Abstract
Background
Late HIV diagnosis is associated with higher medical costs, early mortality among individuals, and HIV transmission in the population. Even under optimal configurations of stable or declining HIV incidence and increase in HIV case findings, no change in proportion of late HIV diagnosis is projected after year 2019. We investigated the association among social capital, gender, and late HIV diagnosis.
Methods
We conduct ecological analyses (ZIP code, N=166) using negative binomial regression of gender-specific rates of late HIV diagnoses (an AIDS defining illness or a CD4 count ≤200 cell/µL within 12 months of a new HIV diagnosis) in 2005 and 2006 obtained from the New York City HIV Surveillance Registry, and social capital indicators (civic engagement, political participation, social cohesion, and informal social control) from the New York Social Indicators Survey, 2004.
Results
Overall, low to high political participation and social cohesion corresponded with significant (p<.0001) decreasing trends in late HIV diagnosis rates. Among men (RR=0.66, 95% CI [0.47—0.98]) and women (RR=0.43, 95% CI [0.28—0.67]), highest political participation was associated with lower relative odds of late HIV diagnosis, independent of income inequality. Highest informal social control (RR=0.67, 95% CI [0.48—0.93]) among men only, and moderate social cohesion (RR=0.71, 95% CI [0.55—0.92]) among women only, were associated with the outcome adjusting for social fragmentation, income inequality, and racial composition.
Discussion
The magnitude of association between social capital and late HIV diagnosis varies by gender and by social capital indicator.
Keywords: Social capital, late HIV diagnosis, social cohesion, income inequality, gender
INTRODUCTION
HIV diagnosis in the advanced stages of AIDS (i.e., late HIV diagnosis) is associated with higher medical costs, lower life expectancy, and early mortality among individuals.1–5 Late HIV diagnosis is associated with HIV transmission in the population,3,6,7 partly through higher community viral load and increased infectivity among persons unaware of their HIV status.8–10 One study estimated that even under optimal configurations of stable or declining HIV incidence and increase in HIV case findings, the proportion of late HIV diagnosis would remain unchanged from year 2019 into 2040.11
In addition to social determinants at the individual level including unemployment and low income with HIV diagnosis,12 analogues of those determinants at the contextual (i.e., neighborhood-level) such as income inequality and socioeconomic deprivation are associated with HIV outcomes,13,14 separately from and in addition to the role played by individual behavior.15–17 This area of research remains, however, underdeveloped and little is known about the contextual social determinants associated with lower late HIV diagnosis rates in the population.
Social capital is one contextual factor associated with HIV-related outcomes that include HIV stigma, unprotected sexual intercourse, and HIV medication adherence18–20 across different population and geographic settings. Neighborhood social capital is defined as the resources embedded within the neighborhood that residents can draw on for mutual benefit.21–23 Social capital is a multi-dimensional construct tapped by several indicators that include trust and reciprocity, neighborhood organization participation, and collective action among residents.24 These various social capital indicators have been shown to have unique, overlapping, and even non-significant associations with health.25,26 Moreover, while there have been some studies that investigated the relationship between social capital and HIV outcomes at the individual level (for example, care engagement),27 there is limited research about the ecological relationship between social capital and HIV-related outcomes.
Social capital in this study was operationalized by four indicators: civic participation, political participation, social cohesion, and informal social control. Civic participation is defined as membership in civic, community or religious organizations.28 Higher civic participation can facilitate stronger advocacy for HIV prevention resources such as HIV testing accessibility. Participation can also foster connectedness among individuals, which can increase availability of resources that increase individuals’ likelihood of timely HIV testing—one aspect of late HIV diagnosis prevention.
Political participation is defined as the extent of individual’s involvement in political processes, which include registering to vote and identifying with a political party.29 Higher political participation can drive lobbying for HIV prevention resources and is more likely to yield fruitful government responses to petitions that seek to improve health, stability and social conditions within neighborhoods.30 Social cohesion is the aggregate of residents’ perceptions of trust and shared values.31,32
Trust can promote sharing and receiving information, for instance, on where to receive an HIV test. Additionally, persons at risk or infected may be more likely to test for HIV within their neighborhood if they perceive it as safe. Informal social control is the degree to which persons take ownership of their neighborhood and share expectations for reducing disorder and deviance.32 Higher social control can mitigate the effects of physical and social characteristics (e.g., alcohol outlets and assaults33) associated with disorder and increase HIV risk.34 For instance, alcohol outlets are associated with HIV risk through a moderating role on individual consumption and high risk sexual behavior as well as facilitating social networks that attract high risk groups and increase high risk behaviors.13,35
In addition to theorized ways in which those indicators can affect HIV risk, empirically; higher social capital was shown to be associated with lower HIV risk among individuals through facilitating increased condom use,36 HIV testing,37 HIV disclosure,38 and reduced multiple sex-partnering.39 Pathways at the ecological level19,40 include reduced HIV stigma and discrimination,37 increased availability of information sharing resources41 such as education for those at risk, and increase economic and social support for those at risk and already infected with HIV.42
Gender moderates the association between social capital and HIV outcomes. The distribution, nature, and way social capital is used is imbued with gender inequalities, which affects the accumulation and investments of capital.43 For example, one study in Britain showed that civic participation among men was related to sports and recreation participation while for women, civic participation was related to greater use of health and social services.44 Inequalities among women are perpetuated when social capital indicators, for example, civic participation, are based on questions with responses limited to activities overrepresented by men. Therefore, women’s lack of interest in those activities may be mistaken for low social capital.43
Social capital is eroded by social fragmentation and income inequality within neighborhood,45 which may weaken any association with late HIV diagnosis. Social fragmentation is defined as disintegration in bonds among people within a neighborhood and is an indication of rapid population turnover and residential instability.46–48 Income inequality widens social distances between persons with high and low socioeconomic status and socially isolate individuals.49 In our other research (Ransome Y, Kawachi I, Braunstein SL, et al. Area-level income inequality is associated with late HIV diagnosis: Intervening roles of HIV testing and accessibility, unpublished data, November 2015), we found that higher income inequality was associated with higher rates of late HIV diagnosis. Racial composition is postulated to affect the association between social capital and health, 50, between income inequality and health,51 and may indirectly affect late HIV diagnosis.
We therefore investigated: (1) the association between social capital and late HIV diagnosis, (2) the extent to which social capital and late HIV diagnosis varies by gender, and (3) whether any protective association between social capital and late HIV diagnosis remain after adjusting for social fragmentation, income inequality, and racial composition.
METHODS
Data on aggregate-ZIP code level gender-specific counts of HIV diagnosis among individuals during 2005 and 2006 were received from the NYC Department of Health and Mental Hygiene’s (DOHMH) HIV surveillance, which is a population-based registry of all persons diagnosed with HIV infection since 2000 or AIDS since 1981 who meet the Centers for Disease Control (CDC) case definitions for surveillance and were reported to the NYC DOHMH.52 We aggregated individual counts of HIV diagnoses (n=2199) across 166 of 176 residential New York City (NYC) ZIP codes with complete data on the exposures and outcome. We chose the ZIP codes as the unit of analysis because ZIP codes have been shown to approximate NYC neighborhoods well, particularly in relation to social capital.53 Moreover, ZIP codes have been shown to explain variation in health among individuals and neighborhoods in NYC.54,55
Measures
Outcome variable
We used the CDC’s definition of late HIV diagnosis: a CD4 count of 200 cells/ml or less, or an AIDS defining illness within 12 months of the date of HIV diagnosis.56 We classified the proportion of persons diagnosed late, among all HIV diagnoses. We combined data for 2005 and 2006 to improve the stability within ZIP codes with small numbers of events.
Social capital indicators
Civic engagement, political participation, social cohesion, and informal social control indicators were the only social capital variables in the New York Social Indicators Survey (NY SIS), Wave 4 conducted in 2004. NY SIS is a population representative telephone-based survey of approximately 1900 New York City residents designed to document individual and family well-being across economic, social, and behavioral indicators, as well as the perception of the City and services.57 The variables were created in two steps. First, for civic engagement—a binary variable; we performed tetrachoric correlation analysis, extracted the correlation matrix and then performed iterated principal factor analysis on the matrix,58 which produced a one factor solution. For political participation, we created a binary variable 0 “does not identify with a political party” and 1 “identifies with a political party”. We then took the sum of that party affiliation measure and a binary variable from the question “are you currently registered to vote” 0 “no”, 1”yes”, and derived a multinomial variable of 0, “neither identify with a party or registered to vote”, 1 “either identify with a party or registered to vote, and 2 “both identify with a party and registered to vote”.
For continuous measures social cohesion and informal social control, we performed principal components analyses (PCA), which produced a one factor solution for each outcome, and we retrieved the predicted scores. In the second step, we used weighted least squares53 and multinomial regression, as appropriate with recommended social capital predictors:31 age, gender, marital status, education, home ownership, years of residence, and ratings of one’s neighborhood. Then, we obtained empirical Bayes predicted scores from the regressions and aggregated those across ZIP codes.
Social fragmentation
We identified indicators from the literature46,59 and obtained those from the Census 2000 summary files 1 100% for NYC ZIP codes. The list of indicators included: % female headed households; housing tenure percent; % vacant units for rent; % vacant housing units; housing tenure rental vacancy rate; % 15 years and older separated; % 15 years and older divorced; % with a disability; % foreign born; % of the population who resided elsewhere 5 years ago; % in different house in different county 5 years ago; and % different house in different state 5 years ago. Consistent with prior studies,60,61 we performed PCA on the indicators and chose, among two factors, the one with highest Cronbach’s alpha α=0.51. That factor included: % vacant housing units, housing tenure rental vacancy rate, % foreign-born, and % of the population who resided elsewhere 5 years ago. A higher social fragmentation score reflects greater fragmentation within ZIP codes.
Income inequality
We used the GINI coefficient, which indicates household income distribution.62 The GINI coefficient ranges from 0 to 1, where 0 indicates perfect equality and 1 indicates perfect inequality. Further information on the calculation of the GINI at the ZIP code level for NYC is available elsewhere.
Racial composition
The measure is the proportion of non-Hispanic black residents within each ZIP code, derived from Census 2000 summary files 1 100%.
Statistical Analyses
We first performed correlation analysis among all variables. Given the high correlation among the social capital indicators, we produced a set of orthogonal indicators using the “orthog” STATA command,63 which reduces collinearity effects in multivariate regression. We tested for trends in late HIV diagnosis rates across the indicators. In regression models, we examined the crude associations among social capital indicators and late HIV diagnosis using negative binomial regression with Census 2000 population as the offset variable.64 We then tested for an interaction with gender and the social capital indicators predicting the outcome and found borderline (p=.06) significance for civic engagement and significance (p<.05) for political participation, and informal social control.
Based on theory and those results, we stratified all analyses by gender. We then examined the crude association among social fragmentation, income inequality, and racial composition with the outcome. We constructed multiple regression models by adding social fragmentation to the model, then income inequality and racial composition, and then all covariates. We classified social capital indicators, social fragmentation, and income inequality into “low”, “moderate”, and “high” to account for non-linearity with the outcome. In all analyses, “low” is the reference category. Relative Risks (RR) are reported but interpreted as relative odds throughout the text.
RESULTS
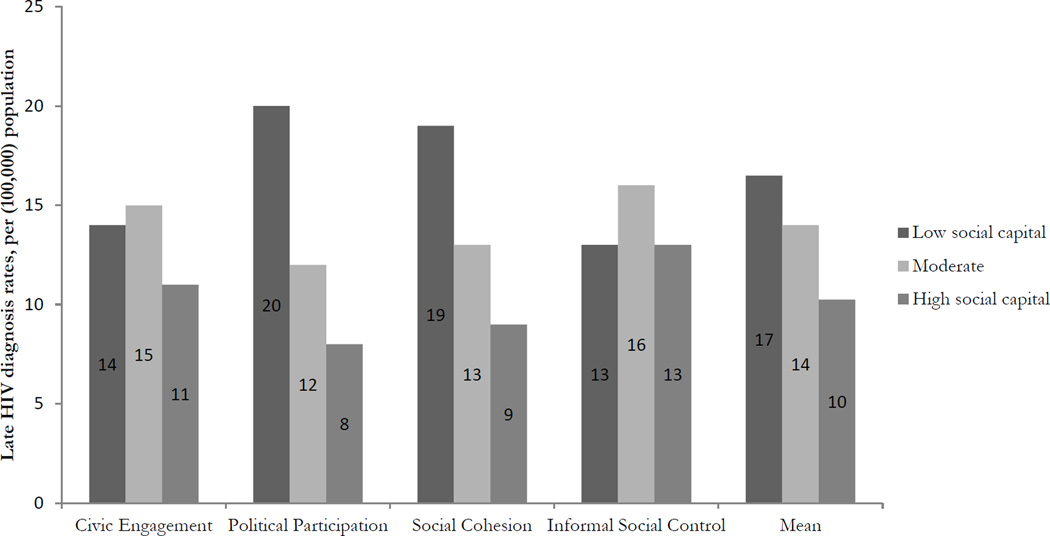
Table 1 shows results of the correlation analysis. The strongest positive correlation was between social cohesion and informal social control (r=0.94) and strongest negative correlation was between social cohesion and social fragmentation (r=−0.74). Figure 1 shows a strong decreasing gradient in late HIV diagnosis rates across low to high levels of civic participation, social cohesion, and mean of overall social capital within NYC neighborhood (p-trend <.001), Table 2 contains the items that were used in the social capital indicators and the distribution at the ZIP code level.
Table 1.
Pearson product moment correlation coefficients among study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
|---|---|---|---|---|---|---|---|---|---|
| 1 | Civic engagement | 1.00 | |||||||
| 2 | Political participation | 0.39*** | 1.00 | ||||||
| 3 | Social cohesion | 0.52*** | 0.71*** | 1.00 | |||||
| 4 | Informal social control | 0.49*** | 0.68*** | 0.94*** | 1.00 | ||||
| 5 | Social fragmentation | −0.27*** | −0.58*** | −0.74*** | −0.66*** | 1.00 | |||
| 6 | Income inequality | −0.35*** | −0.23*** | −0.41*** | −0.45*** | 0.50*** | 1.00 | ||
| 7 | % Black in ZIP code | 0.19** | −0.49*** | −0.40*** | −0.22*** | 0.59*** | 0.13* | 1.00 | |
| 8 | Late HIV diagnosis rate | −0.04 | −0.28*** | −0.37*** | −0.34*** | 0.50*** | 0.35*** | 0.34*** | |
p<.05,
p<.01,
p<.0001.
Note: Higher scores correspond to higher social capital (civic engagement, political participation, social cohesion, and informal social control), higher social fragmentation, greater proportion of Black residents in a ZIP code, and higher income inequality.
Figure 1.
Association between social capital (indicators and overall mean), and late HIV diagnosis rates
Table 2.
Mean for social capital items at the individual level and median and inter-quartile ranges (IQR) in relation with empirical Bayes estimates computed at the neighborhood level
| Statement | Response options |
aMean (SE) or Percent (SE) |
bMedian (IQR) |
|---|---|---|---|
| Civic engagement | 0.09 (0.07 – 0.11) | ||
| Over the past year, have you contacted a local elected official about some need or problem? |
1 "yes" 0 "no" | 12.7 (1.04) | |
| Are you a member of a neighborhood or community organization? |
Idem | 16.2 (1.26) | |
| Are you a member of a Parent/Teacher Association? |
Idem | 10.9 (0.81) | |
| Are you a member of a civic association (e.g., League of Women Voters, Junior League)? |
Idem | 4.9 (0.68) | |
| Are you a member of any other organization that provides services to the community? |
Idem | 15.8 (1.22) | |
| How often do you attend religious services- almost every week or more, once or twice a month, a few times a year, or less often than that? |
1 "attend almost every week or more or once or twice a month" 0 "a few times a year or less often than that" |
48.5 (1.78) | |
| Political participation | 0.21 (0.15 – 0.29) | ||
| Are you currently registered to vote? | 1 "yes" 0 "no" | 71.2 (1.82) | |
| Generally speaking, do you usually think of yourself as a Republican, Democrat, Independent, or what? |
1 "identified with a political party" 0 "no preference or does not identify with a party" |
29.0 (1.63) | |
| Social cohesionc | 0.09 (−0.30 – 0.41) | ||
| How strongly do you agree or disagree with the following statements… People around here are willing to help their neighbors? |
1 "strongly agree" 2 "somewhat agree" 3 "somewhat disagree" 4 " strongly disagree" |
1.9 (0.03) | |
| How strongly do you agree or disagree with the following statements… This is a close-knit neighborhood? |
Idem | 2.2 (0.03) | |
| How strongly do you agree or disagree with the following statements… People in this neighborhood can be trusted? |
Idem | 2.2 (0.04) | |
| Informal social controlc | 0.04 (−0.32 – 0.28) | ||
| If children were skipping school and hanging out on a street corner, would your neighbors be….to intervene? |
Idem1 "very likely" 2 "somewhat likely" 3 "somewhat unlikely" 4 "very unlikely" |
2.5 (0.04) | |
| If children were spray-painting graffiti on a local building, would your neighbors be…to intervene? |
Idem | 1.95 (0.04) | |
| If children were showing disrespect to an adult, would your neighbors be…to intervene? |
Idem | 2.30 (0.04) | |
| If a fight broke out in front of their house, would your neighbors be…to intervene? |
Idem | 2.05 (0.04) | |
Note.
Mean and percent are weighted, and SE=standard error is adjusted for survey weighted analysis among individuals (n=1470).
=based on empirical Bayes predicted estimates mean aggregated ZIP codes (n=166).
=Variables were reverse coded to create neighborhood level analogues so that higher scores indicated higher social capital.
Results among men are found in table 3. In crude analyses, highest political participation (RR=0.48, 95% CI [0.35—0.66]) and social cohesion (RR=0.58, 95% CI [0.43—0.79]) had significantly lower relative odds of late HIV diagnosis (Model 1). Social fragmentation, income inequality, and racial composition each were associated with higher relative odds of late HIV diagnosis rates. In multivariate regression analyses, social fragmentation attenuated the protective association that political participation and social cohesion had with late HIV diagnosis rates (Model 2).
Table 3.
Adjusted associations between social capital and late HIV diagnosis, among men
| Model 1 RR (95 % CI) |
Model 2 RR (95 % CI) |
Model 3 RR (95 % CI) |
Model 4 RR (95 % CI) |
||
|---|---|---|---|---|---|
| Men | n | ||||
| Civic Engagement | |||||
| Low (0.04 to 0.65) | 56 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| Moderate (0.08 to 0.09) | 56 | 1.12 (0.84—1.49) | 1.24 (0.94—1.65) | 1.18 (0.90—1.55) | 1.24 (0.95—1.64) |
| High (0.11 to 0.13) | 54 | 1.10 (0.81—1.50) | 1.33 (0.99—1.81) | 1.25 (0.93—1.69) | 1.38 (1.01—1.89)* |
| Political Participation | |||||
| Low (0.12 to 0.15) | 56 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| Moderate (0.19 to 0.26) | 56 | 0.69 (0.52—0.93)* | 0.82 (0.61—1.11) | 0.84 (0.63—1.13) | 0.85 (0.63—1.16) |
| High (0.30 to 0.35) | 54 | 0.48 (0.35—0.66)*** | 0.78 (0.54—1.11) | 0.66 (0.47—0.98)* | 0.75 (0.51—1.10) |
| Social Cohesion | |||||
| Low (−0.62 to −0.30) | 56 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| Moderate (−0.02 to 0.25) | 56 | 0.75 (0.56—1.01) | 0.84 (0.63—1.11) | 0.92 (0.70—1.20) | 0.93 (0.71—1.21) |
| High (0.41 to 0.70) | 54 | 0.58 (0.43—0.79)** | 0.85 (0.61—1.19) | 0.80 (0.60—1.08) | 0.91 (0.66—1.24) |
| Informal Social Control | |||||
| Low (−0.54 to −0.31) | 56 | 1.00 (Ref) | 1.00 (Ref)* | 1.00 (Ref) | 1.00 (Ref) |
| Moderate (−0.062 to 0.12) |
55 | 0.96 (0.71—1.29) | 0.81 (0.59–1.07) | 0.90 (0.68—1.18) | 0.84 (0.64—1.11) |
| High (0.28 to 0.50) | 55 | 0.75 (0.55—1.02) | 0.60 (0.44—0.82)** | 0.70 (0.50—0.97)* | 0.67 (0.48—0.93)* |
| Social Fragmentation | |||||
| Low (−2.38 to −1.39) | 54 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | |
| Moderate (−0.80 to 0.03) | 56 | 1.44 (1.06—1.97)* | 1.49 (1.07—2.05)* | 1.21 (0.88—1.67) | |
| High (1.73 to 3.64) | 56 | 2.71 (2.01—3.64)*** | 2.69 (1.77—4.09)*** | 1.62 (1.02—2.56)* | |
| Income Inequalitya | |||||
| Low (0.37 to 0.39) | 53 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | |
| Moderate (0.41 to 0.42) | 59 | 1.97 (1.48—2.64)*** | 1.79 (1.32—2.42)*** | 1.68 (1.24–2.28)** | |
| High (0.44 to 0.46) | 54 | 2.63 (1.95—3.54)*** | 2.43 (1.77—3.34)*** | 2.17 (1.55—3.03)*** | |
| Racial Compositiona | |||||
| % Black in ZIP code (3.0 to 3.6) |
2.57 (1.65—3.99)*** | 2.06 (1.07—3.97)*** | 1.53 (0.75—3.12) |
Model 1: Crude association of social capital indicators (civic engagement, political participation, social cohesion, and informal social control). Social capital variables are orthogonalized to reduce co-linearity in regression analyses.
Income inequality is adjusted for racial composition and vice versa.
Model 2: Social capital indicators (civic engagement, political participation, social cohesion, and informal social control) adjusted for social fragmentation.
Model 3: Social capital indicators (civic engagement, political participation, c social cohesion, and informal social control) adjusted for income inequality and racial composition.
Model 4: Social capital indicators (civic engagement, political participation, social cohesion, and informal social control) adjusted for social fragmentation, income inequality, and racial composition.
Abbreviations: RR= Relative Risk; CI= Confidence Interval.
p<.05,
p<.01,
p<.001.
Interquartile ranges of the predictors and covariates are in parentheses.
However, highest level of informal social control emerged as a significant predictor of lower relative odds of late HIV diagnosis rates (RR=0.60, 95% CI [0.44—0.82]). In Model 3, income inequality partially and fully attenuated the association of political participation and social cohesion, respectively with the outcome. However, highest informal social control was independently associated with lower late HIV diagnosis rates (RR=0.70, 95% CI [0.50—0.97]). Adjusting simultaneously for all covariates did not eliminate the protective association between highest levels of informal social control and late HIV diagnosis rates (Model 4). Higher levels of income inequality were associated with higher relative odds of late HIV diagnosis in all models. In the fully adjusted model, highest level of civic engagement was associated with increased, but marginally significant, relative odds of late HIV diagnosis rates (RR=1.38, 95% CI [1.01—1.89]).
Results among women are found in table 4. All social capital indicators in crude analysis were associated with lower late HIV diagnosis rates except informal social control, which was associated with increased relative odds in the outcome. In multiple regression analyses adjusting for social fragmentation; civic engagement and informal social control were no longer independently associated with late HIV diagnosis rates (Model 2). However, both moderate (RR=0.69, 95% CI [0.52—0.93]) and highest levels (RR=0.44, 95% CI [0.29—0.68]) of political participation were associated with lower relative odds of late HIV diagnosis rates (Model 2). Only moderate level of social cohesion was associated with lower relative odds of the outcome (RR=0.64, 95% CI [0.49—0.85]). Higher social fragmentation was associated with higher relative odds of late HIV diagnosis rates. Adjusting for income inequality and racial composition attenuated only the association between moderate levels of political participation and late HIV diagnosis rates. Highest level of political participation (RR=0.43, 95% CI [0.28—0.67]) and both moderate (RR=0.70, 95% CI [0.53—0.92]) and highest (RR=0.65, 95% CI [0.47—0.91]) levels of social cohesion were independently associated with lower relative odds of late HIV diagnosis rates (Model 3). Interestingly, civic engagement emerged as a significant predictor or lower relative odds of late HIV diagnosis rates (RR=0.74, and RR=0.66, p<.05 respectively). Adjusting simultaneously for all covariates fully attenuated the association of all social capital variables on the outcome (Model 4).
Table 4.
Adjusted associations between social capital and late HIV diagnosis, among women
| Model 1 RR (95 % CI) |
Model 2 RR (95 % CI) |
Model 3 RR (95 % CI) |
Model 4 RR (95 % CI) |
||
|---|---|---|---|---|---|
| Women | n | ||||
| Civic Engagement | |||||
| Low (0.04 to 0.65) | 56 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| Moderate (0.08 to 0.09) | 56 | 0.82 (0.59—1.14) | 0.94 (0.72—1.35) | 0.74 (0.56—0.99)* | 0.83 (0.63—1.10) |
| High (0.11 to 0.13) | 54 | 0.63 (0.44—0.89)** | 0.84 (0.61—1.79) | 0.66 (0.47—0.93)* | 0.82 (0.58—1.11) |
| Political Participation | |||||
| Low (0.12 to 0.15) | 56 | 1.00 (Ref) | 1.00 (Ref)* | 1.00 (Ref)* | 1.00 (Ref) |
| Moderate (0.19 to 0.26) | 56 | 0.56 (0.41—0.77)*** | 0.69 (0.52—0.93)** | 0.80 (0.60—1.07) | 0.85 (0.64—1.12) |
| High (0.30 to 0.35) | 54 | 0.21 (0.15—0.32)*** | 0.44 (0.29—0.68)*** | 0.43 (0.28–0.67)*** | 0.59 (0.38—0.91)* |
| Social Cohesion | |||||
| Low (−0.62 to −0.30) | 56 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| Moderate (−0.02 to 0.25) |
56 | 0.59 (0.43—0.82)*** | 0.64 (0.49—0.85)** | 0.70 (0.53—0.92)* | 0.71 (0.55— 0.92)** |
| High (0.41 to 0.70) | 54 | 0.43 (0.30—0.92)*** | 0.74 (0.51—1.07) | 0.65 (0.47—0.91)* | 0.85 (0.60—1.20) |
| Informal Social Control | |||||
| Low (−0.54 to −0.31) | 56 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| Moderate (−0.062 to 0.12) |
55 | 1.33 (0.94—1.88) | 0.98 (0.72—1.35) | 0.98 (0.73—1.34) | 0.88 (0.67—1.19) |
| High (0.28 to 0.50) | 55 | 1.59 (1.10—2.27)** | 1.15 (0.83—1.61) | 0.99 (0.69—1.42) | 0.91 (0.65—1.27) |
| Social Fragmentation | |||||
| Low (−2.38 to −1.39) | 54 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | |
| Moderate (−0.80 to 0.03) |
56 | 2.51 (1.59—3.93)*** | 2.27 (1.44—3.58)*** | 1.68 (1.07—2.64)* | |
| High (1.73 to 3.64) | 56 | 8.35 (5.50—12.68)*** | 4.96 (2.98—8.25)*** | 2.93 (1.73— 4.96)*** |
|
| Income Inequalitya | |||||
| Low (0.37 to 0.39) | 53 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | |
| Moderate (0.41 to 0.42) | 59 | 2.43 (1.64—3.60)*** | 1.94 (1.32—2.85)** | 1.68 (1.15— 2.44)** |
|
| High (0.44 to 0.46) | 54 | 3.25 (2.22—4.76)*** | 2.36 (1.61—3.45)*** | 1.87 (1.29— 2.74)** |
|
| Racial Compositiona | |||||
| % Black in ZIP code (3.0 to 3.6) |
10.19 (6.10— 17.02)*** |
5.41 (2.80—10.46)*** | 3.31 (1.74— 6.29)** |
Model 1: Crude association of social capital indicators (civic engagement, political participation, social cohesion, and informal social control). Social capital variables are orthogonalized to reduce co-linearity in regression analyses.
Income inequality is adjusted for racial composition and vice versa.
Model 2: Social capital indicators (civic engagement, political participation, social cohesion, and informal social control) adjusted for social fragmentation.
Model 3: Social capital indicators (civic engagement, political participation, social cohesion, and informal social control) adjusted for income inequality and racial composition.
Model 4: Social capital indicators (civic engagement, political participation, social cohesion, and informal social control) adjusted for social fragmentation, income inequality, and racial composition.
Abbreviations: RR= Relative Risk; CI= Confidence Interval.
p<.05,
p<.01,
p<.001.
Interquartile ranges of the predictors and covariates are in parentheses.
DISCUSSION
We found that the robustness and direction of association among social capital indicators and late HIV diagnosis had threshold effects and varied by gender. For example, in fully adjusted models, only the highest levels of informal social control had a protective association on late HIV diagnosis among men, whereas among women, only the highest level of political participation and moderate levels of social cohesion was protective.
Our finding that associations between social capital and health outcomes remain after adjustment for indicators of social fragmentation and economic inequality is consistent with other studies.61,65–67 Our finding that from crude to adjusted models, only the highest level of informal social control and political participation remained associated with the outcome suggests that income inequality and social fragmentation may confound the relationship by both eroding social capital32,45 and delaying HIV diagnoses.
The moderating role of gender on social capital indicators associated with late HIV diagnosis in our study is consistent with another study that examined social capital and HIV prevalence.18 The association between civic engagement and higher relative risk of late HIV diagnosis among men could plausibly be attributed to men’s civic engagement, such as participation in sports and leisure, which are different than women.44 In some civic participation environments, men may be more likely to participate in risk behaviors, which can affect HIV risk. For instance, one study showed that men were more likely than women to participate in “storkvels”—a savings club where people meet regularly, contribute money and take turns with yielding the contribution. Participating in storkvels was associated with higher HIV risk among men, which was mediated by alcohol consumption.68
Women have higher levels of political participation than men,69 which could account for why the protective association with late HIV diagnosis was only found among them. One study found that perceived reciprocity—one aspect of social cohesion— was more strongly correlated with lower mortality among middle aged women than men.70 Women are more affected by inequalities that are associated with HIV infection,71 therefore, may be more likely to engage in social cohesion and more efficaciously utilize political will to take action on these issues. For example, women generally have higher HIV testing rates than men, above the fact HIV tests are routine part of prenatal care.72
The following are limitations of our study. We had complete social capital data for 94% (166/176) of residential ZIP codes. The 6 % of ZIP codes not available had statistically lower late HIV diagnoses rates, proportion of persons with less than a high school diploma, and higher median income than ZIP codes. However, there were non-significant differences in other socio-economic demographics including: workforce participation, poverty level, proportion of black residents and population 20 to 50 years of age. Since the social capital indicators were compositional aggregates, weighted for census population and adjusted for individual covariates including socioeconomic status; any likely bias on the outcome is therefore minimal.
The NY SIS 2004 data from which the social capital indicators were derived achieved a 17% response rate. While this rate is low for household survey data, there were no other comprehensive comparable social capital data available for NYC for the study period; therefore, we are unable to determine the magnitude or direction of bias this could potentially have on the outcome. While we theorized on potential pathways between social capital and late HIV diagnosis rates, we did not have data to examine etiological pathways or competing theories,73,74 which are critiques of social capital research.75 Although social capital was temporal to late HIV diagnosis, data nevertheless were cross-sectional, thus limits causal inference. Lastly, our social capital indicators do not tell us about quality of social capital,76 or whether sources of social capital differs across organizations, and subpopulations,77 which plausibly can affect the findings.
The study has several strengths and contributes to the debate on diversity between social capital and health.78 We show that social capital is associated with another diverse health outcome—late HIV diagnosis, and in a diverse location than previously studied. This study overcomes one key critique about the lack of incorporating the multidimensionality of social capital when studying health.79 Specifically, we theorized on how multiple indicators potentially operate and subsequently tested those associations with the outcome. Although additional studies are needed, we show that the associations between social capital and late HIV diagnosis varies by gender. Our findings are consistent with other studies that found gender differences in the association between social capital and HIV outcomes, including HIV incidence.18,80 Next, we used several population-based data sources, which improve generalizability of findings to the NYC population.
Our study lays the foundation for more vigorous research on the social capital and HIV-related outcomes. Although several mediating pathways have been proposed to link social capital with health and with HIV outcomes, there is dearth of empirical work on the topic. We recommend additional research into the association between social capital and hypothesized mediators such as HIV testing, and as well as associations with other HIV-related outcomes including linkage to HIV care and engagement in HIV care.
Acknowledgments
Source of Funding: Y. Ransome is an Alonzo Smythe Yerby Postdoctoral Fellow in the Harvard T.H. Chan School of Public Health. D. Nash is currently receiving a grant (#1R01MH101028-01) from the National Institutes of Health.
Footnotes
Conflicts of Interest: For the remaining authors none were declared.
Contributor Information
Yusuf Ransome, Department of Social and Behavioral Sciences, Harvard T. H. Chan School of Public Health, 677 Huntington Avenue, 7th Floor, Boston MA, 02215, Tel: 617-384-8814, Fax: 617-384-8859, yransome@hsph.harvard.edu.
Sandro Galea, School of Public Health, Boston University, 715 Albany Street - Talbot 301, Boston, MA 02118.
Roman Pabayo, Community Health Sciences, University of Nevada School, 1644 North Virginia Street, Reno, NV 89557.
Ichiro Kawachi, Department of Social and Behavioral Sciences, Harvard T. H. Chan School of Public Health, 677 Huntington Avenue, 7th Floor, Boston, MA 02215.
Sarah Braunstein, HIV Epidemiology and Field Services Program, New York City Department of Health and Mental Hygiene, 42-09 28th Street, Long Island City, NY 11101.
Denis Nash, Graduate School of Public Health and Health Policy, City University of New York 365 5th Avenue, 3rd Floor New York, NY 10016.
References
- 1.Farnham PG, Gopalappa C, Sansom SL, et al. Updates of lifetime costs of care and quality-of-life estimates for HIV-infected persons in the United States: Late versus early diagnosis and entry into care. J Acquir Immune Defic Synd. 2013;64(2):183–189. doi: 10.1097/QAI.0b013e3182973966. [DOI] [PubMed] [Google Scholar]
- 2.Harrison K, McDavid MPH, PhD, Song R, Zhang X. Life expectancy after HIV diagnosis based on national HIV surveillance data from 25 states, United States. J Acquir Immune Defic Syndr. 2010;53(1):124–130. doi: 10.1097/QAI.0b013e3181b563e7. [DOI] [PubMed] [Google Scholar]
- 3.Girardi E, Sabin CA, Antonella d'Arminio Monforte M. Late diagnosis of HIV infection: Epidemiological features, consequences and strategies to encourage earlier testing. J Acquir Immune Defic Synd. 2007;46(suppl 1):S3–S8. doi: 10.1097/01.qai.0000286597.57066.2b. [DOI] [PubMed] [Google Scholar]
- 4.Montlahuc C, Guiguet M, Abgrall S, Daneluzzi V. Impact of late presentation on the risk of death among HIV-infected people in France (2003–2009) J Acquir Immune Defic Synd. 2013;64(2):197–203. doi: 10.1097/QAI.0b013e31829cfbfa. [DOI] [PubMed] [Google Scholar]
- 5.Losina E, Figueroa P, Duncan J, et al. HIV morbidity and mortality in Jamaica: Analysis of national surveillance data, 1993–2005. INT J Infect Dis. 2008;12(2):132–138. doi: 10.1016/j.ijid.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waters L, Sabin CA. Late HIV presentation: Epidemiology, clinical implications and management. Expert Rev Anti Infect Ther. 2011;9(10):877–889. doi: 10.1586/eri.11.106. [DOI] [PubMed] [Google Scholar]
- 7.Wohlgemut J, Lawes T, Laing RB. Trends in missed presentations and late HIV diagnosis in a UK teaching hospital: a retrospective comparative cohort study. BMC Infect Dis. 2012;12(72) doi: 10.1186/1471-2334-12-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fideli ÜS, Allen SA, Musonda R, et al. Virologic and immunologic determinants of heterosexual transmission of human immunodeficiency virus type 1 in Africa. AIDS Res Hum Retrov. 2001;17(10):901–910. doi: 10.1089/088922201750290023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Quinn TC, Wawer MJ, Sewankambo N, et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1. New Engl J Med. 2000;342(13):921–929. doi: 10.1056/NEJM200003303421303. [DOI] [PubMed] [Google Scholar]
- 10.Wilson DP, Law MG, Grulich AE, Cooper DA, Kaldor JM. Relation between HIV viral load and infectiousness: A model-based analysis. Lancet. 2008;372(9635):314–320. doi: 10.1016/S0140-6736(08)61115-0. [DOI] [PubMed] [Google Scholar]
- 11.Xia Q, Kobrak P, Wiewel EW, Torian LV. The high proportion of late HIV diagnoses in the USA is likely to stay: Findings from a mathematical model. AIDS Care. 2015;27(2):206–212. doi: 10.1080/09540121.2014.958430. [DOI] [PubMed] [Google Scholar]
- 12.Girardi E, Aloisi M, Arici C, et al. Delayed presentation and late testing for HIV: Demographic and behavioral risk factors in a multicenter study in Italy. J Acquir Immune Defic Syndr. 2004;36(4):951–959. doi: 10.1097/00126334-200408010-00009. [DOI] [PubMed] [Google Scholar]
- 13.Poundstone K, Strathdee S, Celentano D. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiol Rev. 2004;26(1):22–35. doi: 10.1093/epirev/mxh005. [DOI] [PubMed] [Google Scholar]
- 14.Mukolo A, Villegas R, Aliyu M, Wallston KA. Predictors of late presentation for HIV diagnosis: A literature review and suggested way forward. AIDS Behav. 2013;17(1):5–30. doi: 10.1007/s10461-011-0097-6. [DOI] [PubMed] [Google Scholar]
- 15.Johnston D. Economics and HIV: The sickness of economics. New York, NY: Routledge; 2013. [Google Scholar]
- 16.Feldacker C, Ennett ST, Speizer I. It's not just who you are but where you live: An exploration of community influences on individual HIV status in rural Malawi. Soc Sci Med. 2011;72(5):717–725. doi: 10.1016/j.socscimed.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 17.Obel N. Show me your neighbours and I will tell you how you are. AIDS. 2015;29(2):239–240. doi: 10.1097/QAD.0000000000000457. [DOI] [PubMed] [Google Scholar]
- 18.Pronyk PM, Harpham T, Morison LA, et al. Is social capital associated with HIV risk in rural South Africa? Soc Sci Med. 2008;66(9):1999–2010. doi: 10.1016/j.socscimed.2008.01.023. [DOI] [PubMed] [Google Scholar]
- 19.Sivaram S, Zelaya C, Srikrishnan A, et al. Associations between social capital and HIV stigma in Chennai, India: Considerations for prevention intervention design. AIDS Educ Prev. 2009;21(3):233–250. doi: 10.1521/aeap.2009.21.3.233. [DOI] [PubMed] [Google Scholar]
- 20.Hickey M, Salmen C, Md M, et al. Implementation and operational research: Pulling the network together: Quasiexperimental trial of a patient-defined support network intervention for promoting engagement in HIV care and medication adherence on Mfangano Island, Kenya. J Acquir Immune Defic Syndr. 2015;69(4):e127–e134. doi: 10.1097/QAI.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kawachi I, Berkman L. Social Epidemiology. New York, NY: Oxford University Press; 2000. Social cohesion, social capital and health. [Google Scholar]
- 22.Kawachi I, Berkman L. Social cohesion, social capital and health. In: Kawachi I, Berkman L, Glymour M, editors. Social Epidemiology, 2nd Edition. New York, NY: Oxford University Press; 2014. pp. 291–319. [Google Scholar]
- 23.Putnam R. Making democracy work: Civic traditons in modern Italy. Princeton, NJ: Princeton University Press; 1993. [Google Scholar]
- 24.Kawachi I, Subramanian SV, Kim D, editors. Social capital and health. New York, NY: Springer Science + Business Media LLC; 2008. Actual or potential neighborhood resources for health: What can Bourdieu offer for understanding mechanisms linking social capital to health? pp. 83–94. [Google Scholar]
- 25.Blakely T, Ivory V. Commentary: Bonding, bridging, and linking—but still not much going on. Int J Epidemiol. 2006;35(3):614–615. doi: 10.1093/ije/dyl084. [DOI] [PubMed] [Google Scholar]
- 26.Kawachi I, Subramanian SV, Kim D, editors. Social capital and health. New York, NY: Springer Science + Business Media LLC; 2008. [Google Scholar]
- 27.Ware NC, Idoko J, Kaaya S, et al. Explaining adherence success in sub-Saharan Africa: An ethnographic study. PLoS Med. 2009;6(1):e1000011. doi: 10.1371/journal.pmed.1000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Putnam R. Bowling alone: America's declining social capital. J Democr. 1995;6(1):65–78. [Google Scholar]
- 29.Putnam RD. Tuning in, tuning out: The strange disappearance of social capital in America. PS Polit Sci Polit. 1995;28(04):664–683. [Google Scholar]
- 30.Kawachi I. Social capital and community effects on population and individual health. Ann NY Acad Sci. 1999;896(1):120–130. doi: 10.1111/j.1749-6632.1999.tb08110.x. [DOI] [PubMed] [Google Scholar]
- 31.Harpham T. The measurement of community social capital through surveys. In: Kawachi I, Subramanian SV, Kim D, editors. Social capital and health. New York, NY: Springer Science + Business Media LLC; 2008. pp. 51–62. [Google Scholar]
- 32.Sampson R, Raudenbush S, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 33.Gruenewald PJ, Remer L, Lipton R. Evaluating the alcohol environment: Community geography and alcohol problems. [Accessed May 18, 2014];2014 http://pubs.niaaa.nih.gov/publications/arh26-1/42.48.htm. [PMC free article] [PubMed]
- 34.Latkin C, Weeks MR, Glasman L, Galletly C, Albarracin D. A dynamic social systems model for considering structural factors in HIV prevention and detection. AIDS Behav. 2010;14(2):222–238. doi: 10.1007/s10461-010-9804-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scribner R, Theall KP, Simonsen N, Robinson W. HIV risk and the alcohol environment: Advancing an ecological epidemiology for HIV/AIDS. Alcohol Research & Health. 2010;33(3):179. [PMC free article] [PubMed] [Google Scholar]
- 36.Kerrigan D, Witt S, Glass B, Chung SE, Ellen J. Perceived neighborhood social cohesion and condom use among adolescents vulnerable to HIV/STI. AIDS Behav. 2006;10(6):723–729. doi: 10.1007/s10461-006-9075-9. [DOI] [PubMed] [Google Scholar]
- 37.Fonner VA, Kerrigan D, Mnisi Z, Ketende S, Kennedy CE, Baral S. Social cohesion, social participation, and HIV related risk among female sex workers in swaziland. PLoS One. 2014;9(1):e87527. doi: 10.1371/journal.pone.0087527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wouters E, Meulemans H, van Rensburg HCJ. Slow to share: social capital and its role in public HIV disclosure among public sector ART patients in the Free State province of South Africa. AIDS Care. 2009;21(4):411–421. doi: 10.1080/09540120802242077. [DOI] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. Today's HIV/AIDS Epidemic. [Accessed June 12, 2015];HIV/AIDS Fact Sheets. 2015 Available at: https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/todaysepidemic-508.pdf.
- 40.Karim QA, Meyer-Weitz A, Mboyi L, et al. The influence of AIDS stigma and discrimination and social cohesion on HIV testing and willingness to disclose HIV in rural KwaZulu-Natal, South Africa. Glob Public Health. 2008;3(4):351–365. [Google Scholar]
- 41.Cene CW, Akers AY, Lloyd SW, Albritton T, Hammond WP, Corbie-Smith G. Understanding social capital and HIV risk in rural African American communities. J Gen Intern Med. 2011;26(7):737–744. doi: 10.1007/s11606-011-1646-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Frumence G, Killewo J, Kwesigabo G, Nyström L, Eriksson M, Emmelin M. Social capital and the decline in HIV transmission–A case study in three villages in the Kagera region of Tanzania. SAHARA J Soc Asp H. 2010;7(3):9–20. doi: 10.1080/17290376.2010.9724964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O'Neill B, Gidengil E, editors. Gender and social capital. New York, NY: Routledge; 2005. [Google Scholar]
- 44.Lowndes V. Women, social capital and political participation. In: O'Neill B, Gidengil E, editors. Gender and social capital. New York, NY: Routledge; 2005. pp. 213–240. [Google Scholar]
- 45.Kawachi I, Kennedy BP. Income inequality and health: Pathways and mechanisms. Health Serv Res. 1999;34(1 Part 2):215–227. [PMC free article] [PubMed] [Google Scholar]
- 46.Congdon P. Suicide and parasuicide in London: a small-area study. Urban studies. 1996;33(1):137–158. [Google Scholar]
- 47.Whitley E, Gunnell D, Dorling D, Smith GD. Ecological study of social fragmentation, poverty, and suicide. BMJ. 1999;319(7216):1034–1037. doi: 10.1136/bmj.319.7216.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Congdon P. Commentary: Contextual effects: index construction and technique. Int J Epidemiol. 2004;33(4):741–742. doi: 10.1093/ije/dyh173. [DOI] [PubMed] [Google Scholar]
- 49.Kawachi I, Kennedy BP. Socioeconomic determinants of health: Health and social cohesion: Why care about income inequality? BMJ. 1997;314(7086):1037–1040. doi: 10.1136/bmj.314.7086.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hutchinson RN, Putt MA, Dean LT, Long JA, Montagnet CA, Armstrong K. Neighborhood racial composition, social capital and black all-cause mortality in Philadelphia. Soc Sci Med. 2009;68(10):1859–1865. doi: 10.1016/j.socscimed.2009.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Deaton A, Lubotsky D. Mortality, inequality and race in American cities and states. Soc Sci Med. 2003;56(6):1139–1153. doi: 10.1016/s0277-9536(02)00115-6. [DOI] [PubMed] [Google Scholar]
- 52.Fleming P, Ward JW, Janssen RS, et al. Guidelines for national human immunodeficiency virus case surveillance, including monitoring for human immunodeficiency virus infection and acquired immunodeficiency syndrome. Morb Mortal Wkly Rep. 1999;48(13):1–28. [PubMed] [Google Scholar]
- 53.Silver H, Messeri P. Concentrated poverty, racial/ethnic diversity and neighborhood social capital. In: Amina C, Davis JB, editors. Social capital and economics: Social values, power, and social identity. New York, NY: Routledge; 2014. pp. 115–139. [Google Scholar]
- 54.Lim S, Harris T. Neighborhood contributions to racial and ethinc disparities in obesity among New York City adults. Am J Public Health. 2015;105(1):159–165. doi: 10.2105/AJPH.2013.301782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stark JH, Neckerman K, Lovasi GS, et al. The impact of neighborhood park access and quality on body mass index among adults in New York City. Prev Med. 2014;64(0):63–68. doi: 10.1016/j.ypmed.2014.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schneider E, Whitmore S, Glynn KM, et al. Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years, United States, 2008. Morb Mortal Wkly Rep. 2008;57(RR10):1–8. [PubMed] [Google Scholar]
- 57.Columbia Pupulation Research Center. Social Indicators Survey (SIS) [Accessed June 12, 2015];2015 http://cupop.columbia.edu/research/research-areas/social-indicators-survey-sis. [Google Scholar]
- 58.Stata. Tetrachoric-Tetrachoric correlations for binary variables. [Accessed June 9, 2015];2015a http://www.stata.com/manuals13/rtetrachoric.pdf. [Google Scholar]
- 59.Stjärne MK, de Leon AP, Hallqvist J, Group tSS. Contextual effects of social fragmentation and material deprivation on risk of myocardial infarction—results from the Stockholm Heart Epidemiology Program (SHEEP) Int J Epidemiol. 2004;33(4):732–741. doi: 10.1093/ije/dyh087. [DOI] [PubMed] [Google Scholar]
- 60.Pabayo R, Barnett TA, Datta G, Lambert M, O'Loughlin J. Area-level social fragmentation and walking for exercise: Cross-sectional findings from the Quebec Adipose and Lifestyle Investigation in Youth Study. Am J Public Health. 2012;102(9):e30–e37. doi: 10.2105/AJPH.2012.300868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pabayo R, Molnar BE, Street N, Kawachi I. The relationship between social fragmentation and sleep among adolescents living in Boston, Massachusetts. Am J Public Health. 2014;36(4):587–598. doi: 10.1093/pubmed/fdu001. [DOI] [PubMed] [Google Scholar]
- 62.Bishaw A, Semega J, et al. Income, earnings and poverty: Data from the 2007 American Community Survey. Washington, DC: U.S. Census Bureau; 2008. [Google Scholar]
- 63.Stata. Orthog-Orthogonalize variables and compute orthogonal polynomials. [Accessed June 9, 2015];2015b http://www.stata.com/manuals13/rtetrachoric.pdf. [Google Scholar]
- 64.Sribney W. A comparison of different tests for trend. [Accessed June 25, 2013];1996 http://www.stata.com/support/faqs/statistics/test-for-trend/ [Google Scholar]
- 65.Pabayo R, Janosz M, Bisset S, Kawachi I. School social fragmentation, economic deprivation and social cohesion and adolescent physical inactivity: A longitudinal study. PLos One. 2014;9(6):e99154. doi: 10.1371/journal.pone.0099154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Holtgrave DR, Crosby RA. Social capital, poverty, and income inequality as predictors of gonorrhoea, syphilis, chlamydia and AIDS case rates in the United States. Sex Transm Infect. 2003;79:62–64. doi: 10.1136/sti.79.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mansyur C, Amick BC, Harrist RB, Franzini L. Social capital, income inequality, and self-rated health in 45 countries. Soc Sci Med. 2008;66(1):43–56. doi: 10.1016/j.socscimed.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 68.Campbell C, Williams B, Gilgen D. Is social capital a useful conceptual tool for exploring community level influences on HIV infection? An exploratory case study from South Africa. AIDS care. 2002;14(1):41–54. doi: 10.1080/09540120220097928. [DOI] [PubMed] [Google Scholar]
- 69.Marcelo KB, Lopez MH, Kirby EH. Civic engagement among young men and women. College Park, MD: The Center for Information & Research on Civic Learning & Engagement; 2006. [Google Scholar]
- 70.Skrabski Á, Kopp M, Kawachi I. Social capital in a changing society: cross sectional associations with middle aged female and male mortality rates. J Epidemiol Community Health. 2003;57(2):114–119. doi: 10.1136/jech.57.2.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.United Nations Women. Championing gender equality in the HIV response: The experiences of five programme countries. [Accessed June 23, 2015];2015 http://www.unwomen.org/~/media/headquarters/attachments/sections/library/publications/2015/9211_brief-overview.pdf. [Google Scholar]
- 72.United States Department of Health and Human Services. Rockville, MD: Health Resources and Services Administration; 2012. HIV screening for pregnant women. [Google Scholar]
- 73.Muntaner C, Lynch J. Social capital, class gender and race conflict, and population health: An essay review of Bowling Alone‘s implications for social epidemiology Bowling alone. Int J Epidemiol. 2002;31(1):261–267. [Google Scholar]
- 74.Pearce N, Davey Smith G. Is social capital the key to inequalities in health? Am J Public Health. 2003;93(1):122–129. doi: 10.2105/ajph.93.1.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Muntaner C, Lynch J. Income inequality, social cohesion, and class relations: A critique of Wilkinson's neo-Durkheimian research program. Int J Health Serv. 1999;29(1):59–81. doi: 10.2190/G8QW-TT09-67PL-QTNC. [DOI] [PubMed] [Google Scholar]
- 76.Kushner HI, Sterk CE. The limits of social capital: Durkheim, suicide, and social cohesion. Am J Public Health. 2005;95(7):1139–1143. doi: 10.2105/AJPH.2004.053314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Moore S, Daniel M, Gauvin L, Dubé L. Not all social capital is good capital. Health Place. 2009;15(4):1071–1077. doi: 10.1016/j.healthplace.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 78.van Hooijdonk C, Droomers M, Deerenberg IM, Mackenbach JP, Kunst AE. The diversity in associations between community social capital and health per health outcome, population group and location studied. Int J Epidemiol. 2008;37(6):1384–1392. doi: 10.1093/ije/dyn181. [DOI] [PubMed] [Google Scholar]
- 79.Muntaner C, Lynch J, Davey Smith G. Social capital, disorganized communities, and the third way: Understanding the retreat from structural inequalities in epidemiology and public health. Int J Health Serv. 2001;31:213–237. doi: 10.2190/NVW3-4HH0-74PX-AC38. [DOI] [PubMed] [Google Scholar]
- 80.Gregson S, Mushati P, Grusin H, et al. Social capital and women's reduced vulnerability to HIV infection in rural Zimbabwe. Popul Dev Rev. 2011;37(2):333–359. doi: 10.1111/j.1728-4457.2011.00413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]