 2004;53(37):873–875. [PubMed] [Google Scholar]
- 7.Villarino ME, Mazurek G. Tuberculosis contacts, concerns, and controls: what matters for healthcare workers? Infect Control Hosp Epidemiol. 2006;27(5):433–435. doi: 10.1086/504499. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Census Bureau, DataFerrett [Accessed November 20, 2008];Current Population Survey, July 2003–2007. http://dataferrett.census.gov/
- 9.American Thoracic Society. Centers for Disease Control and Prevention. Infectious Diseases Society of America Treatment of tuberculosis. MMWR Recomm Rep. 2003;52(RR-11):76. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Morb Mortal Wkly Rep. 2005;54(17):1–141. [PubMed] [Google Scholar]
- 11.Fujiwara PI, Larkin C, Frieden TR. Directly observed therapy in New York City; history, implementation, results, and challenges. Chest. 1997;18(1):137. doi: 10.1016/s0272-5231(05)70363-4. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention . Reported tuberculosis in the United States, 2007. Vol. 18. U.S. Department of Health and Human Services; Atlanta, GA: 2008. [Google Scholar]
- 13.Migration Information Source [Accessed November 20, 2008];Foreign-born health-care workers in the United States, 2007. http://www.migrationinformation.org/
- 14.Driver CR, Stricof RL, Granville K, et al. Tuberculosis in health care workers during declining tuberculosis incidence in New York State. Am J Infect Control. 2005;33(9):519–526. doi: 10.1016/j.ajic.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 15.Manangan LP, Jumao-as Salibay C, Wallace RM, et al. Tuberculosis among persons born in the Philippines and living in the United States, 2000–2007. Am J Public Health. 2011;101:101–111. doi: 10.2105/AJPH.2009.175331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xu Y, Kwak C. Characteristics of internationally educated nurses in the United States. Nursing Economics. 2005;23(5):233–238. [PubMed] [Google Scholar]
- 17.World Health Organization (WHO) Global Tuberculosis Control: Surveillance, Planning, Financing: WHO Report 2007. World Health Organization; Geneva: 2007. WHO/HTM/TB/2007.376. [Google Scholar]
- 18.Fiske CT, Griffin MR, Erin H, et al. Black race, sex, and extra-pulmonary tuberculosis risk: an observational study. BMC Infectious Diseases. 2010;10:16. doi: 10.1186/1471-2334-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asghar RJ, Pratt RH, Kammerer S, Navin TR. Tuberculosis in South Asians living in the United States, 1993–2004. Arch Intern Med. 2008;168(9):936–942. doi: 10.1001/archinte.168.9.936. [DOI] [PubMed] [Google Scholar]
- 20.Fulton D, Kline S. Tuberculosis at the University of Minnesota Medical Center, 2000 to 2006, a brief report. Minn Med. 2010;93(6):50–52. [PubMed] [Google Scholar]
- 21.Peto HM, Pratt RH, Harrington TA, LoBue PA, Armstrong LR. Epidemiology of extrapulmonary tuberculosis in the United States, 1993–2006. Clin Infect Dis. 2009;49:1350–1357. doi: 10.1086/605559. [DOI] [PubMed] [Google Scholar]
- 22.Maloney SA, Fielding KL, Laserson KF, et al. Assessing the performance of overseas tuberculosis screening programs: a study among US-bound immigrants in Vietnam. Arch Intern Med. 2006;166(2):234–240. doi: 10.1001/archinte.166.2.234. [DOI] [PubMed] [Google Scholar]
- 23.Cain KP, Benoit SR, Winston CA, Mac Kenzie WR. Tuberculosis among foreign-born persons in the United States. JAMA. 2008;300(4):405–412. doi: 10.1001/jama.300.4.405. [DOI] [PubMed] [Google Scholar]
- 24.Chin DP, DeRiemer K, Small PM, et al. Differences in contributing factors to tuberculosis incidence in U.S.-born and foreign-born persons. Am J Respir Crit Care Med. 1998;158:1797–1803. doi: 10.1164/ajrccm.158.6.9804029. [DOI] [PubMed] [Google Scholar]
- 25.Sterling TR, Hass DW. Transmission of Mycobacterium tuberculosis from health care workers. N Engl J Med. 2006;355(2):118–121. doi: 10.1056/NEJMp068015. [DOI] [PubMed] [Google Scholar]
- 26.Horsburgh CR, Jr, Goldberg S, Bethel J, et al. Latent tuberculosis infection treatment acceptance and completion in the United States and Canada. Chest. 2010;137:401–409. doi: 10.1378/chest.09-0394. [DOI] [PubMed] [Google Scholar]
- 27.LoBue PA, Catanzaro A. Effectiveness of a nosocomial tuberculosis control program at an urban teaching hospital. Chest. 1998;113(5):1184–1189. doi: 10.1378/chest.113.5.1184. [DOI] [PubMed] [Google Scholar]
- 28.Salpeter SR, Salpeter EE. Screening and treatment of latent tuberculosis among healthcare workers at low, moderate, and high risk for TB exposure: a cost-effectiveness analysis. Infect Control Hosp Epidemiol. 2004;25(12):1056–1061. doi: 10.1086/502343. [DOI] [PubMed] [Google Scholar]


