Abstract
This is a retrospective observational hospital-based study aimed to determine the prevalence and outcome of severe acute malnutrition in children less than five years admitted to Omdurman Paediatric Hospital during the period January 2014 to December 2014. Data was collected from patient’s hospital records during the study period. Ethical approval and permission to access patients’ record were obtained. A total of 593 children with severe malnutrition were identified; 305 of cases were male (51.4%) with a male: female ratio of 1:0.9. The mean age these children was 22.3 months. Children 36–59 months were least affected. 35.4% were classified as low socioeconomic class, 22.9% classified as an average class and there were no sufficient data to classify the remaining. The overall prevalence of severe malnutrition was 6.5%, and the general mortality rate was 2.4% while mortality rate among children with severe malnutrition was 9.3%. Among the 593 admitted children with malnutrition, 407 (68.6%) had marasmus, 141 (23.8%) had kwashiorkor and 45 (7.6%) had marasmic-kwashiorkor. The highest prevalence and mortality rate occurred in September. The most common clinical presentations were gastroenteritis, malaria, urinary tract infections, giardiasis, tuberculosis and AIDS. Only 10.8% of the admitted children were exclusively breast fed for the first three months. 33% were fully vaccinated. Overall 75.7% improved and discharged, 15% discharged against medical advice and 9.3% died. We concluded that prevalence and mortality among children with acute severe malnutrition at Omdurman paediatrics hospital were high, and the current management strategies require review to identify the causes. We recommended adopting policies to manage malnutrition in the community and hospitals.
Keywords: Under five children, Protein energy malnutrition, Prevalence, Mortality rate
Introduction
The term Malnutrition covers a wide range of illnesses, including under nutrition, specific nutrient deficiencies and over nutrition. It kills, retards, cripples, blinds and impairs human developments ontruly massive scale worldwide [1]. Severe protein-energy malnutrition (PEM) is a leading cause of death among children younger than five years of age. Malnutrition is classified into two classical syndromes, marasmus (wasting syndrome) and kwashiorkor, or a mixture of both (marasmic-kwashiorkor).
Children are the most nutritionally vulnerable group especially in the developing world. According to surveys conducted between 1987 and 1998, two out of five of these children are stunted, one in three is underweight and one in ten is wasted; the numbers vary considerably among regions. Annually, some 30 million infants, around 82,000 every day, are born with intrauterine malnutrition growth retardation mainly due to poor maternal nutritional status. The highest level of stunting is found in Eastern Africa, where 48.1% of preschool children were affected in the year 2000 [2]. In this part of the world stunting is increasing at 0.08 % per year [2].
Sudan is a one of eastern African countries, where in 1993, the Ministry of Health and the National Nutrition Department (NND) conducted a comprehensive nutrition survey in the states most affected by nutritional problems and displacement. The numbers of children covered by the survey in the selected states were 3600. The overall rate of malnutrition was found to be 19.6% (6.80% severe, 12.8% moderate).
According to the Sudan simple special survey methodology (S3M) survey which is conducted jointly by UNICEF and MOH in 2013, there is a mix of very different realities across the country with high levels of stunting (chronic malnutrition) and low levels of coverage for safe water and sanitation in some areas. Poor feeding practice is a problem across the country, with localities in Kassala and Gedaref states among the most critical. The Eastern region and the three Kordofan states have the lowest coverage of safe drinking water and sanitation facilities, while the Red Sea, Blue Nile and the Darfur region show the highest prevalence of diarrhoea. The good news is that the use of iodized salt has improved, reaching over 90% of households in some localities in Red Sea, South Darfur, Blue Nile and Kassala [3].
The prevalence of malnutrition imposes significant costs on the Sudanese economy as well as society. The high mortality due to malnutrition leads to the loss of the economic potential of the child. It affects children in many ways, predisposing them to different infectious diseases, psychosocial mal-development, and cognitive deficiencies. The cost of hospital admission and treatment in addition to parental days off work should not be ignored.
Reducing malnutrition and its consequences is a global and development goal as stated by the Millennium Development Goals (MDGs) and the Sudan Growth and Development Strategy (SGDS).This study targets the latter by providing information that may assist in improvingcurrent available services for treatment of severe malnutrition.
Although acute malnutrition is acknowledged as one of the major health problems at Omdurman paediatrics hospital, there is paucity of data on the prevalence and outcome of this condition in the hospital. Therefore, the objectives of this study was to determine the prevalence of acute severemalnutrition, and outcomes of severely malnourished children less than five years old admitted to Omdurman paediatrics Hospital and to provide recommendations for improvement accordingly.
Materials and Methods
Study settings
Omdurman Paediatric Hospital
Omdurman is the largest city in Sudan, lying on the western banks of the River Nile. Omdurman, Khartoum and Khartoum North form the capital of Sudan, Khartoum State. Omdurman has a population of 2,395,159 as per 2008 national census and is the national centre of commerce. Omdurman Paediatric Hospital is the biggest public teaching hospital in Sudan, established in 1986 in an area of 6000 m 2with bed capacity of 290 beds.
Methods
This is a oneyear (January 2014 – December 2014) retrospective, quantitative and hospital based study. We identified cases of PEM from hospital registers and obtained relevant information of the study population from patient’s hospital records. These information include type of PEM (marasmus, kwashiorkor, or marasmic-kwashiorkor), date of admission and discharge, history of breast feeding, socioeconomic status of the care-giver, associated co-morbidities, vaccination history, and the outcome (improved and discharge, discharge against medical advice or died).
Inclusion and exclusion criteria
All children with age less than 5-year-old admitted to Omdurman Paediatric hospital with severe malnutrition in 2014 were included. Those with chronic illness in addition to severe malnutrition were excluded (e.g cardiovascular disease, tuberculosis, cerebral palsy, microcephaly or sickle cell disease).
Ethical considerations
Ethical approval was obtained from the hospital administration board to review patient’s records at the hospital statistical office.
Statistical analysis
Data were analysed using SPSS version 19.
Results
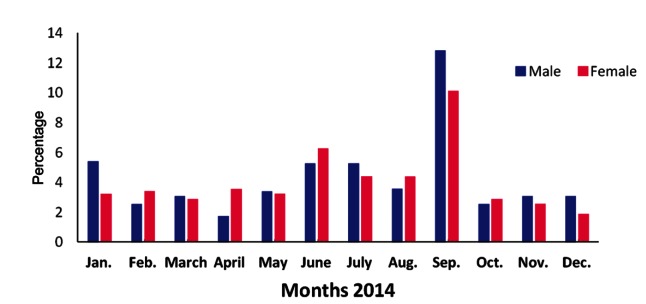
In 2014 a total of 13,352 children were admitted to Omdurman Paediatrics Hospital of which 9,157 were under 5years of age. 610 of these were admitted because of severe acute malnutrition this represent 4.6% of total hospital admissions and 6.7% of under-five admissions. 17 out of the 610 were excluded as per study protocol. The total of under-five children affected by acute severe malnutrition in 2014 was 593; of these 305 were males (51.4%), giving a male: female ratio of 1: 0.9 (Figure 1). The mean age of children admitted with acute severe malnutrition were 22.3 months. Children aged 36–59 months wereleast affected as shown in Table 1.
Figure 1.
Gender distribution of children less than 5-year-old admitted with malnutrition during the year 2014 to Omdurman Paediatric Hospital.
Table 1.
Distribution of children according to age group with protein-energy malnutrition admitted to Omdurman Paediatric Hospital during the year 2014
| Age group (month) | Frequency | Percent |
|---|---|---|
| 0–12 | 137 | 23.10 |
| 12–24 | 250 | 42.15 |
| 24–36 | 104 | 17.54 |
| 36–48 | 53 | 9.78 |
| 48–59 | 44 | 7.42 |
| Total | 593 | 100 |
During the study period the overall prevalence of severe malnutrition was 6.5%, and the general mortality rate at the hospital was 2.4%, while the mortality rate among the children with acute severe PEM was 9.3% (Figure 2).
Figure 2.
Prevalence and mortality rate among children less than 5-year-old admitted with malnutrition during 2014.
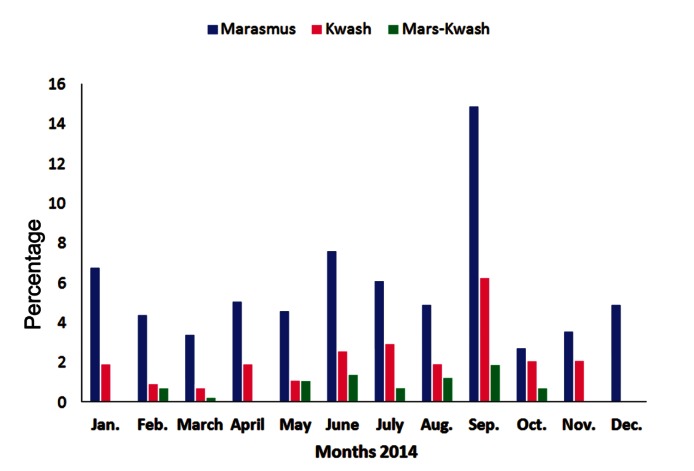
Among the 593 admitted children with severe malnutrition, 397(68.6%) had marasmus, 141(23.8%) had kwashiorkor and only 45 (7.6%) were marasmic-kwashiorkor (Figure 3).
Figure 3.
Distribution of different types of malnutrition among children less than 5-year-old during 2014.
Seasonal variations in the prevalence PEM among admitted children was observed with 52% in autumn (June – September). The most common clinical presentations among the under five children admitted with PEM during the year 2014 were gastroenteritis, malaria, urinary tract infection and Giardiasis. Regarding breast-feeding only 10.8% were exclusively breast fed for the first three months of life, 8.6% exclusive breast fed but the duration was not known. On the other hand, 0.8% was exclusively bottle fed, while 33.4% had mixed feed but the duration is not known as shown in Table 2.
Table 2.
Types and duration of feeding
| Type | Frequency | Percent |
|---|---|---|
| Exclusive breast feeding for three months | 64 | 10.79 |
| Exclusive breast feeding | 51 | 8.60 |
| Bottle feeding | 5 | 0.84 |
| Mixed feeding | 198 | 33.40 |
| No information | 275 | 46.37 |
| Total | 593 | 100 |
Fully vaccinated children represented only 33%, while 30% were not vaccinated and 18.6% were partially vaccinated and no data was available for 18% of the children (Table 3).
Table 3.
Vaccination status among children admitted with malnutrition during the year 2014
| Vaccination status | Frequency | Percent |
|---|---|---|
| Full vaccinated | 198 | 33.38 |
| Partially vaccinated | 110 | 18.55 |
| Not vaccinated | 285 | 48.07 |
| Total | 593 | 100 |
The majority (75.7%) of the study population recovered and were discharged from the hospital, while 15% were discharged against medical advice and 9.3% died as shown in Table 4.
Table 4.
Outcome of children admitted with malnutrition during the year 2014
| Status | Frequency | Percent |
|---|---|---|
| Improved and discharge | 449 | 75.72 |
| Discharged against medical advice | 89 | 15.01 |
| Died | 55 | 9.27 |
| Total | 593 | 100 |
Data about the socio-economic status of children’s family showed that 35.4% of the families were classified as low socio-economic class and 22.9% were classified as an average class family. No data was available to classify the rest of the cases (Table 5).
Table 5.
Socioeconomic status of children’s families
| Status | Number | Percent |
|---|---|---|
| Low | 210 | 35.41 |
| Average | 136 | 22.94 |
| Not mentioned | 247 | 41.65 |
| Total | 593 | 100 |
Discussion
This is a retrospective observational study; involving children less than 5 years of age admitted with malnutrition to Omdurman Paediatrics Hospital during the year 2014. Males and females were affected equally. These results are similar to the findings of Ubesie et al [4] and Cartmell et al [7] who reported a mean age of 21.7 months in under-five years old children admitted with PEM, while the mean age of the children in our study was 22.3 months. Two thirds (65%) of the affected children were younger than 24 months (Table 1). Two studies by Gernaat et al [5] and Nnakwe [6] reported similar findings. It is apparent that children under 2 years of age are the most affected age group. This could be due to a number of factors including low rate of exclusive breast feeding as documented in this study as well as poor weaning and feeding practices. Marasmus was the most common type of PEM noted in this study, affecting more than two thirds of the study population (66.9%). Similar results were reported by Gernaat et al [5]. Another study by Cartmell et al [7] reported kwashiorkor and marasmus as the most common types of PEM among admitted children in 1983, while the situation was changed to kwashiorkor and marasmic-kwashiorkor in 2001 in the same area.
The overall mortality in this study was 9.3%. Certainly this is a very high percentage although it seems low when compared with different studies conducted in various parts of Africa. In Oshogbo, South West Nigeria, Ibekwe and Ashworth [8] documented an average mortality rate of 22% over a five-year-period among 803 children admitted with PEM in a nutritional rehabilitation centre. Another hospital-based study in Zambia involving 288 children below 5 years of age reported an overall mortality rate of 25.8% [5]. The mean duration of length of hospital stay was 9 days, which was lower than that reported by Cartmell et al [7] and Ubesie et al [4] (13 and 16 days, respectively). The pressure on bed spaces in Omdurman Paediatric Hospital could have contributed to earlier discharges than in other hospitals. Although information about socioeconomic status were documented in only 346 cases in our study, still PEM was predominant among children from lower social class (35.4%). Similar high percentage was reported by Ubesie et al [4]. This may be due to the fact that poor families have low purchasing power for adequate nutritious food. Illiteracy may also influence feeding practices. Poverty and illiteracy as risk factors for PEM have been well documented in the literature. Nahar et al [9] found that severely underweight children are more likely to have undernourished poorly educated young mothers, short duration of predominant breastfeeding, and poorly educated unskilled fathers.
The commonest co-morbidities associated with PEM in this study were gastroenteritis, malaria, anaemia, urinary tract infections and giardiasis; similar to those reported in other studies [4].
Benefits of exclusive breastfeeding have been wildly acknowledged. They are known to promote sensory and cognitive development, and protect the infant against infectious and chronic diseases. Exclusive breastfeeding reduces infant mortality due to common childhood illnesses such as diarrhoea or pneumonia, and provide immunoglobulins which helps in a quicker recovery during illness. In the present study only 10.8% were exclusively breast fed for three months, 8.6% had exclusive breast feeding but for unknown duration, 0.8% were bottle fed, 33.4% had mixed feeding and no data was available in almost half of the children (46.4%).
There is a strong association between vaccination and malnutrition, as the role of vaccination in preventing contagious diseases cannot be over-emphasized. Lack of vaccination, fully or partially may be a predisposing factor for malnutrition as shown by a study in Uganda [10]. Lack of vaccination is linked to low socio-economic class, less education, and major family and social problems like divorce, unemployment or death of a parent…etc. In this study only 33% were fully vaccinated, 30% of children were not vaccinated, 18.6% were partially vaccinated and 18% had no available data regarding their vaccination history.
Conclusions
Our study showed a high prevalence of severe malnutrition among children less than 24 months of age. Seasonal variation in the prevalence of malnutrition among the under five-year-old children was noticed, with high prevalence in autumn (June to September) with increased mortality rate during this period. The predominant type of malnutrition among our cohort was marasmus.
We recommend adopting policies to promote exclusive breastfeeding for the first six months of life with continuation of breastfeeding in addition to complementary feeding for up to 24 months of life. Focusing on health education, access to locally available age-appropriate food, and improving water supply and sanitation systems and hygiene practices to protect children against communicable diseases, are the main recommendations of this study. We also recommend thorough review to identify reasons of the observed high mortality in Omdurman Paediatrics Hospital.
Refrences
- 1.World Health Organization. Report on malnutrition worldwide. WHO, Geneva: 2000 [Google Scholar]
- 2.UNICEF. Plan of operation in cooperation with Ethiopian government 1994. –1999.
- 3.Federal Ministry of Health. Central Bureau of Statistics and Unicef. The 2000 Sudan Multiple Indicator Cluster Survey, Sudan - Final Report. MICS 2000;2
- 4.Ubesie AC, Ibeziako NS, Ndiokwelu CI, Uzoka CM, Nwafor CA. Under-five protein energy malnutrition admittedat the University of Nigeria Teaching Hospital, Enugu: a 10 year retrospective review. Nutr J 2012; 11:43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gernaat HB, Dechering WH, Voorhoeve WH. Mortality in severe protein-energy malnutrition at Nchelenge, Zambia. J Trop Pediatr 1998; 44(4):211–217. [DOI] [PubMed] [Google Scholar]
- 6.Nnakwe N. The effect and causes of protein-energy malnutrition in Nigerian children. Nutr Res 1995; 15:785–794. [Google Scholar]
- 7.Cartmell E, Natalal H, Francois I, Ferreira MH, Grahnquist L. Nutritional andclinical status of children admitted to the malnutrition ward, MaputoCentral Hospital: A Comparison of data from 2001 and 1983. J Trop Pediatr 2005; 51(2):102–105. [DOI] [PubMed] [Google Scholar]
- 8.Ibekwe VE, Ashworth A. Management of protein energy malnutrition in Nigeria: an evaluation of the regimen at the Kersey Nutrition Rehabilitation Centre, Nigeria. Trans R Soc Trop Med Hyg 1994; 88:594–595. [DOI] [PubMed] [Google Scholar]
- 9.Nahar B, Ahmed T, Brown KH, Hossain MI. Risk factors associated with severe underweight among young children reporting to a diarrhoea treatment facility in Bangladesh. J health PopulNutr 2010; 28(5):476–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Owor M, Tumwine JK, Kikafunda JK. Socio-economic risk factors for severe protein energymalnutrition among children in Mulago Hospital, Kampala. East Afr Med J 2000;77(9): 471–475 [DOI] [PubMed] [Google Scholar]