Abstract
Background:
Brain metastasis during pregnancy is a rare occurrence. In particular, there have only been three prior cases regarding breast cancer metastasis. We report a patient with breast cancer metastasis to the brain during pregnancy and review the literature.
Case Description:
The patient was a 35-year-old female with a history of breast cancer (estrogen receptor/progesterone receptor negative, human epidermal growth factor receptor 2/neu positive, status post-neoadjuvant docetaxel/carboplatin/trastuzumab/pertuzumab therapy, status post-bilateral mastectomies), and prior right frontal brain metastases (status post-resection, capecitabine/lapatinib/temozolomide therapy, and cyberknife treatment). Patient was found to be pregnant at 9 weeks’ gestation while on chemotherapy; the patient elected to continue with the pregnancy and chemotherapy was discontinued. At 14 weeks’ gestation, she returned with recurrent right frontal disease. She was taken for a craniotomy at 16 weeks’ gestation, which confirmed metastases. Six weeks later, patient returned with worsening headaches and fatigue, with more recurrent right frontal disease. She was started on decadron and chemotherapy (5-fluorouracil, adriamycin, and cyclophosphamide). Serial magnetic resonance imaging (MRI) demonstrated enlarging right frontal lesions. She underwent a craniotomy at 27 weeks’ gestation, and chemotherapy was discontinued promptly. Starting at 30 weeks’ gestation, she received whole brain radiation for 2 weeks. Subsequently, she delivered a baby girl via cesarean section at 32 weeks’ gestation. At 6 weeks follow-up, an MRI brain demonstrated no new intracranial disease, with stable postoperative findings.
Conclusion:
There is a lack of guidelines and clinical consensus on medical and surgical treatment for breast cancer metastases in pregnant patients. Treatment usually varies based upon underlying tumor burden, location, gestational age of the fetus, and patient's preference and symptomatology.
Keywords: Brain metastases, brain surgery, breast cancer
BACKGROUND
Brain metastasis during pregnancy is a rare occurrence. In particular, there have only been three prior cases regarding breast cancer metastasis. Not surprisingly, pregnancy complicates the management of brain metastases. We report a patient with breast cancer metastasis to the brain during pregnancy and review the literature.
CASE PRESENTATION
The patient was a 35-year-old female who had a history of breast cancer (invasive ductal carcinoma of the left breast, estrogen receptor (ER)/progesterone (PR) negative, human epidermal growth factor receptor 2 (HER2)/neu positive, status post-neoadjuvant docetaxel/carboplatin/trastuzumab/pertuzumab therapy (TCH-P therapy), status post-bilateral mastectomies and left axillary lymph node dissection), with a prior right frontal brain metastases (status post-gross total resection, capecitabine/lapatinib/temozolomide therapy (TTX therapy), and cyberknife treatment). Patient was found pregnant at 9 weeks’ gestation; despite potential complications with the fetus during TTX therapy, patient elected to continue with the pregnancy; TTX therapy was discontinued. At 14 weeks’ gestation, she returned with headaches. Imaging showed recurrent right frontal dural-based lesion with significant surrounding vasogenic edema [Figure 1]. Magnetic resonance imaging (MRI) of the spine was negative. She was taken for a craniotomy at 16 weeks’ gestation, which again confirmed metastatic adenocarcinoma.
Figure 1.
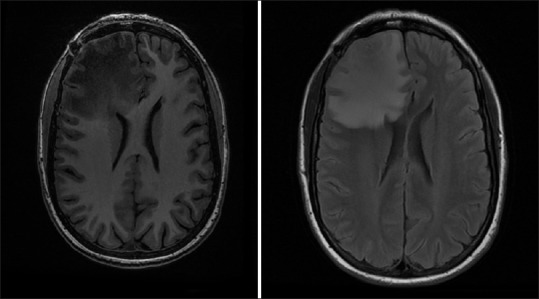
Axial magnetic resonance T1 (left) and fluid-attenuated inversion recovery demonstrates right frontal dural-based lesion
Six weeks later, patient returned with worsening headaches and fatigue. CT head showed recurring disease in the right frontal lobe [Figure 2a]. She was started on decadron and chemotherapy (5-fluorouracil, adriamycin, and cyclophosphamide). Serial MRI demonstrated enlarging right frontal lesions [Figure 2b and c]. She underwent a craniotomy at 27 weeks’ gestation, and chemotherapy was discontinued promptly. Starting at 30 weeks’ gestation, she received whole brain radiation (10 fractions, each at 3000 cGy) for 2 weeks. Subsequently, she delivered a baby girl via cesarean section at 32 weeks’ gestation; at the same time, patient had an elective bilateral tubal ligation. Overall, her pregnancy was complicated by intrauterine growth restriction, with estimated gestation weight at 6th percentile. She was getting weekly biophysical profiles/umbilical arterial Doppler which had been reassuring; in addition, she had a normal fetal echocardiogram at 20 weeks’ gestation. At 6 weeks follow-up, an MRI brain demonstrated no new intracranial disease, with stable postoperative findings [Figure 3].
Figure 2.
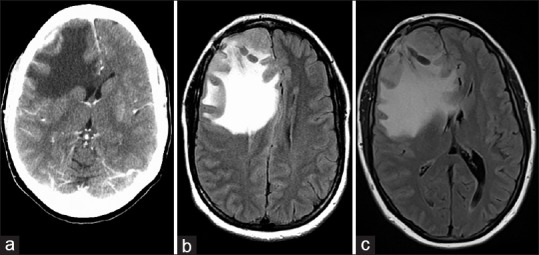
Axial computed tomography of the head (a), and serial fluid-attenuated inversion recovery (b, c) demonstrate progressive growth of recurrent right frontal lesion, with midline shift
Figure 3.
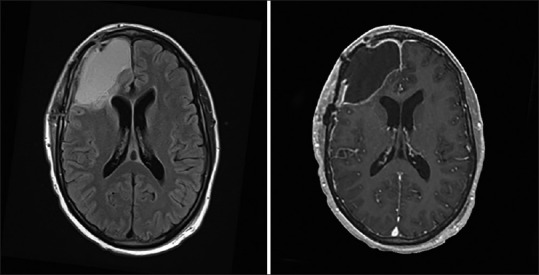
Axial magnetic resonance fluid-attenuated inversion recovery (left) and T1 with contrast demonstrate no residual or recurrent disease
DISCUSSION
The literature is limited regarding intracranial neoplasms during pregnancy. The estimated incidence is 15 per 100,000.[5,7] Common lesions include primary tumors, typically gliomas, pituitary adenoma, and meningiomas.[5,12,15] Brain metastasis during pregnancy is rather rare, where choriocarcinoma is the most common pathology.[5,13] Overall, the management of intracranial neoplasms can be challenging. Patients may opt for less aggressive treatment or to postpone treatment in order to decrease risk to the fetus while others may opt to terminate the pregnancy and proceed with full therapy. Future fertility may also be compromised, which remains an important consideration. Management needs to be tailored for each patient with interdisciplinary cooperation.
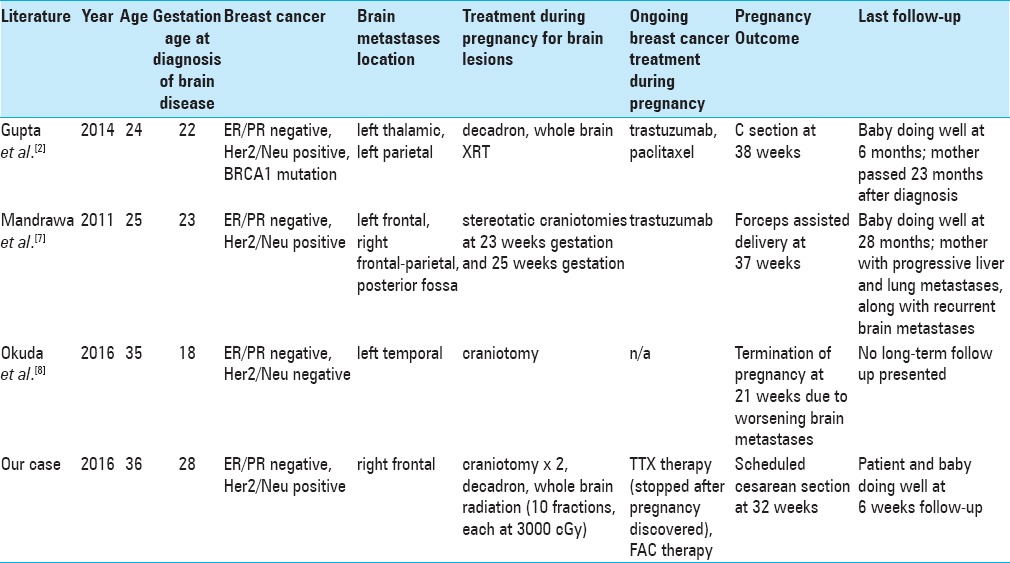
Breast cancer is the most common malignancy during pregnancy.[2] Of the reported cases, up to 3.8% exhibit metastatic disease.[5] Brain metastasis during pregnancy, however, has been rare and has only been reported in three other instances.[5,8,10] These are summarized in Table 1. Mandrawa et al.[8] reported the case of a 25-year-old female who underwent craniotomies at 23 weeks’ gestation and 25 weeks’ gestation for brain metastases; patient took ongoing trastuzumab; forceps-assisted delivery occurred at 37 weeks’ gestation; baby continued to do well up to 28 months follow-up. Gupta et al.[5] presented the case of a 24-year-old female, diagnosed with intracranial metastases at 22 weeks’ gestation, who received whole brain radiation and dexamethasone; patient underwent a cesarean section at 38 weeks; baby continued to do well at 6 months follow-up. Okuda et al.[10] noted a 35-year-old female who underwent a craniotomy for a metastases at 18 weeks’ gestation, however, symptoms worsened, necessitating a termination of pregnancy at 21 weeks’ gestation, followed by aggressive whole brain radiation and adjuvant chemotherapy.
Table 1.
Review of literature
Chemotherapy for the treatment of breast cancer during pregnancy appears to be well-tolerated by the fetus; a large series reported 104 cases where chemotherapy was given starting at a mean gestational age of 20.4 weeks; the malformation rate of exposed neonates was not significantly different than the general population.[2] Radiation to the brain may be feasible during pregnancy, if adjusted accordingly. Mazonakis et al.[9] demonstrated that, for an isocentric dose of 65 Gy, the radiation dose to the fetus does not exceed 100 mGy, a limit where risks toward the fetus are effectively marginalized.[14] According to a meta-analysis by Cohen-Kerem et al.,[4] non-obstetric surgery during pregnancy does not heighten the risk of birth defects, even during the first trimester. On the other hand, scant data exists regarding craniotomies for tumor resection.[3,6] The American College of Obstetrics and Gynecology endorses fetal ultrasound and Doppler before and after the procedure and states that known anesthesia has not been linked to teratogenic effects at any gestational age.[1] Overall, pregnancy-associated breast cancer is more advanced and aggressive at diagnosis than breast cancer during non-pregnancy; on the other hand, patients who become pregnant after breast cancer do not appear to have worse outcomes than patients who do not become pregnant.[11]
Our patient is the fourth case of breast cancer metastases to the brain. She was able to undergo two craniotomies, at 16 weeks’ gestation and at 27 week's gestation, without surgical complications. Her baby was delivered at 32 weeks’ gestation; though the patient exhibited low gestational weight, the patient exhibited no malformation.
CONCLUSION
There is a lack of guidelines and clinical consensus on medical and surgical treatment for breast cancer metastases in pregnant patients. Treatment usually varies based upon underlying tumor burden, location, gestational age of the fetus, and patient's preference and symptomatology. In this patient, our treatment rationale was based upon prolonging the gestational age and attempted gross total-resection of the metastases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Ashish Sharma, Email: ashishsharma@mcw.edu.
Ha Son Nguyen, Email: hsnguyen@mcw.edu.
Andrew Lozen, Email: alozen@mcw.edu.
Abhishiek Sharma, Email: absharma@mcw.edu.
Wade Mueller, Email: wmueller@mcw.edu.
REFERENCES
- 1.ACOG Committee on Obstetric Practice. ACOG Committee Opinion No.474: Nonobstetric Surgery During Pregnancy. Obstet Gynecol. 2011;117:420–1. doi: 10.1097/AOG.0b013e31820eede9. [DOI] [PubMed] [Google Scholar]
- 2.Cardonick E, Dougherty R, Grana G, Gilmandyar D, Ghaffar S, Usmani A. Breast cancer during pregnancy: Maternal and fetal outcomes. Cancer J. 2010;16:76–82. doi: 10.1097/PPO.0b013e3181ce46f9. [DOI] [PubMed] [Google Scholar]
- 3.Cohen-Gadol AA, Friedman JA, Friedman JD, Tubbs RS, Munis JR, Meyer FB. Neurosurgical management of intracranial lesions in the pregnant patient: A 36-year institutional experience and review of the literature. J Neurosurg. 2009;111:1150–7. doi: 10.3171/2009.3.JNS081160. [DOI] [PubMed] [Google Scholar]
- 4.Cohen-Kerem R, Railton C, Oren D, Lishner M, Koren G. Pregnancy outcome following non-obstetric surgical intervention. Am J Surg. 2005;190:467–73. doi: 10.1016/j.amjsurg.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 5.Gupta S, Jain P, McDunn S. Breast cancer with brain metastases in pregnancy. J Community Support Oncol. 2014;12:378–80. doi: 10.12788/jcso.0081. [DOI] [PubMed] [Google Scholar]
- 6.Johnson N, Sermer M, Lausman A, Maxwell C. Obstetric outcomes of women with intracranial neoplasms. Int J Gynaecol Obstet. 2009;105:56–9. doi: 10.1016/j.ijgo.2008.11.037. [DOI] [PubMed] [Google Scholar]
- 7.Lew PS, Tan WC, Tan WK, Tan HK. Dilemmas in management of brain tumours in pregnancy. Ann Acad Med. 2010;39:64–5. [PubMed] [Google Scholar]
- 8.Mandrawa CL, Stewart J, Fabinyi GC, Walker SP. A case study of trastuzumab treatment for metastatic breast cancer in pregnancy: Fetal risks and management of cerebral metastases. Aust N Z J Obstet Gynaecol. 2011;51:372–6. doi: 10.1111/j.1479-828X.2011.01314.x. [DOI] [PubMed] [Google Scholar]
- 9.Mazonakis M, Damilakis J, Theoharopoulos N, Varveris H, Gourtsoyiannis N. Brain radiotherapy during pregnancy: An analysis of conceptus dose using anthropomorphic phantoms. Br J Radiol. 1999;72:274–8. doi: 10.1259/bjr.72.855.10396218. [DOI] [PubMed] [Google Scholar]
- 10.Okuda T, Yamamoto S, Matsuo S, Kataoka H, Kitawaki J. Metastasis of Pregnancy-Associated Breast Cancer (Suspected to Be Hereditary Breast and Ovarian Cancer) to the Brain, Diagnosed at 18 Weeks’ Gestation: A Case Report and Review of the Literature. Case Rep Obstet Gynecol 2016. 2016:9813253. doi: 10.1155/2016/9813253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raphael J, Trudeau M, Chan K. Outcome of patients with pregnancy during or after breast cancer: A review of the recent literature. Curr Oncol. 2015;22(Suppl 1):S8–18. doi: 10.3747/co.22.2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ravindra VM, Braca JA, 3rd, Jensen RL, Duckworth EA. Management of intracranial pathology during pregnancy: Case example and review of management strategies. Surg Neurol Int. 2015;6:43. doi: 10.4103/2152-7806.153845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stevenson CB, Thompson RC. The clinical management of intracranial neoplasms in pregnancy. Clin Obstet Gynecol. 2005;48:24–37. doi: 10.1097/01.grf.0000153209.70749.d0. [DOI] [PubMed] [Google Scholar]
- 14.Stovall M, Blackwell CR, Cundiff J, Novack DH, Palta JR, Wagner LK, et al. Fetal dose from radiotherapy with photon beams: Report of AAPM Radiation Therapy Committee Task Group No.36. Med Phys. 1995;22:63–82. doi: 10.1118/1.597525. [DOI] [PubMed] [Google Scholar]
- 15.Verheecke M, Halaska MJ, Lok CA, Ottevanger PB, Fruscio R, Dahl-Steffensen K, et al. Primary brain tumours, meningiomas and brain metastases in pregnancy: Report on 27 cases and review of literature. Eur J Cancer. 2014;50:1462–71. doi: 10.1016/j.ejca.2014.02.018. [DOI] [PubMed] [Google Scholar]


