Abstract
Identification of health issues in children with autism spectrum disorder (ASD) is paramount to provide appropriate care and interventions. The Autism Treatment Evaluation Checklist (ATEC) is the one of the few current measures that assesses ASD-associated health problems thus informing intervention decisions. However, little research has been conducted to compare ATEC with other more recognized measures such as the Childhood Autism Rating Scale (CARS). It is unclear whether these two scales can be used interchangeably or whether high scores on one scale are comparable to the other. The aim of the current study was to compare the correlation between ATEC and CARS in the evaluation of children with ASD. This prospective cross-sectional study was conducted at the Developmental and Behavioural Paediatrics Outpatient Clinic at King Saud University, King Khalid University hospital (KKUH) in Riyadh, Saudi Arabia. Forty children with a prior diagnosis of ASD seen during the period from October 2014 to August 2015 were included. Each child was assessed using ATEC and CARS independently during the same visit. The Spearman’s rank correlation coefficient test was used. The overall mean CARS score was 34.125 ± 5.535 (range from 22 to 42) and the mean ATEC score was 40.95± 9.1934.1 (range from 24 to 72). The Spearman’s rank correlation coefficient (rs) was 0.015, and p-value was 0.926 (> 0.05) meaning that there was no correlation between CARS and ATEC scales. No correlation between CARS and ATEC scale was found. ATEC should not be used instead of CARS to delineate co-morbid health issues. Future studies are needed to assess the validity of ATEC and its correlation with other well established scales.
Keywords: Autism spectrum disorder, Autism Treatment Evaluation Checklist, Childhood Autism Rating Scale
Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disability. It is characterized by a qualitative impairment in communication and social interaction in addition to a range of restricted stereotyped, repetitive behaviours and interests as described in the Diagnostic and Statistical Manual of Mental Disorders, 4th Revision (DSM-IV) [1]. There is a substantial evidence suggesting that children with ASD tend to have more health-related problems compared to typically developing children [2,3]. Reported co-morbidities include anxiety [4,5], hyperactivity [6], aggressiveness and destructive behaviours [7], gastrointestinal problems [8], sleep disturbances [9,10] and sensory processing abnormalities [11–13].
A few behavioural rating scales in which a wide range of symptoms are assessed have been developed to accurately diagnose ASD. However, most of the well-established ASD measures do not address related health issues. The Autism Treatment Evaluation Checklist (ATEC) [14] is exceptional in that it provides an insight into health issues often missed by most other scales. The ATEC is a parent-rated measure.
The purpose of this study was to compare the scores on the ATEC with those on the Childhood Autism Rating Scale (CARS) which is a well-established professionals-rated measure to identify children with ASD.
Materials and Methods
Participants
This prospective cross-sectional study was conducted at the Developmental and Behavioural Paediatrics outpatient clinic in King Saud University at King Khalid University Hospital (KKUH) in Riyadh, Saudi Arabia. A total of 40 children with a diagnosis of ASD who were attending for routine follow-up in this clinic during the period from October 2014 to August 2015 were included. Participants were previously diagnosed with ASD by qualified professionals using the Autism Diagnostic Observation Schedule (ADOS) which is considered a ‘gold standard’. Children with a genetic, neurologic or metabolic diagnosis were excluded. The study protocol was explained to the parents and informed consent was obtained. Each child was independently assessed using both ATEC and CARS during the same clinic visit. Parents were asked to complete ATEC while in the waiting area. Afterwards, CARS was performed by a qualified psychologist specifically trained to carry out such tests. Scores on both scales were separately collated and raw scores (see below) were obtained by a qualified psychologist.
Neither the professional nor the parent was aware of the scores generated from their respective completed tests. Statistical analysis was performed to examine the relationship between the total scores of CARS and ATEC. Demographic data was collected on each participant as well as a detailed medical history including any periods of developmental regression.
Clinical Measures
CARS was shown to have high sensitivity and specificity in distinguishing children with autism from children with learning disabilities and distinguishing ASD from other developmental disorders [15]. A number of studies found a high agreement between the DSM-IV and CARS [16–18].
CARS is a 15-item behavioural rating scale developed to diagnose autism in combination with clinical judgment. Additionally, it assesses the severity of the disorder. Studies have shown that CARS is a reliable and a stable indicator of autism in any child over 2 years of age as well as in adolescents [19]. Items included in this scale are: relating to people; imitation; emotional response; body use; object use; adaptation to change; visual response; listening response; taste, smell, touch response and use; fear or nervousness; verbal communication; nonverbal communication; activity level; level and consistency of intellectual response and general impressions. Each item is scored from 1 (no pathology) to 4 (severe pathology). Total scores are then calculated as ‘raw scores’ and severity is classified according to the following: a total score of 15–29.5 is considered ‘non-autistic’, a score of 30–36.5 is considered ‘mild to moderate’ autism and a score of 37–60 is considered ‘moderate to severe’ autism [20].
The Autism Treatment Evaluation Checklist (ATEC) was developed by the Autism Research Institute (San Diego, CA) [21]. ATEC is a one page form designed to be completed by parents or teachers [14]. ATEC has been validated to be used in children above the age of 2 years. It consists of four subtest scales: Scale I (speech/language/communication; has 14 items. Scores can range from 0 to 28), Scale II (sociability; has 20 items. Scores can range from 0 to 40), Scale III (sensory/cognitive awareness; has 18 items. Scores can range from 0 to 36) and Scale IV (Health/Physical/Behaviour; has 25 items). Each subcategory of the ATEC scale is scored using a 0–3 point scale as follows: 0= not a problem, 1=minor problem, 2= moderate problem and 3= serious problem. Total score ranges from 0 to 180. The higher the total score, the more impaired the participant. The ATEC has been successfully used to measure treatment effects and progress over time in several ASD studies [22]. However, the ATEC is not nationally normed and the evidence for reliability and validity is limited.
Statistical Analysis
This was performed using Statistical Package for Social Sciences, version 21, software (SPSS Inc., Chicago, IL, USA). Mean ± SD, median and range of the two scales (CARS, ATEC) were calculated. Percentages for all nominal variables (age, gender, nationality, regression and severity of ASD) were also calculated.
Kolmogorov-Smirnov test of normality to check if data of both scales were normally distributed was used. Data of the two scales were not normally distributed, so Spearman correlation coefficient was used to evaluate the correlation between the two total scores. When p-value was less than 0.05 (p< 0.05), this was assumed to be of a statistically significant difference.
Results
As summarized in Table 1, the study participants’ ages ranged between 3 to 12 years with a mean age of 5.6 ± 2.52 years. There were more males (n= 33, 82.5%) than females (n= 7, 17.5%) in the sample. Accordingly, the male: female ratio was 4.7:1. Among the participants, Saudi children were more preponderant than non-Saudis (87.5% vs. 12.5% respectively).The majority of the participants experienced a regressive event in their development at any time from birth (n= 28, 70%) whilst only 12 participants (30%) had a negative history of regression (n= 12, 30%). Based on the CARS scale, 21participants (52.5%) had mild to moderate ASD and 19 participants (47.5%) had moderate to severe ASD.
Table 1.
Demographic characteristic of participants with autism spectrum disorder (ASD) diagnosis
| Age | |
| Mean ± SD | 5.6 ± 2.52 |
| Median (Minimum – Maximum) | 5 (3 – 12) |
| Gender | |
| Male | 33 (82.5 %) |
| Female | 7 (17.5 %) |
| Nationality | |
| Saudi | 35 (87.5 %) |
| *Non-Saudi | 5 (12.5 %) |
| Regression | |
| Yes | 28 (70.0 %) |
| No | 12 (30.0 %) |
| ASD severity | |
| Mild to moderate | 21 (52.5 %) |
| Moderate to severe | 19 (47.5 %) |
Included participants of Yemeni (n=1), Syrian (n=2), Egyptian (n=1) and Sudanese (n=1) origin.
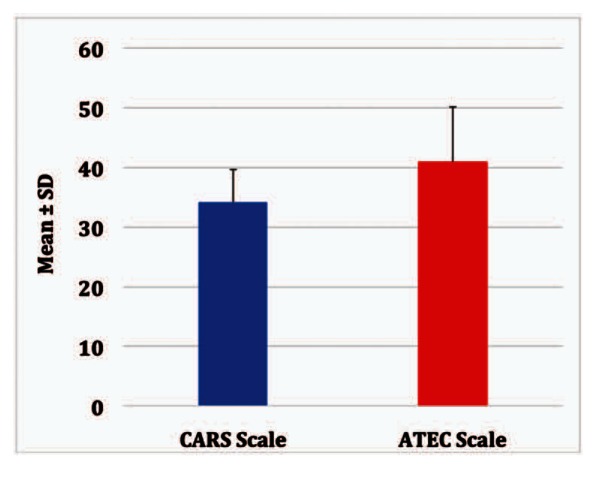
The overall mean CARS score was 34.125 ± 5.535 (range from 22–42) and the mean ATEC score was 40.95± 9.1934 (range from 24 to 72) for study participants. Table 2 summarizes the scores form ATEC and CARS and figure 1 illustrates the comparison. Table 3 summarizes the relationship between CARS and ATEC scores.
Table 2.
Scores from the Autism Treatment Evaluation Checklist (ATEC) and the Childhood Autism Rating Scale (CARS)
| ATEC Scale (n=40) | CARS Scale (n=40) | ||
|---|---|---|---|
| Different scales | Mean ± SD | 5.535 ± 34.125 | 9.193 ± 40.95 |
| Median (Minimum – Maximum) | (42 – 22) 34.25 | (72 – 24) 42 | |
| Interquartile Range | 10 | 9 |
Figure 1.
Comparison of the scores from both the Autism Treatment Evaluation Checklist (ATEC) and Childhood Autism Rating Scale (CARS)
Table 3.
Spearman correlation coefficient between the Autism Treatment Evaluation Checklist (ATEC) and Childhood Autism Rating Scale (CARS)
| CARS Scale | |
|---|---|
| ATEC Scale | *rs = 0.015 |
| P-value = 0.926 |
Spearman correlation coefficient
No significant correlation between CARS and ATEC was found as evidenced by Spearman correlation coefficient (rs = 0.015 and p-value = 0.926).
Discussion
This study demonstrated that no significant statistical correlation between professional-administered CARS scores and parental-administered ATEC scores. Several scales were developed to diagnose ASD focusing mainly on the core features of the disorder [23,24]. However, there is only a small number of measures that address heath and systemic concerns for children with ASD. ATEC is unique in that it does address these issues. To the author’s knowledge, not many studies focused on comparing ATEC with the more well established conventional ASD measures. ATEC scale gives a better understanding of health and systemic issues in ASD such as sleep problems, seizures, eating, gastrointestinal issues, hyperactivity, self-injuries and so forth. ATEC is easy to understand and to administer by parents and only takes little time to be completed. Furthermore, ATEC assesses the severity of impairment in different domains and progress overtime in response to early intervention and medications if used. Lastly, ATEC is readily available on request from the Autism Research Institute (ARI) and it is free of charge. Future studies should focus on the validity of ATEC and its correlation with gold standard scales to determine its usability in clinical settings.
Strengths and limitations
Amongst the strengths of this study was that a single professional performed CARS evaluation on all participants thus minimizing subjective differences in scoring methods. This had led to significantly reducing potential unknown confounding factors in the data examined. Moreover, the psychologist administering the test was blinded to the results of the parallel measure.
Data was collected in a prospective manner on participants that were already diagnosed with ASD thereby lessening results bias and adding strength to the study. Furthermore, data was collected in a method similar to that employed in clinical settings which had probably ensured reproducibility as well as applicability. Given that the demographic data of the study participants bear a degree of resemblance to that of general population of children with ASD, the results could potentially be generalized to an extent.
There are a few limitations to be considered when interpreting the results of this study. The study sample was small and was collected from one developmental clinic. Data collection from ATEC scale was based on parents’ reports which can be subject to social desirability and recall bias. Another limitation is that participants were examined at a single point in time using ATEC and CARS evaluations. It remains unclear how the observed correlations between ATEC and CARS evaluations would vary over the course of time.
Conclusion
Currently, there is no correlation between total ATEC and CARS scores. More studies are needed on the validity of ATEC and its correlation with the more established scales to determine its applicability in clinical practice.
Acknowledgement
The author thanks all clinical staff, psychologists and nurses who supported this study. Special thanks to all parents and children who participated in the study.
References
- 1.Ozonoff S, Goodlin-Jones BL, Solomon M. Evidence-based assessment of autism spectrum disorders in children and adolescents. J Child Adolesc Psychol 2005; 34(3):523–540 [DOI] [PubMed] [Google Scholar]
- 2.Atladóttir HO, Thorsen P, Schendel DE, Østergaard L, pLemcke S, Parner ET. Association of hospitalization for infection in childhood with diagnosis of autism spectrum disorders: A Danish cohort study. Arch Pediatr Adolesc Med. 2010; 164(5): 470–477. [DOI] [PubMed] [Google Scholar]
- 3.Schieve LA, Gonzalez V, Boulet SL, Visser SN, Rice CE, Van Naarden Braun K, et al. Concurrent medical conditions and health care use and needs among children with learning and behavioural developmental disabilities: National Health Interview Survey, 2006–2010. Res Dev Disabil. 2012. March–April; 33(2):467–76. [DOI] [PubMed] [Google Scholar]
- 4.Green SA, Ben-Sasson A, Soto TW, Carter AS. Anxiety and sensory over-responsivity in toddlers with autism spectrum disorders: bidirectional effects acrosstime. J Autism Dev Disord 2012; 42(6):1112–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spiker MA, Lin CE, Van Dyke M, Wood JJ. Restricted interests and anxiety in children with autism. Autism 2012; 16(3):306–320 [DOI] [PubMed] [Google Scholar]
- 6.Banaschewski T, Poustka L, Holtmann M. Autism and ADHD across the life span. Differential diagnoses or comorbidity? Nervenarzt 2011; 82(5):573–580 [DOI] [PubMed] [Google Scholar]
- 7.Smith KR, Matson JL. Behaviour problems: differences among intellectually disabled adults with co-morbid autism spectrum disorders and epilepsy. Res Dev Disabil 2010; 31(5):1062–1069 [DOI] [PubMed] [Google Scholar]
- 8.Nikolov RN, Bearss KE, Lettinga J, Erickson C, Rodowski M, Aman MG, et al. Gastrointestinal symptoms in a sample of children with pervasive developmental disorders. J Autism Dev Disord. 2009; 39(3):405–413. [DOI] [PubMed] [Google Scholar]
- 9.Taira M, Takase M, Sasaki H. Sleep disorder in children with autism. Psychiatry Clin Neurosci 1998; 52(2):182–183 [DOI] [PubMed] [Google Scholar]
- 10.Miano S, Ferri R. Epidemiology and management of insomnia in children with autistic spectrum disorders. Paediatr Drugs 2010; 12(2):75–84 [DOI] [PubMed] [Google Scholar]
- 11.Piek JP, Dyck MJ. Sensory-motor deficits in children with developmental coordination disorder, attention deficit hyperactivity disorder and autistic disorder. Hum Mov Sci 2004; 23:475–488 [DOI] [PubMed] [Google Scholar]
- 12.Green SA, Ben-Sasson A, Soto TW, Carter AS. Anxiety and sensory over-responsivity in toddlers with autism spectrum disorders: bidirectional effects across time. J Autism Dev Disord 2012; 42(6):1112–1119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kern JK, Trivedi MH, Garver CR, Grannemann BD, Andrews AA, Savla JS, et al. The pattern of sensory processing abnormalities in Autism. Autism 2006; 10(5):480–494 [DOI] [PubMed] [Google Scholar]
- 14.Rimland B, Edelson M. Autism Treatment Evaluation Checklist. Autism Research Institute, 4812 Adams Avenue, SanDiego, CA 92116, 1999. [Google Scholar]
- 15.Chlebowski C, Green JA, Barton ML, Fein D. Using the Childhood Autism Rating Scale to diagnose autism spectrum disorders. J Autism Dev Disord 2010 Jul; 40(7):787–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perry A, Condillac RA, Freeman N, Dunn-Geier J, Belair J. Multi-site study of the Childhood Autism Rating Scale (CARS) in five clinical groups of young children. J Autism Dev Disord 2005; 35(5):625–634 [DOI] [PubMed] [Google Scholar]
- 17.Rellini E, Tortolani D, Trillo S, Carbone S, Montecchi F. Childhood Autism Rating Scale (CARS) and Autism Behaviour Checklist (ABC) correspondence and conflicts with DSM-IV criteria in diagnosis of autism. J Autism Dev Disord 2004; 34(6):703–708 [DOI] [PubMed] [Google Scholar]
- 18.Pereira A, Riesgo RS, Wagner MB. Childhood autism: Translation and validation of the Childhood Autism Rating Scale for use in Brazil. J Pediatr (Rio J) 2008; 84(6): 487–494. [DOI] [PubMed] [Google Scholar]
- 19.Garfin DG, McCallon D, Cox R. Validity and reliability of the Childhood Autism Rating Scale with autistic adolescents. J Autism Dev Disord 1988; 18(3):367–378. [DOI] [PubMed] [Google Scholar]
- 20.Schopler E, Reichler RJ, DeVellis RF, Daly K. Toward objective classification of childhood autism: Childhood Autism Rating Scale (CARS). J Autism Dev Disord 1980; 10: 91–103 [DOI] [PubMed] [Google Scholar]
- 21.Geier DA, Kern JK, Geier MR. A comparison of the Autism Treatment Evaluation Checklist (ATEC) and the Childhood Autism Rating Scale (CARS) for the quantitative evaluation of autism. J Ment Health Res Intellect Disabil 2013; 6(4):255–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Magiati I, Moss J, Yates R, Charman T, Howlin P. Is the Autism Treatment Evaluation Checklist a useful tool for monitorin progress in children with autism spectrum disorders? J Intellect Disabil Res. 2011; 55(3): 302–331 [DOI] [PubMed] [Google Scholar]
- 23.Eaves RC, Milner B. The criterion-related validity of the Childhood Autism Rating Scale and the Autism Behaviour Checklist. J Abnorm Child Psychol. 1993; 21(5): 481–491. [DOI] [PubMed] [Google Scholar]
- 24.Freeman BJ, Ritvo ER, Yokota A, Ritvo A. A scale for rating symptoms of patients with the syndrome of autism in real life settings. J Am Acad Child Psychiatry. 1986; 25(1): 130–136. [DOI] [PubMed] [Google Scholar]